Abstract
Background
The surgical management of massive rotator cuff tears remains a challenge. It is suggested that, even in a massive tear that appears irreparable, attempting to repair it as much as possible can be helpful in improving functional outcomes. However the results can be short term and variable. The purpose of our study was to determine if human tissue allograft bridged repair of massive irreparable rotator cuff tears to achieve a complete repair produces similar outcomes compared to partial repair alone.
Methods
We prospectively reviewed outcome scores in 13 patients who underwent partial repair alone for massive irreparable rotator cuff tears and compared them to 13 patients who had partial repairs bridged with allograft. Oxford and Constant scores were compared pre-operatively and at a minimum follow-up of 2 years (range 2 years to 5 years).
Results
The mean improvement in the Constant score at final follow-up compared to pre-operative scores was 27.7 points in the partial repair group and 42.8 points in the allograft group (p < 0.01). The Oxford Shoulder Score improved mean of 19.3 points in the partial repair group and 29 points in the allograft group (p < 0.02) at 2 years.
Conclusions
Human tissue matrix allograft provides a better outcome for open bridging of irreparable rotator cuff tears than partial repair alone.
Keywords: allograft, bridging repair, GraftJacket®, massive rotator cuff tear, outcome, partial repair
Introduction
Massive irreparable rotator cuff tears continue to present a challenging problem. Many different methods have been described to manage such tears including non-operative, surgical debridement,1–3 partial repair,4,5 muscle advancement,6 tendon transfers7 and allograft substitution.8,9 Xenograft,10 allograft and synthetic materials11 have been tried to augment the cuff repair with the expectation of better healing and improved results. However, the use of porcine dermal collagen and small intestinal submucosa were found to be ineffective as a result of graft rejection.12 The use of human tissue allograft as an augmentation graft13 has been shown to be effective but the efficacy of its use as a bridging graft after partial repair of massive rotator cuff tears is not clear. The lack of clear evidence on how to manage irreparable massive cuff tears especially in patients younger than 65 years has lead to a plethora of suggested treatments with variable results for the patients.
Where it is not possible to achieve a complete repair of massive rotator cuff tears despite mobilization and margin convergence of the tendons, it has been suggested that attempting to repair it as much as possible to convert it into a functional rotator cuff tear by re-creating a balanced forced couple can be helpful in reducing pain, as well as improving functional outcomes.14 However, partial repair is associated with high rates of structural failure of the repair and a modest functional improvement.3
It has been suggested previously that the repair of the massive rotator cuff tears can be bridged with an human tissue allograft15 with good results.9 However, it remains unclear whether adding an allograft provides better functional results compared to partial repair alone as to our knowledge partial repair alone has not been directly compared with partial cuff repair bridged with allograft. We present our results of partial repair of massive irreparable rotator cuff tears versus bridging reconstruction with allograft comparing patient reported Oxford Shoulder Score and Constant score.
Materials and methods
Symptomatic patients with massive rotator cuff tears (>5 cm) who had failed conservative management and were suitable for operative management were considered for inclusion in this study. All patients received a course of physiotherapy supervised by a qualified therapist and one steroid injection. If the patients continued to have symptoms or the symptoms recurred despite at least 6 months of non-operative treatment (steroid injection, physiotherapy), they were then offered surgery.
All patients were prospectively reviewed for signs and symptoms of massive rotator cuff tear (significantly reduced active movements) in the outpatient clinics. The patients had a radiograph to exclude proximal migration of humeral head or glenohumeral arthritis. The patients had a magnetic resonance imaging (MRI) scan pre-operatively to identify the size, retraction and the fatty infiltration in the torn cuff muscles. The tears were classified as per classification of Goutallier et al.16 The decision to include patient in the study was taken based on clinical examination and MRI scan that adequately shows whether the cuff is repairable or not. No patient who was included pre-operatively was excluded at the time of surgery. Patients were included in the study if the clinical examination and MRI scan showed that there was a massive cuff tear not amenable to complete repair. Patients who had previous shoulder surgeries, with established glenohumeral osteoarthritis and patients with cuff tears, which could be completely repaired, were excluded from this study.
