Abstract
Purpose
Underestimating one’s weight is often seen as a barrier to weight loss. However, recent research has shown that weight under-perception may be beneficial, with lower future weight gain and fewer depressive symptoms. Here, we examine the relationship between adolescent weight under-perception and future blood pressure.
Methods
Using data from the National Longitudinal Study of Adolescent to Adult Health, we obtained a nationally representative sample of 2463 adolescents with overweight and obesity (students in grades 8–12 in 1996). We used multivariable linear regression to prospectively examine the relationship between weight self-perception in adolescence and blood pressure in adulthood (year 2008; follow-up rate 80.3%), controlling for age, gender, race/ethnicity, smoking, alcohol consumption, education level, household income, and BMI. Additional analyses were stratified by gender and race/ethnicity.
Results
Youth with overweight/obesity who under-perceived their weight had lower blood pressure in adulthood than those who perceived themselves to be overweight. The decrease in systolic blood pressure was −2.5 mmHg (95% CI:−4.3,−0.7; p=0.006). Although the interaction by gender was statistically insignificant (p=0.289), important differences appeared upon stratification by gender. Young men showed no significant difference in adult blood pressure related to weight self-perception. Conversely, in young women, weight under-perception was associated with an average decrease in systolic blood pressure of −4.3 mmHg (95% CI:−7.0,−1.7; p=0.002).
Conclusions
Contrary to conventional wisdom, weight under-perception is associated with improved health markers in young women. The observed differences in blood pressure are clinically relevant in magnitude, and interventions to correct weight under-perception should be re-examined for unintended consequences.
Keywords: overweight, obesity, blood pressure, self concept, body image, adolescent
Childhood obesity is widely regarded as a public health crisis in the United States, and numerous studies have shown that individuals with overweight or obesity in childhood are at higher risk for hypertension and other adverse cardiovascular events in adulthood.[1,2] These findings have spurred efforts to inform parents when their children are overweight and to provide weight-loss interventions at an early age.[3,4] Obesity also has psychological consequences: children and adolescents with overweight or obesity are more likely to be teased by their peers and experience low self-esteem, body dissatisfaction, depressive symptoms, and suicidal ideation.[5,6] These psychosocial factors impact the health trajectories of affected youth, including their future weight and risk of eating disorders.[7,8]
Weight self-perception provides a window to study the interplay of these psychosocial and physical consequences. Despite efforts to inform youth of their weight status, between 20% and 80% of American youth with clinical overweight/obesity perceive themselves to be normal weight. [4,9,10] This incongruence between clinical weight category and self-perception, referred to as weight misperception, is often assumed to be detrimental to health maintenance.[11–13] Indeed, numerous studies have found that adolescents with overweight/obesity who under-perceive their weight are less likely to report that they are exercising, dieting, and trying to lose weight.[9,14] At the same time, self-perception as overweight is associated with binge eating and eating disorder psychopathology.[15,16]
While multiple studies have examined the relationship between weight misperception and self-reported health behavior, investigators have only recently begun examining the relationship between weight misperception and measurable health markers. The results are intriguing: two recent longitudinal cohort studies showed that, contrary to common belief, people with overweight/obesity who underperceive their weight go on to gain significantly less weight in the future than those who perceive themselves as overweight.[17,18] Given the known relationships between weight and blood pressure, psychosocial stress and blood pressure, and weight stigma and psychosocial stress, we hypothesized that weight self-perception might similarly affect future blood pressure.[5,19,20] We further hypothesized that the relationship between weight self-perception and future blood pressure might be mediated by the known relationship between weight self-perception and future BMI. Finally, given the increased weight stigma that women encounter, higher levels of body dissatisfaction among White (as compared to Black) women, and known variation in rates of weight misperception and weight control behaviors by gender and race/ethnicity, we hypothesized that the relationship between weight misperception and blood pressure might be modified by gender and race/ethnicity.[10,21–23]
Current clinical practice relies, in part, on the assumption that making patients aware of their weight status will eventually benefit their long-term health. In this study, we sought to test this assumption by examining the relationship between weight self-perception in adolescence and blood pressure in young adulthood.
