Abstract
Limited national data document the prevalence of incarceration among transgender women, experiences of victimization while incarcerated, and associations of transgender status with health. Data were from the National Transgender Discrimination Survey (NTDS), a large convenience sample of transgender adults in the U.S., collected between September 2008 and March 2009. Respondents who indicated a transfeminine gender identity were included in the current study (n = 3,878). Multivariable logistic regression was used to model ever being incarcerated and experiencing victimization while incarcerated as a function of race/ethnicity and health-related indicators. Overall, 19.3% reported having ever been incarcerated. Black and Native American/Alaskan Native transgender women were more likely to report a history of incarceration than White (non-Hispanic) respondents, and those with a history of incarceration were more likely to report negative health-related indicators, including self-reporting as HIV-positive. Among previously incarcerated respondents, 47.0% reported victimization while incarcerated. Black, Latina, and mixed race transgender women were more likely to report experiences of victimization while incarcerated. Transgender women reported disproportionately high rates of incarceration and victimization while incarcerated, as well as associated negative health-related indicators. Interventions and policy changes are needed to support transgender women while incarcerated and upon release.
Keywords: transgender, incarceration, health disparities
INTRODUCTION
Transgender women—individuals assigned a male sex at birth who identify their current gender identity and/or expression as female, transgender female, male-to-female (MTF), or another gender identity on the transfeminine spectrum—represent an understudied population in national U.S. health research. Evidence is growing that a high burden of adverse health-related outcomes face many transgender women, including high prevalence of unemployment and poverty, violence and victimization, institutional discrimination in a diverse array of settings, cigarette smoking, mental health distress and substance use, HIV, sex work, and barriers to accessing gender affirmation technologies (Bradford et al., 2013; Brennan et al., 2012; Clements-Nolle et al., 2001; Conron et al., 2012; Garofalo et al., 2006; Herbst et al., 2008; Kenagy, 2005; Lombardi et al., 2002; Nuttbrock et al., 2010; Operario et al., 2011). However, few studies of transgender health have offered the opportunity to examine health disparities within transfeminine communities, due to small sample sizes and often limited research scope and design. In particular, a dearth of national data exist about the prevalence of incarceration among transgender women, experiences of victimization or maltreatment while in jail or prison, and the associations of these experiences with health-related indicators.
Transgender inmates are considered a “special population” by correctional systems in the U.S., yet little empirical research has been devoted to understanding this subpopulation. Due to their expressed gender identity, young transgender women are often rejected by their families and communities and forced to strike out on their own (Garofalo et al., 2006). Social marginalization can lead directly to disproportionate homelessness and unemployment, which may then lead to illegal means of securing income and housing (e.g., Galea & Vlahov, 2002; Link & Phelan, 1996; Reisner et al., 2009), such as sex work, drug dealing, and petty theft or credit card fraud. Importantly, socially marginalized communities also bear a disproportionate burden of negative health outcomes on a population-level in the U.S. Incarceration rates have been disproportionately high among transgender women, with estimates of incarceration history ranging from 37% to 65% in convenience sample studies (Brennan et al., 2012; Clements-Nolle et al., 2001; Garofalo et al., 2006; Reback et al., 2001). Further, incarceration has emerged as a risk factor for poor health. In one study of young transgender women in Chicago and Los Angeles, history of incarceration was significantly associated with an index of four health and psychosocial factors (low self-esteem, polysubstance use, victimization, and intimate partner violence) (Brennan et al., 2012).
Gender affirmation, the process by which individuals are affirmed in their gender identity through social interactions, represents a key social determinant of health for transgender women (Sevelius, 2013), including HIV risk behaviors. Jails/prisons facilities are “hypergendered” environments. Scholarship has focused on “hypermasculinity” among men in prisons (Jewkes, 2005; Karp, 2010; Sabo, Kupers, & London, 2001), including enactment of “hegemonic” masculine identities (Connell & Messerschmidt, 2005; Mosher, 1991) through violence, aggression, and dominance within the restricted setting of jail/prison setting (Mosher & Serkin, 1984). Hypermasculinity has been associated with sexual and physical aggression toward women (Mosher & Anderson, 1986; Parrott & Zeichner, 2003).
Correctional systems are among the most highly gendered institutions in our society, and most (if not all) policies dictate that transgender inmates should be housed according to genitalia (Tarzwell, 2006). Transgender women, who already face multiple intersecting layers of discrimination, such as racism, classism, and sexism, often do not have access to gender affirming surgical procedures, and not all transgender women desire such surgeries. Thus, the majority of transgender women who interact with corrections systems (i.e., poor transgender women of color) are housed in men’s prisons. Transgender women housed in men’s prisons are particularly vulnerable to harassment, violence, and maltreatment from other inmates as well as staff (Jenness, 2009). To protect transgender inmates, some prisons place transgender women in special housing situations, such as administrative segregation, or “Ad-Seg” (Tarzwell, 2006). While Ad-Seg may temporarily provide protection from other prisoners, it often heightens transgender women’s vulnerability to victimization by prison staff, and is a harsher and more restrictive environment akin to solitary confinement. Often referred to as “the jail” inside the prison, inmates in Ad-Seg lose privileges they have while housed with the general population. Because transgender prisoners are often sent to Ad-Seg for their own protection, they can stay there indefinitely, while inmates who are sent there for disciplinary reasons have defined sentences.
