Abstract
The treatment of advanced nonsmall cell lung cancer (NSCLC) with PD-1/PD-L1 immune checkpoint inhibitors has improved clinical outcome for a proportion of patients. The current challenge is to find better biomarkers than PD-L1 immunohistochemistry (IHC) that will identify patients likely to benefit from this therapy. In this exploratory study we assessed the differences in T-cell subsets and PD-1 expression levels on T-cells in tumour-draining lymph nodes (TDLNs) and peripheral blood mononuclear cells (PBMCs).
To evaluate this, flow cytometric analyses were performed on endobronchial ultrasound-guided (EBUS) fine-needle aspirates (FNA) from TDLNs of patients with NSCLC, and the results were compared to paired PBMC samples. For a select number of patients, we were also able to obtain cells from a non-TDLN (NTDLN) sample.
Our data show that the frequency of PD-1+ CD4+ and CD8+ T-cells, as well as the PD-1 expression level on activated regulatory T (aTreg) and CD4+ and CD8+ T-cells, are higher in TDLNs than in PBMCs and, in a small sub-analysis, NTDLNs.
These elevated PD-1 expression levels in TDLNs may reflect tumour-specific T-cell priming and conditioning, and may serve as a predictive or early-response biomarker during PD-1 checkpoint blockade.
Short abstract
PD-1 in NSCLC tumour-draining lymph nodes as a potential biomarker http://ow.ly/QedU30bqJ6d
Introduction
Nonsmall cell lung cancer (NSCLC) is the leading cancer-related cause of death worldwide [1]. Although small improvements have been made in the treatment of lung cancer over past decades, success remains limited for the majority of lung cancer patients. Anti-PD-(L)1 checkpoint inhibition offers a new opportunity for patients with NSCLC and is currently the preferred second-line treatment [2–5]. Moreover, a recent phase III clinical trial showed that in patients with ≥50% PD-L1 tumour membrane staining by immunohistochemistry (IHC), pembrolizumab was superior to first-line platinum-based doublet chemotherapy [6]. However, in both first- and second-line studies, the majority of patients (∼55–60% and ∼80%, respectively) did not respond to this form of immunotherapy. Unfortunately, PD-L1 IHC fails to predict for treatment benefit in nivolumab-treated squamous NSCLC patients [3, 7, 8], as up to 10% of patients with completely negative PD-L1 tumour staining still respond [2, 4, 5]. Clearly, more accurate biomarkers are needed [9].
After the primary tumour microenvironment, tumour-draining lymph nodes (TDLNs) are the first site where tumour-induced immune suppression, either through soluble factors or metastatic spread, interferes with the mounting of an efficient antitumour immune response. In particular, because priming of tumour antigen-specific CD4+ and CD8+ effector T-cells occurs at this location, this is an important site at which to study immune status. The immune cell composition in TDLNs may have predictive value for immune-based interventions. In patients with NSCLC, endobronchial ultrasound-guided (EBUS) fine-needle aspirates (FNAs) of lymph nodes are used for diagnostic purposes. In addition to regular diagnostics through cytology, cells derived during this procedure can be used for (immune)phenotyping by flow cytometry [10]. Previous research in melanoma patients has shown a difference in immune status between sentinel lymph nodes and nonsentinel lymph nodes [11, 12]. At present, little is known about the frequency of PD-1+ T-cells in the TDLNs of lung cancer patients. Besides offering a target for PD-1 blockade, recent publications have suggested PD-L1+ CD8+ T-cells to represent a tumour-specific population [13, 14]. The aim of this study was to evaluate whether it is feasible to profile the T-cell compartment in terms of frequencies and the expression of PD-1 on Treg and effector CD4+ and CD8+ T-cells in EBUS-guided FNA samples derived from TDLNs. The results were compared to the frequencies and expression levels in PBMCs and, when available, non-TDLN (NTDLN) samples to identify whether TDLNs form a unique immune compartment and could provide a novel tumour-related biomarker.
