Abstract
Background
Shoulder impingement syndrome (SIS) is a common diagnosis for patients with pain and dysfunction of the shoulder. Variations in the signs and symptoms might lead to uncertainty regarding the definition of SIS. The aim of this review is to explore the participant selection criteria used in the literature when investigating SIS and to assess differences in criteria among treating professions.
Methods
This is a PRISMA systematic review of publications from 2009 to 2014 from MEDLINE, PubMed, The Cochrane Library, Embase, Scopus and CINAHL.
Results
Ninety-seven articles met inclusion criteria for this review. Twenty-five different surgical and nonsurgical treatments were investigated. Impingement-specific index tests were used in all studies. Exclusion index tests were used in 62% of studies. Twenty index tests were identified. Radiological investigations were reported in 53% of all studies, of which a further 53% reported using two or more radiological investigations.
Conclusions
This systematic review has illustrated that studies investigating SIS test for various signs and symptoms, which is in keeping with describing the condition as a ‘syndrome’. However, there are inconsistencies in participant selection criteria between health disciplines, highlighting a need for harmonization of the selection criteria in the form of an international editorial consensus.
Keywords: assessment criteria, index tests, shoulder impingement syndrome, subacromial impingement
Introduction
Shoulder impingement syndrome (SIS) is a common diagnosis for patients who present with pain and dysfunction of the shoulder. The aetiology of the condition is recognized as being multifactorial resulting from an interplay of intrinsic and extrinsic factors.1,2 Since SIS is a clinical syndrome, the diagnosis is determined by a collection of signs and symptoms.3,4 Variations in the signs and symptoms might lead to uncertainty regarding the definition of SIS. Many studies highlight the difficulty in differentiating impingement from other shoulder pathologies, where shoulder pain can be indicative of other conditions such as joint instability, cervical radiculopathy, calcific tendinitis, adhesive capsulitis, degenerative joint disease, acromioclavicular osteoarthrosis and nerve compression.2,5–7 Consequently, the use of the term SIS as a diagnostic label has been the subject of debate, as it has been used for a spectrum of other shoulder and cervical conditions5,6,8–11 Diagnosis of SIS often relies upon a combination of physical examinations and further radiological investigations. However, the literature contains no suitable definition for the diagnosis of SIS using ultrasound and magnetic resonance imaging where such investigations play only a supporting role in the exclusion of other conditions.7,12–14 Multidisciplinary consensus on the clinical criteria used to define SIS is important to avoid inappropriate surgical or nonsurgical intervention and to facilitate the direct comparison of outcomes of various treatment options. If there is no consensus on the selection criteria of study participants between professions and levels of evidence, it is difficult to compare outcomes of various treatment options effectively. The aim of this review was to explore the participant selection criteria for studies investigating SIS and to assess differences in the selection criteria amongst treating professions.
Materials and Methods
This systematic review was conducted and reported according to the protocol outlined by Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).15 The protocol for this systematic review was registered on PROSPERO (CRD42014014740).
Search strategy for identification of studies for this review
In order to identify all studies pertaining to the treatment or identification of SIS, the following medical databases were searched: MEDLINE, PubMed, The Cochrane Library, Embase, Scopus and CINAHL, with papers limited to five years of publication from January 2009 to January 2014. The search strategy determined by the two reviewers (AW and BW) with the assistance of a senior medical librarian (RD, who structured the key words using Boolean language and conducted the final search.
Medical Subject Headings (MeSH) were used in combination with relevant keywords in order to retrieve all publications meeting the inclusion criteria. Papers not in the English language were excluded, as were abstracts from scientific meetings, unpublished reports and review articles. The search strategy included the MeSH term ‘Shoulder Impingement Syndrome’, as well as the terms ‘shoulder*’ OR ‘subacromial’ OR ‘sub-acromial’ AND ‘imping*’ OR ‘burs*’. Where ‘burs*’ can represent ‘bursitis’, ‘bursa’ and ‘bursae’.
Inclusion criteria
Studies
The literature search performed for this review was limited to published clinical studies. Studies included in the final sample were limited to articles detailing the clinical criteria used to classify SIS or the participant inclusion criteria for SIS. Studies were only included if they were reporting on investigations of patients selected using the specific diagnostic labels of SIS, subacromial impingement or subacromial bursitis. There were no restrictions on the kind of intervention or the population being studied. There was also no restriction placed on the Level of Evidence (LOE) of included studies. The classification system for LOE was that of the Journal of Bone and Joint Surgery (JBJS), adapted from the Centre for Evidence-Based Medicine, Oxford, UK.16 Study designs included randomized controlled trials (RCT), prospective comparative studies, case–control studies, case series and retrospective studies.
Exclusion criteria
Studies assessing conditions other than SIS were excluded, such as investigations into the treatment of rotator cuff tears, adhesive capsulitis (frozen shoulder), shoulder tendinitis and other shoulder pathologies.
Outcome measures
The clinical criterion used in the literature to define SIS was retrieved from the ‘materials and methods’ section of studies. The studies used terms such as ‘eligibility criteria’, ‘inclusion criteria for participation in the study’, ‘diagnostic methodology’ or ‘clinical criteria’. Studies reported on the minimum duration of symptoms for inclusion into the study, the inclusion and exclusion criteria based on medical history, the physical examinations performed, the number of positive physical examinations required for inclusion in the study and the radiological investigations used to supplement the diagnosis of SIS. Secondary information collected from the publications was: the type of specialist assessing the condition, LOE, patients’ age range and the type of intervention.
Selection of studies
Studies were reviewed for eligibility based on the title and abstract and if this was insufficient the full manuscript was obtained. All identified studies were independently assessed by two reviewers (AW and BW). Disagreement was resolved by discussion with both reviewers and the senior orthopaedic consultant (JK) until consensus was reached.
Data collection
One reviewer (AW) extracted the outcomes of interest from all included studies. The second reviewer (BW) independently extracted the outcomes of interest from a random selection of twenty percent of included studies to examine the rate of agreement. Any discrepancies were cross-referenced with the original article and disagreements in the data were resolved by discussion.
Assessment of risk of bias in included studies
An assessment of bias was not undertaken as the treatment outcomes were not assessed in this review.