From 2004 to 2007, 13 patients (nine men and four women) with mean age 59 years (45 years to 67 years) years underwent partial repair only (Group A, partial repair group) of a massive rotator cuff tear (>5 cm) in our unit. After the introduction of GraftJacket® (Wright Medical UK Ltd, Letchworth Garden City, UK) at our hospital in 2008 to 2012, 13 patients (nine men and four women) 57 years (45 years to 68 years) years (Group B, allograft group) had a partial repair of the irreparable massive rotator cuff tears, although with the addition of GraftJacket® allograft to bridge the repair. Patients were explicitly informed of the use of human allograft for bridging of the rotator cuff and they consented for the use of graft. The departmental review committee approved the use of the allograft for bridging of irreparable rotator cuff tears and this product was licensed for this use in rotator cuff tears. As the outcome data was collected as part of an on-going audit of senior authors practise, institutional review board approval was not deemed necessary. There was no involvement of the industry, financial or otherwise, in any aspect of this study. Published results on safety of use of this allograft, as a bridging graft in rotator cuff tears were available from other centres before we commenced the trial in our centre. Three patients out of the thirteen patients in each group had bilateral massive irreparable cuff tears and had partial repair on one side and allograft augmented repair on the other shoulder.
The patients in both groups were well matched pre-operatively for demographics variables. There were no patients lost to follow-up. There were eleven Goutallier 2 and two Goutallier 3 cuff tears in patients in Group A and in Group B, there were ten Goutallier 2 and three Goutallier 3. All patients had both supraspinatous and infraspinatous full thickness tendon tears. Subscapularis was intact in all patients without any full thickness tear. There was retraction of tendon in all the patients with the stump around the level of head on the MRI scan results (Patte stage 2). All tears were classed as massive tears with more than 5 cm in diameter in both anteroposterior and mediolateral direction. In Group A, three biceps tendons were found ruptured and in Group B, two biceps tendons were ruptured. After partial repair (margin convergence) of the tears, the residual gap was on average 2.1 cm (2.0 cm to 2.3 cm) in diameter in Group A and 2.5 cm (2.3 cm to 2.6 cm) in Group B.
Surgical method
Surgeries were performed with patients in a beach chair position using an anterosuperior approach to the shoulder with a deltoid split through raphe between anterior and the middle third. The deltoid was minimally elevated from acromion along with sliver of periosteum. This was later repaired with interosseous suture. Acromioplasty was also performed in all cases. A single surgeon (RP) performed all the operations.
The rotator cuff edges were identified and debrided and the size of the cuff tear confirmed. Retraction of the tendon was measured according to Patte:17 Stage 1, stump at level with the footprint; Stage 2, stump at level of humeral head; and Stage 3, stump was at level of glenoid. The long head of the biceps tendon was found to have already ruptured in most cases but, if still present and lying in the groove, the tendon was debrided but no attempt was made to either tenotomize or tenodese the biceps tendon. If the tendon was dislocated in the joint, soft tissue tenodesis was carried out.