Methods
We used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally-representative, longitudinal survey of adolescents in grades 7–12 in the school year 1994–1995 (Wave I). The survey was approved by the institutional review board at the University of North Carolina Chapel Hill, and the interviewers obtained informed assent from the participants and informed consent from their parents in Wave I.[24] Secondary analysis was approved by the Boston Children’s Hospital institutional review board. Our analysis uses data from Wave II (the first wave with measured height and weight), conducted in 1996 with 14,738 participants, and Wave IV, conducted in 2008 with a follow-up rate of 80.3%.[25] Participants were between the ages of 24 and 32 in Wave IV.[24]
We calculated BMI in Wave II using height and weight measured by the interviewer, and adolescents were categorized as underweight, normal weight, overweight, or obese based on BMI-for-age cut-offs recommended by the Centers for Disease Control in the United States.[26] The initial sample of participants with available data and sample weights for Waves II and IV had 9421 individuals.[27] We limited our analysis to individuals with overweight/obesity in adolescence, excluding 6482 individuals with normal weight or underweight and 149 individuals who were missing BMI data. We determined weight self-perception in Wave II using participants’ response to the question, “How do you think of yourself in terms of weight?” (possible responses: very overweight, overweight, normal weight, underweight, and very underweight). Those who perceived themselves as normal weight (despite having a BMI in the clinically overweight/obese range) were termed “under-perceivers.” Those who perceived themselves as underweight or very underweight (71 individuals) were excluded from the sample, as the sample size of these “extreme under-perceivers” was too small to analyze. To investigate the possibility of selection bias, we calculated the percentage of our sample population that switched into the normal weight category between Waves II and IV, stratified by weight self-perception.
For outcome data, we used systolic and diastolic blood pressure data gathered in Wave IV. These blood pressure measurements were taken by trained Add Health interviewers using an automatic oscillometric monitor approved by the British Hypertension Society (BP 3MC1-PC_IB; MicroLife USA, Inc., Dunedin, FL).[28] Three blood pressure readings were taken, 30 seconds apart, while the participant was seated at rest for at least five minutes. The last two readings were double-entered and averaged to obtain the reported measure. Since blood pressure changes during pregnancy, we excluded 86 women who were pregnant and 4 women who did not report their pregnancy status, as well as 112 individuals with missing blood pressure data.
We analyzed the longitudinal relationship between weight self-perception in adolescence and blood pressure in adulthood using linear regression, controlling for BMI in Wave II, age in Wave IV, race/ethnicity (White, Black, Latino/a, Asian, or other), smoking in Wave IV (dichotomized based on self-report of smoking at least once in the past 30 days), frequent alcohol consumption in Wave IV (dichotomized based on self-report of drinking an average of three or more times per week), education level in Wave IV (categorized as less than high school, high school degree or equivalent, some college, and college degree or higher), and Wave I household income (as a percentage of the federal poverty level, imputed when missing; Wave I data was used because household income information was not gathered in Wave II). We did not control for income in Wave IV because it was poorly correlated to other measures of socioeconomic status, most likely because respondents had not reached their full earning potential. Individuals that were missing data for any of these covariates (60 individuals) were excluded from the final analytic sample.
For the subgroup analyses by gender (female and male) and race (White, Black, and Latino/a; other racial groups had sample sizes too small to analyze), we ran tests of interaction, then divided the entire dataset into non-overlapping subpopulations and ran linear regressions on each subpopulation, controlling for all the variables listed above. As additional sensitivity analyses, we stratified by weight category (overweight vs. obese) and antihypertensive use, to confirm robustness across these categories. We defined antihypertensives to include beta-blockers, calcium channel blockers, diuretics, angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, anti-adrenergics, vasodilators, or antihypertensive combination medications as inventoried in the home by the Add Health field interviewer using Lexicon Plus (Lexi-Comp, Inc., Hudson, OH).[28]
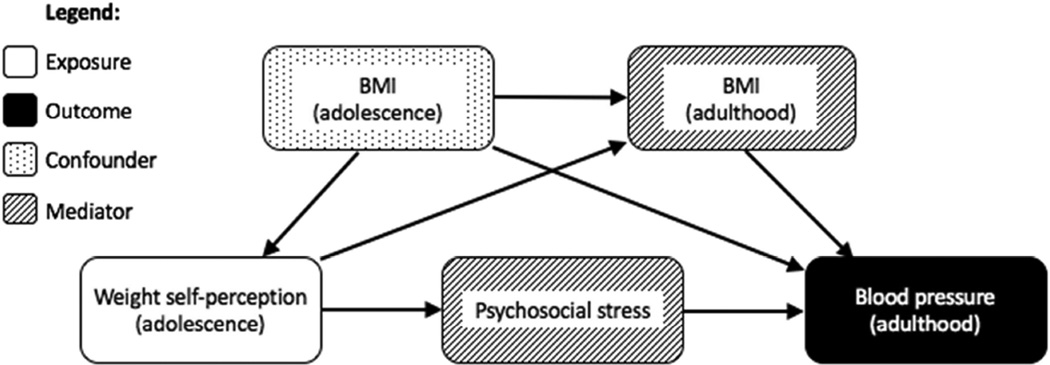
Finally, we performed a mediation analysis to disentangle the relationship between adolescent weight self-perception, adult blood pressure, and adult BMI. Figure 1 shows a directed acyclical graph laying out our hypothesized relationship between weight self-perception, BMI, and blood pressure. Following the principles set out in VanderWeele’s approach to mediation analysis, we added change in BMI (Wave IV BMI-Wave II BMI) as a covariate.[29] Given the known relationships between adolescent weight self-perception and adult BMI as well as between BMI and blood pressure, this analysis allowed us to evaluate the relationship between adolescent weight self-perception and adult blood pressure that is not mediated by differences in adult BMI.