In the largest study of its kind to date, Jenness and colleagues (2009) conducted 315 interviews of transgender female inmates housed in men’s prisons throughout California (Jenness, 2009). They found that the prevalence of sexual assault by other inmates was 58.5% over the entire incarceration history, 23.8% in the current housing unit. The prevalence of sexual assault by staff was 13.6% over the entire incarceration history and 0.6% in current housing unit. Assault by a law enforcement officer outside of prison was 15.2%. In an earlier report on violence in the California correctional system among the general population of inmates found that the prevalence of sexual assault was 4.4% in a random sample of male inmates, but was 59% among the transgender sample (Jenness et al., 2007). Incarceration itself may directly increase transgender women’s HIV risk, due to sexual relationships, survival sex, sex work, and experiences of sexual violence during incarceration. Furthermore, reports of HIV rates among transgender women, especially those of color, are among the highest of any risk group (Baral et al., 2013).
In addition, transgender women may be especially susceptible to having their medical treatment withheld while incarcerated. The U.S. Bureau of Prisons policy is to provide hormones at the level that was maintained prior to incarceration (U.S. Dept. of Justice, 2005); however, in practice wide variability has been observed in access to cross-sex hormones (Brown & McDuffie, 2009). While even non-transgender women with history of incarceration report inconsistent access to health care (Sered & Norton-Hawk, 2013), the special needs of transgender women require additional attention to ensure that their medical needs are met. Transgender women may experience discontinuity of care due to prison transfers, lack of providers willing to continue hormone treatment, and lack of a prescription to document previous hormone use (Tarzwell, 2006). A discontinuity in their medical treatment may leave them vulnerable to the multiple negative effects of discontinuing hormone use abruptly. In one legal case, a U.S. District Court found that prison officials violated a transgender woman’s right to be free of cruel and unusual punishment by withholding her hormones, which constituted necessary medical care (South v. Gomez, 2000).
The goal of the current study was to examine among transgender women the sociodemographic and health correlates of ever being in jail or prison in the National Transgender Discrimination Survey (NTDS), the largest convenience sample of transgender adults conducted to date, with data collected between September 2008 and March 2009 in the U.S. We also explored experiences of victimization and mistreatment while in jail or prison, including victimization perpetrated by inmates and by officers/staff and denial of healthcare while incarcerated. Finally, we examined whether experiences of victimization in jail/prison and denial of healthcare were each associated with health disparities among transgender women with a history of incarceration. These data highlighted the unique intersection of race, class, and gender for transgender women to produce higher risk of incarceration and negative health consequences.
METHOD
Data Source
In 2008, the National Center for Transgender Equality (NCTE) and the National Gay and Lesbian Task Force (NGLTF) partnered to conduct a cross-sectional survey of transgender discrimination (Grant et al., 2011). The National Transgender Discrimination Survey (NTDS) used purposive sampling techniques (Shadish, Cook, & Campbell, 2002) and convenience sampling methods recommended by the Centers for Disease Control and Prevention to identify hard-to-reach populations, including venue-based sampling and snowball sampling (Magnani et al., 2005; Semaan, Lauby, & Liebman, 2002). Eligibility criteria for NTDS participation were: (1) being age 18 years or older; (2) voluntarily agreeing to complete the survey; and (3) identifying as transgender. “Transgender” was defined broadly to include those who transition from one gender to another and those who may not choose to transition fully socially, medically, or legally, including cross-dressers, people who consider themselves to be genderqueer, androgynous, and those whose gender nonconformity is a part of their identity. Inclusive language regarding gender nonconforming was used to ensure broad participation in the survey.
Two data collection methods were used to recruit the sample: (1) an online survey link was distributed via electronic and digital social networks, such as online listservs and email lists; (2) paper surveys were selectively distributed to community-based healthcare and social service organizations that agreed to do in-person, face-to-face outreach to transgender people who were unlikely to get electronic information about the survey or to be able to complete the survey online.
The quantitative survey instrument contained questions about discrimination in a variety of settings, including in jail or prison, and health indicators. The survey took approximately 20 minutes to complete, and no incentives were offered for participating. The anonymous survey was fielded for six months from September 2008 through March 2009. The final sample included 6,456 respondents from all 50 states. Eligibility and participation rates were not collected or available. Institutional Review Board (IRB) approval was obtained from Pennsylvania State University for NTDS. Participants consented by checking a box on the first page of the survey that they understood their participation was completely voluntary and that all information they provided would be anonymous. The current secondary analysis of NTDS data was reviewed by the IRB at Harvard School of Public Health.
Data Analytic Sample
Gender was operationalized using a two-step method to cross-classify natal sex/gender identity status (step1: assigned sex at birth, step 2: gender identity) (Sausa et al., 2009; Tate, Ledbetter, & Youssef, 2013). Those who checked “male” assigned sex at birth were then cross-classified with current primary gender identity (1 = male/man, 2 = female/woman, 3 = part-time one gender, part-time another, 4 = gender not listed here). A total of 3,878 respondents who identified on the transfeminine/MTF spectrum were included in this analysis. Among these respondents, 58.90% endorsed a binary gender identity (described their gender as female/woman); 41.10% indicated a non-binary gender identification (reported living part-time as one gender, part-time as another gender, or identifying as a “gender not listed here”).
Measures
All data collected were from questions that were specifically developed for this survey, and psychometric properties were not evaluated.