Quantitative method
Analyses were carried out using Stata, version 13.1 (StataCorp, College Station, TX, USA). In order to examine whether the use of index tests is associated with profession type, we examined the eight most commonly used tests [Neer sign, Hawkins–Kennedy, Painful arc, Jobe, Resisted tests, X-rays, ultrasound (USA) and magnetic resonance imaging (MRI)] against two professions: Physiotherapy and Orthopaedics. Comparisons were performed using a chi-squared test or Fisher’s exact test, when the assumption for chi-squared test was not met. Studies involving both Physiotherapy and Orthopaedics were excluded from chi-squared analyses. The above eight tests were also examined against the level of evidence (excluding Level IV) for their associations using the chi-squared test. P < 0.05 was considered statistically significant.
Results
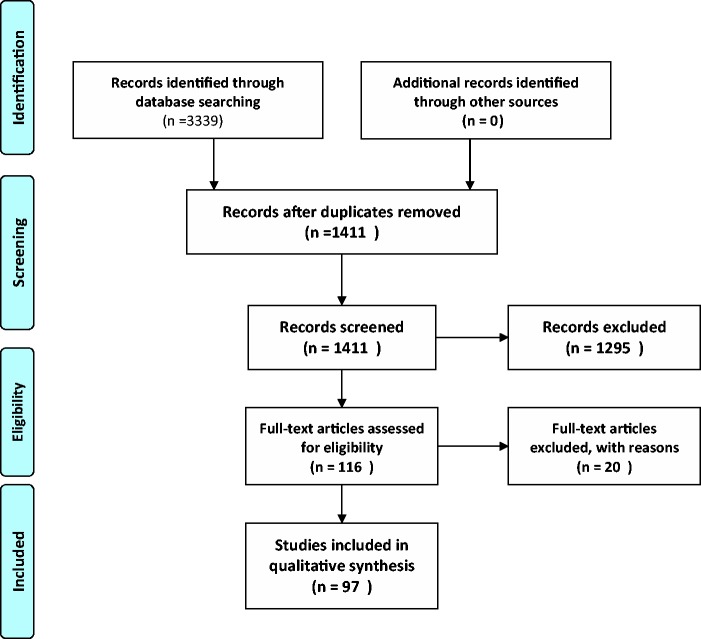
The search of MEDLINE, PubMed, the Cochrane Library, Embase, Scopus and CINAHL databases provided 3339 citations (Fig. 1). After adjusting for duplicates, 1411 citations remained, and after reviewing the abstracts, 1295 studies were excluded, not having met the inclusion criteria. The full text articles of the remaining 116 studies were examined for eligibility and 97 studies were identified for inclusion in the review.7,13,17–111
Figure 1.
PRISMA flow diagram.
Characteristics of included studies
The studies selected in the review reported on 25 different interventions for SIS. When assessing the type of health profession conducting the study, the following breakdown was established; 62% Physiotherapy, 27% Orthopaedic surgery, 7% Rehabilitative medicine, 4% Rheumatology, and 1% from each of the following: Radiology, General Practice and Anaesthesiology.
Using the LOE hierarchy; there were 29 Level I evidence studies, 32 Level II, 23 Level III evidence and 11 Level IV evidence. There were no Level V studies. The sample size of the studies ranged from six to 307 patients, with a total of 5514 participants in the studies. The age of patients reported ranged from 14 years to 92 years. The mean minimum duration of pain for inclusion in the studies was 11.7 weeks with an SD of 10.9 and ranged from 1 week to 72 weeks. Thirteen studies stated that patients required a mean minimum visual-analogue pain score of 3.4, with a SD of 0.8 to be included in the study.
Index tests
Physical examination index tests were stated in all but fourteen studies as part of the clinical inclusion criteria used to define SIS, where, in total, 20 different tests were identified in Table 1. Commonly, a combination of index tests were part of the clinical criteria used to define SIS. Of these, 82% used at least one of Neer sign or Hawkins–Kennedy test, 70% used Neer sign and Hawkins–Kennedy together, and 30% used the Neer sign, Hawkins–Kennedy and Painful arc combination. The positive Neer injection test, described as the injection of 10 mL of 1% lignocaine into subacromial space, relieving pain after 10 minutes, was reported in 15 of the studies as part of their criteria for inclusion. Three of the studies relied exclusively on this test to define SIS. Overall, there were 14 different combinations of the five impingement sign tests used in studies included in the present review.
Table 1.
Reported use of index tests and radiological investigations.
| Impingement specific index tests (%) | |
| Neer sign | 76.3 |
| Hawkins–Kennedy | 76.3 |
| Jobe (empty can) | 39.2 |
| Neer Injection test | 15.5 |
| Yocum | 2.1 |
| Painful arc | 36.1 |
| Exclusion index tests (%) | |
| Resisted tests | 25.8 |
| Pain range of motion | 17.5 |
| Apprehension test | 10.3 |
| Speed | 8.2 |
| Sulcus | 4.1 |
| Spurling | 4.1 |
| Gerber | 4.1 |
| Drop arm sign | 4.1 |
| Yergasons | 2.1 |
| External rotation lag sign | 1 |
| Crossover | 1 |
| Walsh | 1 |
| O’Brien | |
| Use of radiological investigations (%) | |
| Total | 61 |
| X-rays | 53 |
| Ultrasound | 51 |
| Magnetic resonance imaging | 49 |
| Computed tomography scan | 3 |
| Magnetic resonance arthography | 1 |
Further index tests excluding other shoulder pathologies were frequently reported in the included literature, forming part of the clinical criteria used to define SIS. Such tests included, the Jobe (empty can) sign, Resisted tests, Apprehension/relocation test, Speed’s test, Sulcus sign, Spurling sign, Gerber sign, Drop arm sign, Yergason’s test, External rotation lag sign, Walsh test, Crossover test and O’Brien’s test. In the included studies, it was found that 39% used the Jobe sign, 25% used Resisted tests, 17% used painful range of motion, and 10% used the Apprehension test. Speeds, Sulcus, Spurling and Drop arm sign were used equally in 4% of studies and the remaining tests were used only once. More commonly, a combination of exclusion index tests where part of the clinical criteria used to define SIS, 50% used at least one of either the Jobe sign or Resisted tests (68% of those used any exclusion tests), 59% used at least one of the Jobe sign or Resisted tests or Pain tange of motion (83% of those used any exclusion tests) and 38% used no exclusion index tests.
Often as part of the inclusion criteria, studies reported patients needed to test positive to a certain number of impingement sign examinations to be eligible for the study. Out of 41 studies that specified a set number of positive tests required for patient eligibility, 35 (85%) reported that they required two or more positive tests for inclusion into the study. Of these studies, a mean of five physical examinations were used in total (range 2 to 9). It was noted that 30 out of this 35 (85.7%), were studies carried out by Physiotherapists. Overall, there were 21 different combinations of the 11 exclusion tests used in the studies included in the present review.