Figure 1. Directed acyclical graph.
Directed acyclic graph showing the hypothesized relationship between weight self-perception, BMI, and blood pressure. Lines with arrowheads indicate the hypothesized direction of causality.
The final analytic sample comprised 2463 respondents (1280 female and 1183 male). All data analysis was performed in STATA (version 12, College Station, TX). Survey weights were employed to account for the survey’s non-random sampling method.
Results
Table 1 shows the demographic characteristics of the analytic sample, stratified by gender and weight self-perception. Just over half our sample population was overweight in adolescence; the remainder were obese. In adolescence, 39.8% of boys and 17.7% of girls perceived themselves as normal weight. Youth with overweight were more likely to view themselves as normal weight compared to youth with obesity. The vast majority of these adolescents remained overweight or obese in adulthood; only 5.0% became normal weight. The raw rate of switching into the normal weight category by adulthood was higher among under perceivers than among those who self-perceived as overweight (9.4% vs. 3.2%). In young adulthood, over one-fifth of our sample had blood pressure in the hypertensive range.
Table 1.
Demographic, Health, and Health Behavior Characteristics by Gender and Weight Self-Perception
| Female | Male |
Self-perception: Normal Weight |
Self-perception: Overweight |
Total | |||||||
|
Sampled frequency, unweighted (n=1280) |
Weighted percent or mean (SE a) |
Sampled frequency, unweighted (n=1183 |
Weighted percent or mean (SE) |
Sampled frequency, unweighted (n=704) |
Weighted percent or mean (SE) |
Sampled frequency, unweighted (n=1759) |
Weighted percent or mean (SE) |
Sampled frequency, unweighted (n=2463) |
Weighted percent or mean (SE) |
||
| Race/ethnicity | White | 606 | 66.2% (3.29) | 631 | 58.4% (3.70) | 332 | 56.8% (3.76) | 905 | 65.0% (3.31) | 1237 | 62.6% (3.26) |
| Black | 347 | 13.4% (2.00) | 204 | 22.2% (3.07) | 198 | 23.0% (3.27) | 353 | 15.3% (2.23) | 551 | 17.5% (2.38) | |
| Asian | 43 | 2.9% (0.85) | 69 | 1.2% (0.54) | 31 | 2.4% (1.03) | 81 | 2.0% (0.69) | 112 | 2.1% (0.64) | |
| Latino/a | 189 | 11% (2.05) | 192 | 12.6% (2.08) | 92 | 9.8% (2.15) | 289 | 12.5% (1.98) | 381 | 11.7% (1.89) | |
| Other/Multiracial | 95 | 6.5% (1.15) | 87 | 5.5% (0.84) | 51 | 8.0% (1.38) | 131 | 5.3% (0.82) | 182 | 6.1% (0.81) | |
| Wave II | Female | Male |
Self-perception: Normal Weight |
Self-perception: Overweight |
Total | ||||||
| BMIb | Average BMI | - | 29.4 (0.24) | - | 28.6 (0.26) | - | 26.3 (0.15) | - | 30.1 (0.19) | - | 29.0 (0.19) |
| Weight Status | Overweight | 708 | 55.8% (2.01) | 626 | 53.1% (2.02) | 555 | 79.6% (1.97) | 779 | 43.9% (1.47) | 1334 | 54.4% (1.36) |