Materials and methods
Patient cohort and collection of blood and EBUS aspirates
Patients attending the outpatient clinic with (suspected) NSCLC and enlarged/suspected hilar and/or mediastinal lymph node (LN) involvement on either computed tomography (CT) or positron emission tomography (PET)-CT were eligible for this study when there was an indication for EBUS-FNA to either stage the hilum and mediastinum according to international staging guidelines or when tissue was required for molecular analysis. At least one of the LNs had to have a short axis diameter exceeding 10 mm. As this was an exploratory study to test the technical feasibility of performing immune phenotyping on EBUS-FNA samples from TDLNs, a limited number of 11 patients were enrolled between March 2015 and January 2016 in the VU University Medical Center (VUmc) Amsterdam, The Netherlands. This study was approved by the institutional review board and written informed consent was obtained prior to study enrolment, according to the Declaration of Helsinki.
Prior to the EBUS procedure, a 50 mL blood sample was drawn into heparinised tubes to compare LN and blood composition. EBUS-FNA procedures were performed by three experienced pulmonary physicians using an endobronchial ultrasound bronchoscope (Fujifilm Europe GmbH, Dusseldorf, Germany) and a 22-gauge aspiration needle. The procedure was performed with conscious sedation using midazolam with or without alfentanil. LNs were considered to be tumour draining when they were 18F-fluorodeoxyglucose (18F-FDG)-avid on PET-CT or enlarged on CT and ipsilaterally located. NTDLNs were 18F-FDG-negative on PET-CT and were sampled if size allowed. Six aspirates per lymph node, consisting of 15 passes (back and forward movement of the needle), were obtained to maximise cell yield. Whenever possible, IHCs were performed to confirm the diagnosis, and the samples were evaluated by an independent pathologist. LNs qualified as tumour-positive when malignant cells were observed.
Isolation of PBMCs and cells from EBUS aspirates
Peripheral blood was diluted 1:2 with PBS, and PBMCs were separated by Ficoll gradient separation (Lymphoprep; Nycomed AS, Zurich, Switzerland) by pipetting 25 mL of PBS-diluted peripheral blood on top of 15 mL Lymphoprep, followed by centrifugation for 15 min at 1000g without acceleration or brake. PBMCs were harvested and erythrocytes were lysed. A total of 0.5 million PBMCs were used for T-cell phenotyping by flow cytometry. Single-cell suspensions were derived from EBUS-FNA samples from TDLNs and NTDLNs, as described previously [15, 16], with the addition that all samples were treated with shock buffer after digestion to lyse erythrocytes. Depending on yield, between 2350 and 250 000 cells were used for T-cell phenotyping by flow cytometry.
Phenotypic analysis by flow cytometry
PBMC, TDLN and NTDLN single-cell suspensions were washed in FACS buffer (PBS+0.1% bovine serum albumin (BSA)+0.02% NaN3). Cells were resuspended in 50 μL of FACS buffer and stained in a total volume of 75 μL for 30 min at 4 °C for surface expression using monoclonal antibodies directed against CD3 (PerCP-Cy5.5), CD8 (V500), CD25 (APC), CD127 (BV421), CD45RA (APC-H7), PD-1 (PE-Cy7) (BD Biosciences, San Jose, CA, USA) and CD4 (AF700) (Biolegend, San Diego, CA, USA) pre-diluted in Brilliant-violet staining buffer (BD Biosciences). Cells were washed with cold PBS and fixated and permeabilised using the eBioscience FoxP3 staining kit according to the manufacturer's instructions. Antibodies against FoxP3 (PE) (eBioscience, San Diego, CA, USA) and Ki-67 (FITC) (BD Biosciences) were used for intracellular staining and incubated for 30 min at 4 °C. Stained cells were analysed on a BD LSR Fortessa X-20 flow cytometer, and data were analysed using Kaluza analysis software (Beckman Coulter, Brea, CA, USA). Mean fluorescence intensity values calculated by Kaluza were multiplied by ten to be equivalent to the values measured with the Diva software on the LSR Fortessa X-20.
Statistical analysis
Data were analysed using Prism 6 software. Paired t-tests were performed to evaluate differences between matched PBMC and TDLN samples. Unpaired ANOVA tests were performed using the Kruskal–Wallis test with multiple comparisons analyses to determine statistically significant differences in subset and marker expression between PBMCs, TDLNs and NTDLNs. Correlation analyses were performed by calculating the Pearson r coefficient. Differences were deemed statistically significant when p<0.05.