Allograft procedure
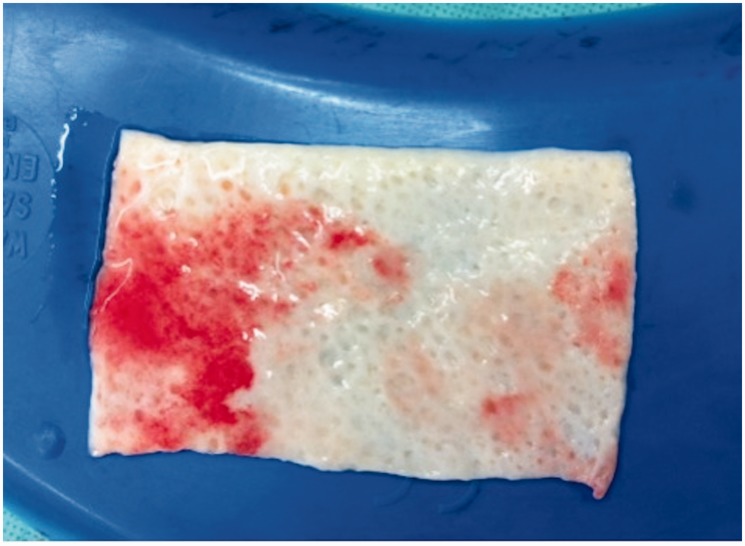
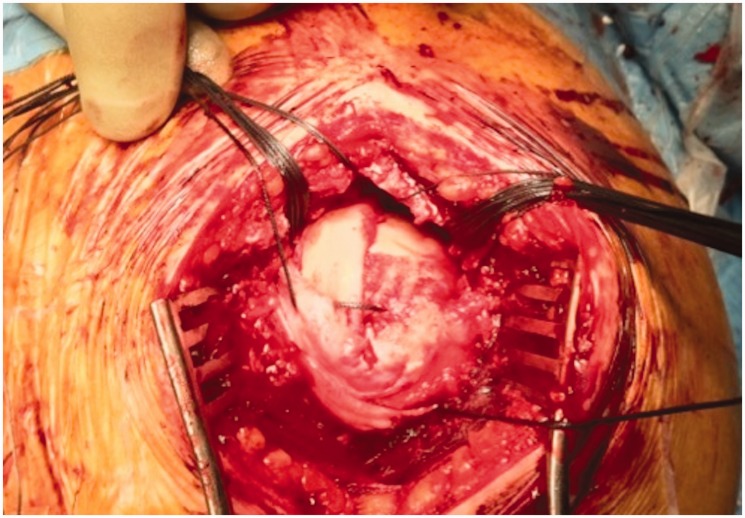
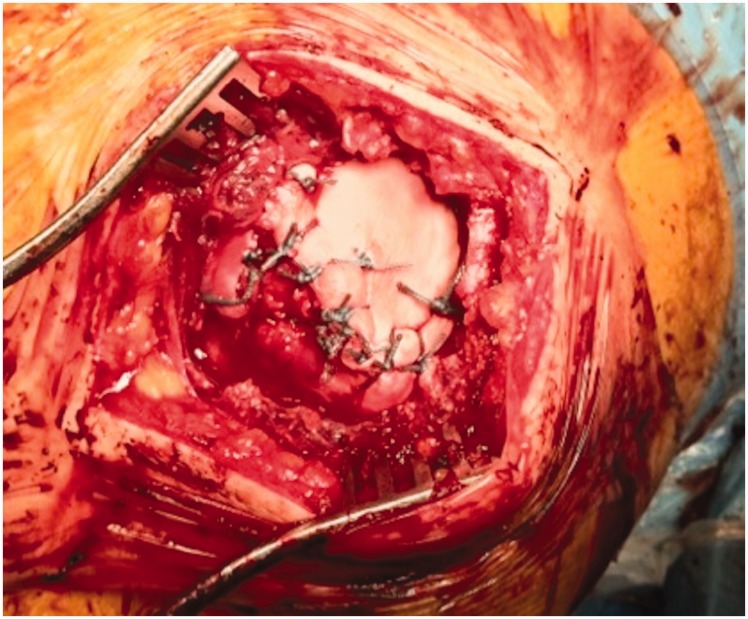
Once it was determined that the rotator cuff was irreparable, the allograft (GraftJacket®) was opened and inserted in saline solution for 10 minutes (Figure 1). Meanwhile the cuff was sufficiently mobilized and cleared of any adhesions. Sutures (No. 2; Ethibond; Ethicon, Somerville, NJ, USA) were then inserted circumferentially into the edges of the cuff to allow the cuff to be manipulated (Figure 2). The cuff foot print area on the humerus was freshened to bleeding bone to facilitate healing of the repaired cuff. Surgeon first achieved a partial repair with margin convergence of the cuff and using two bone anchors (GII; Mitek Depuy, Raynham, MA, USA) and three or four intra-osseous sutures to position the repaired cuff onto bone. The residual defect in the cuff was measured and a template of the defect made. The allograft was then cut to match the template and applied onto the residual cuff defect with the shiny dermal side facing down on to freshened bone. The previously inserted sutures in the cuff were then passed into the allograft to secure it to the surrounding cuff using interrupted and continuous sutures. Two anchors (GII; Mitek Depuy) and four to five intraosseous sutures were inserted into the footprint area to secure the allograft to bone (Figure 3). The aim was to completely bridge the defect and to appropriately tension the allograft by laying it snug on to the bone underneath without any wrinkles. No knots were left under the graft jacket. This was a single row repair with simple sutures.