| Obese | 572 | 44.2% (2.01) | 557 | 46.9% (2.02) | 149 | 20.5% (1.97) | 980 | 56.1% (1.47) | 1129 | 45.6% (1.36) | |
| Age | Average age | - | 15.8 (0.15) | - | 16.0 (0.15) | - | 15.8 (0.15) | - | 16.0 (0.13) | - | 15.9 (0.13) |
| HH incomec |
Average % FPL
d
(data from Wave I) |
- | 250% FPL (15.09) |
- | 250% FPL (15.09) |
- | 244% FPL (10.6) |
- | 263% FPL (10.3) |
- | 257% FPL (9.94) |
|
Weight self- perception |
Self-perception: normal weight |
238 | 17.7%(1.75) | 466 | 39.8%(1.94) | - | - | - | - | 704 | 29.4%(1.32) |
| Among individuals with overweight |
198 | 26.9%(2.57) | 357 | 58.0%(2.40) | - - |
- - |
- - |
- - |
555 | 43.0%(1.79) | |
| Among individuals with obesity |
40 | 6.1%(1.35) | 109 | 19.1%(2.09) | 149 | 13.2%(1.32) | |||||
|
Self-perception: overweight |
1042 | 82.3%(1.75) | 717 | 60.2%(1.94) | - | - | - | - | 1759 | 70.6%(1.32) | |
| Among individuals with overweight |
510 | 73.1%(2.57) | 269 | 42.0%(2.40) | - - |
- - |
- - |
- - |
779 | 57.0%(1.79) | |
| Among individuals with obesity |
532 | 93.9%(1.35) | 448 | 80.9%(2.09) | 980 | 86.8%(1.32) | |||||
| Wave IV | Female | Male |
Self-perception: Normal Weight |
Self-perception: Overweight |
Total | ||||||
|
Blood Pressure Class |
Normal | 404 | 32.8% (1.77) | 324 | 26.7% (1.72) | 213 | 30.8% (2.5) | 515 | 29.0% (1.42) | 728 | 29.5% (1.24) |
| Prehypertension | 624 | 46.5% (1.86) | 601 | 51.5% (1.86) | 352 | 50.7% (2.72) | 873 | 48.5% (1.7) | 1225 | 49.1% (1.35) | |
| Hypertension I | 199 | 16.7% (1.54) | 207 | 17.5% (1.50) | 114 | 15.0% (1.95) | 292 | 18.1% (1.37) | 406 | 17.2% (1.05) | |
| Hypertension II | 53 | 4.1% (0.66) | 51 | 4.3% (0.81) | 25 | 3.6% (1.0) | 79 | 4.4% (0.6) | 104 | 4.2% (0.51) | |
| Blood Pressure | Average systolic BPe | - | 125.2 (0.48) | - | 127.3 (0.53) | - | 125.8 (0.73) | - | 126.6 (0.41) | - | 126.4 (0.35) |
| Average diastolic BP | - | 79.8 (0.38) | - | 80.2 (0.37) | - | 79.6 (0.57) | - | 80.2 (0.32) | - | 80.0 (0.26) | |
| BMI | Average BMI | - | 36.8 (0.35) | - | 34.7 (0.39) | - | 32.2 (0.28) | - | 37.2 (0.26) | - | 35.7 (0.29) |
| Weight status | Underweight | 1 | 0.14% (0.14) | 0 | 0% (0) | 1 | 0.2% (0.23) | 0 | 0% (0) | 1 | 0.1% (0.07) |
| Normal Weight | 67 | 5.3% (0.85) | 54 | 4.7% (0.83) | 66 | 9.4% (1.43) | 55 | 3.2% (0.56) | 121 | 5.0% (0.59) | |
| Overweight | 209 | 15.3% (1.44) | 255 | 22.1% (1.56) | 189 | 27.8% (2.1) | 275 | 15.2% (1.13) | 464 | 18.9% (1.14) | |
| Obese | 1003 | 79.2% (1.63) | 874 | 73.2% (1.67) | 448 | 62.6% (2.28) | 1429 | 81.7% (1.18) | 1877 | 76.0% (1.29) | |
| Age | Average age | - | 28.6 (0.08) | - | 28.4 (0.08) | - | 28.4 (0.11) | - | 28.6 (0.07) | - | 28.5 (0.06) |
|
Highest level of education |
