Abstract
Cognitive deficits are prominent features of the ultra-high risk state for psychosis that are known to impact functioning and course of illness. Cognitive remediation appears to be the most promising treatment approach to alleviate the cognitive deficits, which may translate into functional improvements. This study systematically reviewed the evidence on the effectiveness of cognitive remediation in the ultra-high risk population. The electronic databases MEDLINE, PsycINFO, and Embase were searched using keywords related to cognitive remediation and the UHR state. Studies were included if they were peer-reviewed, written in English, and included a population meeting standardized ultra-high risk criteria. Six original research articles were identified. All the studies provided computerized, bottom-up-based cognitive remediation, predominantly targeting neurocognitive function. Four out of five studies that reported a cognitive outcome found cognitive remediation to improve cognition in the domains of verbal memory, attention, and processing speed. Two out of four studies that reported on functional outcome found cognitive remediation to improve the functional outcome in the domains of social functioning and social adjustment. Zero out of the five studies that reported such an outcome found cognitive remediation to affect the magnitude of clinical symptoms. Research on the effect of cognitive remediation in the ultra-high risk state is still scarce. The current state of evidence indicates an effect of cognitive remediation on cognition and functioning in ultra-high risk individuals. More research on cognitive remediation in ultra-high risk is needed, notably in large-scale trials assessing the effect of neurocognitive and/or social cognitive remediation on multiple outcomes.
Introduction
During the last two decades there have been a surge of studies into the putative prodromal phase of psychosis commonly termed “the ultra-high risk state for psychosis” (UHR) or “the clinical high risk state”. This way of prospectively identifying individuals at heightened risk for psychosis serves as the foundation for intervention studies aimed at avoiding, ameliorating, or delaying progression to psychosis. Furthermore, initiating appropriate treatment as early as possible has the potential of improving both the clinical and functional heterogeneous outcome1 of UHR individuals.2
Cognitive deficits are prominent features of the UHR state that have received increased attention in the research field. The most recent meta-analysis on the subject found an overall impairment in neurocognition compared with healthy controls to have an effect size of Hedges’ g = −0.34, 95% CI: −0.43 to −0.26, with the greatest impairments found in the domains of visual and verbal memory.3 Moreover, evidence indicates that neurocognitive functioning can be predictive of transition to psychosis, as poorer neurocognitive functioning in the domains of verbal fluency, verbal and visual memory, and working memory have been found to be characteristic of those that develop psychosis compared with those that do not.4–10 Social cognitive deficits have also been identified in UHR individuals with meta-analytical evidence of a moderate overall effect size (Cohen’s d = −0.52, 95% Cl = −0.38 to −0.65).11 Studies investigating the relationship between social cognitive deficits and conversion to psychosis report mixed results, with some finding deficits in theory of mind and deficits in affect recognition/discrimination being predictive of conversion to psychosis in UHR samples,12, 13 while others do not find social cognitive deficits to be predictive of psychosis development.14–20 The magnitude of the neurocognitive and social cognitive deficits have been found to be intermediate between that of healthy controls and patients with established psychosis.3, 11, 21, 22
Neurocognitive deficits have a significant impact on UHR individuals’ level of functioning. In cross-sectional studies the association between neurocognitive deficits and poor role and social functioning in UHR has been identified in the areas of verbal learning and memory,23, 24 working memory,25 processing speed,26, 27 reasoning and problem solving,23, 27 and global neurocognition.28 In longitudinal studies, poor functional outcome has been linked to deficits in processing speed,29, 30 verbal learning and memory,24, 29 executive function and disorganized symptoms,31 and global neurocognitive performance.27 Although far fewer studies have been conducted on the association between social cognition and functioning, early evidence indicate that aspects of social cognition, such as theory of mind,28, 32, 33 emotion recognition,33, 34 and attributional bias33 are associated with poor functioning cross-sectionally.
As the abovementioned evidence indicates, cognitive deficits place significant impact on the course of illness and functional outcome of UHR individuals, which parallels findings from patients with established psychosis.35–37 Consequently, it seems essential to search for treatments that may alleviate the cognitive deficits and improve the functional outcome of UHR individuals. Cognitive remediation is a promising treatment approach aimed at reducing cognitive deficits and improving functioning in the UHR state. Cognitive remediation can be defined as “a behavioral training based intervention that aims at improving cognitive processes (attention, memory, executive function, social cognition or metacognition) with the goal of durability and generalization”.38 There is abundant evidence for the effectiveness of cognitive remediation in patients with schizophrenia. The most recent meta-analysis on the subject demonstrates moderate effect sizes of cognitive remediation on both global cognition (effect size 0.45, 95% CI = 0.31–0.59) and functioning (effect size 0.42, 95% CI = 0.22–0.62) at post-treatment, along with a small effect size on symptomatology (effect size 0.18, 95 CI = 0.03–0.32). Moreover, the effect of cognitive remediation on global cognition and functioning appears to be durable, as the follow-up analyses revealed effect sizes for global cognition to be 0.43, 95% CI = 0.18–0.67, and the effect size for functioning to be 0.37, 95% CI = 0.11 to 0.64, albeit no significant effect on symptoms could be found at follow-up.38 In contrast to numerous reviews and meta-analyses on the effectiveness of cognitive remediation in patients with established psychosis,39–44 no systematic review has yet been conducted assessing the effect of cognitive remediation on cognition, functioning, symptomatology, and psychosis prevention in the UHR state. Knowing that the cognitive deficits are already evident in the UHR state for psychosis, it can be hypothesized that the cognitive deficits may be more amenable to treatment at this early stage of illness, with the potential of greater brain plasticity,45 than at more chronic stages. Additionally, cognitive remediation interventions are effective for adolescents and young adults generally,46 and evidence indicate changes in cognition to be related to functional improvements in UHR individuals.30 Consequently, targeting cognitive dysfunctions in the UHR state for psychosis may be the optimal time to intervene when aiming at improving cognition, functioning, and quality of life of the UHR individuals.
The current study aimed at reviewing the evidence for the effectiveness of cognitive remediation on cognition, functional outcome, clinical symptoms, and psychosis prevention in the UHR population.