Figure 1.
GraftJacket® allograft soaked in saline before application.
Figure 2.
The residual defect in the rotator cuff tear after partial repair showing the sutures placed through the edge of the rotator cuff.
Figure 3.
The allograft was stitched to the margins of the cuff defect and using anchors and intra-osseous sutures to the footprint to achieve a watertight bridging repair.
Partial repair procedure
The partial repair procedure followed the same sequence as the allograft procedure except after performing a partial repair of the cuff, there remained a residual defect in the cuff of at least 1 cm.
The same postoperative rehabilitation protocol was used for all patients. A polysling was used for 6 weeks postoperatively to immobilize the shoulder and, at 6 weeks, the patients started to mobilize the shoulder progressing from assisted active exercises to full active exercises under the supervision of a physiotherapist. At 3 months, the strengthening exercises were initiated. The partial repair group was followed up for 2 years to 5 years, whereas the allograft group completed a follow-up between 2 years and 3 years. All group B patients underwent an ultrasound scan 2 years postoperatively (as MRI scans could not be performed due to metallic anchors).
The outcome measures used were the Oxford Shoulder Score and Constant score (Absolute constant score used, a spring balance used to measure strength). All patients completed these scores pre-operatively 2 weeks before surgery at the time of pre-operative assessment and were completed again at a minimum of 2 years after surgery. Independent assessors who were not involved in surgery administered the outcome scores.
The data was analyzed using SPSS, version 16 (SPSS Inc, Chicago, IL, USA). As the data showed a skewed distribution, nonparametric tests were used to analyze the groups. Pre- and postoperative data were compared using Wilcoxon’s signed ranks test, and data between groups were analyzed using the Mann–Whitney U-test.
Results
Both groups of patients showed significant improvement compared to pre-operative scores (p < 0.01) (Table 1). The allograft group (B) showed a greater improvement in both Oxford Shoulder Score and Constant score compared to the partial repair group (p < 0.01). There were no significant complications in either group of patients. Four patients (30%) in Group B suffered a retear with sizes ranging from 1.2 cm to 1.8 cm. However, there was no further reduction in Oxford Shoulder Score and Constant score in cases of re-rupture in the allograft group at 2 years.
Table 1.
Mean and range (in brackets) of pre-operative and postoperative outcome scores 2 years after surgery for both groups.
| Partial repair | Partial repair + Allograft | ||||
|---|---|---|---|---|---|
| (n = 13) | (n = 13) | p-value | |||
| Oxford Shoulder Score | |||||
| Baseline | Mean (SD) (range) | 17.8 (3.6) (10–22) | 14.9 (3.5) (10–22) | 0.17 | |
| Final follow-up | Mean (SD) (range) | 37.1 (2.4) (34–40) | 43.9 (2.4) (38–46) | 0.01 | |
| p-value Baseline versus Final follow-up | 0.009 | 0.005 | |||
| CONSTANT Score | |||||
| Baseline | Mean (SD) (range) | 43.1 (3.9) (36–48) | 41.2 (3.1) (37–48) | 0.48 | |
| Final follow-up | Mean (SD) (range) | 70.8 (5.3) (62–78) | 83.9 (6.0) (70–91) | <0.01 | |
| p-value Baseline versus Final follow-up | 0.01 | 0.005 | |||
Discussion
Allograft augmentation with rotator cuff tears has been previously reported in the literature8,9 to produce good results in patients with massive, irreparable rotator cuff tears, although it is not known how this compares to only partial repair of the rotator cuff. We compared the outcome of allograft-bridged graft with partial repair alone in patients with massive cuff tears. Prior to using allograft, we performed partial repair of massive irreparable rotator cuff tears by reducing the size of the defect by margin convergence and side-to-side re-approximation of the rotator cuff, as well as securing the cuff to bone with anchors and intra-osseous sutures leaving a defect in the cuff that could not be closed. When using allograft, we could cover the residual defect with the allograft and complete the repair and functionally patients reported improvement in strength and motion as measured by Oxford Shoulder Score and Constant score compared to only partial repair group.