Radiological investigations
Radiological investigations were reported as part of the criteria to aid in identification of SIS in 59 (61%) of the studies. Of those studies, 27 (46%) used more than one investigation. Table 1 shows the studies that reported use of radiological investigations. Further analysis found that 13 (22%) used US only, nine (15%) used MRI only and nine (15%) used X-rays only.
Of the studies using radiological investigations, 14% used X-rays and MRI together and 12% used X-rays and US together. In total, 39% did not include radiological investigations in their diagnostic assessment for SIS. Overall, there were 11 different combinations of the five imaging modalities used in studies included in this review.
Use of index tests and treating professions
The two most common treating professions were Physiotherapy and Orthopaedics; 53 and 19 studies were identified, respectively. The incidence of the different clinical tests used by physiotherapists and orthopaedic surgeons is presented in Table 2. Physiotherapists were significantly more likely to use Neer sign, Hawkins–Kennedy sign, Painful arc and Jobe sign (p = 0.009, 0.004, 0.032 and 0.005, respectively), whereas Orthopaedic surgeons were more likely to use X-rays (p < 0.001) and MRIs (p < 0.001) as part of their diagnostic assessment. US imaging was reported broadly across both professions.
Table 2.
Use of index tests and treating professions.
| Factor | Physiotherapy | Orthopaedics | p-value |
|---|---|---|---|
| n | 53 | 19 | |
| Neer sign | 44 (83%) | 10 (53%) | 0.009 |
| Hawkins–Kennedy | 45 (85%) | 10 (53%) | 0.004 |
| Painful arc | 23 (43%) | 3 (16%) | 0.032 |
| Jobe (empty can) | 28 (53%) | 3 (16%) | 0.005 |
| Resisted tests | 17 (32%) | 2 (11%) | 0.067 |
| X-rays | 9 (17%) | 13 (68%) | <0.001 |
| Ultrasound | 14 (26%) | 7 (37%) | 0.39 |
| Magnetic resonance imaging | 7 (13%) | 12 (63%) | <0.001 |
Use of tests and LOE
There were eighty-four studies that had a LOE of III or higher. There was no significant association between the use of tests and level of evidence except for the X-rays, which was more likely to be used with studies with higher level of evidence (p = 0.024) (Table 3).
Table 3.
Index tests and level of evidence.
| Levels of evidence | I | II | III | p-value |
|---|---|---|---|---|
| n | 29 | 32 | 23 | |
| Neer sign | 21 (72%) | 26 (81%) | 16 (70%) | 0.57 |
| Hawkins–Kennedy | 22 (76%) | 25 (78%) | 16 (70%) | 0.76 |
| Painful arc | 12 (41%) | 10 (31%) | 7 (30%) | 0.63 |
| Jobe (empty can) | 8 (28%) | 16 (50%) | 7 (30%) | 0.15 |
| Resisted tests | 10 (34%) | 8 (25%) | 3 (13%) | 0.21 |
| X-rays | 15 (52%) | 9 (28%) | 4 (17%) | 0.024 |
| US | 8 (28%) | 11 (34%) | 7 (30%) | 0.85 |
| Magnetic resonance imaging | 8(28%) | 12 (38%) | 5 (22%) | 0.43 |
Discussion
The aim of this review was to assess the participant selection criteria when investigating SIS in the literature and to assess variations in methodology amongst treating professions. The descriptive analyses presented herein demonstrate the diverse combination of index examinations and radiological investigations used in current practice. The Neer impingement sign and Hawkins–Kennedy test are the most commonly used physical examinations employed by all professions investigating SIS and across all LOE. However, there is a wide range in the number and choice of tests used in combination with these two tests. In studies where physiotherapy was the nominated profession, there was a reliance on the use of an index test for a diagnosis. On the other hand, a significant reliance on the use of radiological investigations was demonstrated in orthopaedic lead studies. Although this may simply be a reflection of what occurs in standard practice where orthopaedic surgeons have access to imaging and physiotherapists do not, it is encouraging to see an importance placed on the two diagnostic methods in both professions. Physiotherapy and Orthopaedic studies illustrated a wide range in the total number of index tests used; (0 to 9) and (0 to 8) respectively. Thus the use of such a range demonstrates the diversity of signs and symptoms being tested for in the participant selection criteria for SIS within the professions themselves. These findings demonstrate a strong emphasis on use of a cluster of positive impingement sign tests as well as additional tests to exclude other shoulder pathologies. Although this is consistent with the nature of SIS as a syndrome, there appears to be poor consensus on the combination of tests required to define and ultimately diagnose shoulder impingement.
The use of numerous index tests and radiological investigations may be an indication of the widespread uncertainties in understanding the aetiology of SIS and difficulties in distinguishing SIS from other shoulder pathologies. Level I and II evidence is purportedly a good indicator for common standard of practice, where a ‘gold standard’ practice may be identified. However, as the Levels of evidence I and II made up 30% and 33% of the included studies, respectively, there does not appear to be a ‘gold standard’ for the classification of SIS.
In a Cochrane review of RCTs, Hanchard et al.112 investigated the accuracy of physical tests for SIS and other shoulder pathologies. When a combination of seven positive tests was used, the sensitivity estimate was 5% [95% confidence interval (CI) 1% to 11%] and specificity estimate was 97% (95% CI 86% to 100%). When only a combination of a positive Hawkins’ test or Neer’s sign was used, the sensitivity estimates increased markedly to 96% (95% CI 79% to 100%) and specificity estimates fell to 41% (95% CI 29% to 54%).112 Although the combination of the two most commonly used index tests was found to be highly sensitive in detecting impingement sign, a large number of false positives were observed. Hanchard et al.112 concluded that there are no strong index tests for diagnosing impingement and that greater emphasis should be placed on making a diagnosis based on the exclusion of other shoulder pathologies.