Less than high school | 89 | 6.3% (0.90) | 90 | 7.2% (1.05) | 67 | 9.0% (1.51) | 112 | 5.9% (0.82) | 179 | 6.8% (0.74) |
|
High school degree or equivalent |
205 | 16.1% (1.34) | 202 | 17% (1.36) | 111 | 16.7% (1.8) | 296 | 16.6% (1.21) | 407 | 16.6% (0.98) | |
|
Some college/trade school |
578 | 48.0% (1.74) | 547 | 46.9% (1.75) | 318 | 45.5% (2.53) | 807 | 48.2% (1.39) | 1125 | 47.4% (1.33) | |
|
College graduate or beyond |
408 | 29.5% (1.74) | 344 | 28.9% (1.80) | 208 | 28.7% (2.59) | 544 | 29.4% (1.55) | 752 | 29.2% (1.45) | |
| Substance Use | Smoker | 477 | 38.8% (1.49) | 431 | 36.9% (1.68) | 251 | 37.3% (2.15) | 657 | 38.0% (1.47) | 908 | 37.8% (1.16) |
| Heavy drinker | 115 | 7.7% (0.81) | 150 | 12.5% (1.36) | 81 | 11.8% (1.74) | 184 | 9.6% (0.94) | 265 | 10.3% (0.89) | |
SE=standard error;
BMI=body mass index;
HH income=household income;
FPL=federal poverty line;
BP=blood pressure
Overall, weight under-perception in adolescence was associated with significantly lower systolic blood pressure in young adulthood, controlling for age, race, ethnicity, smoking and alcohol consumption, education level, adolescent household income, and adolescent BMI. Youth who under-perceived their weight in adolescence had systolic blood pressures an average of 2.5 mmHg lower (95% confidence: 0.7, 4.3) than those who perceived themselves as overweight (Supplementary Table 1). A test of interaction by gender was not statistically significant (p=0.289). However, given our a priori hypothesis, we stratified by gender, and found marked differences between young men and young women (Figure 2). Among young men, the reduction in systolic blood pressure was small (1.3 mmHg; 95% confidence: −1.1, 3.7) and statistically insignificant (Supplementary Table 1). Race-stratified analyses in young men revealed similarly insignificant results.
Figure 2. Relationship between weight self-perception and systolic blood pressure, stratified by gender.
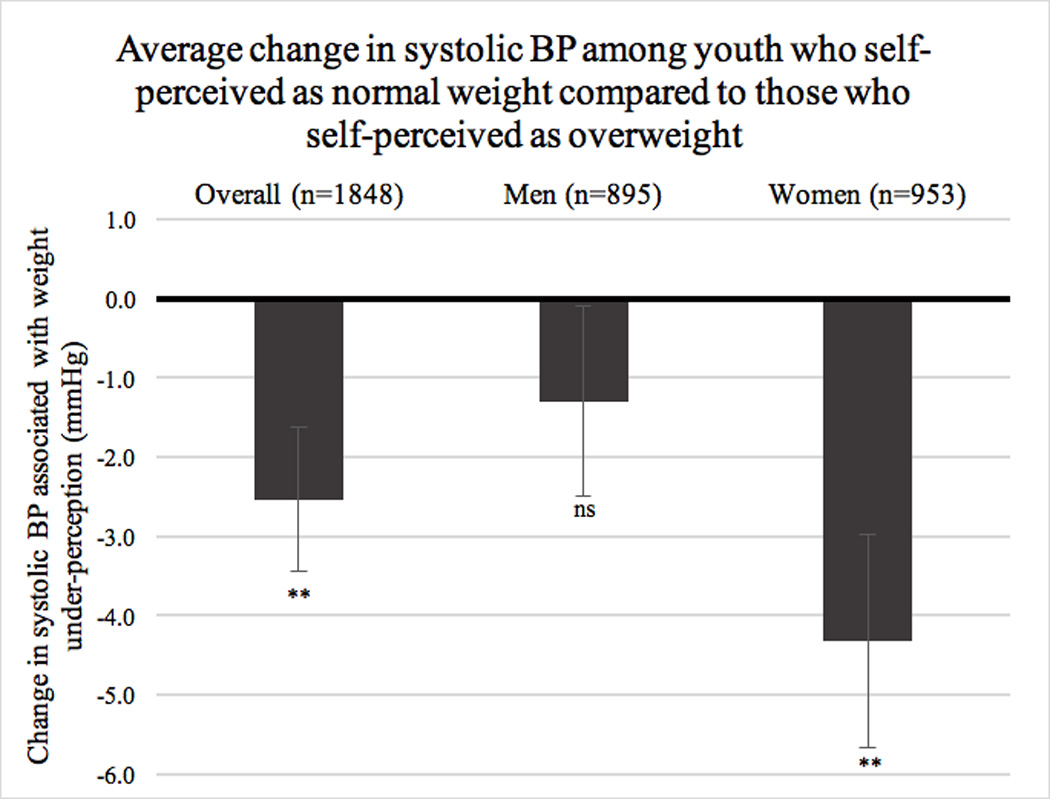
Average change in Wave IV systolic blood pressure among youth who self-perceived as normal weight in Wave II as compared to those who self-perceived as overweight. Results are stratified by gender. Negative numbers indicate a decrease in blood pressure among under-perceivers; positive numbers indicate an increase. Error bars show standard error. BP=blood pressure. *p≤0.05; **p≤0.01, ***p≤0.001, ns=not significant
