Abstract
Prosthetic joint infection is an unfortunate though well-recognized complication of total joint arthroplasty. An iliacus and/or iliopsoas muscle abscess is a rarely documented presentation of hip prosthetic joint infection. It is thought an unrecognized retroperitoneal nidus of infection can be a source of continual seeding of the prosthetic hip joint, prolonging attempts to eradicate infection despite aggressive debridement and explant attempts. The current study presents five cases demonstrating this clinical scenario, and discusses various treatment challenges.
In each case we report the patient's clinical history, pertinent imaging, management and outcome. Diagnosis of the iliacus muscle abscess was made using computed tomography imaging. In brief, the mean number of total drainage procedures (open and percutaneous) per patient was 4.2, and outcomes consisted of one patient with a hip girdlestone, two patients with delayed revisions, and two patients with retained prosthesis. All patients ended with functional pain and on oral antibiotic suppression with an average follow up of 18 months.
This article highlights an iliacus muscle abscess as an unrecognized source of infection to a prosthetic hip. It demonstrates resilience to standard treatment protocols for prosthetic hip infection, and is associated with poor patient outcomes. Aggressive surgical debridement appears to remain critical to treatment success, and early retroperitoneal debridement of the abscess should be considered.
Keywords: iliopsoas abscess, total hip arthroplasty, prosthetic joint infection.
Introduction
Prosthetic joint infection (PJI) is a serious complication after total joint arthroplasty with a reported incidence of 1-3%1, 2. Treatment options range from incision and drainage (I&D) to one or two-stage revision, or even resection arthroplasty3. Success rates of the gold standard two-stage revision have been reported as high as 66% to 90%4, 5, though there is a well-recognized subset of patients with refractory, chronic PJI despite appropriate treatment measures. The etiology remain multifactorial, with suggested reasons for treatment failure associated with patient comorbidity burden, organism virulence and the quality of debridement5, 6. In the setting of hip PJI, a more unusual factor influencing treatment success is the presence of an infectious source not managed by standard debridement, such as an iliacus muscle abscess (IMA).
An IMA and/or an iliopsoas abscess in the context of hip PJI is an infrequently documented clinical phenomenon. Single case reports make up the majority of the literature7-13, highlighting its under recognition. Computed tomography (CT) or magnetic resonance imaging (MRI) is required for diagnosis, though neither are routinely recommended by MSIS consensus guidelines in the diagnosis of PJI14. Therefore, IMA undoubtedly presents a unique challenge to clinicians, because it may serve as an unrecognized chronic source of persistent infection.
The purpose of this series is to review five cases at a tertiary medical center between 2009-2015 that demonstrate the challenges in treating hip PJI associated with IMA. We compare our outcomes to the current literature, as well as delineate the anatomic etiology behind IMA association with hip PJI. Lastly, surgical treatment strategies are discussed as we seek to better manage this difficult complication of hip PJI.
Case Reports
Case 1
A 64-year-old female status post right total hip arthroplasty (THA) six years prior presented acutely ill, febrile with right groin pain. She was admitted with Staphylococcus aureus bacteremia. A CT scan of the pelvis revealed a right IMA (Fig. 1A). She underwent a retroperitoneal debridement of the iliacus muscle and a hip I&D followed by an explant of all hardware. Repeat CT imaging three weeks later revealed a persistent right IMA, and new left IMA (Fig. 1B). She underwent debridement of both through bilateral retroperitoneal approaches. A percutaneous CT guided drain was placed in the left iliacus abscess. Right hip cultures revealed superinfections with Serratia marcescens and Enterococcus faecalis, in addition to known Staphylococcus aureus. Additionally, she underwent five I&D procedures for a native right septic wrist. She was discharged after a two-month admission with a wound vac over the soft tissue wounds, on intravenous (IV) antibiotics. At seven-months post-op, she wears a two-inch shoe lift utilizing crutches for ambulation, and showed complete healing of her wound.
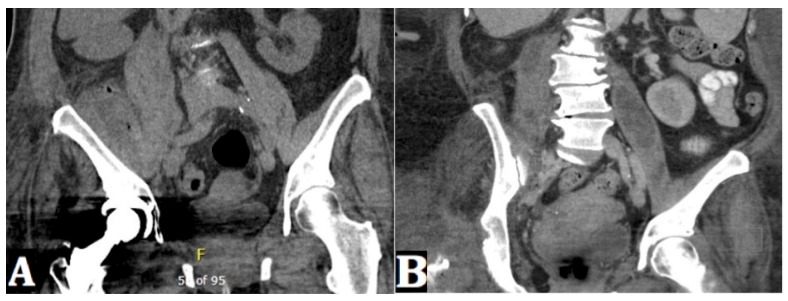
Figure 1.