Results
Patient samples
Eleven patients were included in this study. Both PBMC and TDLN material were obtained from nine patients. In two patients it was technically not feasible to sample the TDLNs with EBUS and these patients were therefore excluded from the analyses. In six patients, the contralateral mediastinum and hilum did not contain lymph nodes that were large enough to obtain NTDLN samples. Hence, matched PBMC, TDLN and NTDLN specimens were available from three patients. Table 1 provides an overview of the patient characteristics as well as the location, cell yields and cytology results of the TDLNs and NTDLNs. Analyses including NTDLN samples are only presented for the three patients for whom matched PBMC and TDLN samples were available.
TABLE 1.
Patient characteristics
| Patient | Sex | Age years | Stage | Primary tumour | Mutation | Treatment pre-EBUS | Treatment post-EBUS | TDLN | NTDLN | OS | ||||||
| Location | LN size mm | Yield ×106 | Tumour presence | Location | LN size mm | Yield ×106 | Tumour presence | |||||||||
| 1 | F | 49 | IIIA | SCC | NT | None | Chemoradiation (66 Gy) | N4R | 8.3 | 0.01 | − | N7 | 20.2 | 0.002 | – | 23 months# |
| 2 | F | 55 | IV | AC | EGFR | Cis-Pem, gefitinib, gefitinib+crizotinib, Carbo-Pem | Afatinib-cetuximab | N7 | 15.6 | 0.03 | + | 3 weeks | ||||
| 3 | F | 78 | IIIB | AC | KRAS | None | None (patient decision) | N4R | 17.1 | 4.3 | + | 11L | 8.9 | 0.03 | NT | 21 months# |
| 4 | F | 68 | IIA | AC | KRAS | None | Resection | N7 | 12.1 | 1.1 | – | 21 months# | ||||
| 5 | M | 27 | IV | AC | ALK | None | Multiple ALK-TKIs | N11L | 13.8 | 0.35 | + | N7 | 8.6 | 1.6 | – | 21 months# |
| 6 | M | 46 | IV | SCC | None | Chemoradiation (66 Gy) | Nivolumab | N2L | 9 | 0.4 | – | 5 months | ||||
| 7 | F | 66 | IV | AC | EGFR | Erlotinib | Osimertinib | N4R | 23.6 | 0.45 | + | 16 months# | ||||
| 8 | M | 60 | IV | AC | None | None | Carbo-Pem | N11R N7 |
10.7 15.3 |
1.3 1.3 |
+ + |
17 months# | ||||
| 9 | M | 67 | IV | AC | NT | Cis-Pem | Nivolumab | N4R | 14.6 | 1.3 | + | 8 weeks | ||||
| 10 | M | 74 | IV | AC | None | None | Cis-Pem | N7 | 27 | 0.4 | + | 11 months | ||||
| 11 | M | 62 | IV | AC | KRAS | None | Carbo-Pacl-Atezo | N7 | 22.6 | 0.16 | + | 13 months# | ||||
Patients 4 and 6 were excluded from the comparative analyses because no tumour-draining lymph node (TDLN) sample was available. Bold rows represent those patients who died of the disease within the monitoring period. EBUS: endobronchial ultrasound; NTLDN: non-tumour-draining lymph node; LN: lymph node; OS: overall survival time from EBUS–fine-needle aspiration (diagnosis) to March 2017; F: female; M: male; SCC: squamous cell carcinoma; AC: adenocarcinoma; NT: not tested; Cis: cisplatin; Pem: pemetrexed; Carbo: carboplatin; TKI: tyrosine kinase inhibitor; Pacl: paclitaxel; Atezo: atezolizumab. #: survival time is censored; patient was still alive at the time of follow-up.
