Abstract
Introduction:
Elbow epicondylar tendinitis is a common problem for patients whose activities require strong gripping or repetitive wrist movements in the day-to-day activities of life. Histologic specimens from chronic cases confirm that tendinitis is not an acute inflammatory condition but rather a failure of the normal tendon repair mechanism associated with angiofibroblastic degeneration. Tendon regeneration may be improved by injecting autologous growth factors obtained from the patient's own blood. Autologous growth factors can be injected with autologous whole blood or platelet-rich plasma (PRP).
Materials and Methods:
A randomized study with 83 patients was done. The study population comprised two groups. Group A (n = 50) treated with local steroid injection and Group B (n = 33) treated with autologous PRP. Patients were allocated randomly using computer-generated random number table. The base-line evaluation was done using visual analog score (VAS) and modified Mayo performance index for elbow (MAYO). Re-evaluation was after 1, 2, and 6 months of the procedure. Statistical analysis was done using independent t-test.
Results:
Six months after treatment with PRP, patient's with elbow epicondylitis had a significant improvement in their VAS (P < 0.05) and MAYO (P < 0.05) in contrast to steroid, whereas no statistical difference was found between the two groups at 1 and 2 months after intervention.
Conclusion:
Treatment of patients with epicondylitis with PRP reduces pain and significantly increases function, exceeding the effect of corticosteroid injection.
Keywords: Corticosteroid injection, elbow epicondylitis, platelet-rich plasma
Introduction
With an annual incidence of 4–7/1000, epicondylitis is the most common problem of the elbow in the age group between 35 and 54 years. Although these conditions affect opposite sides of the elbow, the underlying pathology is similar and lateral epicondylitis (tennis elbow) is more common than medial (Golfer's elbow).[1]
It is believed that the lesion starts as a tear in the common extensor tendon caused by mechanical overloading and is followed by abnormal microvascular responses. The microscopic finding demonstrates immature tissue that resembles angiofibroblastic hyperplasia;[2,3] however, it is uncertain about the pathophysiology of epicondylitis.
Numerous treatment modalities have been mentioned in literature for the management of epicondylitis including nonsteroidal anti-inflammatory drugs, physiotherapy, local anesthetics, autologous blood constituents, etc.[4,5,6,7,8,9] Corticosteroid injections are the gold standard, but they have a short-term effect (2–6 weeks).[10]
Autologous platelet-rich plasma (PRP) delivered into various tissues to achieve a high local concentration of platelet-derived growth factors has been shown to enhance healing in wounds, tendons, and bones.[11] We believe that supplementing the natural healing process with PRP would give better long-term results in the management of epicondylitis as compared to local corticosteroids. In this study, we compared the short-term and long-term outcomes of corticosteroid injection and autologous PRP injection in cases of elbow epicondylitis randomly selected for treatment modality.
Materials and Methods
Institutional Ethics Committee clearance was taken before starting the research. One hundred and thirty cases with a primary diagnosis of elbow epicondylitis were recruited in this study over a period of 15 months after taking written informed consent. A computer random number table for two intervention groups was generated, and the patients were distributed according to the table randomly after subjecting them to the exclusion criteria. Cases with the following conditions were excluded from the study, age <18 years, diabetes mellitus, cervical radiculopathy, rheumatoid arthritis, pregnancy, hemoglobin <10 mg/dl, platelet count <1.5 lakh/cumm, patients on aspirin, or similar drugs. Pain and elbow function were assessed using the visual analog score (VAS) and modified Mayo performance index for elbow (MAYO), respectively. Plain anterioposterior and lateral radiographs of affected elbow were obtained for all the patients. Patients were randomly divided into two groups. Group I received steroid (80 mg of methyl prednisolone + 1 ml of lignocaine) and Group II received PRP (2 ml of PRP + 1 ml of lignocaine). All infiltrations were done under sterile condition by the senior author using a 22 gauge needle at the most tender point. After the injection, the patient was kept in a supine position for 15 min and then was sent home with instructions to limit the use of the arm for at least 24 h. All interventions were carried out on the outpatient basis, and patients were called for follow-up at 1, 2, 6 months, and 1 year.