(A) A coronal CT pelvis image shows fluid and gas within the enlarged right iliacus and iliopsoas musculature. (B) A repeat coronal CT pelvis image (at one month from index imaging) shows an interval development of fluid collection within the right posterior pararenal space/right psoas muscle while there has been interval resolution of loculated fluid collection within the right iliacus muscle region. Right hip hardware has been removed. Additionally, there has been interval development of a loculated fluid collection within the left psoas muscle.
Case 2
A 73-year-old man status post bilateral THA four years prior presented with a painful left hip. A CT scan of the pelvis revealed a fluid collection in the left iliacus muscle (Fig. 2A). The hip was aspirated and a percutaneous CT guided drain was placed in the abscess. Both samples grew Propionibacterium acnes (P. acnes). He underwent explant of the infected prosthesis with antibiotic laden spacer placement. Repeat CT imaging at six weeks following antibiotic treatment revealed persistent abscess (Fig. 2B), and he underwent retroperitoneal debridement of the iliacus muscle. Intraoperative cultures grew Candida parapsilosis. After six weeks of IV antibiotics, repeat CT scan revealed persistent abscess. He underwent two sequential retroperitoneal I&D's and two antibiotic spacer exchanges. Repeat CT imaging revealed a substantially smaller fluid collection in the iliacus muscle (Fig. 2C). After a final course of IV antibiotics a revision hip prosthesis was finally re-implanted 13 months after initial presentation. At ten months post-op, patient is ambulating with minimal limp on lifelong suppressive antibiotics (Fig. 2D).
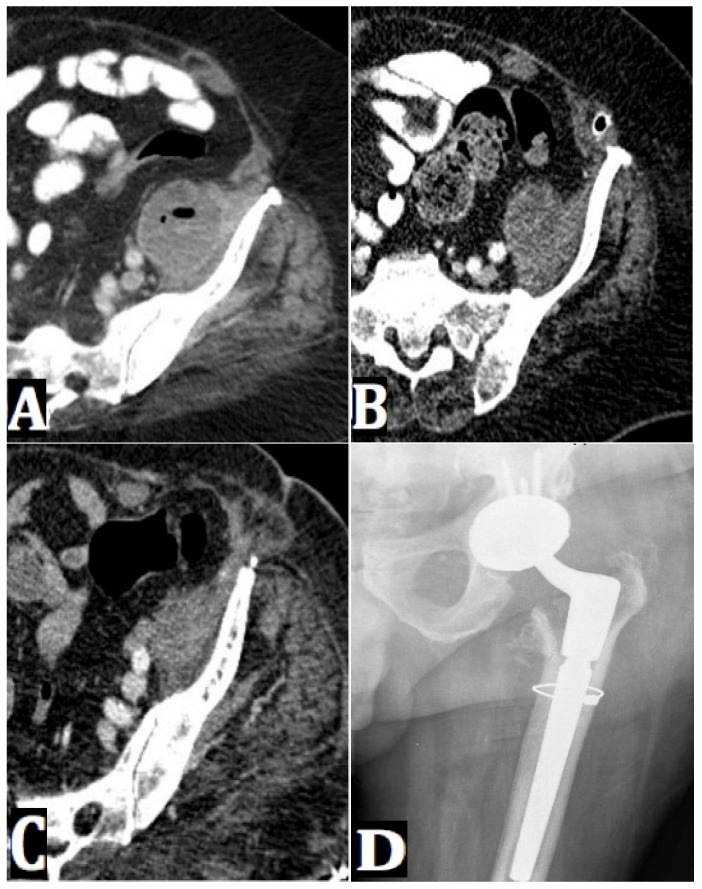
Figure 2.
(A) An axial CT pelvis image shows a fluid collection in the left iliacus muscle. (B) A repeat axial CT pelvis image (at six weeks from index imaging) shows no significant change in size of the left iliacus abscess. (C) A repeat axial CT pelvis image (at four months from index imaging) shows a decrease in size of the left iliacus abscess. This occurred following three retroperitoneal debridements, and two spacer exchanges. (D) An AP radiograph of the left hip shows a left hip revision arthroplasty with a cerclage wire in proximal femur and components in expected position. There is no evidence of radiographic loosening at 10 months post-op.