T-cell frequencies and PD-1 expression
There were no significant differences in the frequencies of CD3+, CD4+ and CD8+ T-cells between the TDLN and PBMC compartments (supplementary table S1). CD4+ T-cells were subdivided into naïve CD4+ T-cells (naïve), activated CD4+ T-cells (actCD4+) and cytokine-secreting CD45RA−FoxP3lo nonsuppressive CD4+ T-cells (cytCD4+) based on CD45RA and Foxp3 expression (supplementary figure S1a), as previously described [17]. There were no differences in the frequencies of these cell populations between TDLNs and PBMC (supplementary table S1). For Treg analyses, activated Treg (aTreg) frequencies were determined based on Ki67, CD45RA and FoxP3 expression on CD25+ CD127− CD4+ T-cells [17, 18]. For the Treg analyses, we excluded samples where fewer than 3000 CD4+ T-cells could be counted to ensure acquisition of >50 aTreg events. This threshold was not met for 4 out of 9 TDLN samples and 2 out of 3 matched NTDLN samples (supplementary table S1). With the exception of one patient, there were no dramatic increases in aTreg frequencies in TDLNs compared to PBMC (figure 1a and supplementary table S1). Of note, patient 2, who rapidly progressed and died within a month of the EBUS procedure after having experienced a durable response to targeted treatment for epidermal growth factor receptor (EGFR)-positive NSCLC, had an extremely high frequency of 69% aTreg of CD4+ T-cells in TDLNs (supplementary figure S1b and supplementary table S1).
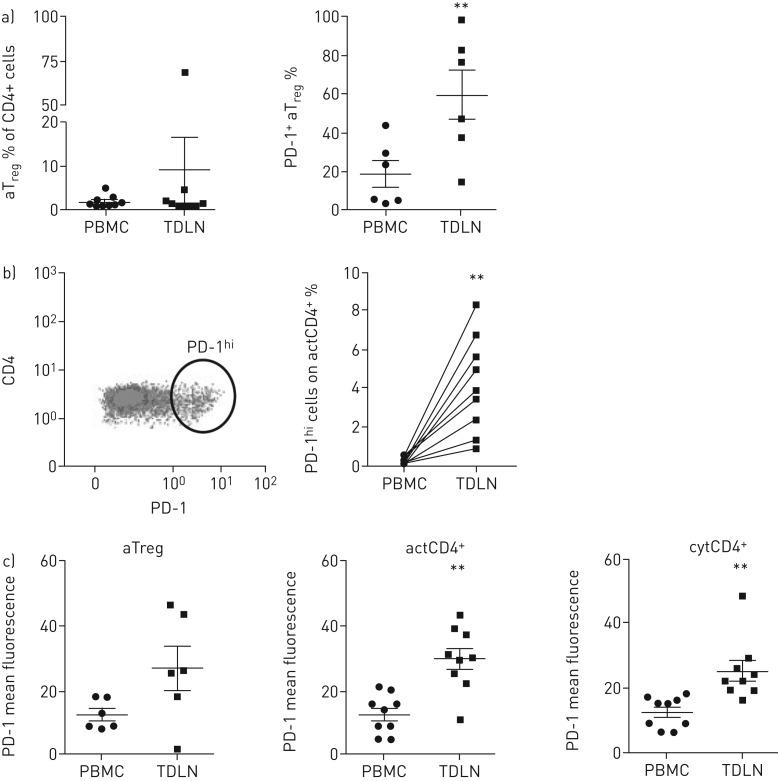
FIGURE 1.
PD-1 expression on activated regulatory T-cells (aTreg) and CD4+ T-cells. a) Frequencies of aTreg and PD-1+ aTreg in peripheral blood mononuclear cells (PBMCs) and tumour-draining lymph nodes (TDLNs) (p<0.01). b) Representative dot plot showing PD-1hi gating on activated (act)CD4+ T-cells in TDLNs, and frequencies of PD-1hi actCD4 T-cells among PBMCs and TDLNs (p<0.001). c) PD-1 mean fluorescence intensity levels on aTreg, actCD4+ and cytokine-secreting (cyt)CD4+ T-cells. Paired t-tests were performed to determine statistical significance between matched PBMCs and TDLNs: **: p<0.01.
Higher percentages of PD-1+ aTreg could be observed in TDLNs than in PBMCs (p<0.01) (figure 1a). Percentages of PD-1+ actCD4+ and cytCD4 T-cells were also significantly increased in TDLNs than in PBMCs (p<0.01; data not shown). In TDLNs, a population of PD-1hi actCD4+ T-cells could be discerned (figure 1b) that was absent in PBMCs. In all patients, this population was more frequent in TDLNs than in the matching PBMC sample (p<0.001). PD-1 expression levels (in mean fluorescence intensity) were elevated on aTreg (NS), actCD4+ (p<0.01) and cytCD4+ T-cells (p<0.01) in TDLNs when compared to PBMCs (figure 1c). No differences in the frequencies of PD-1+ cells or PD-1 levels were observed on naïve CD4+ T-cells between PBMCs and TDLNs (data not shown). Table 2 gives an overview of the percentages of PD-1 for the T-cell subsets analysed.
