Abstract
Objective
To synthesize findings from the published literature on the use of technology in the NICU to improve communications and interactions among health care providers, parents, and infants.
Data Sources
Electronic databases including Ovid MEDLINE, CINAHL, Web of Science, and Google Scholar were searched for related research published through May 2016. The reference lists of all studies were reviewed, and a hand search of key journals was also conducted to locate eligible studies.
Study Selection
Eleven studies (five quantitative, two qualitative, and four mixed methods) were identified that met the inclusion criteria. Only studies published in English were included.
Data Extraction
Whittemore and Knafl’s methodology for conducting integrative reviews was used to guide data extraction, analysis, and synthesis. Data were extracted and organized according to the following headings: author, year, and location; study purpose and design; sample size and demographics; technology used; study findings; and limitations.
Data Synthesis
Various technologies were used, including videoconferencing, videophone, and commercially available modalities such as Skype, FaceTime, AngelEye, and NICView Webcams. In the 11 studies, three main outcomes were evaluated: parents’ perception of technology use, health care providers’ perceptions of technology use, and objective outcomes, such as parental anxiety or stress or infant length of stay. Overall, parents and health care providers perceived the varied interventions quite favorably, although a few significant differences were found for the objective measures.
Conclusion
Several interventions have been tested to improve communications and promote interactions among NICU health care team members, parents, and infants. Although initial findings are positive, research in this area is quite limited, and the reviewed studies had several limitations. There is a significant need for further rigorous research to be conducted with diverse samples.
Keywords: communication, family-centered care, integrative review, neonatal intensive care unit, NICU, parent perceptions, technology
For the parents of the nearly 280,000 newborns admitted to NICUs in the United States annually, the NICU experience is stressful and overwhelming (Osterman, Martin, Mathews, & Hamilton, 2011). Indeed, 15% to 63% of parents have reported clinically relevant symptoms of anxiety, depression, acute stress disorder, or posttraumatic stress disorder during their infants’ hospitalizations (Ahlund, Clarke, Hill, & Thalange, 2009; Carter, Garrity-Rokous, Chazan-Cohen, Little, & Briggs-Gowan, 2001; Lefkowitz, Baxt, & Evans, 2010; Miles, Holditch-Davis, Schwartz, & Scher, 2007; Rogers, Kidokoro, Wallendorf, & Inder, 2013; Vanderbilt, Bushley, Young, & Frank, 2009; Woodward et al., 2014). Lasting problems such as posttraumatic stress disorder, poor coping, and depression are not uncommon (Ahlund et al., 2009; Feeley et al., 2011; Kersting et al., 2004; Shaw, Bernard, Storfer-Isser, Rhine, & Horwitz, 2013). Further, these lasting effects may play a negative role in infant development (Carter et al., 2001; Woodward et al., 2014; Zelkowitz, Na, Wang, Bardin, & Papageorgiou, 2011) and parent–infant bonding (Nicol-Harper, Harvey, & Stein, 2007; Youngblut, Brooten, Cantwell, del Moral, & Totapally, 2013).
Although some predictors of these problems may be caused by factors outside of our control, such as the severity of infant illness or parent demographic factors (Feeley et al., 2011; Rogers et al., 2013), the NICU experience, specifically parents’ stress regarding role alteration, may contribute to these problems (Miles et al., 2007; Woodward et al., 2014). Factors associated with parental stress in the NICU setting, such as separation, helplessness, and inability to share the infant with other family members, may be modifiable with effective interventions.
Interventions to support parent–provider communication and collaboration during NICU hospitalization are vital for family-centered care and may reduce parents’ stress and anxiety.
Parents of infants in the NICU face unique challenges in maintaining physical proximity to their infants. Infants in the NICU often have prolonged hospital stays and may have restrictions imposed on visitation for a variety of reasons. Additionally, many parents may not be able to visit regularly because of employment obligations, financial strain, child care responsibilities, and geographic separation. These barriers are particularly salient for low-income families and families who reside in rural regions, because they must travel great distances to visit their infants. Finally, infants may need to be transferred to institutions with appropriate resources for high-risk infant care while the mother recovers at the hospital where she gave birth. Thus, there is increasing recognition that alternative modes to foster contact between parents and their infants, as well as with health care providers who care for the infants, is needed.
Family involvement is vital to optimize attachment between families and infants and to enhance infants’ physical, cognitive, and socioemotional development (Craig et al, 2015). Family-centered care (FCC), endorsed by the American Academy of Pediatrics and many other organizations, is based on the principles of communication, collaboration, and respect (Eichner & Johnson, 2012; Ramezani, Hadian Shirazi, Sabet Sarvestani, & Moattari, 2014). A central tenet of FCC is the establishment of trusting relationships between caregivers and members of the health care team through optimal communication (Epstein, Sherman, Blackman, & Sinkin, 2015). However, little is known about alternative methods of communication with health care team members and interaction with NICU infants whose parents are not able to be physically present in the NICU. Despite significant advances in communication technology, unanswered questions remain. For example, what types of technology are used in the NICU to foster communication? What are parents’ perceptions of communicating with health care team members via technology? Similarly, how do health care team members perceive the use of alternative methods of communication with parents? Is the use of varied types of technology to facilitate interaction and communication associated with improved parental or infant outcomes?