Case 3
A 63-year-old man status post right THA seven years prior underwent an explant and spacer placement for PJI with P. acnes. Following six weeks of IV antibiotics, inflammatory markers remained elevated and right hip joint aspirate revealed 23,000 white blood cells (WBC) with 92% neutrophils. Due to elevated clinical suspicion, a CT scan was obtained, revealing a fluid collection in the right iliacus muscle (Fig. 3A, 3B). He underwent a spacer exchange where gross purulence was noted down into the anterior pelvic brim where the iliopsoas tendon crossed over the anterior hip capsule - decompressed thru an extra-pelvic approach. After the second course of IV antibiotics, a right hip aspirate showed persistent infection, and repeat CT images revealed an unchanged IMA (Fig. 3C). Along with a second spacer exchange, the iliacus muscle was debrided via a retroperitoneal approach - intra-operative cultures did not yield culture growth. After a third six-week course of IV antibiotics, inflammatory markers had normalized, and a revision THA was implanted (Fig. 3D). Intraoperative cultures unfortunately grew a single colony of P. acnes. The patient is performing activities of daily living without limitation at ten months post-op on lifelong oral antibiotics.
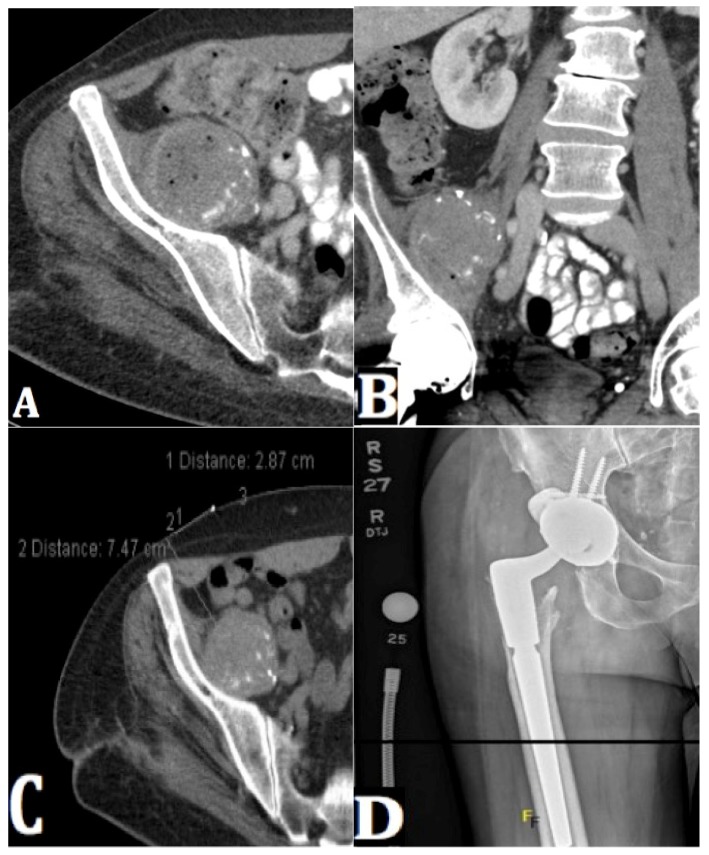
Figure 3.
(A) An axial CT pelvis shows fluid distension with intermittent gas in the right iliacus muscle, also containing scattered calcifications. (B) A coronal CT pelvis image shows fluid distension with intermittent gas in the right iliacus muscle, also containing scattered calcifications. This was biopsy and aspirate proven to be consistent with infected hematoma. Notably, the patient was on Coumadin following his initial primary THA operation. (C) A repeat axial CT pelvis image reveals a persistent right iliacus abscess. (D) An AP radiograph of the right hip shows a right hip revision arthroplasty with hardware intact and no evidence of loosening at four months post-op.