Results
The literature search resulted in 107 original articles. Out of these, six met the eligibility criteria. Figure 1 illustrates the study selection and exclusion process.
Fig. 1.
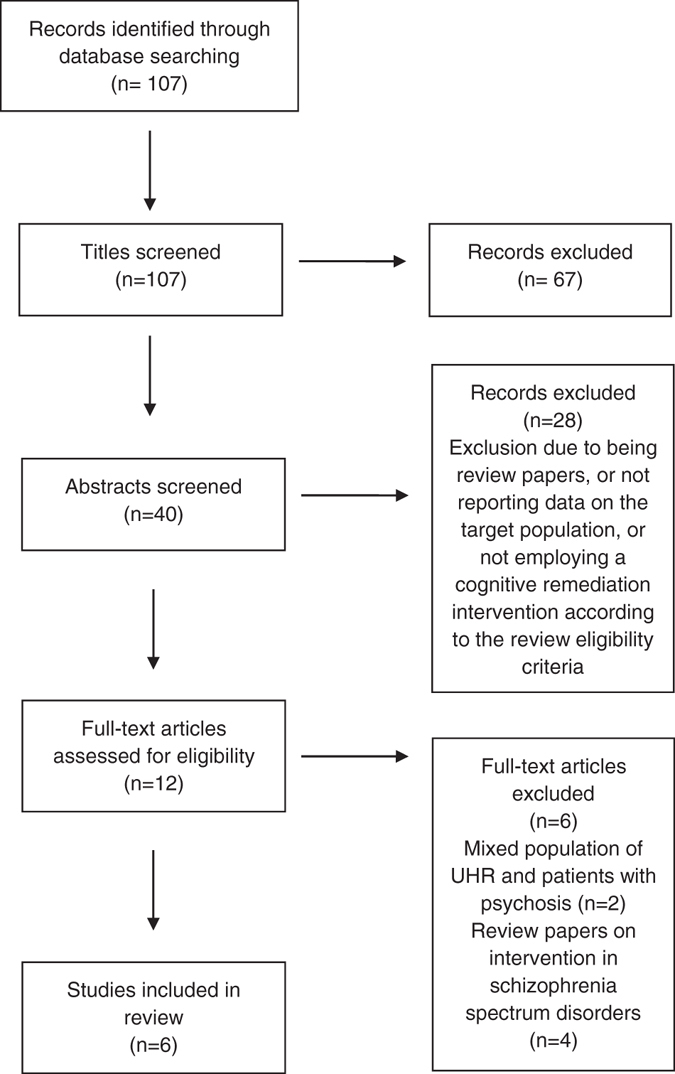
PRISMA flow diagram
All of the six studies offered cognitive remediation within a restorative approach47 as opposed to a compensatory approach,48 and used computer-based drill-and-practice training programs. This treatment approach can also be conceptualized within a bottom-up based training framework, in which the cognitive remediation targets lower level cognitive processes,49 opposed to a top-down-based training approach that emphasizes training of higher order cognitive functions (e.g., problem solving and complex memory strategies).50, 51
One study52 offered cognitive remediation as part of a broad integrated treatment program, and another study53 offered a combined neurocognitive and social cognitive remediation program, while the last four studies offered neurocognitive remediation exclusively. In two of the trials,54, 55 the cognitive remediation consisted of targeted auditory training used in the Brain Fitness program (http://www.brainhq.com). The computer exercises employed in the studies were designed to improve speed and accuracy of auditory information processing while engaging auditory and verbal working memory. Two other studies52, 56 used the computerized digital training software from the Cogpack training program (http://www.markersoftware.com), which comprises training of the cognitive domains of attention, memory, and executive function. One study specifically targeted processing speed using the Processing Speed Training (PST) program developed by Jimmy Choi.57 This tablet-based, targeted training of processing speed ability intends at strengthening or resuscitating neuroanatomical connections linked to processing speed. Moreover, the intervention comprised pupillometric neurofeedback techniques that were employed to enhance and adjust the cognitive training by giving immediate biofeedback to the training software enabling it to automatically adjust the training exercises. The PST program draws on motivational theories of learning, and aims at promoting intrinsic motivation when doing cognitive remediation. Finally, the study employing both neurocognitive and social cognitive remediation53 used computer exercises from the Lumosity program (http://www.lumosity.com) that targeted processing speed, memory, attention, flexibility, and problem solving. The social cognitive training was done according to the SocialVille (http://www.positscience.com) training program addressing key social cognitive deficits such as social perception, emotion recognition, and theory of mind. The cognitive remediation in the studies relied predominantly on participants doing individual cognitive training, and did not include specific strategy training, or targeted training elements aiming at transferring the effect of the group training to the participants’ daily life. Table 1 displays study details and outcomes. No studies had a low risk of bias, but the risk of bias demonstrated to be lower in the randomized controlled trials (RCTs).
Table 1.