A better understanding of how technology is used in NICU settings to enhance communication and interaction and the effects of this technology on parent and infant outcomes may lead to the development and testing of interventions to strengthen aspects of FCC. Ultimately, these interventions may improve parental and infant outcomes. Thus, the purpose of our integrative review was to summarize studies conducted in NICU settings by researchers who used alternative methods to enable communication and interaction among health care team members, parents, and infants.
Methods
Design
The current analysis was guided by Whittemore and Knafl’s (2005) updated integrative review method, which provided a more comprehensive understanding of the concepts of interest. This approach begins with a well-defined and comprehensive literature search strategy, critical to avoid bias and increase the validity of the integrative review. Next, the search is conducted based on the outlined search strategy. Third, although critical appraisal of the literature with various methods is not a requirement of an integrative review, quality scores may help support data interpretation (Whittemore & Knafl, 2005). During the analytic phase, a systematic approach is used to extract, code, and reduce primary sources, thereby allowing for conclusions to be made (Whittemore & Knafl, 2005). We decided to use an integrative review method because it allows for diverse research designs and methods to be included, thereby providing a more comprehensive analysis of the use of technology in the NICU to facilitate communication and interaction. Further, given that this is an emerging phenomenon of interest, much of the literature is descriptive in nature and thus more appropriate for an integrative review than a systematic review, which often includes more rigorous clinical trials.
Data Sources and Search Methods
Three strategies were used in the literature search: electronic searches, ancestral searches, and hand-searches of journals known to publish articles related to communication in the NICU. An electronic keyword search was conducted with the Ovid MEDLINE, CINAHL, Web of Science, and Google Scholar databases. Additionally, a search of grey literature was conducted with searches limited to domains that used .gov, .org, and .edu. The search used keywords and MeSH terms in two main search topic areas: neonatal intensive care and alternative modes of communication. MeSH terms or keywords for neonatal intensive care included intensive care units, neonatal intensive care unit, and NICU. For alternative modes of communication used in NICU settings, MeSH terms or keywords included Skype, videoconferencing, facetime, google hangout, webcam, virtual visitation, jabber, periscope, oovoo, and web camera. Our search was limited to original research that included qualitative, quantitative, or mixed-methods studies written in English in which researchers examined the effects of some aspect of communication technology on parents, health care team members, or infant outcomes in the NICU setting. No date restriction was placed on published articles.
Search Outcome and Study Selection
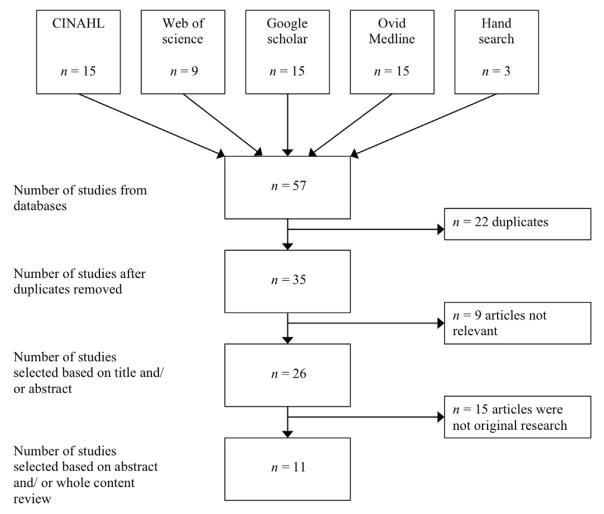
Our search yielded 57 records (see Figure 1). The abstracts of these articles were reviewed independently for relevance and eligibility criteria by the authors. Articles that were not relevant or did not meet the inclusion criteria were discarded. Any discrepancies in study inclusion were resolved through consensus. This process resulted in 15 studies that were reviewed in entirety by the authors. Again, any discrepancies in eligibility criteria were discussed with the entire team and resolved through consensus; the result was a total of 11 studies that met eligibility criteria.
Figure 1.
Summary of search outcome and study selection for integrative review.
Quality Appraisal
Consistent with Whittemore and Knafl’s (2005) approach to conducting an integrative review, a formal quality appraisal tool was not used. However, study limitations are addressed in Supplemental Table S1. Although a quality appraisal tool can assist with data interpretation, the studies included in this review were quite varied in methods and largely descriptive in nature, which precluded formal appraisal. We did not exclude any studies based on critique of rigor.
Data Extraction and Synthesis
From the 11 studies that met inclusion criteria, data were extracted and organized according to the following headings: author, year, and location; study purpose and design; sample size and demographics; technology used; study findings; and limitations. The studies were divided into three groups based on target population: parent only, parent and other (health care provider or infant), or health care provider only. The first and last authors evaluated each study independently to identify common themes. They then compared findings, arrived at consensus, and tabulated the data (see Supplemental Table S1). Although the authors did not conduct a systematic review, they were guided by the meta-analysis of observational studies in epidemiology (MOOSE) guidelines in all aspects of the review including title, abstract, introduction, sources, study selection, results, and discussion (Stroup et al., 2000).