Statistical analysis was done using the IBM SPSS Version 22 software. Quantitative data were expressed in terms of mean ± standard deviation. Independent t-test was used to compare the means of the study groups.
Preparation of platelet-rich plasma
Patients in the autologous PRP group were subjected to a platelet count. Only those with counts above 1.5 lakh/cumm were selected for the study. A volume of 200 ml whole blood was collected in a standard 350 ml blood bag after removal of 21 ml of anticoagulant from the blood bag. The blood was collected on a biomixer (Terumo Pempol D 601) for continuous running of blood. The bag was kept at room temperature (20°C–24°C), and separation was carried out as soon as possible. The blood was centrifuged using a light/soft spin with 1400 rpm at 22°C for 10 min. The supernatant was expressed into the transfer bag intended for platelet storage. The tubing was sealed twice and cut between the two seals. This bag was further centrifuged at 20°C using a heavy spin with 3500 rpm for 10 min. The “platelet-poor plasma” was expressed out into another bag, and tubing was sealed. Some plasma was left along with the settled platelets. The product was kept stationary at room temperature for approximately 1 h. Platelets were then transferred to platelet agitator at 20–24°C. The prepared unit was inspected for swirling movement, and platelet count was one prior to intervention.
Results
After exclusion, we had a total of 112 cases; 62 in Group I and 50 in Group II. Twelve patients in Group I and 17 patients in Group II were lost to follow-up at the end of 6 months. We had a total of 83 patients; 50 in Group I and 33 in Group II for analysis in the end.
There were 39 (46.98%) males and 44 (53.01%) females. Thirty-three (39.75%) patients were between >20–40 years, 44 (53.01%) patients were in the age group of >40–≤60 years, while 6 (7.22%) patients were more than 60 years. Sixty-three (75.90%) patients had lateral epicondylitis (Tennis elbow), and 20 (24.09%) patients had medial epicondylitis (Golfer's elbow). The right side was involved in 61 (73.49%) patients, while 22 (26.50%) had their left side involved.
On plain radiograph, there was no abnormality detected in any of the affected elbows. Baseline scores and scores at follow-up are described in Tables 1 and 2.
Table 1.
Comparison of visual analog score in the study groups
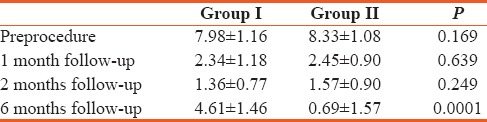
Table 2.
Comparison of Mayo score in the study groups
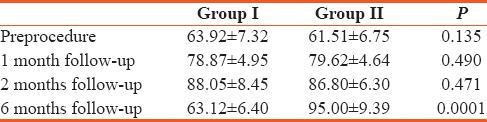
Initially, PRP-treated patients had a mean VAS of 8.33 and mean MAYO score of 61.51. The steroid-treated patients had a mean VAS of 7.98 and MAYO score of 63.92.
One month after the procedure, PRP-treated patients reported a mean of 70% improvement (8.33–3.45) in VAS scores versus 70.6% improvement (7.98–2.34) in PRP group. Both had a favorable outcome at 1 month with no significant difference (P = 0.639). Furthermore, after 1 month MAYO scores had improved 29.4% (61.51–79.62) in PRP-treated patients versus 23.3% improvement (63.92–78.87) in steroid group with no statistically significant difference (P = 0.490).
Similar results were observed at the end of 2 months, and both the treatment modalities were comparable with P = 0.249 and 0.471, respectively, for VAS and MAYO score.
At the end of 6 months, the PRP-treated patients showed a mean 91% improvement (8.33–0.69) in VAS score as compared to 42.2% improvement (7.98–4.61) in steroid-treated patients, with a significant difference between the two groups (P = 0.0001). MAYO elbow scores also showed a favorable response in PRP-treated patients with a mean 54.4% improvement (61.51–95.0) as compared to 1.25% improvement (63.92–63.12) in steroid-treated patients, which showed a significant difference (P = 0.0001).
Corticosteroid and PRP proved to be equally effective at short-term follow-up (1 and 2 months), while PRP was still superior to steroid when patients were evaluated at 6 months.