Cognitive remediation studies in the UHR population
| Study | Country | UHR sample (N) | Mean agea | UHR criteria | Experimental condition | Study design | Effect of cognitive remediation | Risk of bias |
|---|---|---|---|---|---|---|---|---|
| Bechdolf et al. (2012) | Germany | N = 1283% attrition rate | 26.0 | Basic symptoms (EIPS criteria) | Integrated psychological intervention: Cognitive remediation (Cogpack), cognitive behavioral therapy, skills training, psychoeducational multi-family groups12 sessions | RCT: 63 UHR in Integrated psychological intervention65 UHR in supportive counseling | Reduced rate of conversion to psychosis at 12-month and 24-month: 12-month:3.2 vs. 16.9%, p = .00824-month: 6.3 vs. 20.0%, p = .019 | Selection bias: Low Performance bias: HighDetection bias: UnclearAttrition bias: LowIntention to treat: HighReporting bias: High |
| Piskulic et al. (2015) | USA | N = 3248% attrition rate | 18.61 | SIPS | Neurocognitive, computerized training program (Brain Fitness)40 h of cognitive training | RCT: 18 UHR in targeted cognitive remediation14 UHR doing computer games. | Improvement in social functioning (GF:Social) (t(28) = −3.26, p < .05) between baseline and 9-months follow-up, d = 3.09Trending improvement in speed of processing between baseline and 9-months follow-up (t(29) = −2.91, p = .06 and between post-intervention and 9-months follow-up (t(29) = −2.99, p < .05)(MCCB)No improvements in cognition or clinical symptoms | Selection bias: LowPerformance bias: HighDetection bias: LowAttrition bias: HighIntention to treat: LowReporting bias: Low |
| Loewy et al. (2016) | USA | N = 8338% attrition rate | 18.25 | SIPS | Neurocognitive, computerized training program (Brain Fitness)Participants asked to complete 2040 h of training | RCT:50 UHR in targeted cognitive remediation 33 UHR doing computer games. | Significant improvement in verbal memory (effect size d = .61). Hopkins verbal learning testrevisedNo improvements in functional outcome or clinical symptoms | Selection bias: LowPerformance bias: LowDetection bias: LowAttrition bias: HighIntention to treat: LowReporting bias: Low |
| Choi et al. (2016) | USA | N = 6210% attrition rate | 18.35 | SIPS | Neurocognitive training program (PST)30 h of training | RCT:30 UHR in PST32 UHR in active control group | Post-treatment: Significant improvements in processing speed: Digit symbol coding (p = 0.03, d = 0.50)4-month follow-up: Significant improvements in processing speed: Digit symbol coding (p = 0.01, d = 0.84).Significant improvements on self-report social adjustment (SAS-SR) p = 0.01, d = 1.04No improvements in clinical symptoms | Selection bias: LowPerformance bias: LowDetection bias: LowAttrition bias: LowIntention to treat: UnclearReporting bias: Low |
| Rauchensteiner et al. (2011) | Germany | N = 10Attrition rate not reported | 27.2 | Basic symptoms (the Revised Bonn Scale for the Assessment of Basic Symptoms)SIPS criteria of: 1. Attenuated psychotic symptoms 2. Brief limited intermittent psychotic symptoms | Neurocognitive, computerized training program (Cogpack)10 sessions | Cohort study: 10 UHR16 Patients with schizophrenia | Improvementin long-term memory function and attention at post-treatmentRey-Auditory Verbal Learning Test (German version) (VLMT) D6 improvement from 10.0813.9, p = 0.01), d = 1.23Continuous Performance Test (CPT-IP) Shapes Improvement from 0.730.81, p = 0.04, d = 0.69No improvement in clinical symptoms | SelectioncComparabilitycOutcomeb |
| Hooker et al. (2014) | USA | N = 1217% attrition rate | 21.9 | SIPS | Neurocognitive and social cognitive computerized training programs (Lumosity and SocialVille)40 h of cognitive training | Cohort study:14 UHR 14 healthy controls(performing as baseline reference on cognitive tests) | Significant improvements in processing speed (p = .01, d = .63) at post-treatmentTrending improvements in visual learning and memory (p = .06, d = .54), and global cognition (p = .06, d = .45)(MCCB)No improvements in functional outcome or clinical symptoms | SelectioncComparabilitycOutcome |
UHR ultra-high risk patients, HC healthy controls, SIPS the Structured Interview for Prodromal Symptoms, EIPS early initial prodromal state, RCT randomized controlled trial, MCCB MATRICS consensus cognitive battery, GF:Social Global functioning Social Scale
Risk of bias in the RCTs have been assessed according to the Cochrane criteria, with the categories of low risk of bias, high risk of bias, or unclear risk of bias
Risk of bias in the cohort studies have been assessed according to the NOS, in which a study can achieve a maximum of four stars within the Selection category, two stars within the Comparability category, and three stars within the Outcome category
a UHR patients mean age at baseline
b The attrition rate is reported as the proportion of the individuals in the intervention group discontinuing treatment
c d = Cohens d. Effect sizes for significant between-group or within group improvements have been highlighted
Noteworthy, the study by Bechdolf et al. (2012) only reported data on transition to psychosis, and use of antidepressants, even though the registration of the trial at clinicaltrials.gov (NCT00204087) indicate that improvements in prodromal symptoms and social adjustment were secondary outcomes of the trial. This lack of reporting of secondary outcomes may indicate a reporting bias and precludes using the study to assess the effect of the intervention on functional and symptomatological outcomes.
Effect on cognition
Five of the six studies reported the effect of cognitive remediation on cognition. Three of them were described as pilot studies (with two cohort studies), while the last two were double-blinded RCTs. All, except one study,54 found a beneficial effect of cognitive remediation on cognition with improvements in the domains of attention, processing speed, and memory functions. A significant improvement in verbal memory was found at post-treatment in a double-blind RCT by Loewy et al. (2016) in the group of UHR individuals receiving targeted cognitive training compared to an active control group.55 Improvements in processing speed were found at post-treatment, and 4-month follow-up, in a double blind RCT by Choi et al. (2016) in the group of individuals receiving targeted cognitive remediation compared to an active control group (Choi et al. 2016). Likewise, significant improvements in processing speed at post-treatment were found in a cohort study by Hooker et al. that offered cognitive remediation to a group of UHR individuals, however, the study did not include a control group. Noteworthy, the study found the improvements in processing speed to be associated with gains in role functioning.53 In line with the findings in the RCT by Loewy et al. (2016), a cohort study by Rauchensteiner et al. (2011) reported improvements in long-term memory functions, along with improvements in attention, in UHR individuals relative to patients with schizophrenia undergoing the same cognitive remediation program.56 Contrary to these positive findings on the effect of cognitive remediation on cognition, a pilot study by Piskulic et al. (2015) did not find cognitive remediation to have a significant effect on cognition at post-treatment or at 9-month follow-up. However, the study did report a statistically non-significant tendency towards improvement in speed of processing between baseline and 9-month follow-up.54 Noteworthy, the only study employing social cognitive remediation in combination with neurocognitive remediation did not assess the effect of this cognitive remediation approach on social cognitive outcomes.