Incarceration History
Participants were asked whether they had ever been in jail/prison in their lifetime (yes/no) (outcome 1). Participants who reported having been in jail/prison were also asked about experiences of victimization and mistreatment. This included victimization from other inmates (harassment, physical assault/attack, and sexual assault/attack) and from jail/prison officers/staff (harassment, physical assault/attack, sexual assault/attack, denied hormones, denied regular medical care). Two composite variables were created: any victimization experienced while in jail/prison (yes/no) (outcome 2) and any denial of medical care (yes/no) (outcome 3).
Sociodemographics
Age
Participants were asked to provide their current age in years. We categorized age into three groups (18–24 years, 25–44 years, 45 years and older) to be consistent with U.S. Census categories often used to age-adjust prevalence in health research. The referent for age comparisons was age 25–44 years. Here and for all variables in analysis, the largest category was selected as the referent group.
Race/Ethnicity
Participants were asked to indicate their race/ethnicity (all that apply). Race/Ethnicity was operationalized as: 1 = White (non-Hispanic), 2 = Black/African American, 3 = American Indian or Alaska Native, 4 = Hispanic/Latino, 5 = Other Race/Ethnicity, 6 = Multiracial or Mixed Race. A binary indicator for people of color (any racial/ethnic minority yes/no) was also specified. The referent for all comparisons was White (non-Hispanic).
Annual income and educational attainment
Respondents were asked their annual household income (current gross annual household income before taxes). Anticipating a nonlinear association of income and health (Kawachi, 2000), income was initially coded into tertiles. The top two tertiles were subsequently combined to compare respondents with lower income (<$19,999) to those with higher income ($20,000–$99,999). The highest income reported was $99,999. Also queried was the highest degree or level of school respondents had completed. Education was categorized into high school only or below versus some college or more.
Health insurance
Participants were asked their type of health insurance. Participants were categorized as 1 = insured private, 2 = insured public, and 3 = uninsured. The referent for all comparisons was private health insurance.
Medical gender affirmation
Participants were asked about whether they had ever taking hormones for transgender-related purposes (yes/no) and whether they had ever had surgery for transgender related purposes (yes/no).
Survey Variables
Paper data collection methods were not implemented in all geographic regions sampled; therefore, by design, the probability of paper versus online response was zero for certain geographic areas. Geographic region was therefore considered a potential confounder and was parameterized to ensure a distribution of paper and online probabilities that would allow exertion of some statistical control for geographic location. Four geographic regions were specified: region 1 (29.9% New England/Mid Atlantic), region 2 (18.1% Southern), region 3 (37.4% Midwest/West), and region 4 (14.6% California). The referent for geographic comparisons was Midwest/West. Data collection method (online versus paper) was also specified as a covariate.
Health-Related Indicators
Seven health-related variables were considered: (1) current daily cigarette smoker (current daily smoking/current occasional smoking or smoking not at all); (2) substance use to cope with mistreatment (ever yes/no); (3) history of suicidality (lifetime history of one or more suicide attempts yes/no); (4) self-reported HIV serostatus (HIV positive/HIV negative or unknown); (5) sex work involvement (ever engaged in transactional sex yes/no); (6) physical assault/attack (ever physically assaulted/attacked yes/no); and (7) sexual assault/attack (ever sexually assaulted/attacked yes/no).
Statistical Analyses
SAS® version 9.3 statistical software was used to analyze data. Univariable, descriptive statistics were obtained for all variables of interest. Distributions of individual items were assessed, including missingness. Because in-person recruited respondents who completed the survey via paper were more likely to have missing item-level data than online respondents, violating the missing completely at random assumption required for valid statistical inferences using list-wise deletion (Allison, 2001), data were multiply imputed. A fully conditional specification (FCS) (Van Buuren, 2007; Van Buuren et al., 2006) imputation method was used (5 burns), implemented in PROC MI with the FCS statement. FCS is a semi-parametric and flexible imputation procedure that specifies the multivariate model by a series of conditional models, one for each incomplete variable. All subsequent statistical analyses were conducted using the imputed dataset.
First, we compared transgender women (N = 3,878) with and without a self-reported history of ever having been in jail/prison. Two multivariable logistic regression models were estimated with ever incarceration in jail/prison (yes/no) as an outcome (outcome 1). The first model included sociodemographics only (age, binary gender, race/ethnicity, education, income, health insurance, medical gender affirmation, geographic region, and data collection method). The second model added all health-related indicators to the first model (daily cigarette smoking, substance use to cope, suicide attempt, HIV, sex work, any physically assault/attack, and any sexual assault/attack). Risk ratios (RRs) were estimated (Spiegelman & Hertzmark, 2005) rather than odds ratios because the prevalence of the outcome was >10%. Appropriate goodness-of-fit tests and diagnostic statistics were used to evaluate fitted models for multivariable logistic regression (Hosmer & Lemeshow, 1980; Hosmer et al., 1997). No interactions of variables were examined.
Second, analyses were restricted to transgender women who had been in jail/prison (N = 748). We descriptively explored self-reported experiences of victimization and denial of medical care while in jail/prison. We then compared transgender women who had been in jail/prison by experiences of victimization and by denial of medical care. Two multivariable logistic regression models were estimated, first for any victimization while in jail/prison ever (yes/no) (outcome 2) and then for any denial of medical care (yes/no) (outcome 3). The model included sociodemographics (age, binary gender, race/ethnicity, education, income, health insurance, medical gender affirmation, geographic region, and data collection method) and health-related indicators (daily cigarette smoking, substance use to cope, suicide attempt, HIV, and sex work). Any physically assault/attack and any sexual assault/attack were not included as covariates due to collinearly with the outcome.