Results
The primary purpose of most of the studies was to examine parents’ or health care providers’ perceptions of technology (e.g., Web cameras, videophone, text messages) to augment communication or interaction with health care team members, parents, or NICU infants. Other researchers described viewing habits of NICU infants by their mothers and fathers (Rhoads, Green, Gauss, Mitchell, & Pate, 2015), examined how viewing infants influenced parental anxiety or stress (Rhoads, Green, Mitchell, & Lynch, 2015), or evaluated the effect of Web camera viewing on NICU infants’ length of stay (Yeo, Ho, Khong, & Lau, 2011). The 11 studies included five quantitative studies (Globus et al., 2016; Gray et al., 2000; Joshi, Chyou, Tirmizi, & Gross, 2016; Yeo, Ho, Khong, & Lau, 2011), two qualitative studies (Lindberg, Axelsson, & Ohrling, 2009a, 2009b), and four mixed-methods studies (Epstein, Sherman, Blackman, & Sinkin, 2015; Gund et al., 2013; Piecuch et al., 1983; Rhoads, Green, Mitchell, et al., 2015). Six studies were conducted in the United States, three were conducted in Sweden, one was conducted in Singapore, and one was conducted in Israel.
Eight studies were tests of interventions during the NICU admission. The three Swedish studies involved videoconferencing interventions during an “on leave” period after infants went home but were still being monitored by NICU staff. In two studies, researchers examined family perceptions of various aspects of the quality of care 1 to 5 months after discharge (Gray et al., 2000; Gund et al., 2013). Piecuch et al. (1983) examined use of a videophone by hospitalized mothers of infants transferred to a different institution and also collected data related to the number of calls made to the NICU after mothers were discharged from the hospital.
Several different modes of technology were used. In three studies, researchers used a videophone whereby mothers in the intervention group could initiate a call to their infant’s unit and a video picture was transmitted for viewing (Lindberg et al., 2009a, 2009b; Piecuch et al., 1983). Epstein et al. (2015) and Gund et al. (2013) used Web-based videoconferencing such as Skype (Skype Technologies, Redmond, WA) or Face-Time (Apple, Cupertino, CA). Researchers also used commercially available Webcam systems, such as NICView (Joshi et al., 2016) or Angel Eye (Rhoads, Green, Gauss, et al., 2015; Rhoads, Green, Mitchell, et al., 2015), and three groups of researchers used investigator-developed systems (Gray et al., 2000; Gund et al., 2013; Yeo et al., 2011). Globus et al. (2016) used short message services (SMS) texting with parents. The main findings from the 11 studies were categorized under three key areas of focus: (a) parents’ perceptions of the use of technology for communication and interaction, (b) nurses’ perceptions of the use of technology for communication and its effect on workflow, and (c) parent and infant outcomes associated with the use of technology in the NICU. More than one area of focus was captured in several studies (n = 5).
Parents’ Perceptions of the Use of Technology for Communication and Interaction
In eight studies, researchers evaluated parents’ perceptions of the intervention on various aspects of the NICU experience, such as communication, satisfaction, confidence in caring for their infants, and impressions of seeing their infants. Overall, parents’ perceptions were positive, although because outcome measures and methods varied, summarizing consistent findings was difficult with one exception—parents’ ability to see their infants. All researchers who explored parents’ impressions of seeing their infants reported positive findings. Parents were generally appreciative of the opportunity to see their infants, believed that being able to do so reduced their stress and anxiety (Rhoads, Green, Mitchell, et al., 2015), or felt relief that their imagined view of their infants was worse than reality (Piecuch et al., 1983). Rhoads, Green, Mitchell, et al. (2015) did find, however, that a small number of parents expressed helplessness, sadness, stress, or guilt when they saw their infants on the Webcam rather than being physically with them in the NICU. Epstein et al. (2015) found that several parents reported that videoconferencing allowed other family members such as elderly grandparents and young siblings who would not otherwise be able to visit the NICU to see the infant, which they found to be highly valuable.
Perceptions of communication and satisfaction were less consistent across studies, largely because what was evaluated varied from study to study. For example, Globus et al. (2016) measured satisfaction with one question of overall satisfaction with “treatment and staff attitude during hospitalization,” whereas Gray et al. (2000) assessed satisfaction using the Picker Institute’s NICU Family Satisfaction survey, which addresses quality of care, continuity of care, family and infant support, and confidence and trust in clinicians (Picker Institute, 2000). Epstein et al. (2015) did not report satisfaction scores individually but as a combined score with other concepts of communication, information sharing, and relationships with staff using Penticuff’s Parents’ Understanding of Infant Care and Outcomes survey (Penticuff & Arheart, 2005). In terms of outcomes, Globus et al. (2016) did not find significant differences in overall satisfaction between intervention and control groups, although significant improvement was found for some aspects of communication (see Supplemental Table S1). Gray et al. (2000) found that 3% of parents in the intervention group versus 13% of parents in the usual care group reported problems with quality of care and that 13% of intervention group parents reported problems with the NICU environment and visitation policy, compared with 50% of usual care group parents, suggesting significant differences between the intervention and usual care participants. Both of these findings were significantly different. Parents who used Skype or FaceTime to interact with staff reported significantly higher postintervention scores for overall views of having an infant in the NICU compared with pre-intervention scores (mean score = 69.2, standard deviation [SD] = 5.7 vs. mean score = 63.2, SD = 5.8, respectively; p < .001) and for scores of experiences within the last week (mean score = 29.5, SD = 3.2, vs. mean score = 27.6, SD = 2.8, respectively; p = .04; Epstein et al., 2015).