Young women, however, showed a large and statistically significant association between weight under-perception in adolescence and lower blood pressure in young adulthood (Table 2, Model 1). Among women who had overweight or obesity in adolescence, weight under-perception was associated with 4.3 mmHg lower systolic blood pressure (SBP) (95% confidence: 1.7, 7.0) and 2.8 mmHg lower diastolic blood pressure (DBP) (95% confidence: 0.7, 5.0) in young adulthood. Our model explained about 8% of the variation in adult blood pressure. Our mediation analysis – which added change in BMI (between adolescence and adulthood) as a covariate – revealed surprising results (Table 2, Model 2; Figure 3). In this model, the relationship between weight self-perception in adolescence and blood pressure in adulthood was nearly identical to that seen in Model 1. This suggests that the relationship between weight self perception in adolescence and blood pressure in adulthood is independent of the relationship between weight self-perception in adolescence and weight gain into adulthood.
Table 2.
Association of Weight Perception, Demographics, and Health Behavior with Blood Pressure in Women
| SYSTOLIC BLOOD PRESSURE |
Model 1 (Basic Model) | R2: 0.0811 | Model 2 (Mediation Model)a | R2: 0.0812 | ||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | Std. Error | p | 95% conf. | Coefficient | Std. Error | p | 95% conf. | |
|
Under-perceived weight in adolescence |
−4.332264 | 1.3434 | 0.002 | (−7.0, −1.7) | −4.299657 | 1.328441 | 0.002 | (−6.9, −1.7) |
| Baseline BMI (Wave II)b | −0.2404429 | 0.1211781 | 0.049 | (−0.5, 0.0) | −0.2397624 | 0.1210288 | 0.05 | (−0.5, 0.0) |
|
Change in BMI (Wave IV-Wave II) |
- | - | - | - | 0.0209898 | 0.081654 | 0.798 | (−0.1, 0.2) |
| Age (Wave IV) | 0.1964945 | 0.2977571 | 0.51 | (−0.4, 0.8) | 0.1969628 | 0.2978378 | 0.51 | (−0.4, 0.8) |
| HH income (Wave I)c | −0.1498125 | 0.0897367 | 0.097 | (−0.3, 0.0) | −0.1501639 | 0.0899251 | 0.097 | (−0.3, 0.0) |
| Smoker | −0.7653298 | 1.261085 | 0.545 | (−3.3, 1.7) | −0.7487237 | 1.261571 | 0.554 | (−3.2, 1.7) |
| Heavy drinker | 5.236133 | 1.885457 | 0.006 | (1.5, 9.0) | 5.24255 | 1.88182 | 0.006 | (1.5, 9.0) |
|
Education: Less than high school |
0 (base) | 0 (base) | ||||||
|
Education: High school degree or equivalent |
−0.3690492 | 2.871724 | 0.898 | (−6.1, 5.3) | −0.3722861 | 2.868201 | 0.897 | (−6.0, 5.3) |
|
Education: Some college/trade school |
−7.212969 | 2.639116 | 0.007 | (−12.4, −2.0) | −7.227459 | 2.63023 | 0.007 | (−12.4, −2.0) |
|
Education: College graduate or beyond |
−6.737811 | 2.628904 | 0.012 | (−11.9, −1.5) | −6.739062 | 2.631413 | 0.012 | (−11.9, −1.5) |
| Race/ethnicity: White | 0 (base) | 0 (base) | ||||||
| Race/ethnicity: Black | 1.092905 | 1.31892 | 0.409 | (−1.5, 3.7) | 1.071395 | 1.350003 | 0.429 | (−1.6, 3.7) |
| Race/ethnicity: Asian | −2.145592 | 2.348059 | 0.363 | (−6.8, 2.5) | −2.091369 | 2.328933 | 0.371 | (−6.7, 2.5) |
| Race/ethnicity: Latina | −0.6363533 | 1.496349 | 0.671 | (−3.6, 2.3) | −0.6368818 | 1.491402 | 0.67 | (−3.6, 2.3) |
|