RESULTS
Sociodemographic and Health Correlates of Ever Having Been in Jail/Prison
Overall, 19.3% of transgender women respondents reported having ever been in jail/prison in their lifetime. In a multivariable model with sociodemographics (Table 1, Model 1), respondents with a history of incarceration were somewhat more likely to be binary gender-identified and significantly more likely to be people of color, have low income, have lower educational attainment, be publicly insured or uninsured compared to privately insured, and to have been sampled in-person compared to online. No significant differences in geographic region or medical gender affirmation between transgender women with and without history of incarceration.
TABLE 1.
Comparing Transgender Women (n = 3,878) With and Without a Self-Reported Lifetime History of Jail or Prison*
| Jail/prison (N = 748) 19.3% | No jail/prison (N = 3,130) 80.7% | Model 1: Demographics | Model 2: Demographics and health-related indicators | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| % | % | RR (95% CI) | p-Value | RR (95% CI) | p-Value | |
| Age | ||||||
| 18–24 years | 15.9 | 11.5 | 0.91 (0.69, 1.20) | 0.51 | 0.63 (0.56, 1.02) | 0.07 |
| 25–44 years | 51.0 | 44.9 | 1.00 | 1.00 | ||
| 45+ years | 33.1 | 43.6 | 0.91 (0.75, 1.11) | 0.36 | 1.15 (0.93, 1.42) | 0.19 |
| Natal Sex/Gender Identity | ||||||
| Status | ||||||
| Non-binary gender identity | 34.9 | 42.6 | 1.00 | 1.00 | ||
| Binary gender identity | 65.1 | 57.4 | 1.23 (0.99, 1.52) | 0.07 | 1.22 (0.97, 1.53) | 0.09 |
| Race/Ethnicity | ||||||
| White (non-Hispanic) | 58.4 | 81.6 | 1.00 | 1.00 | ||
| Black | 14.8 | 2.8 | 3.26 (2.24, 4.75) | <0.0001 | 1.87 (1.21, 2.88) | 0.01 |
| Native American/Alaskan | 7.4 | 3.6 | 2.18 (1.53, 3.12) | <0.0001 | 1.65 (1.12, 2.42) | 0.01 |
| Native | ||||||
| Latina/Hispanic | 8.1 | 4.1 | 1.47 (0.99, 2.17) | 0.05 | 1.03 (0.67, 1.56) | 0.91 |
| Asian/Pacific Islander | 2.8 | 2.7 | 1.04 (0.61, 1.76) | 0.89 | 0.78 (0.44, 1.40) | 0.40 |
| Mixed Race/Ethnicity | 8.5 | 5.2 | 1.82 (1.31, 2.53) | 0.0004 | 1.28 (0.89, 1.83) | 0.18 |
| Annual Income | ||||||
| High income | 59.5 | 78.8 | 1.00 | 1.00 | ||
| Low income (≤ $19,999) | 40.5 | 21.2 | 1.31 (1.06, 1.61) | 0.1 | 1.14 (0.91, 1.42) | 0.25 |
| Educational Attainment | ||||||
| Some college or more | 74.7 | 87.8 | 1.00 | 1.00 | ||
| High school only or less | 25.3 | 12.2 | 1.39 (1.10, 1.76) | 0.01 | 1.28 (0.99, 1.65) | 0.05 |
| Health Insurance | ||||||
| Private | 37.3 | 62.1 | 1.00 | 1.00 | ||
| Public | 33.0 | 20.4 | 2.01 (1.62, 2.51) | <0.0001 | 1.64 (1.30, 2.07) | <0.0001 |
| Uninsured | 29.7 | 17.5 | 1.94 (1.53, 2.46) | <0.0001 | 1.55 (1.21, 1.99) | 0.0006 |
| Medical Gender Affirmation | ||||||
| Hormones | 65.4 | 62.5 | 1.04 (0.83, 1.30) | 0.73 | 0.88 (0.70, 1.12) | 0.31 |
| Surgery | 32.4 | 30.1 | 1.03 (0.84, 1.26) | 0.77 | 0.95 (0.76, 1.17) | 0.61 |
| Region | ||||||
| New England/Mid Atlantic | 22.6 | 28.8 | 0.84 (0.67, 1.06) | 0.15 | 0.86 (0.67, 1.09) | 0.21 |
| Southern | 19.7 | 20.3 | 1.02 (0.81, 1.29) | 0.85 | 1.08 (0.85, 1.38) | 0.54 |
| Midwest/West | 34.7 | 37.9 | 1.00 | 1.00 | ||
| California | 23.0 | 13.0 | 1.21 (0.92, 1.58) | 0.17 | 1.12 (0.84, 1.49) | 0.43 |
| Data Collection Method | ||||||
| Online | 76.5 | 94.2 | 1.00 | 1.00 | ||
| Paper | 23.5 | 5.8 | 2.03 (1.48, 2.78) | <0.0001 | 1.43 (1.00, 2.03) | 0.05 |
| Health Indicators | ||||||
| Daily cigarette smoker | 35.5 | 17.3 | – | – | 1.80 (1.46, 2.21) | <0.0001 |
| Substance use to cope | 39.6 | 20.6 | – | – | 1.39 (1.13, 1.71) | 0.002 |
| Suicide attempt | 50.9 | 35.4 | – | – | 1.20 (0.99, 1.46) | 0.07 |
| HIV-positive | 11.7 | 2.2 | – | – | 1.65 (1.09, 2.49) | 0.02 |
| Sex work | 35.4 | 7.1 | – | – | 2.87 (2.21, 3.73) | <0.0001 |
| Any physical assault | 46.5 | 20.0 | – | – | 1.32 (1.06, 1.66) | 0.01 |
| Any sexual assault | 28.0 | 6.3 | – | – | 2.16 (1.63, 2.87) | <0.0001 |
Bolded values indicate statistical significance at the alpha 0.05 level.