TABLE 2.
PD-1 on T-cell subsets
| Patient | PD-1+ aTreg | PD-1+ CD8+ | PD-1+ actCD4+ | PD-1hi actCD4+ | PD-1+ naïve CD4+ | PD-1+ cytCD4+ | ||||||||||||
| PBMC | TDLN | NTDLN | PBMC | TDLN | NTDLN | PBMC | TDLN | NTDLN | PBMC | TDLN | NTDLN | PBMC | TDLN | NTDLN | PBMC | TDLN | NTDLN | |
| 1 | 31 | – | – | 10 | 29 | 27 | 28 | 61 | 44 | 0.02 | 6.7 | 1.2 | 5 | 44 | 14 | 36 | 64 | 53 |
| 2 | 30 | 98 | 32 | 81 | 23 | 50 | 0.34 | 8.3 | 2 | 5 | 26 | 87 | ||||||
| 3 | 44 | 77 | – | 48 | 74 | 64 | 50 | 45 | – | 0.55 | 3.9 | – | 63 | 3 | – | 57 | 61 | – |
| 4 | 32 | 52 | 43 | 45 | 43 | 55 | 0.04 | 3.4 | 9 | 6 | 34 | 42 | ||||||
| 5 | 28 | – | 56 | 21 | 52 | 13 | 23 | 41 | 32 | 0.15 | 2.4 | 0.7 | 0.4 | 0.9 | 1 | 30 | 53 | 44 |
| 6 | 11 | 35 | 30 | 49 | 21 | 33 | 0.28 | 1.8 | 15 | 29 | 6 | 10 | ||||||
| 7 | 2 | – | 8 | 40 | 3 | 15 | 0.17 | 1.4 | 0.3 | 2 | 3 | 13 | ||||||
| 8 | 24 | 83/– | 31 | 85/87 | 23 | 55/62 | 0.06 | 4.9/11.7 | 4 | 13/4 | 22 | 69/82 | ||||||
| 9 | 3 | 15 | 19 | 43 | 9 | 23 | 0.08 | 1.0 | 4 | 3 | 4 | 11 | ||||||
| 10 | 5 | 48 | 10 | 37 | 8 | 22 | 0.35 | 3.4 | 0.8 | 6 | 4 | 17 | ||||||
| 11 | 6 | 38 | 7 | 26 | 14 | 26 | 0.15 | 5.6 | 4 | 3 | 11 | 28 | ||||||
Data are presented as percentages of PD-1+ cells gated for the different T-cell subsets per patient. Patients 4 and 6 were excluded from the comparative analyses because no tumour-draining lymph node (TDLN) sample was available. Specimens that were not available for research are left open. Bold rows represent those patients who died of the disease within the monitoring period. aTreg: activated regulatory T-cell; act: activated; cyt: cytokine-secreting; PBMC: peripheral blood mononuclear cell; NTDLN: non-tumour draining lymph node; −: could not be evaluated due to too low counts.