Case 4
A 64-year-old woman with a multiply revised right THA for instability presented with chronic low back pain for several months, and new fevers. Radiographs were obtained (Fig. 4A). Given the chronicity of her symptoms, a CT scan was also obtained and revealed a right IMA (Fig. 4B). An aspirate of the right hip joint and the iliacus fluid collection both grew Coagulase negative Staphylococcus (CoNS), and a CT-guided drain was placed into the abscess. Two-stage revision was not advised given her poor bone quality and soft tissue envelope, unlikely to withstand another large revision surgery. She was treated with a course of IV antibiotics. For the next three years, her right hip was functional, though continued to have baseline pain that did not limit her. During routine follow-up with her spine surgeon for known lumbar stenosis, a CT scan of the lumbar spine revealed an enlarging right IMA, confirmed by subsequent dedicated CT pelvis (Fig. 4C). Hip and iliacus collection aspirates both revealed CoNS. She underwent a retroperitoneal approach to a multi-loculated necrotic mass that tracked down the iliopsoas tendon into the hip joint (Fig. 4D). Approximately 50% of the muscle was debrided (Fig. 4E), and the hip joint was debrided through a direct lateral arthrotomy, foregoing explantation after extensive conversations with the patient. Intraoperative cultures grew CoNS. She was discharged on a course of IV antibiotics followed by lifelong suppression with oral antibiotics. She reports previous pain has resolved in her right hip at ten months post-op.
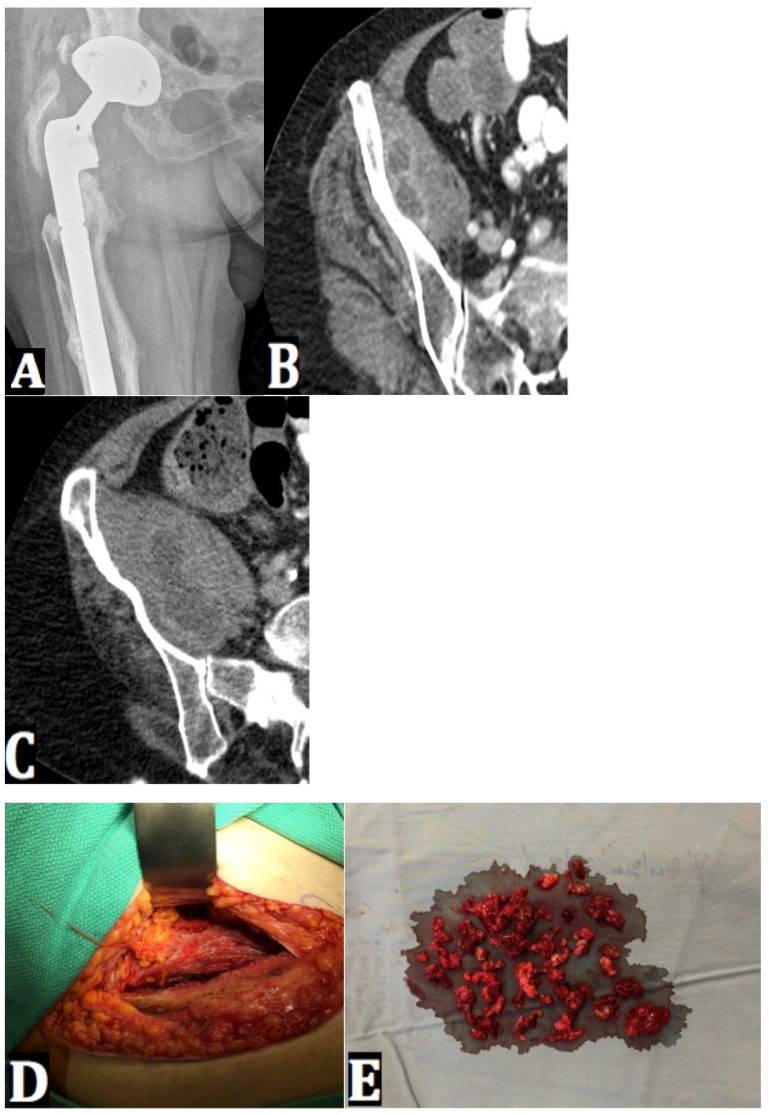
Figure 4.
(A) An AP radiograph of the right hip shows a revision hip prosthesis with minimal femoral bone stock and lucency surrounding the femoral stem. The component position has not changed over a ten-year period. (B) An axial CT right hip image shows new enlargement of right iliacus muscle containing multi-loculated fluid collection. (C) A repeat axial CT right hip image of the right hip shows an interval increase in size of the collection in the right iliacus muscle. (D) An intraoperative photo of the retroperitoneal approach to the inner table of pelvis shows the point of access to the proximal belly of the iliacus muscle. (E) An intraoperative photo shows debrided iliacus muscle abscess tissue.