Our study has shown that allograft bridged repairs produce greater improvement in outcome scores at 2 years postoperatively compared to partial repair alone. It has been reported that allograft acts as a biological scaffold spanning the residual cuff deficiency and allowing tissue ongrowth to produce a complete repair of rotator cuff tears.18
Burkhart et al.4 in 1994 introduced the concept of the ‘functional rotator cuff tear’, which was described as an anatomically deficient yet biomechanically intact rotator cuff. This has essentially formed the basis of partial rotator cuff repair, producing a functional rotator cuff capable of force transmission, but which is still anatomically deficient with a residual unrepaired hole in the cuff. Burkhart reported the results of partial repair as producing good functional benefits in patients with massive rotator cuff tears (average of 20.1 cm2). In his study, UCLA (University of California at Los Angeles) shoulder scores improved from a mean 9.8 pre-operatively to 27.6 postoperatively. Other studies have subsequently reported improvements in patients treated with partial repair with one study showing ASES (American Shoulder and Elbow Surgery) scores improving from a mean of 41 pre-operatively to 80 at a minimum 2 years postoperatively. The difficulty in comparing the results from the studies is the variable outcome measures used, although the study by Berth et al.3 did use the Constant score and they reported an improvement from a mean of 45.9 pre-operatively to 72.8 at a mean 24 months postoperatively. Our study has shown similar improvements in the group of patients having a partial repair with a mean improvement in Constant score from 43.2 to 70.9.
All of our patients had an acromioplasty performed as part of their procedure and acromioplasty with debridement of the cuff tear has been reported in previous studies to produce good outcomes in terms of pain relief and improved function.2 However, the initial improvement in outcome of these patients has been shown to deteriorate at longer-term follow-up. The study by Berth et al.3 comparing debridement with partial repair showed that the Constant score improved from 37 points pre-operatively to 61.3 at 16 months for the debridement group, although these results deteriorated to 50.4 points at 24 months follow-up. Therefore, we feel that this procedure alone does not produce the significant improvements seen in our group of patients at 2 years follow-up.
In the Allograft group, three patients suffered a retear of the rotator cuff of 1.2 cm to 1.8 cm measured on ultrasound scan, although there was no significant deterioration in function compared to other patients in the group at 2 years as measured by Oxford Shoulder Score and Constant score. This could be because the size of the retear was much smaller compared to the initial tear of more than 5 cm. In addition, after surgery, by the time the retear happened, the patients were able to undergo rehabilitation with improvement in symptom and restoration of function in the rotator cuff muscles. In the published literature, retear also occurs in 40% to 60%19,20 of patients who undergo complete repair of smaller rotator cuff tears but the functional outcome is not significantly different between patients who have a retear compared to ones with complete healing of the cuff after surgical repair.21
Bridging an irreparable massive cuff tear with GraftJacket® has been reported to produce significant improvements in shoulder pain and function in a number of studies. Bond et al.8 reported their preliminary results of the first 16 patients having arthroscopic GraftJacket® augmentation for massive rotator cuff tear and reported an improvement in Constant scores from 53.8 to 84 and UCLA scores improving from 18.4 to 30.4 postoperatively. This is consistent with our results, but our patients had a worse pre-operative Constant score of 41.2 but, despite this, still showed significant improvement in the Constant score postoperatively to 83.9. This level of improvement is comparable to a previous study22 of patients having complete repair of large or massive rotator cuff tears in which the Constant score improved from 36 to 68 postoperatively.