Postinjection exacerbation of pain was present in 15 patients, 5 in steroid and 10 in PRP group, which was managed by oral analgesics (aceclofenac + paracetamol) for 2 days. None of the patients had any sign of infection after the procedure [Figures 1 and 2].
Figure 1.
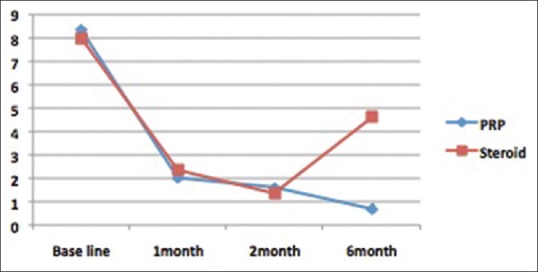
Comparison of visual analog scores
Figure 2.
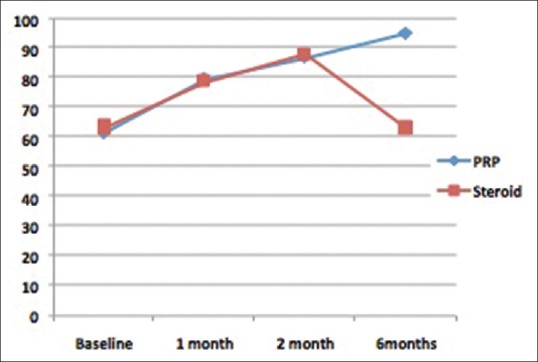
Comparison of modified Mayo performance index for elbow scores
Discussion
Lateral epicondylitis is a common problem with many available treatment options. The most commonly recommended treatment is rest, physiotherapy, and bracing. Approximately, 87% patients benefit from this combination of treatment methods.[12]
Smidt et al. in their randomized control trial compared corticosteroid injection, physiotherapy, and wait and see policy for the treatment of lateral epicondylitis and concluded that corticosteroid injections are the best treatment option only for the short-term outcome. Treatment with steroids has a significant rate of relapse also, probably because of permanent structural changes in the tendon caused by the steroid.[6]
In a systematic review, Assendelft et al. to assess the effectiveness of corticosteroid injections for lateral epicondylitis found that steroid injection appears to be safe and seem to be effective in short-term only and also realized that the issues of optimal timing, dosage, injection technique, and injection volume remain unanswered.[10]
Various types of surgical procedures are also available for patients with chronic lateral epicondylitis. Veerhar et al. noted an improvement in 60%–70% of the patients after surgical treatment (lateral release of the common extensor origin).[3,13] Patients however are seldom interested in operative procedures for this and seek an alternative.
PRP is an autologous blood-derived product which has been used in humans for its healing properties attributed to the increased concentrations of autologous growth factors and secretory proteins that may enhance the healing process on a cellular level. PRP contains a 3–5-fold increase in growth factors concentration and is associated with enhancement of healing process.[11]
PRP has been demonstrated as a potent agent for tissue healing in chronic wounds, tendinitis, and even bone. A possible explanation for the long-lasting effect of PRP in chronic tendinopathy is that it promotes revascularization and enhances healing at the microscopic level.[14,15,16]
Edwards and Calandrucio injected whole blood into patients with lateral epicondylitis and saw a success rate of 79%; however, multiple injections were necessary in 32% of patients. They attributed their result to the fact that autologous blood provides necessary cellular and humoral mediators to induce healing cascade.[5]
Our results are coherent with the results of the study conducted by Mishra and Paveloko. They reported a significant improvement of symptoms after 8 weeks in 60% of the patients treated with buffered PRP versus 16% of the patients treated with a local anesthetic. Similar results were observed by Hechtman et al. in their nonrandomized trial where they treated 31 patients with failed previous conservative treatment. They injected PRP in all the elbows and 90% of patients and elbows met the criterion of successful treatment: A 25% reduction in worst pain score for at least 1 follow-up visit with no further intervention at 12 months.[17,18]
This randomized study was designed to evaluate the outcome of autologous PRP in patients with elbow epicondylitis. Its application proved to be both safe and easy. Corticosteroid group was better only in the beginning and then declined, whereas the PRP group improved progressively and sustained. Our study offered encouraging results of an alternative treatment that addresses the pathophysiology of elbow epicondylitis that has failed traditional nonsurgical modalities.