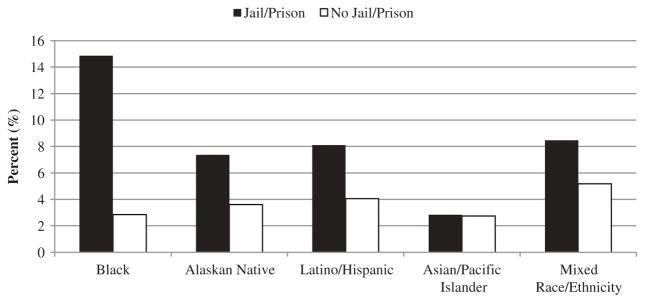
Overall, people of color comprised 41.6% of transgender women with a history of incarceration (311/748) and 18.4% of transgender women with no incarceration history (576/3,130); aRR = 1.90; 95% CI = 1.54, 2.35; p < 0.0001) (Figure 1). However, the racial/ethnic disparity in incarceration history was most apparent for Black transgender women (14.8% Black versus 2.8% White). Black transgender women had three-fold increased risk of correctional system engagement compared to white transgender women (aRR = 3.26; 95% CI = 2.24, 4.75; p < 0.0001), adjusting for sociodemographics (Table 1, Model 1).
FIGURE 1.
Racial/ethnic disparities in having been in jail/prison among transgender women (N = 3,878).
Adding health indicators (Table 1, Model 2) revealed health disparities by history of incarceration. Compared to their counterparts who had not been institutionalized, transgender women with a history of jail/prison were disproportionately burdened by negative health indicators, including smoking, substance use to cope, HIV-positive status, sex work, any physical assault, and any sexual assault, even after adjustment for sociodemographic characteristics. Adjusted RRs ranged from 1.32 to 2.87 across health outcomes (all p < 0.05), indicating 32% to 187% higher risk of poorer health for previously incarcerated women compared to those who had never been incarcerated. The only exception was suicide attempt, which approached statistical significance (p = 0.07). Furthermore, the racial, educational, and health insurance disparities in jail/prison history remained significant even when health indicators were added to the multivariable model.
Experiences of Victimization/Mistreatment and Denial of Healthcare in Jail/Prison
Self-reported victimization and mistreatment while in jail/prison was reported by 748 transgender women who reported a history of incarceration (Table 2). Overall, 47.0% of previously incarcerated transgender women reported any victimization in jail/prison. Denial of health care was reported by 24.5%.
TABLE 2.
Victimization and Maltreatment in Jail or Prison Among Transgender Women Reporting a History of Incarceration in Their Lifetime (N = 748)
| % | |
|---|---|
| Mistreatment from other inmates: | |
| Harassed | 37.4 |
| Physically assaulted/attacked | 16.7 |
| Sexually assaulted/attacked | 16.3 |
| Mistreatment from jail or prison officers/staff: | |
| Harassed | 35.1 |
| Physically assaulted/attacked | 8.5 |
| Sexually assaulted/attacked | 6.9 |
| Denied hormones | 20.7 |
| Denied regular medical care | 14.5 |
| Any mistreatment, victimization, or denial of healthcare in jail or prison | 50.1 |
| Any mistreatment or victimization | 47.0 |
| Any denied care | 24.5 |
In a multivariable model, Black, Latina/Hispanic, and mixed race/ethnicity transgender women of color disproportionately reported violence while incarcerated, as did uninsured and publicly insured women, and women who had ever taken hormones for gender affirmation (Table 3, left column, Model 1A). Transgender women who had been victimized while in jail/prison were more likely to report daily cigarette smoking, substance use to cope, suicide attempt, and reported HIV-seropositivity compared to transgender women who had not been victimized in jail or prison. Adjusted RRs ranged from 1.49 to 2.06 across health outcomes (all p < 0.05), indicating 49% to 106% higher risk of poorer health for transgender women experiencing victimization while in jail/prison compared to those who did not experience mistreatment while incarcerated.
TABLE 3.