Effect on functional outcome
Four of the six studies evaluated the effect of cognitive remediation on functional outcomes. Two of the studies found a beneficial effect of cognitive remediation on aspects of functioning (social functioning and self-report social adjustment). In the double-blind RCT by Choi et al. (2016), lower scores on a self-report social maladjustment scale were found in participants in the intervention group compared to the active controls at 4-month follow-up. Significant improvements in social functioning between baseline and 9-month follow-up were found in the pilot study by Piskulic et al. (2015). Loewy et al. (2016) did not find an effect of cognitive remediation on either measures of global functioning, or measures of social and role functioning in their double-blind RCT. Likewise, Hooker et al. (2014) failed to find a significant effect of cognitive remediation on social and role functioning in their cohort study.
Effect on clinical symptoms
The effects of cognitive remediation on clinical symptoms were assessed in five out of the six studies, but none of the studies reported a beneficial effect of cognitive remediation on clinical symptoms. This lack of a significant effect was seen in regard to positive and negative symptoms,53, 55, 56 and disorganized and general symptoms in both double-blinded RCTs and cohort studies.53, 55 Lack of significant effect was seen in regard to depressive symptoms in a double-blind RCT.57
Effect on preventing transition to psychosis
The only trial evaluating the effect of cognitive remediation on transition to psychosis was a large scale trial conducted by Bechdolf et al. (2012). The active intervention in the trial comprised four treatment modalities: cognitive behavioral therapy, skills training, psychoeducational multi-family groups, and cognitive remediation. The study found a beneficial effect of the integrated intervention, compared to supportive counseling, in reducing the rate of transition to psychosis at 12-month follow-up and at 24-month follow-up,52 but as the experimental intervention was an integrated intervention, it is not possible to evaluate the separate effect of the cognitive remediation.
Discussion
This is the first systematic review focusing exclusively on cognitive remediation in the UHR population. As the results from the six published studies indicate, there is some evidence for the effectiveness of cognitive remediation in the UHR population as a means to enhance cognition and improve functional outcome. Two of the three RCTs assessing the specific effect of cognitive remediation in the UHR state, found the cognitive remediation to have a beneficial effect on cognition in the domains of verbal memory and processing speed. The two cohort studies conducted found a beneficial effect of cognitive remediation in the cognitive domains of memory, attention, and processing speed. Moreover, two out of three RCTs that assessed gains in functional outcome, reported improvements in functional outcome in the domains of social function and self-report social adjustment as a result of a neurocognitive remediation program. One of the studies reporting a beneficial effect of cognitive remediation on functional outcome was a methodologically rigorous, double-blind RCT demonstrating a low risk of bias,57 while the other was a pilot study.54 The RCT not finding a significant effect on outcome does suffer the methodological limitation of having a high attrition rate.55 No effect on functional outcome was reported in the one cohort study assessing this outcome.
None of the studies found a significant effect of cognitive remediation in regard to clinical symptoms (i.e., positive, negative, disorganized, general, or depressive symptoms). It is not possible to assess the effect of cognitive remediation on preventing transition to psychosis, since the only study addressing this issue offered cognitive remediation as a part of an integrated treatment, precluding any conclusions to be drawn regarding the separate effect of the cognitive remediation on psychosis prevention. The two largest studies conducted to date by Loewy et al. (2016) and Choi et al. (2016), which have assessed the direct effect of cognitive remediation in the UHR population, are strengthened by being RCTs with a low risk of bias. These studies both show encouraging results regarding the effect of cognitive remediation on cognition, and on functional outcome in one of the studies. However, it must be emphasized that the evidence level is still low, as the effect of cognitive remediation in the UHR population has not been thoroughly investigated at this stage. The remaining studies reviewed were pilot studies with small sample sizes, and thus they may have been statistically underpowered to detect significant effects of the cognitive remediation. Moreover, it must be emphasized that two studies were cohort studies, lacking a control group, which may raise concerns about the risk of bias. Speculating, it may be that the equivocal findings on the effectiveness of cognitive remediation on functional outcome and symptoms may be due to the assessments being carried out too early to see a strong effect in these domains, as evidence from patients with schizophrenia suggest that functional and symptomatological improvements of cognitive remediation may manifest themselves over the longer-term (e.g., 6-month follow-up).58 This underlines the need for long-term follow-up of cognitive remediation studies in the UHR population.
It is noteworthy, that only three of the studies; the RCT by Choi et al. (2016), the RCT by Bechdolf et al. (2012), and the cohort study by Rauschensteiner et al. (2011) delivered the cognitive remediation as a group-based training. Additionally, in the Choi et al. (2016) study, the group-based approach included a facilitator being present in the group sessions to assist participants in case of questions (e.g., on loading the remediation program, or explaining how the computer exercises work). In the remaining three studies, the cognitive remediation was done individually at the participants’ home, or at the research facility, with no or minimal support offered by a facilitator. As mentioned in the Result section, all the studies offered cognitive remediation within a bottom-up training-based framework targeting basic cognitive processes. This suggests the need for future studies investigating the effect of top-down-based approaches to cognitive remediation, which have been found to result in cognitive and functional gains in patients with schizophrenia.59 All the studies offered a cognitive training dose of 20–40 h, except the studies by Bechdolf et al. and Rauschensteiner et al. offering 12 and 10 h of training, respectively. It may be speculated that these delivery characteristics of the cognitive remediation may have influenced the equivocal results that was achieved, although evidence from patients with schizophrenia indicate that the differences in the delivery of the cognitive remediation do not seem to be critical to the benefit of the cognitive remediation on cognitive outcome.38, 39
Evidence suggests motivational deficits to be central features of schizophrenia spectrum disorders,60, 61 that may critically affect the ability to engage in and benefit from cognitive remediation.62 Hence, it may be essential to address motivational aspects directly (e.g., using motivational interviewing, motivational booster meetings, or cognitive remediation programs, such as the Neuropsychological and Educational Approach to Remediation model designed to target intrinsic motivation51) when doing cognitive remediation in a UHR population. Motivational aspects were addressed in the trial by Choi et al. (2016) that notably demonstrated a rather low attrition rate compared to other cognitive remediation trials in the UHR population showing high attrition rates.54, 55 This high attrition rate in many of the trials constitutes an important bias when interpreting the effectiveness of the cognitive remediation programs. This also points to the need for the development of new ways of delivering cognitive remediation that are engaging for the participants as this is essential for the feasibility and scalability of cognitive remediation programs in clinical practice.