Lindberg et al. (2009b) evaluated parents’ perceptions of videoconferencing, and Gund et al. (2013) examined the benefit of the use of a Web application or Skype to interact with staff during the “on leave” period when the infant was at home but still being monitored by NICU staff. Parents in both studies appeared to find the interventions helpful in terms of building confidence to take care of their infants at home and providing a sense of security during that time of transition, although in both studies the sample sizes were small, and significant differences could not be evaluated because of a lack of comparison group, questionnaire design, and other methods issues.
Overall, videoconferencing that provides an opportunity for parents to see their infants appears to be helpful and meaningful to parents. Videocon-ferencing with staff may also be useful to parents during and after hospitalization. The usefulness of other interventions such as educational resources and Web applications is less understood.
Health Care Providers’ Perceptions of the Use of Technology for Communication and Interaction and Its Affect on Work Flow
In five studies, researchers examined health care providers’ perceptions of technology use in the NICU to facilitate communication or interaction with parents and NICU infants (Epstein et al., 2015; Globus et al., 2016; Gund et al., 2013; Joshi et al., 2016; Lindberg et al., 2009a). Interventions included Skype, FaceTime, SMS texting, NICView, and videoconferencing. Parents and nurses were included in all studies except that of Joshi et al. (2016), and only Epstein et al. (2015) included health care providers other than nurses.
Using a randomized controlled trial design, families were randomized to standard home health care, standard home health care augmented with a Web application, or standard home health care augmented with videoconferencing via Skype (Gund et al., 2013). Nurses were asked to give daily feedback through the Web application in response to parents’ questions and assessments of their infants. Additionally, nurses who cared for families in the Skype arm were asked to make regular video calls to families. Most (80%) nurses responded favorably to the use of technology to augment their services; however, one nurse, who reported the least computer experience, was “neutral” with the incorporation of technology. Most nurses (80%) thought that parents appreciated the additional contact via the Web or Skype, and two thirds of the nurses believed that the technology facilitated the provision of safe care. However, the nurse who rated herself as having minimal computer experience expressed a negative attitude about the use of information and communication technology, voicing concerns over the potential for information and communication technology to interfere with the nurse–patient relationship (Gund et al., 2013).
Most parents and health care providers perceived technology use to be feasible and helpful, although not all expectations were met.
Lindberg et al. (2009a) examined nurses’ perceptions of videoconferencing to support parents after their infants were discharged from the NICU. Nurses perceived the use of technology quite favorably; they noted that videoconferencing enabled meetings with the entire family, facilitated a more comprehensive assessment of the overall home situation, and provided extra security to the family. Epstein et al. (2015) examined the feasibility and acceptability of an intervention that used Skype or FaceTime to provide daily updates from the nurse, nurse practitioner, or physician to parents. Most health care providers (94%) perceived the integration of technology to be feasible. Additionally, more than 90% of providers believed that the technology intervention was reliable to communicate updates with parents of NICU infants (Epstein et al., 2015). Joshi et al. (2016) examined nurses’ perceptions of a Web camera that allowed parents to view their infants. Nearly three quarters (72.9%) of nurses believed that having the Web camera was useful for parents. Further, nearly two thirds (64.6%) of nurses believed that parental anxiety was reduced with the use of a Web camera, although it is not clear how that was measured. Through open-ended questions, nurses expressed concerns related to work flow with the use of the Web camera, with the time it took to reposition the camera when an infant was moved as the major concern. Finally, Globus et al. (2016) also examined the effect of SMS on nurses’ workflow. From their results, they reported that in the postintervention period, more than three quarters of nurses (78.1%) found SMS communication to be convenient and user friendly compared with 66% of nurses before the intervention (p < .001).
From these combined results, we suggest that health care providers, and nurses in particular, perceive the use of technology to foster communication and interaction with parents quite favorably. Concerns related to its use stemmed primarily from glitches in the various systems, including episodes of cameras freezing and blurred images, and the need to reposition cameras to facilitate views of the infants.