Comparing Transgender Women With a Self-Reported History of Jail or Prison (N = 748) Who Report and Do Not Report Experiences of Mistreatment and/or Victimization (Outcome 1) and Denial of Healthcare (Outcome 2) While in Jail/Prison*
| Mistreated/victimized in jail/prison 47.0%
|
Denied healthcare in jail/prison 24.5%
|
|||
|---|---|---|---|---|
| Model 1B
|
Model 2B
|
|||
| RR (95% CI) | p-Value | RR (95% CI) | p-Value | |
| Age | ||||
| 18–24 years | 1.18 (0.72, 1.96) | 0.51 | 1.07 (0.64, 1.82) | 0.79 |
| 25–44 years | 1.00 | 1.00 | ||
| 45+ years | 0.61 (0.41, 0.92) | 0.02 | 0.52 (0.33, 0.83) | 0.006 |
| Natal Sex/Gender Identity | ||||
| Status | ||||
| Non-binary gender identity | 1.00 | 1.00 | ||
| Binary gender identity | 1.16 (0.76, 1.76) | 0.49 | 1.81 (1.12, 2.92) | 0.02 |
| Race/Ethnicity | ||||
| White (non-Hispanic) | 1.00 | 1.00 | ||
| Black | 2.31 (1.17, 4.55) | 0.02 | 1.17 (0.56, 2.47) | 0.67 |
| Native American/Alaskan Native | 1.66 (0.88, 3.14) | 0.12 | 1.09 (0.55, 2.13) | 0.81 |
| Latina/Hispanic | 2.73 (1.32, 5.67) | 0.007 | 0.53 (0.21, 1.33) | 0.17 |
| Asian/Pacific Islander | 1.85 (0.67, 5.12) | 0.24 | 0.16 (0.03, 0.75) | 0.02 |
| Mixed Race/Ethnicity | 2.51 (1.33, 4.71) | 0.004 | 0.71 (0.35, 1.42) | 0.33 |
| Annual Income | ||||
| High income | 1.00 | 1.00 | ||
| Low income (≤ $19,999) | 1.20 (0.80, 1.79) | 0.38 | 1.21 (0.78, 1.87) | 0.39 |
| Educational Attainment | ||||
| Some college or more education | 1.00 | 1.00 | ||
| High school only or less | 0.86 (0.55, 1.35) | 0.51 | 0.85 (0.52, 1.39) | 0.52 |
| Health Insurance | ||||
| Private | 1.00 | 1.00 | ||
| Public | 1.64 (1.05, 2.57) | 0.03 | 2.21 (1.32, 3.69) | 0.003 |
| Uninsured | 2.09 (1.31, 3.31) | 0.002 | 1.58 (0.91, 2.72) | 0.10 |
| Medical Gender Affirmation | ||||
| Hormones | 1.76 (1.11, 2.79) | 0.02 | 2.72 (1.64, 4.54) | 0.0001 |
| Surgery | 0.94 (0.64, 1.36) | 0.69 | 0.65 (0.42, 1.01) | 0.05 |
| Region | ||||
| New England/Mid Atlantic | 0.91 (0.57, 1.44) | 0.69 | 0.47 (0.27, 0.84) | 0.01 |
| Southern | 0.99 (0.62, 1.59) | 0.97 | 1.21 (0.73, 2.01) | 0.45 |
| Midwest/West | 1.00 | 1.00 | ||
| California | 1.19 (0.74, 1.94) | 0.47 | 1.11 (0.66, 1.87) | 0.70 |
| Data Collection Method | ||||
| Online | 1.00 | 1.00 | ||
| Paper | 1.04 (0.58, 1.85) | 0.89 | 1.10 (0.57, 2.14) | 0.77 |
| Health | ||||
| Daily cigarette smoker | 1.49 (1.04, 2.12) | 0.03 | 1.37 (0.91, 2.04) | 0.13 |
| Substance use to cope | 2.06 (1.45, 2.93) | <0.0001 | 1.53 (1.04, 2.26) | 0.03 |
| Suicide attempt | 1.87 (1.33, 2.62) | 0.0003 | 1.14 (0.77, 1.68) | 0.52 |
| HIV positive | 1.95 (1.07, 3.55) | 0.03 | 1.57 (0.85, 2.91) | 0.15 |
Bolded values indicate statistical significance at the alpha 0.05 level.
Characteristics associated with having been denied healthcare while in jail/prison were age, being Asian/Pacific Islander versus white (non-Hispanic), binary gender identity, public health insurance, hormones for gender affirmation, and substance use to cope (Table 3, right column, Model 1B).
DISCUSSION
This large study of transgender women in the U.S. found that transgender women of color, particularly Black, Native American/Alaskan Native, and mixed race/ethnicity women, disproportionately experienced corrections system engagement relative to white transgender women. In addition, Black and Latina/Hispanic transgender women were more likely to experience victimization while incarcerated. Health disparities were associated with a history of incarceration, as well as with victimization and/or mistreatment in these settings. These findings demonstrate disproportionate rates of incarceration among transgender women, especially among women of color. Transgender women of color were not only incarcerated at higher rates than White non-Hispanic transgender women, but also experienced higher rates of victimization and mistreatment while incarcerated. The intersecting forces of racism and transphobia produce multiple layers of marginalization among transgender women of color, which may ultimately result in a disproportionate burden of social, mental, and physical health disparities.
An extensive report on violence in California prisons recommended additional research on transgender inmates, with more empirical data on a broad range of types of sexual assault including staff-on-inmate assault (Jenness et al., 2007). To improve research on the situation faced by transgender inmates in the U.S., federal agencies must improve data collection to capture accurately the number of transgender inmates, where they are housed, their access and barriers to medical care, and their experiences of violence and mistreatment from both inmates and staff. In addition, training for prison staff is needed to improve knowledge about transgender inmates, and trainings should be inclusive of medical staff, corrections staff, and legal professionals. Furthermore, correctional intervention programs that address and respond to the pernicious effects of hypermasculinity in jails/prisons (Karp, 2010) are needed. Transgender peer educators and peer-led support groups for inmates while they are incarcerated could improve HIV prevention efforts and provide opportunities for inmates to share survival skills and self-protection strategies. Housing transgender inmates is a complicated issue that should be reviewed on a case-by-case basis with high priority given to the safety of the inmate. All inmates should be ensured access to appropriate medical care. For transgender inmates, the provision of hormones should not be dependent on their ability to document proof of prior use.