Our review highlighted that there is no preferred current imaging modalities. Furthermore, half used two or more radiological investigations in their diagnostic methodology. Lee et al.67 discussed that US and MRI often fail to provide useful information for assessing the patients and that these investigations should not be used as diagnostic instruments to identify shoulder lesions. This recommendation was based on findings that radiologic analyses were frequently incompatible with the clinical manifestation.67
The literature often reports that X-ray and US imaging are used to confirm a diagnosis of SIS; however, it would be more accurate to state that their primary use is to confirm the exclusion of other pathologies. Neer’s original work in 1972 reported using arthrograms to determine rotator cuff integrity, on the grounds that abnormalities such as chronic bursitis, partial-thickness tears, calcium deposits and complete tears could not be distinguished by physical examinations and radiographic findings alone.113 Although only one study in this systematic review used a magnetic resonance arthrography (MRA) in their method of diagnosis, there is increasing evidence to support the use of MRA when considering surgical treatment.114. Pavic et al.,114 in a study of 200 consecutive patients, compared the accuracy of US, MRI and MRA, where all patients underwent an arthroscopy to confirm diagnosis of shoulder pathology. Interestingly, US was found to be a valuable diagnostic tool in several studies for rotator cuff complete or incomplete tears, MRI was indicated to be accurate in determining Hills–Sach lesions or bony lesions, and MRA was found to be superior in accurately diagnosing labral capsular ligamentous complex lesions such as internal subacromial impingement.7,114
This research can be used as an aid for the development of diagnostic and treatment protocols. It highlights the most current methods used to diagnose SIS and can help clinicians reflect on what truly defines a case of impingement syndrome. If SIS is suspected in a patient Neer impingement sign and Hawkins–Kennedy should be tested as they are the only impingement specific and widely validated index tests. Further use of the index tests found in this study are important as they provide the examiner with an overall indication of the integrity and kinematics of a problem shoulder joint. Ultimately, understanding the pathology and awareness of diagnostic tools available may help clinicians distinguish between a need for conservative or surgical treatment of the condition.
Largely, the studies included in this review were testing for a wide range of signs and symptoms, in keeping with the description of the condition as a ‘syndrome’.
Strengths and limitations
To our knowledge, this is the first systematic review to assess the participant selection criteria used in studies investigating SIS. This study also assessed the correlation between level of evidence and diagnostic criteria. By PRISMA guidelines, registering the review with PROSPERO and using the JBJS evidence hierarchy, this study used a transparent method of assessing and reporting the evidence.
In our search strategy, we did not include grey literature. Incomplete reporting of inclusion criteria and diagnostic methodology in the included studies is also a limitation. It is important to highlight that there may be variances in practices of some countries where the role of the physiotherapist and the orthopaedic specialist will differ.
Conclusions
This review provides insight into the extensive research undertaken in the last 5 years for the treatment and management of Shoulder impingement syndrome. It highlights inconsistencies in selection criteria currently used within and between health disciplines when reporting on their investigations of this syndrome. The use of a wide range of diagnostic index tests and multiple radiological investigations illustrates the complex nature of a condition such as SIS where the pathogenesis remains unclear.
There is little uniformity in the signs and symptoms being tested for, which is reflected in the variety combinations of physical examinations and radiological investigations reported in the 97 papers included in this review. Future research studies investigating SIS should at a minimum use a positive Neer sign and Hawkins–Kennedy test to define the cohort of study patients. Highlighting the poor uniformity is important as current management of SIS is based on evidence derived from clinical trials. If there is no consensus on the selection criteria of study participants between professions and levels of evidence, it is difficult to compare outcomes of various treatment options effectively.
There needs to be harmonization of the selection criteria in the form of an international editorial consensus and more research into the patho-aetiology of SIS. Clarity is pertinent to ensure practitioners and researchers across all disciplines are treating and investigating the same pathology in their quest to establish evidence-based and effective practice. It is possible that the development of a more detailed understanding of, and agreement on, the signs and symptoms of SIS would contribute to our improved understanding of the common pathology.
Acknowledgements
We thank Ms Raechel Damarell (Senior Medical Librarian BA, Grad Dip Info Stud, AALIA).
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Level of evidence
Level IV
References
- 1.Harrison AK, Flatow EL. Subacromial impingement syndrome. J Am Acad Orthop Surg 2011; 19: 701–8. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani LU, Levine WN. Subacromial impingement syndrome. J Bone Joint Surg Am 1997; 79: 1854–68. [PubMed] [Google Scholar]
- 3.Yu CM, Chen CH, Liu HT, Dai MH, Wang IC, Wang KC. Subacromial injections of corticosteroids and xylocaine for painful subacromial impingement syndrome. Chang Gung Med J 2006; 29: 474–9. [PubMed] [Google Scholar]
- 4.Hayes PR, Flatow EL. Attrition sign in impingement syndrome. Arthroscopy 2002; 18: E44–E44. [DOI] [PubMed] [Google Scholar]
- 5.de Witte PB, de Groot JH, van Zwet EW, et al. Communication breakdown: clinicians disagree on subacromial impingement. Med Biol Eng Comput 2014; 52: 221–31. [DOI] [PubMed] [Google Scholar]