Race/ethnicity: Other/Multiracial |
4.416886 | 2.115056 | 0.039 | (0.2, 8.6) | 4.396326 | 2.12206 | 0.04 | (0.2, 8.6) |
| Constant | 133.0763 | 9.506365 | 0 | (114.3, 151.9) | 132.8879 | 9.550305 | 0 | (114.0, 151.8) |
| DIASTOLIC BLOOD PRESSURE |
Model 1 (Basic Model) | R2: 0.0754 | Model 2 (Mediation Model) | R2: 0.0767 | ||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | Std. Error | p | 95% conf. | Coefficient | Std. Error | p | 95% conf. | |
|
Under-perceived weight in adolescence |
−2.84683 | 1.062517 | 0.008 | (−4.9, −0.7) | −2.758042 | 1.054343 | 0.01 | (−4.8, −0.7) |
| Baseline BMI (Wave II | −0.0861327 | 0.0949588 | 0.366 | (−0.3, 0.1) | −0.0842799 | 0.0953669 | 0.378 | (−0.3, 0.1) |
|
Change in BMI (Wave IV-Wave II) |
- | - | - | - | 0.0571551 | 0.0750006 | 0.447 | (−0.1, 0.2) |
| Age (Wave IV) | 0.5323076 | 0.2213804 | 0.018 | (0.1, 1.0) | 0.5335828 | 0.2216036 | 0.017 | (0.1, 1.0) |
| HH income (Wave I) | −0.094356 | 0.058793 | 0.111 | (−0.2, 0.0) | −0.0953128 | 0.0587873 | 0.107 | (−0.2, 0.0) |
| Smoker | 0.2623774 | 0.9203384 | 0.776 | (−1.6, 2.1) | 0.3075955 | 0.9174208 | 0.738 | (−1.5, 2.1) |
| Heavy drinker | 2.954486 | 1.347413 | 0.03 | (0.3, 5.6) | 2.97196 | 1.346451 | 0.029 | (0.3, 5.6) |
|
Education: Less than high school |
0 (base) | 0 (base) | ||||||
|
Education: High school degree or equivalent |
0.9136078 | 2.216271 | 0.681 | (−3.5, 5.3) | 0.9047937 | 2.214289 | 0.684 | (−3.5, 5.3) |
|
Education: Some college/trade school |
−4.185112 | 1.972273 | 0.036 | (−8.1, −0.3) | −4.224568 | 1.970765 | 0.034 | (−8.1, −0.3) |
|
Education: College graduate or beyond |
−3.831632 | 1.989512 | 0.056 | (−7.8, 0.1) | −3.835039 | 1.998098 | 0.057 | (−7.8, 0.1) |
| Race/ethnicity: White | 0 (base) | 0 (base) | ||||||
| Race/ethnicity: Black | 0.1269613 | 0.9780845 | 0.897 | (−1.8, 2.1) | 0.0683913 | 0.9956202 | 0.945 | (−1.9, 2.0) |
| Race/ethnicity: Asian | 4.095696 | 1.402955 | 0.004 | (1.3, 6.9) | 4.243347 | 1.37936 | 0.003 | (1.5, 7.0) |
| Race/ethnicity: Latina | −2.130563 | 1.03454 | 0.041 | (−4.2, −0.1) | −2.132003 | 1.02582 | 0.04 | (−4.2, −0.1) |
|
Race/ethnicity: Other/Multiracial |
1.617907 | 1.685563 | 0.339 | (−1.7, 5.0) | 1.561924 | 1.700393 | 0.36 | (−1.8, 4.9) |
| Constant | 70.50183 | 7.659066 | 0 | (55.3, 85.7) | 69.98883 | 7.706222 | 0 | (54.7, 85.2) |
See Methods section for detailed explanation of the mediation model.
BMI=body mass index. See methods section for detailed explanations of the covariates.
HH income=household income, as a percentage of the federal poverty line. Data from Wave I is used because household income data was not collected in Wave II.
Figure 3. Relationship between weight self-perception and blood pressure, stratified by race, basic and mediation models.