Additionally, meta-analytical evidence from patients with schizophrenia indicate that an enhanced effect of cognitive remediation can be achieved when provided in the context of psychiatric rehabilitation.38 This suggests the need to offer cognitive remediation along with other treatment modalities to maximize the effect on outcome.52
Only one of the trials reviewed offered social cognitive remediation in addition to neurocognitive remediation, but did not include any social cognitive outcome measure, which precludes any conclusions to be drawn on the effect of cognitive remediation on social cognitive function. Social cognition has been found to be highly impaired in UHR individuals,11, 21 and social cognition may be proximal to the functioning of UHR individuals,32–34 and patients with schizophrenia.63 Evidence from patients with schizophrenia points to the beneficial effect of social cognitive remediation on both social cognitive function and functional outcome.64 Hence, there is a need for remediation studies targeting social cognitive function in UHR individuals. Given that both neurocognition and social cognition are impaired in UHR individuals it may be speculated that a combined treatment approach may enhance the effect on outcome. Beneficial results of such combined treatment approaches have been found in patients with schizophrenia with improvements seen in relation to both neurocognition, social cognition, functional outcome, and symptomatology.65, 66
Methodological considerations
A strength of the review is that a high effort was put into identifying studies meeting the eligibility criteria by contacting numerous key researchers in the area, in addition to the systematic literature search. That did not result in any additional studies being identified, indicating that the literature search had been optimal. Moreover, the studies reviewed used related computer-based training programs, aimed at restoring cognitive function, which enhances the comparability. An additional strength is that risk of bias in the studies reviewed were assessed according to the well-defined criteria of the Newcastle–Ottawa Scale (NOS) for cohort studies, and the Cochrane review criteria for RCTs. Limitations are that only very few studies have been conducted on the effect of cognitive remediation in the UHR state, and thus the results must be interpreted with caution. Moreover, the studies differed in the criteria used to identify UHR individuals, and on demographic parameters such as age and use of medication. Furthermore, the studies used different outcome assessments on cognition, functioning, and symptomatology, precluding a meta-analysis to be conducted on these outcomes.
Conclusion
To conclude, evidence is still scarce on the effectiveness of cognitive remediation in the UHR population, and more research is needed. The six studies published to date provide preliminary evidence for the effectiveness of cognitive remediation on cognition and aspects of functional outcome, but methodological considerations can be raised regarding the majority of studies, precluding any firm conclusions to be drawn. None of the studies reviewed deployed targeted social cognitive training, or assessed social cognitive function as an outcome. Hence, there is a need for methodologically rigorous trials that may not only confirm the abovementioned findings, but also provide additional evidence on the effectiveness of neurocognitive and/or social cognitive remediation on multiple aspects of cognitive outcome, functional outcome, clinical symptoms, along with the potential of preventing transition to psychosis. Additionally, future research is warranted into the effectiveness of cognitive remediation in conjunction with other treatment components in UHR populations (e.g., vocational rehabilitation, exercise, oxytocin) as it has been done in patients with established psychosis,67–70 as this treatment augmentation may enhance the effect on outcome.
Given that the UHR paradigm is proving useful in identifying help-seeking patients that may never develop a psychotic disorder, but are still troubled by functional deficits in the majority of cases,71 there is a need for safe and tolerable interventions in this population. This review suggests cognitive remediation to be a viable way to affect cognition and functional outcome, although many questions on its effectiveness still need to be answered.
Method
Study registration
The study adheres to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The protocol for the study was registered at PROSPERO international prospective register of systemic reviews (registration number CRD42016047980), before initiation of the literature search.
Search strategy
A literature search was conducted from inception until September 2016 in the electronic databases of MEDLINE, PsycINFO and Embase using the following words: (“at risk mental state” or “UHR” or “clinical high risk”, or “prodromal”, or “prodrome”, or “at risk psychosis”) and (“cognitive remediation”, or “cognitive rehabilitation”, or “cognitive training”).
Eligibility criteria
Articles were included if they provided cognitive remediation, or an intervention designed to enhance cognitive functioning,39 and used a clinical validated measure of the UHR state, i.e., the Comprehensive Assessment of At-Risk Mental States,72 the Structured Interview for Prodromal Symptoms (SIPS),73 or the basic symptoms approach [e.g., Early Initial Prodromal State (EIPS) criteria].74, 75 Studies were included irrespective of whether they included a control group or not. Both RCTs and cohort studies were included. While we acknowledge that it may be challenging to evaluate treatment effect in cohort studies, and that RCTs are considered the ideal way to evaluate treatment effect, we did include both RCTs and cohort studies in this review, as it intends to convey a preliminary description of the current evidence for the effectiveness of cognitive remediation in the UHR state. A primary emphasis when interpreting the results is, though, put on the results obtained from RCTs. Articles were excluded if they were in other languages than English, or did not report results separately for the UHR group. Four conference papers meeting the eligibility criteria of the review were identified. The authors of these papers were contacted to clarify if any publications on the data were underway. Moreover, numerous key researchers in the area were contacted to identify any potential, additional cognitive remediation studies approaching publication. That did not result in any additional papers being identified.
Risk of bias in the RCTs were assessed according to the Cochrane criteria,76 operating with the categories of low risk of bias, high risk of bias, or unclear risk of bias. Risk of bias is assessed in the areas of selection bias, performance bias, detection bias, attrition bias, and reporting bias. Selection bias is assessed based on information on biased allocation to interventions due to random sequence generation or allocation concealment. Performance and Detection bias is assessed based on information on partly blinding of participants or personnel during the study; and secondly blinding of outcome assessors. Attrition bias is evaluated based on amount, nature or handling of incomplete outcome data; and Reporting bias is concerned with the risk of selective outcome reporting. Other bias not addressed in the domain might be reported, if important concerns or specific questions might affect study quality.