Parent and Infant Outcomes
Four research groups evaluated outcomes such as Webcam log-in frequency and duration, parental stress and anxiety, maternal–infant bonding, and infant length of stay. Stress and anxiety were key concepts in three studies. Rhoads, Green, Mitchell, et al. (2015) used the Parental Stressor Scale: NICU (PSS:NICU; Miles et al., 2007) and the State–Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1977) to evaluate parental stress and anxiety at the time of enrollment and at 1 and 2 weeks after enrollment in their Webcam intervention study. No correlation was found between overall PSS:NICU scores and minutes logged into the Webcam (watching infant) at any of the time points. However, a significant positive correlation was found at all three time points between the maximum number of minutes watching the infant in any one session and the PSS:NICU subscale assessing stress due to the infant’s appearance, which suggested that parents’ stress may increase with Webcam use. Interviews with parents clarified this finding somewhat, in that some parents who saw their infants but who could not act to comfort, change position, or intervene reported increased stress. Increased stress was expressed by a small number of parents but is worth further investigation. No relationship was found for STAI scores and any measure at any time point. Similarly, in their study of SMS texting, Globus et al. (2016) found no significant change in parents’ anxiety as measured by two questions (How anxious I feel now and How anxious I feel when I think about taking my infant home) after the intervention. However, in their qualitative interviews with parents, Rhoads, Green, Mitchell, et al. (2015) found that some parents expressed decreased anxiety because, for example, the Webcam allowed parents to see how their infants were doing when they could not be in the NICU with them. Other parents expressed increased anxiety when, for example, the camera was turned off, because parents tended to worry about reasons why the camera may have been turned off.
Rhoads, Green, Mitchell, et al. (2015) examined maternal–infant bonding and Webcam use and found a significant correlation (r(8) = 0.84, p = .01) between bonding scores and minutes viewing infant at the last time point (2 weeks after enrollment) but not the previous two time points (at enrollment and 1 week after enrollment). However, it is unclear whether this correlation is due to Webcam use or the passage of time itself, because the number of participants at Time Point 3 was very small (n = 8). Yeo et al. (2011) were the only researchers to examine Webcam use and infant outcomes such as length of stay and postgestational age at discharge, and they found no significant differences in either outcome between control and intervention group infants.
Discussion
Our review was needed because technologies to assist patients with health care needs are increasingly varied, creative, and easy to use and because identification of effective, meaningful uses of these technologies may improve FCC—a goal for quality health care (Institute of Medicine, 2001). Parents whose infants are in the NICU are vulnerable to stress, depression, anxiety, and posttraumatic stress disorder; are entrenched in an unfamiliar environment; and participate in making decisions that affect their infants’ well-being. Health care providers seek to guide them through NICU hospitalization and modern, easy-to-use, widely available technology may help build the familiarity and trust needed to accomplish this goal.
We sought to better understand the kinds of interventions that have been tested for NICU parents, the outcomes of greatest interest to researchers, and the methods used to evaluate interventions with the goal of identifying next steps in this field. We found that a variety of technologies have been used, including investigator-designed videoconferencing and videophone, as well as commercially available modalities that are free and publicly available, such as Skype and FaceTime, or that are available for purchase by hospital systems, such as the AngelEye or NICView Webcams. Only three author groups (Epstein et al., 2015; Gray et al., 2000; Rhoads, Green, Lewis, et al., 2012) discussed security measures, national or international privacy regulations, or the Health Insurance Portability and Accountability Act laws. The lack of attention to privacy is surprising given the levels of concern in the research ethics and regulatory realms. However, Skype has been used by military personnel to communicate with family members, even from highly sensitive areas such as Afghanistan (Luxton, Mishkind, Crumpton, Ayers, & Mysliwiec, 2012). Although health care regulations are different from military regulations, the military’s practice may help guide our lines of thought about how health care providers can use technology to support families while still maintaining confidentiality.
We found that most researchers reported positive findings in terms of parents’ perceptions of text and video/Webcam interventions. Overall, parents appreciated the ability to see or receive information about their infants. However, there also is cause for caution. Some parents expressed negative feelings about Webcam use, and, although only a small number of parents expressed these perspectives, this must be taken seriously and explored more deeply. Objective measures of parental stress and anxiety and infant length of stay showed no significant changes among intervention participants. It is likely that Webcam use alone may be inadequate in relieving parental stress or reducing length of stay because many other factors are involved that may influence these outcomes. Further identification and evaluation of expected outcomes is needed. Moreover, the use of bundled interventions, such as those used by Gray et al. (2000), which included pictures of the infant, parent support tools, and educational resources, may be more effective at achieving outcomes goals. Our review showed that nurses largely support the use of technology to communicate with parents but that increased workload is a real and common concern.
Limitations
Several limitations warrant discussion. First, a quality appraisal of individual studies was not undertaken. Consistent with Whittemore and Knafl’s (2005) method for integrative reviews, we included all studies meeting eligibility criteria irrespective of the rigor of the design or methods used. Although this allowed for a comprehensive review of all relevant studies, findings must be viewed in light of the limitations identified, including the relatively limited number of studies reviewed and the inclusion of studies with significant design or implementation limitations. Second, our review was limited to studies published in English. We appreciate that improvement to communications and interactions in the NICU setting is a global issue, and studies published in other languages may provide a more comprehensive assessment.
The studies included in the current review have a number of identified weaknesses (see Supplemental Table S1). Authors of most studies used small sample sizes and/or convenience sampling or required eligible participants to have a certain level of technologic expertise or access. These limitations can be indicative of inherent bias and restrict generalizability of the results. Additionally, many of the researchers included rather homogenous samples, which further limits generalizability. Moreover, several studies included very limited demographic information, which limits interpretation of study findings. Finally, with the exception of one study, health care provider perceptions were limited to nurses. Given the multidisciplinary nature of NICU care, researchers should include all members of the health care team for more diverse perspectives.