Case 5
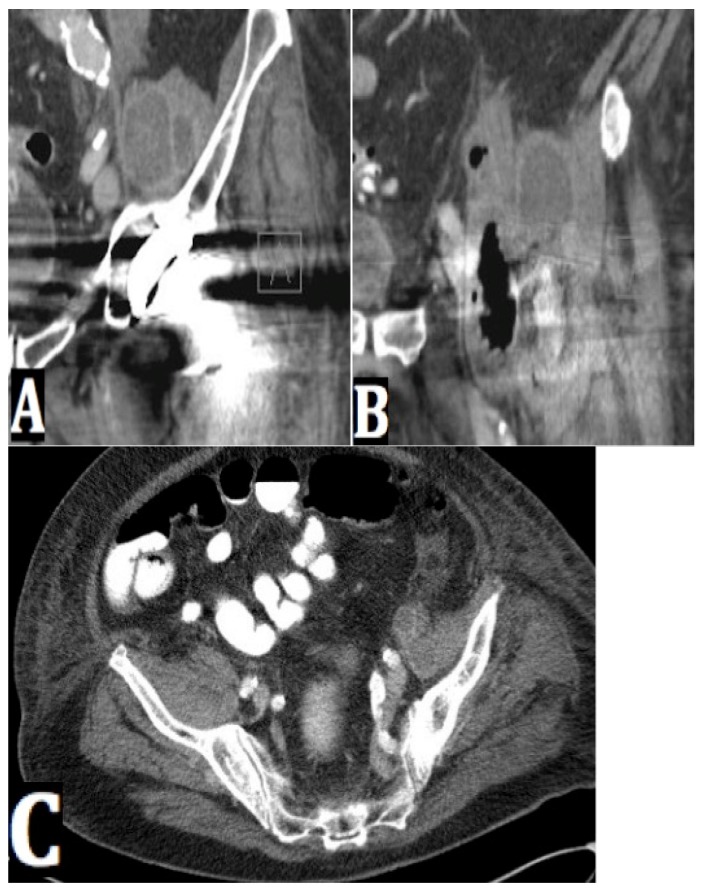
An 87-year-old man status post bilateral THA fifteen years prior developed several days of confusion, bilateral hip pain and flu-like symptoms. A CT scan of the pelvis revealed bilateral iliacus muscle abscesses extending into iliopsoas bursa (Fig. 5A-C). He underwent a bilateral hip prosthesis femoral head/liner exchange - intraoperative cultures grew Bacteroides fragilis. The patient was placed on six weeks of IV antibiotics and subsequent oral suppression antibiotics. During an attempt to taper the dose of oral suppressive antibiotics, his symptoms recurred one year later. CT imaging revealed recurrence of bilateral iliac muscle abscesses with Bacteroides fragilis, without proven bowel fistula communication. Staged debridements and head and liner exchanges of both hips were carried out. Components were once again noted to be well fixed. He was placed on IV antibiotics and remains on high dose oral antibiotic suppression thereafter at nine months post-op.
Figure 5.
(A) A coronal CT left hip image shows a large retroperitoneal fluid collection in the iliacus left muscle. (B) A coronal CT left hip image in a more distal image cut than Figure A shows fluid and gas extending down the iliopsoas tendon to the level of the hip joint. (C) An axial CT pelvis image reveals bilateral fluid collections in the left and right iliacus muscle.
Discussion
IMA poses a diagnostic and treatment dilemma in the setting of hip PJI. This series highlights six iliacus muscle abscesses in five patients with ipsilateral hip PJI. Key findings are summarized in Table 1. Mean patient age was 70 years old (range 63-87). Diagnosis of IMA required CT imaging. The mean number of hip and/or abscess drainage procedures per patient was 4.2 (range 2-9). Causative organisms varied. Two patients developed superinfections with indolent and multidrug-resistant organisms. Four of five patients underwent hospital readmission (three unplanned) for an abscess refractory to initial treatment. Overall outcomes included one patient with hip girdlestone, two with delayed revisions and two with retained prosthesis. Average follow up from time of diagnosis with CT imaging was 21.8 months (range 7-42).
Table 1.