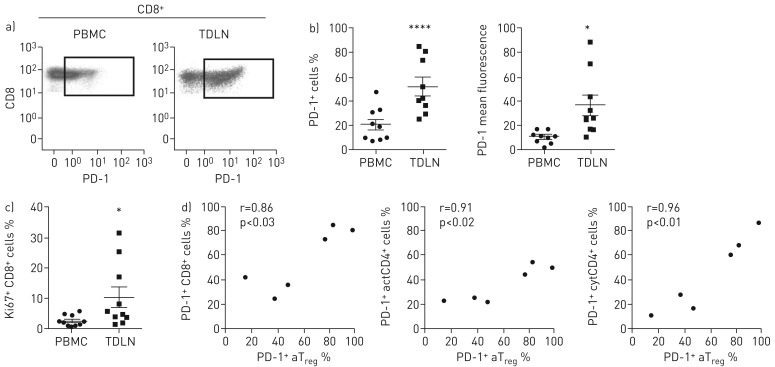
Although a separate PD-1hi population was not as apparent in the CD8 T-cell compartment as on the actCD4+ T-cells in TDLNs (figure 2a), there were clear differences in PD-1 expression on CD8+ T-cells between TDLNs and PBMCs and matching NTDLNs. CD8+ T-cells in TDLNs contained higher frequencies of PD-1+ cells than PBMCs (p<0.0001) (figure 2b). Also, PD-1 expression levels on CD8+ T-cells were higher in TDLNs than in PBMCs (p<0.02) (figure 2b). This was the case for each individual patient (data not shown). Studying the CD8+ T-cell compartment, we observed a significant difference in the frequency of proliferating CD8+ T-cells between the groups, based on Ki67 staining (p<0.05), with more proliferating CD8+ T-cells in TDLNs versus PBMCs (figure 2c). Within the TDLN samples, there was a positive correlation between the percentages of Ki67+ CD8+ T-cells and PD-1+ CD8+ T-cells (r=0.71, p<0.03) (data not shown), indicating active proliferation of a putatively tumour-reactive effector T-cell population in the TDLNs. Finally, in TDLNs, PD-1 expression on aTreg correlated with PD-1 expression on effector CD8+ and CD4+ T-cell populations (figure 2d). These correlations are suggestive of co-induction or co-activation of these immune subsets.
FIGURE 2.
PD-1 expression on CD8+ T-cells. a) Representative examples of PD-1 expression on CD8+ T-cells in peripheral blood mononuclear cells (PBMCs) and tumour-draining lymph nodes (TDLNs). b) Percentages of PD-1 (p<0.0001) and PD-1 mean fluorescence intensity levels on CD8+ T-cells present in PBMCs and TDLNs (p<0.05). c) Percentages of proliferating Ki67+ CD8+ T-cells in PBMCs and TDLNs (p<0.05). d) Pearson correlations between total percentages of PD-1+ cells on activated regulatory T-cells (aTreg) and CD8+ T-cells, activated (act)CD4+ T-cells and cytokine-secreting (cyt)CD4+ T-cells for the six TDLN samples in which we could evaluate aTreg frequencies.
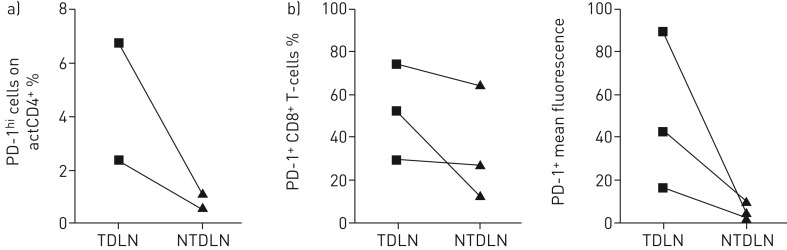
For three patients, matched TDLN and NTDLN specimens could be collected. Due to the small number, there were no statistically significant differences, but a trend towards lower frequencies and intensity levels of PD-1 expression was observed on both actCD4+ and CD8+ T-cells in the NTDLN versus its matched TDLN (figure 3).
FIGURE 3.
PD-1 expression on CD4+ and CD8+ T-cells in matched tumour-draining lymph nodes (TDLN) and non-tumour draining lymph node (NTDLN) samples. a) Percentages of PD-1hiactivated (act)CD4+ T-cells in matched TDLNs and NTDLNs (n=2). b) Percentages of PD-1+ and PD-1 mean fluorescence intensity levels on CD8+ T-cells in matched TDLNs and NTDLNs (n=3).