Interventions such as Webcams, Skype, text messaging, and online educational resources show promise in supporting communication, relieving parental stress, and promoting parent–infant attachment.
Implications for Practice and Research
Findings from multiple studies have affirmed parents’ desires for effective communication with their infants’ providers (Bialoskurski, Cox, & Wiggins, 2002; Stubblefield & Murray, 1999; Wigert, Dellenmark, & Bry, 2013) and that the NICU experience is highly stressful and may put parents and infants at risk for attachment and development challenges later (Ahlund et al., 2009; Carter et al., 2001; Feeley et al., 2011; Kersting et al., 2004; Shaw et al., 2013; Woodward et al., 2014; Zelkowitz et al., 2011). The use of contemporary technologies to effectively bolster communication, promote parent–infant attachment, and relieve stress may significantly affect parents’ and infants’ NICU experiences and future outcomes. Overall, the findings from this integrative review support the use of interventions such as Webcam systems for infant viewing and Skype, FaceTime, text messaging, and online educational resources for provider–parent communication and parent updates. It should not be an expectation that any technology-based intervention could replace effective in-person communication or parent–infant interaction. However, for parents who must work, who live a distance from the hospital, or who are busy with care for other children, or for NICU settings in which there is little space to accommodate parents for extended hours, these interventions may supplement or augment NICU standard practices. Future research, including randomized controlled trials with larger and more demographically diverse sample sizes, is needed. Additionally, the types of technologies, individual or bundled, that are likely to benefit parents and the ways in which parents are likely to benefit (e.g., measurable, logical outcomes) deserve thoughtful consideration.
Interventions to support communication with parents and parents’ interactions with infants have involved, almost exclusively, nurses as contact points or intermediaries. In terms of nursing practice, then, the workability and benefit of these interventions must be evaluated for nurses as well as for parents. Given the current shift in health care toward an interprofessional team-based approach (Chesluk et al., 2012; Manser, 2009) and parents’ desire for communication with their infants’ doctors, future studies should consider interventions that involve active input from providers in multiple professions.
Conclusion
The findings of our review provide a summary of the types of technologies used and outcomes identified thus far to promote communication and parent–infant interaction in the NICU. Because outcomes measured varied among studies, the findings were difficult to summarize and compare, but this difficulty highlights the fact that the goals of technology use to support FCC in the NICU have yet to be clearly defined. To date, researchers have focused on nurse–parent interactions, but given the current focus on team-based care, in future studies, researchers should include interventions to target multiple professions, because parents interact with many providers in addition to nurses. Bundled interventions that provide parents with opportunities to interact with their infants and NICU staff may ultimately be most efficient and useful. Finally, although multiple technologic modalities have been used with somewhat mixed results, our integrative review provides enough support for continued study of the use of technology to promote communication and interaction between parents, health care providers, and infants. Larger randomized controlled trials with carefully selected interventions and outcome measures are now warranted and necessary.
Supplementary Material
Acknowledgments
Supported by a career development award from the National Institute of Nursing Research (NINRK23NR015810; primary investigator: J. Alhusen).
Footnotes
The authors report no conflict of interest or relevant financial relationships.
Note: To access the supplementary material that accompanies this article, visit the online version of the Journal of Obstetric, Gynecologic, & Neonatal Nursing at http://jognn.org and at http://dx.doi.org/10.1016/j.jogn.2016.11.019.
Contributor Information
Elizabeth G. Epstein, Associate professor for the University of Virginia School of Nursing, Charlottesville, VA.
Jaqueline Arechiga, Student at the University of Virginia School of Nursing, Charlottesville, VA.
Margaret Dancy, Student at the University of Virginia School of Nursing, Charlottesville, VA.
Jordan Simon, Student at the University of Virginia School of Nursing, Charlottesville, VA.
Daniel Wilson, Associate Director for Collections and Library Services, University of Virginia Claude Moore Health Sciences Library, Charlottesville, VA.
Jeanne L. Alhusen, Associate professor for the University of Virginia School of Nursing, Charlottesville, VA.