Case data and outcomes.
| Case | Age/Sex | Past Surgical History | Presentation | Type of Drainage Procedure | Organism(s) | Follow-up from time of Diagnosis (months) | Clinical Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 64/F | R THA 6 years prior | Fevers, R groin pain x2 weeks, decreased urine output | PCTD x1 and open x3 - explant | MSSA; Serratia marcesens and Enterococcus faecalis superinfection |
7 | Hip girdlestone |
| 2 | 73/M | Bilateral THA 4 years prior | L hip pain x6 weeks | PCTD x2 and open x7 - explant w/spacer | Propionibacterium acnes; Candida parapsilosis superinfections | 23 | Revision THA |
| 3 | 63/M | R THA 7 years prior | R hip pain x4 weeks | Open x2 - explant w/spacer | Propionibacterium acnes | 16 | Revision THA |
| 4 | 64/F | R THA multiply revised x5 for instability | Low back pain for several months and fevers x1 week | PCTD x1 and open x1 - I&D | CoNS | 42 | Retained prosthesis |
| 5 | 87/M | L THA and R THA 15 years prior | Bilateral hip pain, confusion and flu like symptoms for several days | Open x4 - I&D w/head and liner exchanges | Bacteroides fragiles | 21 | Retained prostheses |
M = male; F = female; L = left; R = right; THA = total hip arthroplasty; PCTD = percutaneous CT guided drainage; MSSA = methicillin sensitive staphylococcus aureus; I&D = incision and drainage; CoNS = coagulase negative staphylococcus; CRAB = carbapenem resistant acinetobacter baumannii.
Table 2 summarizes key findings from the case reports in the literature7-12. In general, the current literature would indicate more favorable outcomes than our series. Five of six case reports in the literature either underwent percutaneous intervention and washout resulting in prosthesis retention or two-stage exchange with successful reimplantation, without requiring multiple two stage exchanges or retroperitoneal debridements. Functionally, all patients in our series reported pain to varying degrees, which is contrasted to the large majority of asymptomatic patients reported in prior literature.
Table 2.
Literature review: data and outcomes.
| Case | Age/Sex | Past Surgical History | Presentation | Type of Drainage Procedure | Organism(s) | Follow-up (months) | Clinical Outcome |
|---|---|---|---|---|---|---|---|
| Buttaro et al 2002 [7] | 65/M | L THA 11 years prior | Fevers and low back pain x6 months | Open - explant and PCTD | Escherichia coli | 12 | Hip girdlestone |
| Plaza et al 2006 [12] | 46/F | L THA 10 years prior with revision THA for instability | Lumbar pain x2 months | PCTD x1, Open x1 - explant w/spacer | No organism identified | 24 | Revision THA (Asymptomatic) |
| Querton 2009 [9] | 77/M | R THA 3 years prior | Fevers x3 days, back pain, erythema and warmth in R groin | Open - explant w/spacer | Group C Streptococcus | 15 | Revision THA (Asymptomatic) |
| De Nardo et al 2012 [11] | 67/F | L THA 1.5 years prior | L hip pain and stiffness | PUSD x1, Open x2 - I&D | Mycobacterium tuberculosis | 15 | Retained prosthesis (Asymptomatic) |
| Dhinsa et al 2014 [8] | 81/M | R THA 6 years prior | Fevers, lethargy, R hip pain x2 weeks | Open x1 - I&D, PUSD x1 | Staphylococcus aureus | 24 | Retained prosthesis (Asymptomatic) |
| Volpin et al 2015 [10] | 68/F | L THA 20 years prior, R THA 8 years prior | Bilateral dull hip pain x6 months | Bilateral Open - explant w/spacer | Streptococcus aginosus | 60 | Revision THA (Asymptomatic) |
M = male; F = female; L = left; R = right; THA = total hip arthroplasty; PUSD = percutaneous ultrasound guided drainage; I&D = incision and drainage.