Discussion
The aim of this study was to investigate whether the frequencies of conventional (nonregulatory) and regulatory T-cell subsets and PD-1 expression on these cells differed between TDLNs, NTDLNs and PBMCs. A previous study by Bugalho et al. [10] showed the feasibility of using EBUS-FNA samples of lung lymph nodes for flow cytometric analysis of CD4+ and CD8+ T-cells. That study did not include Treg analyses. Due to the low yield of some FNA samples, aTreg analyses were challenging, though still feasible for the majority of the TDLNs (6 out of 9). We found aTreg frequencies to be comparable between TDLNs and PBMCs. Nevertheless, an interesting observation was made for patient 2: this patient had a remarkably high frequency of aTreg in the TDLNs (69%), something we never observed in any TDLN sample in previous lymph node samples ([19] and unpublished data). This patient progressed and died within a month of the EBUS-FNA procedure after having experienced a durable response on EGFR-directed therapy. This patient also displayed high frequencies of PD-1+ aTreg, CD8+, actCD4+ and cytCD4+ cells (table 2), suggesting that such high frequencies of aTreg in the TDLNs could be indicative of immune escape, rapid progression and poor prognosis, even in the face of an activated tumour-recognising effector T-cell population.
Especially in the CD8 compartment, but also on aTreg and activated- and cytokine-producing nonsuppressive CD4+ T-cells, we observed higher levels of PD-1 expression in TDLNs than in PBMCs. Although in the majority of patients the NTDLNs were too small to sample by EBUS-FNA, differences in mean PD-1 fluorescence intensity levels within the CD8 compartment almost reached statistical significance between matched PBMCs, TDLNs and NTDLNs (p=0.05). This suggests a higher frequency of tumour-antigen experienced effector T-cells within TDLNs [13]. We found TDLNs to contain a specific population of PD-1hi actCD4+ T-cells that was not present in PBMCs, and much lower in the matching NTDLNs (n=2). For PD-1 expression on CD4+ T-cells there is no data available at the moment showing that these CD4+ cells are tumour-antigen specific. Although the underlying cellular and molecular mechanisms as yet remain unknown, the observed significant correlation between PD-1 expressing CD4+, CD8+ T-cells and aTreg is suggestive of co-induction or co-activation in TDLNs.
Taken together, it seems feasible to analyse the T-cell repertoire and PD-1 expression in the majority of EBUS-FNA samples of TDLNs, and the TDLN immune compartment has unique characteristics that differ from circulating T-cells. It will be interesting to investigate whether PD-1 expression levels on T-cell subsets within TDLNs could serve as a predictive biomarker to identify NSCLC patients more likely to respond to anti-PD-(L)1 therapy. The recent findings that neo-antigen load (indicative of tumour immunogenicity) is related to response to immune checkpoint blockade in NSCLC [20] and that PD-1+ CD8+ T-cells represent tumour-reactive T-cells [13, 14] suggests that this may well be the case.
Also, changes in the compartment might be used as an early response biomarker to checkpoint inhibition. Increasing numbers or proliferation rates of PD-1 expressing effector cells in TDLNs could serve as an early sign of response to immunotherapy regimens like anti-CTLA-4 and anti-PD-(L)1. Due to the exploratory character of this study, with emphasis on technical feasibility the current cohort was not selected on histological or (pre)treatment parameters and therefore no conclusive relationship to clinical outcome could be ascertained.
In conclusion, compared to PBMCs, NSCLC TDLNs contain a higher percentage, as well as increased expression levels, of PD-1 on CD4+ and CD8+ T-cell subsets. These observations warrant further research on monitoring the T-cell compartment in TDLNs to determine whether PD-1 expression on T-cells in TDLNs could be used as a predictive or early response biomarker for a response to checkpoint inhibition regimens.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Figure S1. Gating. 00110-2016_figureS1 (149.3KB, pdf)
Table S1. Frequencies of T-cell subsets. 00110-2016_tableS1 (54.9KB, pdf)
Disclosures
R. van de Ven 00110-2016_van_de_Ven (1.2MB, pdf)
Acknowledgements
The authors would like to thank the patients for their participation in this study.
Footnotes
This article has supplementary material available from openres.ersjournals.com
Support statement: R. van de Ven was supported through a fellowship from the Dutch Cancer Society (KWF BUIT 2010-4643). Funding information for this article has been deposited with the Crossref Funder Registry.