When comparing the outcomes of massive rotator cuff repair bridged with partial repair of the rotator cuff, patients having one procedure on each shoulder represent an interesting group. Our study had three such patients and they all reported subjectively that the allograft augmented shoulder felt functionally stronger than the shoulder having partial repair. The change in Oxford Shoulder Score in these patients was from a mean (SD) of 25.3 (4.4) points to 30.7 (4.2) points and the change in Constant score was from a mean of 29.7 (1.4) points to 40.7 (2.5) points (p = 0.05).
Wong et al.9 more recently reported on 45 patients having arthroscopic GraftJacket® repair and found mean UCLA scores improving from 18.4 to 27.5 and a mean ASES score of 84.1 at a minimum 2 years postoperatively. In both of these studies, the allograft-augmented repair was performed arthroscopically but all our patients had an open procedure. In our hands, an open repair allowed us to achieve better tensioning of the allograft and a more secure repair.
GraftJacket® allograft consists of human dermal tissue with all cellular components removed, but with an intact matrix to retain collagen, proteoglycans and elastin. It is believed that this process reduces the inflammatory response and allows revascularization and cellular repopulation.23 GraftJacket® is reported to work by acting as a biologic scaffold allowing pluripotential cells from the adjacent bone marrow to migrate onto the tissue and form a neotendon. In the study by Bond et al.,8 a biopsy in one patient did confirm neotendon formation over the allograft at 4 months postoperatively. A postoperative MRI scan was performed in all patients in the same study and this confirmed presence of GraftJacket® at 1 year postoperatively in 13 out of 16 patients. Other biological scaffolds that have been studied for use in rotator cuff tear include porcine small intestine submucosa (Restore Orthobiologic soft tissue implant, DePuy Orthopaedics Inc., Indiana, USA) and porcine dermal Xenograft (Zimmer collagen repair patch, Zimmer, Warsaw, Indiana, USA). Clinical studies have shown that both these scaffolds can elicit a severe inflammatory response and subsequent failure of the graft.10,12,24
The present study does have some limitations. It is a nonrandomized, nonblinded comparative study with differing follow-up times with the possibility of performance bias and the graft group results could decrease over time. We have as yet not performed postoperative MRI scans in patients having GraftJacket® augmentation but, clinically, there is no justification for a postoperative MRI as the patients report good outcome. There are limitations with the use of Constant score as the method of strength measurement is not standardized and the values were not corrected for age or sex. However, we have used an additional Oxford shoulder score for outcome assessment, that is designed as a patient independent questionnaire and has been observed to be a robust tool for the quantitative assessment and tracking of patient outcomes after rotator cuff surgery.25 We have included patients who underwent partial repair on one shoulder and allograft repair on the other side in this study, although there is potential for bias as the patients were not blinded. The follow-up period for the two groups is also variable but this reflects the time periods during which each procedure was favoured with Graft Jacket being increasingly used more recently. Although the allograft is more expensive, we feel this can be justified by the better results we have achieved to date; however, we need more long-term data to confirm if these early results are maintained.