Aggressive surgical debridement appears to remain important in the management consideration of IMA. In two of our five cases (cases 2 and 3), our results highlight that explant and multiple spacer exchanges can fail if the iliacus muscle abscess is not directly debrided in a concurrent manner. The iliacus muscle sits in a retroperitoneal location within the pelvis, originating off the inner table of the innominate bone. The psoas muscle originates off the transverse processes of the lumbar vertebrae, and comes to a confluence with the iliacus muscle as the two exit the pelvis over the anterior pelvic brim, and travel intimately with the anterior hip capsule to insert onto the lesser trochanter of the proximal femur. Based upon the anatomic proximity of the iliopsoas bursa to the anterior hip capsule and frequent communication with the hip joint as described by Steinbach et al., it is theorized IMA develops from a hip PJI in a directly seeded fashion15. Bacteria infect the joint, seed the iliopsoas tendon and/or bursa, track proximally and harbor in the iliacus muscle where it generates a reservoir to feed the joint through the tendon. Only after a separate retroperitoneal debridement of the iliacus muscle was performed in cases 2 and 3 did the clinical infection clear from the hip joint, allowing for re-implanation of a revision hip prosthesis, and eventual improvement. Even with prompt explant and multiple retroperitoneal debridements, however, elimination of the IMA is not guaranteed (case 1).
Alternative to contiguous bacterial spread, IMA may develop from hematogenous seeding of a preexisting sterile collection in the iliacus muscle. In the setting of a prosthetic hip joint, a fluid collection can form due to adverse local tissue reaction (ALTR) - formerly known as particle matter disease. Though historically more associated with osteolysis in metal-on-metal arthroplasty, non-specific ALTR is thought to occur in various types of bearing surfaces16, 17. This type of particle matter disease could be responsible for a local inflammatory response that forms an intra-muscular fluid collection that is seeded during bacteremia.
Aggressive hip synovectomy with or without head/liner exchange was performed in two of five cases (cases 4 and 5). A simple debridement with head/liner exchange may only be a temporizing measure, as case 5 ultimately recurred with bilateral IMA requiring repeat debridements. “Less is more” may be a mantra to follow in select patients where explantation of implants is a relative contraindication due to poor bone stock and lack of reconstructive options available - focusing instead on abscess debridement and implant retention. As a point of emphasis, percutaneous CT-guided drainage was not successful in clearing local infection in all three cases it was utilized, thus, additional invasive procedures were needed to address persistent infection collections.
Overall, these findings stimulate discussion as to how aggressive and what type of debridement is sufficient. Though this report is limited by its small case series nature in drawing any definitive conclusions, our initial findings have led our group to advocate for aggressive surgical debridement at the hip joint (often explant, with or without spacer placement) with additional retroperitoneal debridement of the abscess at the proximal muscle belly.
This report represents the second largest case series describing iliacus and/or psoas muscle abscesses associated with hip PJI. In 2009, Dauchy et al. performed a retrospective analysis of patients with hip PJI and using abdominal CT scans, described a 12% (13/106) IMA incidence18. While the authors performed a lower mean amount of drainage procedures than this current series (1.76 vs. 4.2), they did report 3 of 13 abscesses remained persistent after prosthesis explant, indicating a similar resilience of these abscesses. Logistic regression analysis led to their recommendation that CT scan be considered on patients with hip PJI with hematogenous etiology, or past medical history of neoplasm to look for concomitant IMA. Further investigation into the incidence of IMA and hip PJI may lead to more strategic treatment plans for these patients.
Conclusion
The current cases demonstrate IMA as a serious consideration with hip PJI that can be associated with multiple surgical procedures, intravenous antibiotic courses, hospital readmissions, and significant morbidity. While the incidence of IMA with hip PJI is unknown, heightened clinical suspicion to order advanced pelvis imaging may help us to better delineate epidemiology, with further follow-up determining whether aggressive management with separate open retroperitoneal abscess debridement is indicated.