The disproportionate prevalence of incarceration among transgender women, especially those of color, are ultimately the product of larger issues of social marginalization and the intersectionality of racism, transphobia, sex-ism, and classism. Any system that enforces strict gender segregation will push transgender people to the margins, resulting in exclusion from social programs and support that non-transgender people generally benefit from. Gender segregation policies related to incarceration alternatives, drug treatment programs, homeless shelters, and other social welfare programs should be examined to understand fully how the exclusion of transgender people may contribute to their high rates of incarceration.
This study had several limitations that should be noted. First, data were from a cross-sectional survey; thus, any relationships observed between variables were associations only and cannot be presumed to be causal because temporal relationships were not established. Second, we did not have any information about the length of time a person was incarcerated, the length of time that had elapsed since incarceration, whether they were incarcerated in a jail, prison, or juvenile justice facility, whether they were presenting as transgender while incarcerated, or what the reason was for incarceration. Therefore, we do not know how these factors may have influenced our results. Last, all measures in NTDS were developed specifically for this survey. Lack of validated measures could have resulted in misclassification of information and non-comparability of data to other studies that have used standardized instruments. Despite these limitations, this is the largest sample of transgender women enrolled to date and provides key information to guide public health and policy efforts, including the importance of contextualizing health adversities (Sevelius et al., 2009; Sevelius, Keatley, & Gutierrez-Mock, 2011). These public health and policy efforts must be fully guided by the awareness that the intersection of racism, transphobia, sexism, and classism may create conditions of marginalization at all levels of society for transgender women of color that make them extremely vulnerable to a multitude of psychosocial and health disparities that must be addressed with multi-level, multi-systems approaches.
Acknowledgments
The authors are indebted to the National Gay & Lesbian Task Force (NGLTF) and the National Center for Transgender Equality (NCTE) for their leadership, resources, and community mobilization that made possible the National Transgender Discrimination Survey. Thank you especially to Jaime M. Grant, Lisa A. Mottet, Justin Tanis, Jack Harrison, Jody L. Herman, and Mara Keisling. The authors are grateful to the thousands of transgender people who generously volunteered to participate in this national survey.
Contributor Information
SARI L. REISNER, Department of Epidemiology, Harvard School of Public Health, Boston, Massachusetts, USA; and The Fenway Institute, Fenway Health, Boston, Massachusetts, USA.
ZINZI BAILEY, Social and Behavioral Sciences, Harvard School of Public Health, Boston, Massachusetts, USA.
JAE SEVELIUS, Center for AIDS Prevention Studies, Department of Medicine, University of California San Francisco, San Francisco, California, USA.
References
- Allison PD. Missing data. Thousand Oaks, CA: SAGE Publications; 2001. [Google Scholar]
- Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: A systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22. doi: 10.1016/S1473-3099(12)70315-8. http://dx.doi.org/10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. Am J Publ Health. 2013;103(10):1820–9. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R. Syndemic theory and HIV-related risk among young transgender women: The role of multiple, co-occurring health problems and social marginalization. Am J Publ Health. 2012;102(9):1751–7. doi: 10.2105/ajph.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GR, McDuffie E. Health care policies addressing transgender inmates in prison systems in the United States. J Correct Health Care. 2009;15(4):280–91. doi: 10.1177/1078345809340423. [DOI] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. Am J Publ Health. 2001;91(6):915–21. doi: 10.2105/AJPH.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell RW, Messerschmidt JW. Hegemonic masculinity: Rethinking the concept. Gender & Soc. 2005;19(6):829–59. doi: 10.1177/0891243205278639. [DOI] [Google Scholar]
- Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: Results from a household probability sample of adults. Am J Publ Health. 2012;102(1):118–22. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Vlahov D. Social determinants and the health of drug users: Socioeconomic status, homelessness, and incarceration. Publ Health Rep. 2002;117(s1):s135–45. [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Deleon J, Osmer E, Doll M, Harper G. Overlooked, misunderstood, and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adoles Health. 2006;38(3):230–6. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: A report of the Transgender Discrimination Survey. Washington, DC: National Centre for Transgender Equality and National Gay and Lesbian Task Force; 2011. [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Goodness of fit tests for the multiple logistic regression model. Commun Statist: Theory Methods. 1980;9(10):1043–69. doi: 10.1080/03610928008827941. [DOI] [Google Scholar]
- Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Statist Med. 1997;16(9):965–80. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Jenness V. The California Department of Corrections and Rehabilitation Wardens’ Meeting. Irvine, CA: University of California, Irvine, Center for Evidence-Based Corrections, Department of Criminology, Law and Society; 2009. Transgender inmates in California’s prisons: An empirical study of a vulnerable population. [Google Scholar]