References
- Ahlund S, Clarke P, Hill J, Thalange NK. Post-traumatic stress symptoms in mothers of very low birth weight infants 2–3 years post-partum. Archives of Women’s Mental Health. 2009;12(4):261–264. doi: 10.1007/s00737-009-0067-4. http://dx.doi.org/10.1007/s00737-009-0067-4. [DOI] [PubMed] [Google Scholar]
- Bialoskurski MM, Cox CL, Wiggins RD. The relationship between maternal needs and priorities in a neonatal intensive care environment. Journal of Advanced Nursing. 2002;37(1):62–69. doi: 10.1046/j.1365-2648.2002.02057.x. http://dx.doi.org/10.1046/j.1365-2648.2002.02057.x. [DOI] [PubMed] [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, Briggs-Gowan MJ. Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(1):18–26. doi: 10.1097/00004583-200101000-00012. http://dx.doi.org/10.1097/00004583-200101000-00012. [DOI] [PubMed] [Google Scholar]
- Chesluk BJ, Bernabeo E, Hess B, Lynn LA, Reddy S, Holmboe ES. A new tool to give hospitalists feedback to improve interprofessional teamwork and advance patient care. Health Affairs. 2012;31(11):2485–2492. doi: 10.1377/hlthaff.2011.0611. http://dx.doi.org/10.1377/hlthaff.2011.0611. [DOI] [PubMed] [Google Scholar]
- Craig J, Glick C, Phillips R, Hall S, Smith J, Browne J. Recommendations for involving the family in developmental care of the NICU baby. Journal of Perinatology. 2015;35:S5–S8. doi: 10.1038/jp.2015.142. http://dx.doi.org/10.1038/jp.2015.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichner JM, Johnson BH. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404. doi: 10.1542/peds.2011-3084. http://dx.doi.org/10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- Epstein E, Sherman J, Blackman A, Sinkin RA. Testing the feasibility of skype and facetime updates with parents in the neonatal intensive care unit. American Journal of Critical Care. 2015;24(4):290–296. doi: 10.4037/ajcc2015828. http://dx.doi.org/10.4037/ajcc2015828. [DOI] [PubMed] [Google Scholar]
- Feeley N, Zelkowitz P, Cormier C, Charbonneau L, Lacroix A, Papageorgiou A. Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit. Applied Nursing Research. 2011;24(2):114–117. doi: 10.1016/j.apnr.2009.04.004. http://dx.doi.org/10.1016/j.apnr.2009.04.004. [DOI] [PubMed] [Google Scholar]
- Globus O, Leibovitch L, Maayan-Metzger A, Schushan-Eisen I, Morag I, Mazkereth R, … Strauss T. The use of short message services (SMS) to provide medical updating to parents in the NICU. Journal of Perinatology. 2016;36:739–743. doi: 10.1038/jp.2016.83. http://dx.doi.org/10.1038/jp.2016.83. [DOI] [PubMed] [Google Scholar]
- Gray JE, Safran C, Davis RB, Pompilio-Weitzner G, Stewart JE, Zaccagnini L, Pursley D. Baby CareLink: Using the internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000;106(6):1318–1324. doi: 10.1542/peds.106.6.1318. http://dx.doi.org/10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- Gund A, Sjoqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. Neonatal Intensive Care. 2013;26(4):42–50. doi: 10.1186/1472-6947-13-22. http://dx.doi.org/10.1186/1472-6947-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Joshi A, Chyou PH, Tirmizi Z, Gross J. Web camera use in the neonatal intensive care unit: Impact on nursing workflow. Clinical Medicine & Research. 2016;14(1):1–6. doi: 10.3121/cmr.2015.1286. http://dx.doi.org/10.3121/cmr.2015.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kersting A, Dorsch M, Wesselmann U, Ludorff K, Witthaut J, Ohrmann P, … Arolt V. Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. Journal of Psychosomatic Research. 2004;57(5):473–476. doi: 10.1016/j.jpsychores.2004.03.011. http://dx.doi.org/10.1016/j.jpsychores.2004.03.011. [DOI] [PubMed] [Google Scholar]
- Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the neonatal intensive care unit (NICU) Journal of Clinical Psychology in Medical Settings. 2010;17(3):230–237. doi: 10.1007/s10880-010-9202-7. http://dx.doi.org/10.1007/s10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- Lindberg B, Axelsson K, Ohrling K. Experience with videoconferencing between a neonatal unit and the families’ home from the perspective of certified paediatric nurses. Journal of Telemedicine and Telecare. 2009a;15(6):275–280. doi: 10.1258/jtt.2009.090112. http://dx.doi.org/10.1258/jtt.2009.090112. [DOI] [PubMed] [Google Scholar]
- Lindberg B, Axelsson K, Öhrling K. Taking care of their baby at home but with nursing staff as support: The use of videoconferencing in providing neonatal support to parents of preterm infants. Journal of Neonatal Nursing. 2009b;15(2):47–55. http://dx.doi.org/10.1016/j.jnn.2009.01.004. [Google Scholar]
- Luxton D, Mishkind M, Crumpton R, Ayers T, Mysliwiec C. Usability and feasibility of smartphone video capabilities for telehealth care in the U.S. military. Telemedicine and E-Health. 2012;18(6):409–412. doi: 10.1089/tmj.2011.0219. http://dx.doi.org/10.1089/tmj.2011.0219. [DOI] [PubMed] [Google Scholar]
- Manser T. Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica. 2009;53(2):143–151. doi: 10.1111/j.1399-6576.2008.01717.x. http://dx.doi.org/10.1111/j.1399-6576.2008.01717.x. [DOI] [PubMed] [Google Scholar]
- Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. Journal of Developmental and Behavioral Pediatrics. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. http://dx.doi.org/10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- Nicol-Harper R, Harvey AG, Stein A. Interactions between mothers and infants: Impact of maternal anxiety. Infant Behavior & Development. 2007;30(1):161–167. doi: 10.1016/j.infbeh.2006.08.005. http://dx.doi.org/10.1016/j.infbeh.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterman MJ, Martin JA, Mathews TJ, Hamilton BE. Expanded data from the new birth certificate, 2008. National Vital Statistics Reports. 2011;59(7):1–28. [PubMed] [Google Scholar]
- Penticuff JH, Arheart KL. Effectiveness of an intervention to improve parent–professional collaboration in neonatal intensive care. Journal of Perinatal and Neonatal Nursing. 2005;19(2):187–202. doi: 10.1097/00005237-200504000-00016. http://dx.doi.org/10.1097/00005237-200504000-00016. [DOI] [PubMed] [Google Scholar]
- Picker Institute. Improving the quality of health care through the eyes of patients: Surveys. 2000 [No longer available from www.picker.org http://www.pickereurope.org/wp-content/uploads/2014/10/Parents-experiences-of-neonatal-care...pdf. European version retrieved from.