References
- 1.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop. 2008;466(7):1710–1715. doi: 10.1007/s11999-008-0209-4. doi:10.1007/s11999-008-0209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg Br. 2003;85(7):956–959. doi: 10.1302/0301-620x.85b7.14095. [DOI] [PubMed] [Google Scholar]
- 3.Parvizi J, Adeli B, Zmistowski B, Restrepo C, Greenwald AS. Management of periprosthetic joint infection: the current knowledge: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(14):e104.. doi: 10.2106/JBJS.K.01417. doi:10.2106/JBJS.K.01417. [DOI] [PubMed] [Google Scholar]
- 4.Chen S-Y, Hu C-C, Chen C-C, Chang Y-H, Hsieh P-H. Two-Stage Revision Arthroplasty for Periprosthetic Hip Infection: Mean Follow-Up of Ten Years. BioMed Res Int. 2015;2015:345475.. doi: 10.1155/2015/345475. doi:10.1155/2015/345475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sherrell JC, Fehring TK, Odum S. et al. The Chitranjan Ranawat Award: fate of two-stage reimplantation after failed irrigation and débridement for periprosthetic knee infection. Clin Orthop. 2011;469(1):18–25. doi: 10.1007/s11999-010-1434-1. doi:10.1007/s11999-010-1434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zmistowski B, Tetreault MW, Alijanipour P, Chen AF, Della Valle CJ, Parvizi J. Recurrent periprosthetic joint infection: persistent or new infection? J Arthroplasty. 2013;28(9):1486–1489. doi: 10.1016/j.arth.2013.02.021. doi:10.1016/j.arth.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 7.Buttaro M, González Della Valle A, Piccaluga F. Psoas abscess associated with infected total hip arthroplasty. J Arthroplasty. 2002;17(2):230–234. doi: 10.1054/arth.2002.28734. [DOI] [PubMed] [Google Scholar]
- 8.Dhinsa BS, Abdul-Jabar HB, Rajkumar S, Kochhar T. A rare case of primary psoas abscess causing hip pain in a patient with hip replacement. Acta Orthop Traumatol Turc. 2014;48(5):598–601. doi: 10.3944/AOTT.2014.2994. [DOI] [PubMed] [Google Scholar]
- 9.Querton L, Tintillier M, Chaput A, Cuvelier C, Pochet JM. Group C streptococcal psoas abscess associated with a homolateral hip joint prosthesis infection: a case report. Acta Clin Belg. 2009;64(4):361–365. doi: 10.1179/acb.2009.058. doi:10.1179/acb.2009.058. [DOI] [PubMed] [Google Scholar]
- 10.Volpin A, Kini SG, Berizzi A. Psoas muscle pyogenic abscess in association with infected hip arthroplasty: a rare case of simultaneous bilateral presentation. BMJ Case Reports; 2015. p. 2015. doi:10.1136/bcr-2015-209711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Nardo P, Corpolongo A, Conte A, Gentilotti E, Narciso P. Total hip replacement infected with Mycobacterium tuberculosis complicated by Addison disease and psoas muscle abscess: a case report. J Med Case Reports. 2012;6:3.. doi: 10.1186/1752-1947-6-3. doi:10.1186/1752-1947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plaza R, Soriano A, Tomas X, Gallart X, Garcia S. Psoas abscess associated with infected total hip arthroplasty: a case report. Hip Int J Clin Exp Res Hip Pathol Ther. 2006;16(3):234–237. doi: 10.1177/112070000601600310. [DOI] [PubMed] [Google Scholar]
- 13.Lopez-Zabala I, Garcia-Ramiro S, Bori G. Psoas abscess associated with hip arthroplasty infection. Rev Española Quimioter Publicación Of Soc Española Quimioter. 2013;26:198–202. [PubMed] [Google Scholar]
- 14.Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Jt J. 2013;95(11):1450–1452. doi: 10.1302/0301-620X.95B11.33135. doi:10.1302/0301-620X.95B11.33135. [DOI] [PubMed] [Google Scholar]
- 15.Steinbach LS, Schneider R, Goldman AB, Kazam E, Ranawat CS, Ghelman B. Bursae and abscess cavities communicating with the hip. Diagnosis using arthrography and CT. Radiology. 1985;156(2):303–307. doi: 10.1148/radiology.156.2.4011891. doi:10.1148/radiology.156.2.4011891. [DOI] [PubMed] [Google Scholar]
- 16.Bauer TW, Campbell PA, Hallerberg G, Biological Working Group. How have new bearing surfaces altered the local biological reactions to byproducts of wear and modularity? Clin Orthop. 2014;472(12):3687–3698. doi: 10.1007/s11999-014-3817-1. doi:10.1007/s11999-014-3817-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carli A, Reuven A, Zukor DJ, Antoniou J. Adverse soft-tissue reactions around non-metal-on-metal total hip arthroplasty - a systematic review of the literature. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S47–51. [PubMed] [Google Scholar]
- 18.Dauchy F-A, Dupon M, Dutronc H. et al. Association between psoas abscess and prosthetic hip infection: a case-control study. Acta Orthop. 2009;80(2):198–200. doi: 10.3109/17453670902947424. doi:10.3109/17453670902947424. [DOI] [PMC free article] [PubMed] [Google Scholar]