Risk of bias in the cohort studies were assessed according to the NOS,77 which is recommended by the Cochrane Collaboration for assessing the quality of published non-randomized studies. NOS can be used as a checklist or scale, and contains eight items, categorized into three broad dimensions: the selection of study-groups, the comparability of groups; and the assessment of the outcome of interest. For each item, response options are provided. A star system is used to allow a semi-quantitative assessment of study quality, assigning up to a maximum of nine points for the least risk of bias (provided in the following manner: four stars within the Selection category, two stars within the Comparability category, and three stars within the Outcome category).
Acknowledgements
The authors would like to thank all the esteemed researchers worldwide for their essential contribution in identifying any possible impending studies on cognitive remediation in the UHR population. This work was supported by Mental Health Services in the Capital Region of Denmark; the research fund of the Capital Region of Denmark; TrygFonden (grant number ID 108119); The Danish Council for Independent Research (grant number DFF-4004-00314); and the Lundbeck Foundation Center for Clinical Intervention and Neuropsychiatric Schizophrenia Research, CINS (grant number R155-2013-16337). The funding source had no role in any aspect of the study.
Author contributions
L.B.G. conducted the literature search, wrote the first draft, and finalized the manuscript. C.H., T.D.K., C.A.D., and M.N. provided scientific support and assisted in the writing the manuscript and critical revision of the work. All authors contributed to and have approved the final manuscript.
Competing interests
The authors L.B.G., C.H., T.D.K., and M.N. are involved in an ongoing trial, the FOCUS trial78, that evaluates the effectiveness of cognitive remediation in the UHR population, but none of the researchers declare any competing interests.
References
- 1.Fusar-Poli P, et al. Predicting psychosis. Arch. Gen. Psychiatry. 2012;69:220–229. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- 2.McGorry PD, et al. Intervention in individuals at ultra-high risk for psychosis: a review and future directions. J. Clin. Psychiatry. 2009;70:1206–1212. doi: 10.4088/JCP.08r04472. [DOI] [PubMed] [Google Scholar]
- 3.Fusar-Poli P, et al. Cognitive functioning in prodromal psychosis. Arch. Gen. Psychiatry. 2012;69:562–571. doi: 10.1001/archgenpsychiatry.2011.1592. [DOI] [PubMed] [Google Scholar]
- 4.Brewer WJ, et al. Memory impairments identified in people at ultra-high risk for psychosis who later develop first-episode psychosis. Am. J. Psychiatry. 2005;162:71–78. doi: 10.1176/appi.ajp.162.1.71. [DOI] [PubMed] [Google Scholar]
- 5.Seidman L, Giuliano A, Walker E. Neuropsychology of the prodrome to psychosis in the NAPLS consortium. Arch. Gen. Psychiatry. 2010;67:578–588. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woodberry Ka, et al. Neuropsychological profiles in individuals at clinical high risk for psychosis: relationship to psychosis and intelligence. Schizophr. Res. 2010;123:188–198. doi: 10.1016/j.schres.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koutsouleris N, et al. Early recognition and disease prediction in the at-risk mental states for psychosis using neurocognitive pattern classification. Schizophr. Bull. 2012;38:1200–1215. doi: 10.1093/schbul/sbr037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riecher-Rössler A, et al. Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol. Psychiatry. 2009;66:1023–1030. doi: 10.1016/j.biopsych.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Becker HE, et al. Neurocognitive functioning before and after the first psychotic episode: does psychosis result in cognitive deterioration? Psychol. Med. 2010;40:1599–1606. doi: 10.1017/S0033291710000048. [DOI] [PubMed] [Google Scholar]
- 10.Pukrop R, et al. Neurocognitive indicators for a conversion to psychosis: comparison of patients in a potentially initial prodromal state who did or did not convert to a psychosis. Schizophr. Res. 2007;92:116–125. doi: 10.1016/j.schres.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 11.van Donkersgoed RJM, Wunderink L, Nieboer R, Aleman A, Pijnenborg GHM. Social cognition in individuals at ultra-high risk for psychosis: a meta-analysis. PLoS One. 2015;10:e0141075. doi: 10.1371/journal.pone.0141075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HS, et al. Social cognition and neurocognition as predictors of conversion to psychosis in individuals at ultra-high risk. Schizophr. Res. 2011;130:170–175. doi: 10.1016/j.schres.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 13.Corcoran CM, et al. Emotion recognition deficits as predictors of transition in individuals at clinical high risk for schizophrenia: a neurodevelopmental perspective. Psychol. Med. 2015;45:2959–2973. doi: 10.1017/S0033291715000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Healey KM, Penn DL, Perkins D, Woods SW, Addington J. Theory of mind and social judgments in people at clinical high risk of psychosis. Schizophr. Res. 2013;150:498–504. doi: 10.1016/j.schres.2013.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill KE, et al. Social inference in individuals at clinical high risk for psychosis. Early Interv. Psychiatry. 2016;10:77–80. doi: 10.1111/eip.12182. [DOI] [PubMed] [Google Scholar]
- 16.Stanford AD, Messinger J, Malaspina D, Corcoran CM. Theory of Mind in patients at clinical high risk for psychosis. Schizophr. Res. 2011;131:11–17. doi: 10.1016/j.schres.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Addington J, et al. Affect recognition in people at clinical high risk of psychosis. Schizophr. Res. 2012;140:87–92. doi: 10.1016/j.schres.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allott Ka, et al. Emotion recognition as a predictor of transition to a psychotic disorder in ultra-high risk participants. Schizophr. Res. 2014;153:25–31. doi: 10.1016/j.schres.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 19.Pinkham AE, Penn DL, Perkins DO, Graham KA, Siegel M. Emotion perception and social skill over the course of psychosis: a comparison of individuals ‘at-risk’ for psychosis and individuals with early and chronic schizophrenia spectrum illness. Cogn. Neuropsychiatry. 2007;12:198–212. doi: 10.1080/13546800600985557. [DOI] [PubMed] [Google Scholar]