Conflict of interest: Disclosures can be found alongside this article at openres.ersjournals.com
References
- 1.Youlden DR, Cramb SM, Baade PD. The International Epidemiology of Lung Cancer: geographical distribution and secular trends. J Thorac Oncol 2008; 3: 819–831. [DOI] [PubMed] [Google Scholar]
- 2.Borghaei H, Paz-Ares L, Horn L, et al. . Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 2015; 373: 1627–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brahmer J, Reckamp KL, Baas P, et al. . Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N Engl J Med 2015; 373: 123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herbst RS, Baas P, Kim D-W, et al. . Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016; 387: 1540–1550. [DOI] [PubMed] [Google Scholar]
- 5.Rittmeyer A, Barlesi F, Waterkamp D, et al. . Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017; 389: 255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reck M, Rodriguez-Adreu D, Robinson AG, et al. . Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 2016; 375: 1823–1833. [DOI] [PubMed] [Google Scholar]
- 7.Ang YL, Lim JS, Soo RA. Profile of nivolumab in the treatment of metastatic squamous non-small-cell lung cancer. Onco Targets Ther 2016; 9: 3187–3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chae YK, Pan A, Davis AA, et al. . Biomarkers for PD-1/PD-L1 blockade therapy in non-small-cell lung cancer: is PD-L1 expression a good marker for patient selection? Clin Lung Cancer 2016; 17: 350–361. [DOI] [PubMed] [Google Scholar]
- 9.Sacher AG, Gandhi L. Biomarkers for the clinical use of PD-1/PD-L1 inhibitors in non-small-cell lung cancer: a review. JAMA Oncol 2016; 2: 1217–1222. [DOI] [PubMed] [Google Scholar]
- 10.Bugalho A, Martins C, Dias SS, et al. . Cytokeratin 19, carcinoembryonic antigen, and epithelial cell adhesion molecule detect lung cancer lymph node metastasis in endobronchial ultrasound-guided transbronchial aspiration samples. Clin Lung Cancer 2013; 14: 704–712. [DOI] [PubMed] [Google Scholar]
- 11.Mohos A, Sebestyén T, Liszkay G, et al. . Immune cell profile of sentinel lymph nodes in patients with malignant melanoma – FOXP3. J Transl Med 2013; 11: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cochran AJ, Huang R-R, Lee J, et al. . Tumour-induced immune modulation of sentinel lymph nodes. Nat Rev Immunol 2006; 6: 659–670. [DOI] [PubMed] [Google Scholar]
- 13.Gros A, Robbins PF, Yao X, et al. . PD-1 identifies the patient-specific CD8+ tumor-reactive repertoire infiltrating human tumors. J Clin Invest 2014; 124: 2246–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gros A, Parkhurst MR, Tran E, et al. . Prospective identification of neoantigen-specific lymphocytes in the peripheral blood of melanoma patients. Nat Med 2016; 22: 433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van de Ven R, van den Hout MFCM, Lindenberg JJ, et al. . Characterization of four conventional dendritic cell subsets in human skin-draining lymph nodes in relation to T-cell activation. Blood 2011; 118: 2502–2510. [DOI] [PubMed] [Google Scholar]
- 16.Vuylsteke RJCLM, van Leeuwen PAM, Meijer S, et al. . Sampling tumor-draining lymph nodes for phenotypic and functional analysis of dendritic cells and T cells. Am J Pathol 2002; 161: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyara M, Yoshioka Y, Kitoh A, et al. . Functional delineation and differentiation dynamics of human CD4+ T cells expressing the FoxP3 transcription factor. Immunity 2009; 30: 899–911. [DOI] [PubMed] [Google Scholar]
- 18.Santegoets SJAM, Dijkgraaf EM, Battaglia A, et al. . Monitoring regulatory T cells in clinical samples: consensus on an essential marker set and gating strategy for regulatory T cell analysis by flow cytometry. Cancer Immunol Immunother 2015; 64: 1271–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Pul KM, Vuylsteke RJCLM, Bril H, et al. . Feasibility of flowcytometric quantitation of immune effector cell subsets in the sentinel lymph node of the breast after cryopreservation. J Immunol Methods 2012; 375: 189–195. [DOI] [PubMed] [Google Scholar]
- 20.Rizvi NA, Hellmann MD, Snyder A, et al. . Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015; 348: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Figure S1. Gating. 00110-2016_figureS1 (149.3KB, pdf)
Table S1. Frequencies of T-cell subsets. 00110-2016_tableS1 (54.9KB, pdf)
R. van de Ven 00110-2016_van_de_Ven (1.2MB, pdf)