- 6.Braman JP, Zhao KD, Lawrence RL, Harrison AK, Ludewig PM. Shoulder impingement revisited: evolution of diagnostic understanding in orthopedic surgery and physical therapy. Med Biol Eng Comput 2014; 52: 211–9. [DOI] [PubMed] [Google Scholar]
- 7.Park J-Y, Park S-G, Keum J-S, Oh J-H, Park J-S. The diagnosis and prognosis of impingement syndrome in the shoulder with using quantitative SPECT assessment: a prospective study of 73 patients and 24 volunteers. Clin Orthop Surg 2009; 1: 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA., III Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Joint Surg Am 2011; 93: 1827–32. [DOI] [PubMed] [Google Scholar]
- 9.Schellingerhout JM, Verhagen AP, Thomas S, Koes BW. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Manual Ther 2008; 13: 478–83. [DOI] [PubMed] [Google Scholar]
- 10.Green S, Buchbinder R, Glazier R, Forbes A. Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessment, and efficacy. BMJ 1998; 316: 354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop 2014; 85: 314–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zanetti M, Jost B, Hodler J, Gerber C. MR imaging after rotator cuff repair: full-thickness defects and bursitis-like subacromial abnormalities in asymptomatic subjects. Skeletal Radiol 2000; 29: 314–9. [DOI] [PubMed] [Google Scholar]
- 13.Hsieh LF, Hsu WC, Lin YJ, Wu SH, Chang KC, Chang HL. Is ultrasound-guided injection more effective in chronic subacromial bursitis? Med Sci Sports Exerc 2013; 45: 2205–13. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor PJ, Rankine J, Gibbon WW, Richardson A, Winter F, Miller JH. Interobserver variation in sonography of the painful shoulder. J Clin Ultrasound 2005; 33: 53–6. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006–12. [DOI] [PubMed] [Google Scholar]
- 16.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am 2003; 85: 1–3. [PubMed] [Google Scholar]
- 17.Abrisham SM, Kermani-Alghoraishi M, Ghahramani R, Jabbari L, Jomeh H, Zare M. Additive effects of low-level laser therapy with exercise on subacromial syndrome: a randomised, double-blind, controlled trial. Clin Rheum 2011; 30: 1341–6. [DOI] [PubMed] [Google Scholar]
- 18.Akyol Y, Ulus Y, Durmus D, et al. Effectiveness of microwave diathermy on pain, functional capacity, muscle strength, quality of life, and depression in patients with subacromial impingement syndrome: a randomized placebo-controlled clinical study. Rheumatol Int 2012; 32: 3007–16. [DOI] [PubMed] [Google Scholar]
- 19.Aydin A, Yildiz V, Kalali F, Yildirim OS, Topal M, Dostbil A. The role of acromion morphology in chronic subacromial impingement syndrome. Acta Orthop Belg 2011; 77: 733–6. [PubMed] [Google Scholar]
- 20.Bae YH, Lee GC, Shin WS, Kim TH, Lee SM. Effect of motor control and strengthening exercises on pain, function, strength and the range of motion of patients with shoulder impingement syndrome. J Phys Ther Sci 2011; 23: 687–92. [Google Scholar]
- 21.Bal A, Eksioglu E, Gurcay E, Gulec B, Karaahmet O, Cakci A. Low-level laser therapy in subacromial impingement syndrome. Photomed Laser Surg 2009; 27: 31–6. [DOI] [PubMed] [Google Scholar]
- 22.Başkurt Z, Başkurt F, Gelecek N, H. Özkan M. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil 2011; 24: 173–9. [DOI] [PubMed] [Google Scholar]
- 23.Beaudreuil J, Lasbleiz S, Yelnik A, Bardin T, Orcel P. Effect of dynamic humeral centering on painful active elevation of the arm in subacromial impingement syndrome: a randomized trial, Effet du recentrage humeral dynamique sur la douleur provoquee par l'elevation active du bras au cours du conflit sous-acromial: une etude randomisee. [French, English]. Ann Physical Rehabil Med 2012; 55: e158–e9. [Google Scholar]
- 24.Bernhardsson S, Klintberg IH, Wendt GK. Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clin Rehab 2011; 25: 69–78. [DOI] [PubMed] [Google Scholar]
- 25.Biberthaler P, Beirer M, Kirchhoff S, Braunstein V, Wiedemann E, Kirchhoff C. Significant benefit for older patients after arthroscopic subacromial decompression: a long-term follow-up study. Int Orthop 2013; 37: 457–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyles RE, Ritland BM, Miracle BM, et al. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Manual Ther 2009; 14: 375–80. [DOI] [PubMed] [Google Scholar]
- 27.Cadogan A, Laslett M, Hing W, McNair P, Taylor S. Clinical predictors of a positive response to guided diagnostic block into the subacromial bursa. J Rehabil Med 2012; 44: 877–84. [DOI] [PubMed] [Google Scholar]
- 28.Calis HT, Berberoglu N, Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. Eur J Phys Rehabil Med 2011; 47: 375–80. [PubMed] [Google Scholar]
- 29.Camargo PR, Avila MA, Alburquerque-Sendin F, Asso NA, Hashimoto LH, Salvini TF. Eccentric training for shoulder abductors improves pain, function and isokinetic performance in subjects with shoulder impingement syndrome – a case series. Revista Brasileira de Fisioterapia 2012; 16: 74–83. [DOI] [PubMed] [Google Scholar]
- 30.Camargo PR, Avila MA, Asso NA, Salvini TF. Muscle performance during isokinetic concentric and eccentric abduction in subjects with subacromial impingement syndrome. Eur J Appl Physiol 2010; 109: 389–95. [DOI] [PubMed] [Google Scholar]
- 31.Celik D, Sirmen B, Demirhan M. The relationship of muscle strength and pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc 2011; 45: 79–84. [DOI] [PubMed] [Google Scholar]
- 32.Chew K, Pua YH, Chin J, Clarke M, Wong YS. Clinical predictors for the diagnosis of supraspinatus pathology. Physiother Singapore 2010; 13: 12–7. [Google Scholar]
- 33.Cook C, Learman K, Houghton S, Showalter C, O'Halloran B. The addition of cervical unilateral posterior–anterior mobilisation in the treatment of patients with shoulder impingement syndrome: a randomised clinical trial. Manual Ther 2014; 19: 18–24. [DOI] [PubMed] [Google Scholar]
- 34.Crawshaw DP, Helliwell PS, Hensor EMA, Hay EM, Aldous SJ, Conaghan PG. Exercise therapy after corticosteroid injection for moderate to severe shoulder pain: large pragmatic randomised trial. BMJ (Online) 2010; 341: 30–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cummins CA, Sasso LM, Nicholson D. Impingement syndrome: temporal outcomes of nonoperative treatment. J Shoulder Elbow Surg 2009; 18: 172–7. [DOI] [PubMed] [Google Scholar]