- Jenness V, Maxson CL, Matsuda KN, Sumner JM. Violence in California correctional facilities: An empirical examination of sexual assault. Irvine, CA: University of California, Irvine; 2007. Report submitted to the California Department of Corrections and Rehabilitation. [Google Scholar]
- Jewkes Y. Men behind bars: “Doing masculinity” as an adaptation to imprisonment. Men Masculin. 2005;8(1):44–63. doi: 10.1177/1097184X03257452. [DOI] [Google Scholar]
- Karp DR. Unlocking men, unmasking masculinities: Doing men’s work in prison. J Men’s Stud. 2010;18(1):63–83. doi: 10.3149/jms.1801.63. [DOI] [Google Scholar]
- Kawachi I. Income inequality and health. In: Berkman L, Kawachi I, editors. Social epidemiology. New York, NY: Oxford University Press; 2000. pp. 76–94. [Google Scholar]
- Kenagy GP. Transgender health: Findings from two needs assessment studies in Philadelphia. Health & Soc Work. 2005;30(1):19–26. doi: 10.1093/hsw/30.1.19. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Understanding sociodemographics differences in health—The role of fundamental social causes. Am J Publ Health. 1996;86(4):471–3. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi EL, Wilchins RA, Priesing D, Malouf D. Gender violence: Transgender experiences with violence and discrimination. J Homosexual. 2002;42(1):89–101. doi: 10.1300/j082v42n01_05. [DOI] [PubMed] [Google Scholar]
- Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19:S67–72. doi: 10.1097/01.aids.0000172879.20628.e1. [DOI] [PubMed] [Google Scholar]
- Mosher DL. Macho men, machismo, and sexuality. Ann Rev Sex Res. 1991;2(1):199–247. doi: 10.1080/10532528.1991.10559871. [DOI] [Google Scholar]
- Mosher DL, Anderson RD. Macho personality, sexual aggression, and reactions to guided imagery of realistic rape. J Res Person. 1986;20(1):77–94. http://dx.doi.org/10.1016/0092-6566(86)90111-X. [Google Scholar]
- Mosher DL, Serkin M. Measuring a macho personality constellation. J Res Person. 1984;18(2):150–63. http://dx.doi.org/10.1016/0092-6566(84)90026-6. [Google Scholar]
- Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, Becker J. Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res. 2010;47(1):12–23. doi: 10.1080/00224490903062258. [DOI] [PubMed] [Google Scholar]
- Operario D, Nemoto T, Iwamoto M, Moore T. Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS Behav. 2011;15(3):674–82. doi: 10.1007/s10461-010-9795-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott DJ, Zeichner A. Effects of hypermasculinity on physical aggression against women. Psychol Men & Masculin. 2003;4(1):70–8. doi: 10.1037/1524-9220.4.1.70. [DOI] [Google Scholar]
- Reback CJ, Simon P, Bemis C, Gatson B. The Los Angeles Transgender Health Study: Community report. Los Angeles, CA: University of California, Los Angeles; 2001. [Google Scholar]
- Reisner SL, Mimiaga MJ, Bland S, Mayer KH, Perkovich B, Safren SA. HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts. J Assoc Nurses AIDS Care. 2009;20(5):373–86. doi: 10.1016/j.jana.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabo DF, Kupers TA, London W. Prison masculinities. Philadelphia, PA: Temple University Press; 2001. [Google Scholar]
- Sausa LA, Sevelius J, Keatley J, Iñiguez JR, Reyes M. Policy recommendations for inclusive data collection of trans people in HIV prevention, care and services. San Francisco, CA: Center of Excellence for Transgender HIV Prevention: University of California, San Francisco; 2009. [Google Scholar]
- Semaan S, Lauby J, Liebman J. Street and network sampling in evaluation studies of HIV risk-reduction interventions. AIDS Rev. 2002;4(4):213–23. [PubMed] [Google Scholar]
- Sered S, Norton-Hawk M. Criminalized women and the health care system: The case for continuity of services. J Correctional Health Care. 2013;19(3):164–77. doi: 10.1177/1078345813486323. [DOI] [PubMed] [Google Scholar]
- Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–89. doi: 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius JM, Keatley J, Gutierrez-Mock L. HIV/AIDS programming in the United States: Considerations affecting transgender women and girls. Womens Health Iss. 2011;21(6 Suppl):S278–82. doi: 10.1016/j.whi.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: The importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ Prev. 2009;21(2):113–27. doi: 10.1521/aeap.2009.21.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- South v. Gomez, No. 99-15976, 2000 U.S. App. LEXIS 3200 (9th Cir. Feb. 25, 2000).
- Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- Tarzwell S. The gender lines are marked with razor wire: Addressing state prison policies for the management of transgender prisoners. Columbia Human Rights Law Rev. 2006;38(167):70. [Google Scholar]
- Tate CC, Ledbetter JN, Youssef CP. A two-question method for assessing gender categories in the social and medical sciences. J Sex Res. 2013;50(8):767–76. doi: 10.1080/00224499.2012.690110. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice. Federal Bureau of Prisons Program Statement 6031.01, Patient Care (Jan. 15, 2005) Bureau of Prisons Health Services Manual, Program Statement 6000.3, §6803. 2005 Retrieved from http://www.bop.gov/policy/progstat/6031_001.pdf.
- Van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Statist Methods Med Res. 2007;16(3):219–42. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- Van Buuren S, Brand J, Groothuis-Oudshoorn C, Rubin DB. Fully conditional specification in multivariate imputation. J Statist Comput Simul. 2006;76(12):1049–64. [Google Scholar]