- Piecuch RE, Roth RS, Clyman RI, Sniderman SH, Riedel PA, Ballard RA. Videophone use improves maternal interest in transported infants. Critical Care Medicine. 1983;11(8):655–656. doi: 10.1097/00003246-198308000-00014. http://dx.doi.org/10.1097/00003246-198308000-00014. [DOI] [PubMed] [Google Scholar]
- Ramezani T, Hadian Shirazi Z, Sabet Sarvestani R, Moattari M. Family-centered care in neonatal intensive care unit: A concept analysis. International Journal of Community Based Nursing and Midwifery. 2014;2(4):268–278. [PMC free article] [PubMed] [Google Scholar]
- Rhoads SJ, Green A, Gauss CH, Mitchell A, Pate B. Web camera use of mothers and fathers when viewing their hospitalized neonate. Advances in Neonatal Care. 2015;15(6):440–446. doi: 10.1097/ANC.0000000000000235. http://dx.doi.org/10.1097/ANC.0000000000000235. [DOI] [PubMed] [Google Scholar]
- Rhoads SJ, Green A, Mitchell A, Lynch CE. Neuro-protective core measure 2: Partnering with families—Exploratory study on web-camera viewing of hospitalized infants and the effect on parental stress, anxiety, and bonding. Newborn & Infant Nursing Reviews. 2015;15(3):104–110. http://dx.doi.org/10.1053/j.nainr.2015.06.011. [Google Scholar]
- Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for post-partum depression and anxiety before discharge. Journal of Perinatology. 2013;33(3):171–176. doi: 10.1038/jp.2012.75. http://dx.doi.org/10.1038/jp.2012.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw RJ, Bernard RS, Storfer-Isser A, Rhine W, Horwitz SM. Parental coping in the neonatal intensive care unit. Journal of Clinical Psychology in Medical Settings. 2013;20(2):135–142. doi: 10.1007/s10880-012-9328-x. http://dx.doi.org/10.1007/s10880-012-9328-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger D, Gorsuch R, Lushene R. The STAI manual. Palo Alto, CA: Consulting Psychologists; 1977. [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, … Thacker SB. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Journal of the American Medical Association. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. http://dx.doi.org/10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Stubblefield C, Murray RL. Parents call for concerned and collaborative care. Western Journal of Nursing Research. 1999;21(3):356–371. doi: 10.1177/01939459922043929. [DOI] [PubMed] [Google Scholar]
- Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: A preliminary study. Journal of Developmental & Behavioral Pediatrics. 2009;30(1):50–56. doi: 10.1097/DBP.0b013e318196b0de. http://dx.doi.org/10.1097/DBP.0b013e318196b0de. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Knafl K. The integrative review: Updated methodology. Journal of Advanced Nursing. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. http://dx.doi.org/10.1111/j.1365-2648.2005.03612.x. [DOI] [PubMed] [Google Scholar]
- Wigert H, Dellenmark MB, Bry K. Strengths and weaknesses of parent–staff communication in the NICU: A survey assessment. BMC Pediatrics. 2013;13:71. doi: 10.1186/1471-2431-13-71. http://dx.doi.org/10.1186/1471-2431-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward LJ, Bora S, Clark CA, Montgomery-Hönger A, Pritchard VE, Spencer C, Austin NC. Very pre-term birth: Maternal experiences of the neonatal intensive care environment. Journal of Perinatology. 2014;34(7):555–561. doi: 10.1038/jp.2014.43. http://dx.doi.org/10.1038/jp.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo C, Ho SK, Khong K, Lau Y. Virtual visitation in the neonatal intensive care: Experience with the use of internet and telemedicine in a tertiary neonatal unit. The Permanente Journal. 2011;15(3):32–36. doi: 10.7812/tpp/11-063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngblut JM, Brooten D, Cantwell GP, del Moral T, Totapally B. Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics. 2013;132(5):e1295–e1301. doi: 10.1542/peds.2013-1194. http://dx.doi.org/10.1542/peds.2013-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelkowitz P, Na S, Wang T, Bardin C, Papageorgiou A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatrica. 2011;100(5):700–704. doi: 10.1111/j.1651-2227.2010.02128.x. http://dx.doi.org/10.1111/j.1651-2227.2010.02128.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.