- 20.Devylder JE, Ben-David S, Kimhy D, Corcoran CM. Attributional style among youth at clinical risk for psychosis. Early Interv. Psychiatry. 2013;7:84–88. doi: 10.1111/j.1751-7893.2012.00347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee TY, Hong S, Bin, Shin NY, Kwon JS. Social cognitive functioning in prodromal psychosis: a meta-analysis. Schizophr. Res. 2015;164:28–34. doi: 10.1016/j.schres.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Thompson A, et al. Social cognition in clinical ‘at risk’ for psychosis and first episode psychosis populations. Schizophr. Res. 2012;141:204–209. doi: 10.1016/j.schres.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Niendam TA, et al. Neurocognitive performance and functional disability in the psychosis prodrome. Schizophr. Res. 2006;84:100–111. doi: 10.1016/j.schres.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Lin A, et al. Neurocognitive predictors of functional outcome two to 13years after identification as ultra-high risk for psychosis. Schizophr. Res. 2011;132:1–7. doi: 10.1016/j.schres.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Goghari VM, et al. Spatial working memory ability in individuals at ultra high risk for psychosis. J. Psychiatr. Res. 2014;50:100–105. doi: 10.1016/j.jpsychires.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carrión RE, et al. Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am. J. Psychiatry. 2011;168:806–813. doi: 10.1176/appi.ajp.2011.10081209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer EC, et al. The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr. Bull. 2014;40:1452–1461. doi: 10.1093/schbul/sbt235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbato M, et al. Social cognition as a mediator between neurocognition and functional outcome in individuals at clinical high risk for psychosis. Schizophr. Res. 2013;150:542–546. doi: 10.1016/j.schres.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrión RE, et al. Prediction of functional outcome in individuals at clinical high risk for psychosis. JAMA Psychiatry. 2013;70:1133. doi: 10.1001/jamapsychiatry.2013.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niendam TA, et al. The course of neurocognition and social functioning in individuals at ultra high risk for psychosis. Schizophr. Bull. 2007;33:772–781. doi: 10.1093/schbul/sbm020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ali E, Jahshan C, Cadenhead KS. Disorganized Symptoms and Executive Functioning Predict Impaired Social Functioning in Subjects at Risk for Psychosis. J. Neuropsychiatry. Clin. Neurosci. 2011;23:457–460. doi: 10.1176/jnp.23.4.jnp457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cotter, J. et al. Examining the association between social cognition and functioning in individuals at ultra-high risk for psychosis. Aust. N. Z. J. Psychiatry doi:10.1177/0004867415622691 (2015). [DOI] [PubMed]
- 33.Glenthøj LB, et al. Social cognition in patients at ultra-high risk for psychosis. What is the relation to social skills and functioning? Schizophr. Res. Cogn. 2016;5:21–27. doi: 10.1016/j.scog.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amminger GP, et al. Affect recognition and functioning in putatively prodromal individuals. Schizophr. Res. 2013;147:404–405. doi: 10.1016/j.schres.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 36.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the ‘right stuff’? Schizophr. Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 37.Bellack aS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr. Bull. 1999;25:257–274. doi: 10.1093/oxfordjournals.schbul.a033377. [DOI] [PubMed] [Google Scholar]
- 38.Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. Am. J. Psychiatry. 2011;168:472–485. doi: 10.1176/appi.ajp.2010.10060855. [DOI] [PubMed] [Google Scholar]
- 39.Mcgurk S, Twamley E, Sitzer D, Mchugo G, Mueser K. Analysis of cognitive remediation in schizophrenia. Am. J. Psychiatry. 2007;164:1791–1802. doi: 10.1176/appi.ajp.2007.07060906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krabbendam L, Aleman A. Cognitive rehabilitation in schizophrenia: a quantitative analysis of controlled studies. Psychopharmacology (Berl.) 2003;169:376–382. doi: 10.1007/s00213-002-1326-5. [DOI] [PubMed] [Google Scholar]
- 41.Kurtz MM, Moberg PJ, Gur RC, Gur RE. Approaches to cognitive remediation of neuropsychological deficits in schizophrenia: a review and meta-analysis. Neuropsychol. Rev. 2001;11:197–210. doi: 10.1023/A:1012953108158. [DOI] [PubMed] [Google Scholar]
- 42.Twamley EW, Jeste DV, Bellack AS. A review of cognitive training in schizophrenia. Schizophr. Bull. 2003;29:359–382. doi: 10.1093/oxfordjournals.schbul.a007011. [DOI] [PubMed] [Google Scholar]
- 43.Grynszpan O, et al. Efficacy and specificity of computer-assisted cognitive remediation in schizophrenia: a meta-analytical study. Psychol. Med. 2011;41:163–173. doi: 10.1017/S0033291710000607. [DOI] [PubMed] [Google Scholar]
- 44.Pilling S, et al. Psychological treatments in schizophrenia: II. Meta-analyses of randomized controlled trials of social skills training and cognitive remediation. Psychol. Med. 2002;32:783–791. doi: 10.1017/s0033291702005640. [DOI] [PubMed] [Google Scholar]
- 45.Keshavan MS, Hogarty GE. Brain maturational processes and delayed onset in schizophrenia. Dev. Psychopathol. 1999;11:525–543. doi: 10.1017/S0954579499002199. [DOI] [PubMed] [Google Scholar]
- 46.Wexler BE, et al. Cognitive priming and cognitive training: immediate and far transfer to academic skills in children. Sci. Rep. 2016;6:32859. doi: 10.1038/srep32859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Medalia A, Choi J. Cognitive Remediation in Schizophrenia. Neuropsychol. Rev. 2009;19:353–364. doi: 10.1007/s11065-009-9097-y. [DOI] [PubMed] [Google Scholar]
- 48.Twamley EW, Burton CZ, Vella L. Compensatory cognitive training for psychosis: who benefits? who stays in treatment? Schizophr. Bull. 2011;37:55–62. doi: 10.1093/schbul/sbr059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fisher M, Holland C, Merzenich MM, Vinogradov S. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am. J. Psychiatry. 2009;166:805–811. doi: 10.1176/appi.ajp.2009.08050757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wykes T, Reeder C, Corner J, Williams C, Everitt B. The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophr. Bull. 1999;25:291–307. doi: 10.1093/oxfordjournals.schbul.a033379. [DOI] [PubMed] [Google Scholar]
- 51.Medalia, A., Revenheim, N., Herlands, T. Cognitive remediation for psychological disorders: therapist guide. (Oxford University Press, New York, 2009).