- 36.De Mey K, Danneels L, Cagnie B, Cools AM. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med 2012; 40: 1906–15. [DOI] [PubMed] [Google Scholar]
- 37.de Oliveira VMA, Batista LSP, Pirauá ALT, Pitangui ACR, de Araújo RC. Electromyographic activity and scapular dyskenesia in athletes with and without shoulder impingement syndrome. Revista Brasileira de Cineantropometria e Desempenho Humano 2013; 15: 193–203. [Google Scholar]
- 38.Djordjevic OC, Vukicevic D, Katunac L, Jovic S. Mobilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder: results of a clinical trial.[Erratum appears in J Manipulative Physiol Ther 2012; 35:659]. J Manipulative Physiol Ther 2012; 35: 454–63. [DOI] [PubMed] [Google Scholar]
- 39.Dogan SK, Ay S, Evcik D. The effectiveness of low laser therapy in subacromial impingement syndrome: a randomized placebo controlled double-blind prospective study. Clinics 2010; 65: 1019–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dogu B, Dalgic Yucel S, Yamac Sag S, Bankaoglu M, Kuran B. Blind or ultrasound-guided corticosteroid injections and short-term response in subacromial impingement syndrome: a randomized, double-blind, prospective study. Am J Physical Med Rehab 2012; 91: 658–65. [DOI] [PubMed] [Google Scholar]
- 41.Engebretsen K, Grotle M, Bautz-Holter E, Ekeberg OM, Juel NG, Brox JI. Supervised exercises compared with radial extracorporeal shock-wave therapy for subacromial shoulder pain: 1-year results of a single-blind randomized controlled trial. Phys Ther 2011; 91: 37–47. [DOI] [PubMed] [Google Scholar]
- 42.Galace de Freitas D, Marcondes FB, Monteiro RL, Rosa SG, Maria de Moraes Barros Fucs P, Fukuda TY. Pulsed electromagnetic field and exercises in patients with shoulder impingement syndrome: a randomized, double-blind, placebo-controlled clinical trial. Arch Phys Med Rehab 2014; 95: 345–52. [DOI] [PubMed] [Google Scholar]
- 43.Garrison JC, Shanley E, Thigpen C, Hegedus E, Cook C. Between-session changes predict overall perception of improvement but not functional improvement in patients with shoulder impingement syndrome seen for physical therapy: an observational study. Physiother Theory Pract 2011; 27: 137–45. [DOI] [PubMed] [Google Scholar]
- 44.Gwilym SE, Oag HC, Tracey I, Carr AJ. Evidence that central sensitisation is present in patients with shoulder impingement syndrome and influences the outcome after surgery. J Bone Joint Surg Br 2011; 93: 498–502. [DOI] [PubMed] [Google Scholar]
- 45.Haik MN, Camargo PR, Zanca GG, Alburquerque-Sendin F, Salvini TF, Mattiello-Rosa SM. Joint position sense is not altered during shoulder medial and lateral rotations in female assembly line workers with shoulder impingement syndrome. Physiother Theory Pract 2013; 29: 41–50. [DOI] [PubMed] [Google Scholar]
- 46.Hakgüder A, Taştekin N, Birtane M, Uzunca K, Zateri C, Süt N. Comparison of the short-term efficacy of physical therapy in subacromial impingement syndrome patients with stage i and ii magnetic resonance imaging findings. Arch Rheumatol 2011; 26: 127–34. [Google Scholar]
- 47.Hall LC, Middlebrook EE, Dickerson CR. Analysis of the influence of rotator cuff impingements on upper limb kinematics in an elderly population during activities of daily living. Clin Biomech 2011; 26: 579–84. [DOI] [PubMed] [Google Scholar]
- 48.Hallstrom E, Karrholm J. Shoulder rhythm in patients with impingement and in controls: dynamic RSA during active and passive abduction. Acta Orthop 2009; 80: 456–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hekimoglu B, Aydin H, Kizilgoz V, Tatar IG, Ersan O. Quantitative measurement of humero-acromial, humero-coracoid, and coraco-clavicular intervals for the diagnosis of subacromial and subcoracoid impingement of shoulder joint. Clin Imaging 2013; 37: 201–10. [DOI] [PubMed] [Google Scholar]
- 50.Henkus HE, de Witte PB, Nelissen RG, Brand R, van Arkel ER. Bursectomy compared with acromioplasty in the management of subacromial impingement syndrome: a prospective randomised study. J Bone Joint Surg Br 2009; 91: 504–10. [DOI] [PubMed] [Google Scholar]
- 51.Heredia-Rizo AM, Lopez-Hervas A, Herrera-Monge P, Gutierrez-Leonard A, Pina-Pozo F. Shoulder functionality after manual therapy in subjects with shoulder impingement syndrome: a case series. J Bodywork Mov Ther 2013; 17: 212–8. [DOI] [PubMed] [Google Scholar]
- 52.Hidalgo-Lozano A, Fernandez-De-Las-Penas C, Alonso-Blanco C, Ge HY, Arendt-Nielsen L, Arroyo-Morales M. Muscle trigger points and pressure pain hyperalgesia in the shoulder muscles in patients with unilateral shoulder impingement: a blinded, controlled study. Exp Brain Res 2010; 202: 915–25. [DOI] [PubMed] [Google Scholar]
- 53.Hidalgo-Lozano A, Fernandez-de-las-Penas C, Diaz-Rodriguez L, Gonzalez-Iglesias J, Palacios-Cena D, Arroyo-Morales M. Changes in pain and pressure pain sensitivity after manual treatment of active trigger points in patients with unilateral shoulder impingement: a case series. J Bodywork Mov Ther 2011; 15: 399–404. [DOI] [PubMed] [Google Scholar]
- 54.Holmgren T, Hallgren HB, Oberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ (Online) 2012; 344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsu Y-H, Chen W-Y, Lin H-C, Wang WTJ, Shih Y-F. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J Electromyogr Kinesiol 2009; 19: 1092–9. [DOI] [PubMed] [Google Scholar]
- 56.Huang H-Y, Lin J-J, Guo YL, Wang WT-J, Chen Y-J. EMG biofeedback effectiveness to alter muscle activity pattern and scapular kinematics in subjects with and without shoulder impingement. J Electromyogr Kinesiol 2013; 23: 267–74. [DOI] [PubMed] [Google Scholar]
- 57.Hultenheim Klintberg I, Karlsson J, Svantesson U. Health-related quality of life, patient satisfaction, and physical activity 8-11 years after arthroscopic subacromial decompression. J Shoulder Elbow Surg 2011; 20: 598–608. [DOI] [PubMed] [Google Scholar]
- 58.Hung C-J, Jan M-H, Lin Y-F, Wang T-Q, Lin J-J. Scapular kinematics and impairment features for classifying patients with subacromial impingement syndrome. Manual Ther 2010; 15: 547–51. [DOI] [PubMed] [Google Scholar]