Conclusions
Our study has shown that both partial repair and Graft GraftJacket® allograft reconstruction are effective methods to treat patients with massive, irreparable rotator cuff tears. Patients having GraftJacket® allograft show a greater improvement in Constant score and Oxford Shoulder Score at a minimum of 2 years postoperatively compared to patients having just partial repair. Future long-term studies are required to evaluate outcome and improvement in shoulder function with the use of allograft as bridging graft for massive irreparable rotator cuff tears.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Level of evidence
Level 3
References
- 1.Melillo AS, Savoie FH, III, Field LD. Massive rotator cuff tears: debridement versus repair. Orthop Clin North Am 1997; 28: 117–24. [DOI] [PubMed] [Google Scholar]
- 2.Rockwood CA, Jr, Williams GR, Jr, Burkhead WZ., Jr Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg 1995; 77: 857–66. [DOI] [PubMed] [Google Scholar]
- 3.Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 2010; 11: 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy 1994; 10: 363–70. [DOI] [PubMed] [Google Scholar]
- 5.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg 2005; 14: 121–7. [DOI] [PubMed] [Google Scholar]
- 6.Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg 1985; 67: 974–9. [PubMed] [Google Scholar]
- 7.Gerber C, Hersche O. Tendon transfers for the treatment of irreparable rotator cuff defects. Orthop Clin North Am 1997; 28: 195–203. [DOI] [PubMed] [Google Scholar]
- 8.Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: technique and preliminary results. Arthroscopy 2008; 24: 403–9 e1. [DOI] [PubMed] [Google Scholar]
- 9.Wong I, Burns J, Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg 2010; 19: 104–9. [DOI] [PubMed] [Google Scholar]
- 10.Soler JA, Gidwani S, Curtis MJ. Early complications from the use of porcine dermal collagen implants (Permacol) as bridging constructs in the repair of massive rotator cuff tears. A report of 4 cases. Acta Orthop Belgica 2007; 73: 432–6. [PubMed] [Google Scholar]
- 11.Visuri T, Kiviluoto O, Eskelin M. Carbon fiber for repair of the rotator cuff. A 4-year follow-up of 14 cases. Acta Orthop Scand 1991; 62: 356–9. [DOI] [PubMed] [Google Scholar]
- 12.Iannotti JP, Codsi MJ, Kwon YW, Derwin K, Ciccone J, Brems JJ. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J Bone Joint Surg 2006; 88: 1238–44. [DOI] [PubMed] [Google Scholar]
- 13.Barber FA, Burns JP, Deutsch A, Labbe MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy 2012; 28: 8–15. [DOI] [PubMed] [Google Scholar]
- 14.Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 2012; 28: 761–8. [DOI] [PubMed] [Google Scholar]
- 15.Modi A, Singh HP, Pandey R, Armstrong A. Management of irreparable rotator cuff tears with the GraftJacket allograft as an interpositional graft. Shoulder Elbow 2013; 5: 188–94. [Google Scholar]
- 16.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Rel Res 1994, pp. 78–83. [PubMed] [Google Scholar]
- 17.Patte D. Classification of rotator cuff lesions. Clin Orthop Rel Res 1990; 254: 81–6. [PubMed] [Google Scholar]
- 18.Adams JE, Zobitz ME, Reach JS, Jr, An KN, Steinmann SP. Rotator cuff repair using an acellular dermal matrix graft: an in vivo study in a canine model. Arthroscopy 2006; 22: 700–9. [DOI] [PubMed] [Google Scholar]
- 19.Mansat P, Cofield RH, Kersten TE, Rowland CM. Complications of rotator cuff repair. Orthop Clin North Am 1997; 28: 205–13. [DOI] [PubMed] [Google Scholar]
- 20.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Rel Res 1997; 344: 275–83. [PubMed] [Google Scholar]
- 21.Kim KC, Shin HD, Cha SM, Park JY. Repair integrity and functional outcome after arthroscopic conversion to a full-thickness rotator cuff tear: articular- versus bursal-side partial tears. Am J Sports Med 2014; 42: 451–6. [DOI] [PubMed] [Google Scholar]
- 22.Hanusch BC, Goodchild L, Finn P, Rangan A. Large and massive tears of the rotator cuff: functional outcome and integrity of the repair after a mini-open procedure. J Bone Joint Surg 2009; 91: 201–5. [DOI] [PubMed] [Google Scholar]
- 23.Longo UG, Lamberti A, Maffulli N, Denaro V. Tendon augmentation grafts: a systematic review. Br Med Bull 2010; 94: 165–88. [DOI] [PubMed] [Google Scholar]
- 24.Walton JR, Bowman NK, Khatib Y, Linklater J, Murrell GA. Restore orthobiologic implant: not recommended for augmentation of rotator cuff repairs. J Bone Joint Surg 2007; 89: 786–91. [DOI] [PubMed] [Google Scholar]
- 25.Olley LM, Carr AJ. The use of a patient-based questionnaire (the Oxford Shoulder Score) to assess outcome after rotator cuff repair. Ann Royal Coll Surg Eng 2008; 90: 326–31. [DOI] [PMC free article] [PubMed] [Google Scholar]