- 52.Bechdolf A, et al. Preventing progression to first-episode psychosis in early initial prodromal states. Br. J. Psychiatry. 2012;200:22–29. doi: 10.1192/bjp.bp.109.066357. [DOI] [PubMed] [Google Scholar]
- 53.Hooker CI, et al. A pilot study of cognitive training in clinical high risk for psychosis: Initial evidence of cognitive benefit. Schizophr. Res. 2014;157:314–316. doi: 10.1016/j.schres.2014.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Piskulic D, Barbato M, Liu L, Addington J. Pilot study of cognitive remediation therapy on cognition in young people at clinical high risk of psychosis. Psychiatry Res. 2015;225:93–98. doi: 10.1016/j.psychres.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 55.Loewy R, et al. Intensive auditory cognitive training improves verbal memory in adolescents and young adults at clinical high risk for psychosis. Schizophr. Bull. 2016;42:sbw009. doi: 10.1093/schbul/sbw009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rauchensteiner S, et al. Test-performance after cognitive training in persons at risk mental state of schizophrenia and patients with schizophrenia. Psychiatry Res. 2011;185:334–339. doi: 10.1016/j.psychres.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 57.Choi, J. et al. Pupillometer-Based Neurofeedback Cognitive Training to Improve Processing Speed and Social Functioning in Individuals at Clinical High Risk for Psychosis. Psychiatr. Rehabil. J. doi:10.1037/prj0000217 (2016). [DOI] [PMC free article] [PubMed]
- 58.Fisher M, Holland C, Subramaniam K, Vinogradov S. Neuroplasticity-based cognitive training in schizophrenia: an interim report on the effects 6 months later. Schizophr. Bull. 2010;36:869–879. doi: 10.1093/schbul/sbn170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Medalia A, Revheim N, Casey M. Remediation of problem-solving skills in schizophrenia: evidence of a persistent effect. Schizophr. Res. 2002;57:165–171. doi: 10.1016/S0920-9964(01)00293-6. [DOI] [PubMed] [Google Scholar]
- 60.Nakagami E, Hoe M, Brekke JS. The prospective relationships among intrinsic motivation, neurocognition, and psychosocial functioning in schizophrenia. Schizophr. Bull. 2010;36:935–948. doi: 10.1093/schbul/sbq043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schlosser DA, et al. Modeling the role of negative symptoms in determining social functioning in individuals at clinical high risk of psychosis. Schizophr. Res. 2015;169:204–208. doi: 10.1016/j.schres.2015.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Medalia, A. & Saperstein, A. The role of motivation for treatment success. Schizophr. Bull. 37, S122–S128 (2011). [DOI] [PMC free article] [PubMed]
- 63.Schmidt SJ, Mueller DR, Roder V. Social cognition as a mediator variable between neurocognition and functional outcome in Schizophrenia: empirical review and new results by structural equation modeling. Schizophr. Bull. 2011;37:S41–S54. doi: 10.1093/schbul/sbr079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kurtz MM, Gagen E, Rocha NBF, Machado S, Penn DL. Comprehensive treatments for social cognitive deficits in schizophrenia: a critical review and effect-size analysis of controlled studies. Clin. Psychol. Rev. 2016;43:80–89. doi: 10.1016/j.cpr.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 65.Eack SM, et al. Cognitive enhancement therapy for early course Schizophrenia: effects of a two-year randomized controlled trial. Psychiatr. Serv. 2009;60:1468–1476. doi: 10.1176/ps.2009.60.11.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roder, V., Mueller, D. R. & Schmidt, S. J. Effectiveness of integrated psychological therapy (IPT) for schizophrenia patients: a research update. Schizophr. Bull. 37, S71–S79 (2011). [DOI] [PMC free article] [PubMed]
- 67.Bell MD, Zito W, Greig T, Wexler BE. Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. Schizophr. Res. 2008;105:18–29. doi: 10.1016/j.schres.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 68.Davis MC, et al. Oxytocin-augmented social cognitive skills training in schizophrenia. Neuropsychopharmacology. 2014;39:2070–2077. doi: 10.1038/npp.2014.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Malchow B, et al. Effects of endurance training combined with cognitive remediation on everyday functioning, symptoms, and cognition in multiepisode schizophrenia patients. Schizophr. Bull. 2015;41:847–858. doi: 10.1093/schbul/sbv020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nuechterlein KH, et al. Enhancing cognitive training through aerobic exercise after a first Schizophrenia episode: Theoretical conception and pilot study. Schizophr. Bull. 2016;42:S44–S52. doi: 10.1093/schbul/sbw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fusar-Poli P, et al. At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry. 2015;14:322–332. doi: 10.1002/wps.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yung AR, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust. N. Z. J. Psychiatry. 2005;39:964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- 73.McGlashan, T., Walsh, B., Woods, S. The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-Up. (Oxford University Press, New York, 2010).
- 74.Hafner H, et al. Early detection and secondary prevention of psychosis: facts and visions. Eur. Arch. Psychiatry Clin. Neurosci. 2004;254:117–128. doi: 10.1007/s00406-004-0508-z. [DOI] [PubMed] [Google Scholar]
- 75.Bechdolf A, et al. Interventions in the initial prodromal states of psychosis in Germany: concept and recruitment. Br. J. Psychiatry Suppl. 2005;48:s45–s48. doi: 10.1192/bjp.187.48.s45. [DOI] [PubMed] [Google Scholar]
- 76.Higgins, J. & Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011)www.handbook.cochrane.org (2011).
- 77.Wells, G. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyseshttp://www.ohri.ca/programs (2011).
- 78.Glenthøj LB, et al. The FOCUS trial: cognitive remediation plus standard treatment versus standard treatment for patients at ultra-high risk for psychosis: study protocol for a randomised controlled trial. Trials. 2015;16:25. doi: 10.1186/s13063-014-0542-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