Conclusion
This report demonstrates that one single injection of autologous PRP improves pain and function more than steroid in cases of elbow epicondylitis, and these improvements were sustained over a long period of time with no complications.
Limitations of this study are a comparatively small study group and second, the patients were followed only for a period of 6 months. Further studies are required with a greater number of patients in each group with even longer periods of follow-up. Nonetheless, this novel method can be considered as a primary method to treat chronic tendinopathies or for patients who have failed traditional nonsurgical modalities before thinking of any surgical intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: A population study. Am J Epidemiol. 2006;164:1065–74. doi: 10.1093/aje/kwj325. [DOI] [PubMed] [Google Scholar]
- 2.Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61:832–9. [PubMed] [Google Scholar]
- 3.Geoffroy P, Yaffe MJ, Rohan I. Diagnosing and treating lateral epicondylitis. Can Fam Physician. 1994;40:73–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Coonrad RW, Hooper WR. Tennis elbow: Its course, natural history, conservative and surgical management. J Bone Joint Surg Am. 1973;55:1177–82. [PubMed] [Google Scholar]
- 5.Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Bone Joint Surg. 2003;28:272–8. doi: 10.1053/jhsu.2003.50041. [DOI] [PubMed] [Google Scholar]
- 6.Smidt N, van der Windt DA, Assendelft WJ, Devillé WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: A randomised controlled trial. Lancet. 2002;359:657–62. doi: 10.1016/S0140-6736(02)07811-X. [DOI] [PubMed] [Google Scholar]
- 7.Haake M, König IR, Decker T, Riedel C, Buch M, Müller HH. Extracorporeal Shock Wave Therapy Clinical Trial Group. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: A randomized multicenter trial. J Bone Joint Surg Am. 2002;84:1982–91. doi: 10.2106/00004623-200211000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Keizer SB, Rutten HP, Pilot P, Morre HH, Van OJ, Verburg AD. Botulinum toxin injection versus surgical treatment for tennis elbow: A randomized pilot study. Clin Orthop. 2002;401:125–31. doi: 10.1097/00003086-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Campbell WC. Shoulder and elbow injuries. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby, Elsevier; 2008. pp. 2640–5. [Google Scholar]
- 10.Assendelft WJ, Hay EM, Adshead R, Bouter LM. Corticosteroid injections for lateral epicondylitis: A systematic overview. Br J Gen Pract. 1996;46:209–16. [PMC free article] [PubMed] [Google Scholar]
- 11.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: From basic science to clinical applications. Am J Sports Med. 2009;37:2259–72. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 12.Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: Platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38:255–62. doi: 10.1177/0363546509355445. [DOI] [PubMed] [Google Scholar]
- 13.Verhaar J, Walenkamp G, Kester A, Van MH, Van der LT. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg. 1993;75:1034–43. doi: 10.2106/00004623-199307000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Gurgen M. Treatment of chronic wounds with autologous platelet rich plasma. Eur Wound Manag Assoc J. 2008;8:5–10. [Google Scholar]
- 15.Kon E, Filardo G, Delcogliano M, Presti ML, Russo A, Bondi A, et al. Platelet-rich plasma: New clinical application: A pilot study for treatment of jumper's knee. Injury. 2009;40:598–603. doi: 10.1016/j.injury.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 16.Kamoda H, Ohtori S, Ishikawa T, Miyagi M, Arai G, Suzuki M, et al. The effect of platelet-rich plasma on posterolateral lumbar fusion in a rat model. J Bone Joint Surg Am. 2013;95:1109–16. doi: 10.2106/JBJS.L.00320. [DOI] [PubMed] [Google Scholar]
- 17.Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34:1774–8. doi: 10.1177/0363546506288850. [DOI] [PubMed] [Google Scholar]
- 18.Hechtman KS, Uribe JW, Botto-vanDemden A, Kiebzak GM. Platelet-rich plasma injection reduces pain in patients with recalcitrant epicondylitis. Orthopedics. 2011;34:92. doi: 10.3928/01477447-20101221-05. [DOI] [PubMed] [Google Scholar]