- 59.Johansson K, Bergstrom A, Schroder K, Foldevi M. Subacromial corticosteroid injection or acupuncture with home exercises when treating patients with subacromial impingement in primary care – a randomized clinical trial. Fam Pract 2011; 28: 355–65. [DOI] [PubMed] [Google Scholar]
- 60.Kalter J, Apeldoorn AT, Ostelo RW, Henschke N, Knol DL, van Tulder MW. Taping patients with clinical signs of subacromial impingement syndrome: the design of a randomized controlled trial. BMC Musculoskelet Disord 2011; 12: 188–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kappe T, Knappe K, Elsharkawi M, Reichel H, Cakir B. Predictive value of preoperative clinical examination for subacromial decompression in impingement syndrome. Knee Surg Sports Traumatol Arthrosc 2013, pp. 1–6. [DOI] [PubMed] [Google Scholar]
- 62.Karthikeyan S, Kwong HT, Upadhyay PK, Parsons N, Drew SJ, Griffin D. A double-blind randomised controlled study comparing subacromial injection of tenoxicam or methylprednisolone in patients with subacromial impingement. J Bone Joint Surg Br 2010; 92: 77–82. [DOI] [PubMed] [Google Scholar]
- 63.Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatol 2011; 30: 201–7. [DOI] [PubMed] [Google Scholar]
- 64.Ketola S, Lehtinen J, Arnala I, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg Br 2009; 91: 1326–34. [DOI] [PubMed] [Google Scholar]
- 65.Kim Y-S, Park J-Y, Lee C-S, Lee S-J. Does hyaluronate injection work in shoulder disease in early stage? A multicenter, randomized, single blind and open comparative clinical study. J Shoulder Elbow Surg 2012; 21: 722–7. [DOI] [PubMed] [Google Scholar]
- 66.Kromer TO, Bie RA, Bastiaenen CH. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskelet Disord 2010; 11: 114–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee JH, Lee SH, Song SH. Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. Clin J Pain 2011; 27: 523–8. [DOI] [PubMed] [Google Scholar]
- 68.Leong H-T, Tsui S, Ying M, Leung VY-F, Fu SN. Ultrasound measurements on acromio-humeral distance and supraspinatus tendon thickness: test–retest reliability and correlations with shoulder rotational strengths. J Sci Med Sport 2012; 15: 284–91. [DOI] [PubMed] [Google Scholar]
- 69.Lin-Fen H, Wei-Chun H, Yi-Jia L, Shih-Hui W, Kae-Chwen C, Hsiao-Lan C. Is ultrasound-guided injection more effective in chronic subacromial bursitis? Med Sci Sports Exerc 2013; 45: 2205–13. [DOI] [PubMed] [Google Scholar]
- 70.Lu Y, Zhang Q, Zhu Y, Jiang C. Is radiofrequency treatment effective for shoulder impingement syndrome? A prospective randomized controlled study. J Shoulder Elbow Surg 2013; 22: 1488–94. [DOI] [PubMed] [Google Scholar]
- 71.Lunsj K, Bengtsson M, Nordqvist A, Abu-Zidan FM. Patients with shoulder impingement remain satisfied 6 years after arthroscopic subacromial decompression. Acta Orthop 2011; 82: 711–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maenhout AG, Mahieu NN, De Muynck M, De Wilde LF, Cools AM. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1158–67. [DOI] [PubMed] [Google Scholar]
- 73.Magaji SA, Singh HP, Pandey RK. Arthroscopic subacromial decompression is effective in selected patients with shoulder impingement syndrome. J Bone Joint Surg Br 2012; 94: 1086–9. [DOI] [PubMed] [Google Scholar]
- 74.Marcondes FB, Rosa SG, de Vasconcelos RA, Basta A, Freitas DG, Fukuda TY. Rotator cuff strength in subjects with shoulder impingement syndrome compared with the asymptomatic side. Acta Ortopedica Brasileira 2011; 19: 333–7. [Google Scholar]
- 75.Mayerhoefer ME, Breitenseher MJ, Wurnig C, Roposch A. Shoulder impingement: relationship of clinical symptoms and imaging criteria. Clin J Sport Med 2009; 19: 83–9. [DOI] [PubMed] [Google Scholar]
- 76.Michener LA, Subasi Yesilyaprak SS, Seitz AL, Timmons MK, Walsworth MK. Supraspinatus tendon and subacromial space parameters measured on ultrasonographic imaging in subacromial impingement syndrome. Knee Surg Sports Traumatol Arthrosc 2013, pp. 1–7. [DOI] [PubMed] [Google Scholar]
- 77.Min KS, St Pierre P, Ryan PM, Marchant BG, Wilson CJ, Arrington ED. A double-blind randomized controlled trial comparing the effects of subacromial injection with corticosteroid versus NSAID in patients with shoulder impingement syndrome. J Shoulder Elbow Surg 2013; 22: 595–601. [DOI] [PubMed] [Google Scholar]
- 78.Myers JB, Hwang J-H, Pasquale MR, Blackburn JT, Lephart SM. Rotator cuff coactivation ratios in participants with subacromial impingement syndrome. J Sci Med Sport 2009; 12: 603–8. [DOI] [PubMed] [Google Scholar]
- 79.Osteras H, Myhr G, Haugerud L, Torstensen TA. Clinical and MRI findings after high dosage medical exercise therapy in patients with long lasting subacromial pain syndrome: a case series on six patients. J Bodywork Mov Ther 2010; 14: 352–60. [DOI] [PubMed] [Google Scholar]
- 80.Osteras H, Torstensen TA. The dose-response effect of medical exercise therapy on impairment in patients with unilateral longstanding subacromial pain. Open Orthop J 2010; 4: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Park SI, Choi YK, Lee JH, Kim YM. Effects of shoulder stabilization exercise on pain and functional recovery of shoulder impingement syndrome patients. J Phys Ther Sci 2013; 25: 1359–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Paul TM, Soo Hoo J, Chae J, Wilson RD. Central hypersensitivity in patients with subacromial impingement syndrome. Arch Phys Med Rehab 2012; 93: 2206–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Penning LI, de Bie RA, Walenkamp GH. The effectiveness of injections of hyaluronic acid or corticosteroid in patients with subacromial impingement: a three-arm randomised controlled trial. J Bone Joint Surg Br 2012; 94: 1246–52. [DOI] [PubMed] [Google Scholar]
- 84.Phadke V, Ludewig PM. Study of the scapular muscle latency and deactivation time in people with and without shoulder impingement. J Electromyogr Kinesiol 2013; 23: 469–75. [DOI] [PubMed] [Google Scholar]
- 85.Pijls BG, Kok FP, Penning LI, Guldemond NA, Arens HJ. Reliability study of the sonographic measurement of the acromiohumeral distance in symptomatic patients. J Clin Ultrasound 2010; 38: 128–34. [DOI] [PubMed] [Google Scholar]
- 86.Radnovich R, Marriott TB. Utility of the heated lidocaine/tetracaine patch in the treatment of pain associated with shoulder impingement syndrome: a pilot study. Int J Gen Med 2013; 6: 641–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ramos CE, Ferreira FV, Sposito Gde C, Nogueira-Barbosa MH, de Oliveira AS. Intra and inter-examiner reliability of the subacromial impingement index. Skelet Radiol 2010; 39: 35–9. [DOI] [PubMed] [Google Scholar]
- 88.Roy J, Moffet H, Hébert LJ, Lirette R. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Manual Ther 2009; 14: 180–8. [DOI] [PubMed] [Google Scholar]
- 89.Roy JS, Moffet H, McFadyen BJ. Effect of supervised movement training with feedback on the upper limb kinematic patterns of persons with shoulder impingement. J Orthop Sports Phys Ther 2009; 39: A97–8. [Google Scholar]
- 90.Saeed A, Khan M, Morrissey S, Kane D, Fraser AD. Impact of outpatient clinic ultrasound imaging in the diagnosis and treatment for shoulder impingement: a randomized prospective study. Rheumatol Int 2013, pp. 1–7. [DOI] [PubMed] [Google Scholar]
- 91.Santamato A, Solfrizzi V, Panza F, et al. Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of people with subacromial impingement syndrome: a randomized clinical trial [corrected] [published erratum appears in Phys Ther 2009; 89:999]. Phys Ther 2009; 89: 643–52. [DOI] [PubMed] [Google Scholar]
- 92.Seitz AL, McClure PW, Finucane S, et al. The scapular assistance test results in changes in scapular position and subacromial space but not rotator cuff strength in subacromial impingement. J Orthop Sports Phys Ther 2012; 42: 400–12. [DOI] [PubMed] [Google Scholar]
- 93.Shakeri H, Keshavarz R, Arab AM, Ebrahimi I. Clinical effectiveness of kinesiological taping on pain and pain-free shoulder range of motion in patients with shoulder impingement syndrome: a randomized, double blinded, placebo-controlled trial. Int J Sports Phys Ther 2013; 8: 800–10. [PMC free article] [PubMed] [Google Scholar]
- 94.Simsek HH, Balki S, Keklik SS, Ozturk H, Elden H. Does Kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthop Traumatol Turc 2013; 47: 104–10. [DOI] [PubMed] [Google Scholar]
- 95.Smith M, Sparkes V, Busse M, Enright S. Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: is there imbalance and can taping change it? Phys Ther Sport 2009; 10: 45–50. [DOI] [PubMed] [Google Scholar]
- 96.Struyf F, Nijs J, Mollekens S, et al. Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin Rheum 2013; 32: 73–85. [DOI] [PubMed] [Google Scholar]
- 97.Subasi V, Toktas H, Demirdal US, Turel A, Cakir T, Kavuncu V. Water-based versus land-based exercise program for the management of shoulder impingement syndrome. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi 2012; 58: 79–84. [Google Scholar]
- 98.Tate AR, McClure PW, Young IA, Salvatori R, Michener LA. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. J Orthop Sports Phys Ther 2010; 40: 474–93. [DOI] [PubMed] [Google Scholar]
- 99.Tekeoglu I, Ediz L, Hiz O, Toprak M, Yazmalar L, Karaaslan G. The relationship between shoulder impingement syndrome and sleep quality. Eur Rev Med Pharmacol Sci 2013; 17: 370–4. [PubMed] [Google Scholar]
- 100.Theisen C, van Wagensveld A, Timmesfeld N, et al. Co-occurrence of outlet impingement syndrome of the shoulder and restricted range of motion in the thoracic spine – a prospective study with ultrasound-based motion analysis. BMC Musculoskelet Disord 2010; 11: 135–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Timmons MK, Lopes-Albers AD, Borgsmiller L, Zirker C, Ericksen J, Michener LA. Differences in scapular orientation, subacromial space and shoulder pain between the full can and empty can tests. Clin Biomech 2013; 28: 395–401. [DOI] [PubMed] [Google Scholar]
- 102.Toprak U, Ustuner E, Ozer D, et al. Palpation tests versus impingement tests in Neer stage I and II subacromial impingement syndrome. Knee Surg Sports Traumatol Arthrosc 2013; 21: 424–9. [DOI] [PubMed] [Google Scholar]
- 103.van Rensburg KJ, Atkins E. Does thoracic manipulation increase shoulder range of movement in patients with subacromial impingement syndrome? A pilot study. Int Musculoskeletal Med 2012; 34: 101–7. [Google Scholar]
- 104.Wang YC, Wang HK, Chen WS, Wang TG. Dynamic visualization of the coracoacromial ligament by ultrasound. Ultrasound Med Biol 2009; 35: 1242–8. [DOI] [PubMed] [Google Scholar]
- 105.Worsley P, Warner M, Mottram S, et al. Motor control retraining exercises for shoulder impingement: effects on function, muscle activation, and biomechanics in young adults. J Shoulder Elbow Surg 2013; 22: e11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yeldan I, Cetin E, Ozdincler AR. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disabil Rehabil 2009; 31: 935–40. [DOI] [PubMed] [Google Scholar]
- 107.Yeoman TFM, Wigderowitz CA. The effect of psychological status on pain and surgical outcome in patients requiring arthroscopic subacromial decompression. Int J Surg 2011; 9: 369–369. [Google Scholar]
- 108.Ylinen J, Vuorenmaa M, Paloneva J, et al. Exercise therapy is evidence-based treatment of shoulder impingement syndrome. Current practice or recommendation only. Eur J Phys Rehab Med 2013; 49: 499–505. [PubMed] [Google Scholar]
- 109.Youn Hee B, Gyu Chang L, Won Seob S, Tae Hoon K, Suk Min L. Effect of motor control and strengthening exercises on pain, function, strength and the range of motion of patients with shoulder impingement syndrome. J Phys Ther Sci 2011; 23: 687–92. [Google Scholar]
- 110.Zanca GG, Oliveira AB, Saccol MF, Ejnisman B, Mattiello-Rosa SM. Functional torque ratios and torque curve analysis of shoulder rotations in overhead athletes with and without impingement symptoms. J Sports Sci 2011; 29: 1603–11. [DOI] [PubMed] [Google Scholar]
- 111.Zanca GG, Saccol MF, Oliveira AB, Mattiello SM. Shoulder internal and external rotations torque steadiness in overhead athletes with and without impingement symptoms. J Sci Med Sport 2013; 16: 433–7. [DOI] [PubMed] [Google Scholar]
- 112.Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev 2013; 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Neer CS., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am 1972; 54: 41–50. [PubMed] [Google Scholar]
- 114.Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury 2013; 44: S26–S32. [DOI] [PubMed] [Google Scholar]