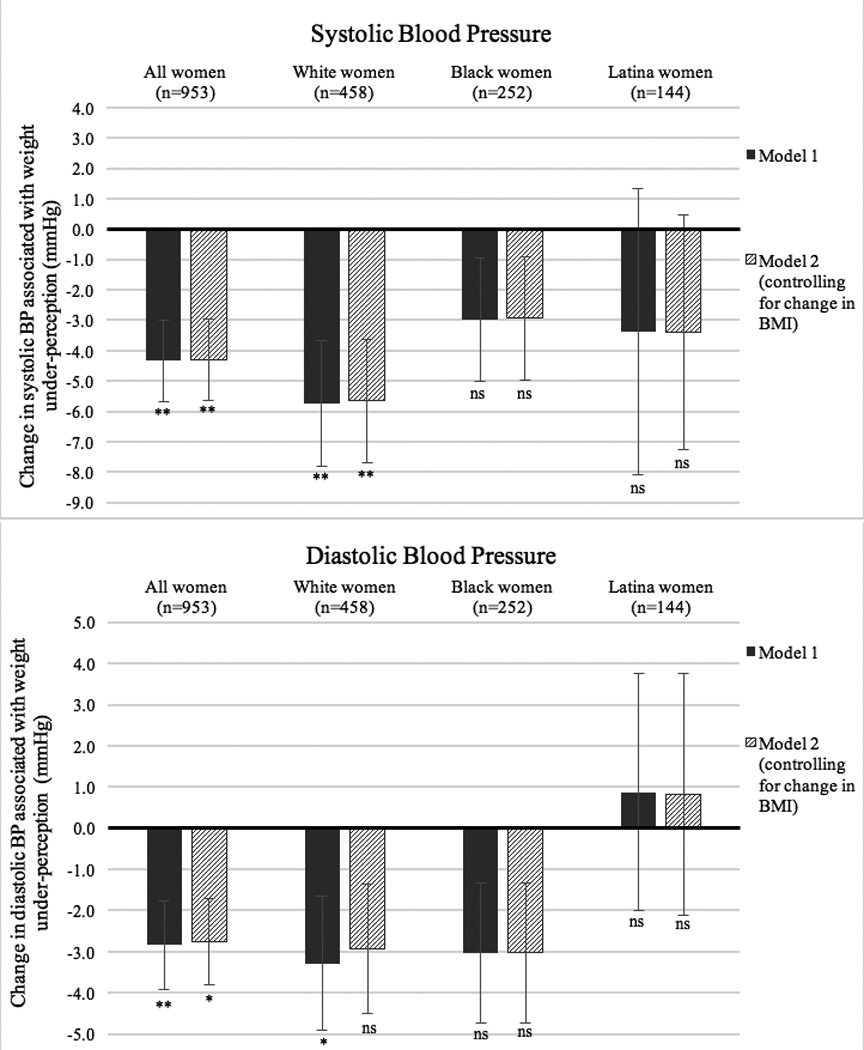
Average change in Wave IV systolic and diastolic blood pressure among women who self-perceived as normal weight in Wave II as compared to those who self-perceived as overweight. Results are stratified by race, and compare Model 1 (solid black columns, controlling for adolescent BMI and all other covariates) and Model 2 (striped columns, controlling for adolescent BMI, change in BMI between adolescence and adulthood, and all other covariates). Negative numbers indicate a decrease in blood pressure among under-perceivers; positive numbers indicate an increase. Error bars show standard error. BP=blood pressure. *p≤0.05; **p≤0.01, ***p≤0.001, ns=not significant
In race-stratified analyses, the association between weight under-perception and blood pressure was more pronounced among white women (Figure 3). White women who under-perceived their weight in adolescence had 5.8 mmHg lower SBP (95% confidence: 1.7, 9.8) and 3.3 mmHg lower DBP (95% confidence: 0.1, 6.5). Black women showed a similar pattern of smaller magnitude, but the small sample size precluded precise results. Latina women showed no clear association, and our analysis was again impeded by small sample size. Across all races, change in BMI was not an important mediator. A test of interaction by race/ethnicity within the female subpopulation was not statistically significant (p= 0.1624).
Our sensitivity analysis by weight category showed that the statistically significant association persisted only among women with overweight, not obesity, although the results varied markedly by race (Supplementary Figure 1). Our analysis was hampered by the small number of adolescent girls with obesity who perceived themselves as normal weight (n=40), and a test of interaction by weight category was not statistically significant (p= 0.6999). Our sensitivity analysis by antihypertensive use showed that the statistically significant relationship persisted regardless of antihypertensive use, although young women who used antihypertensives had a much larger effect size (Supplementary Figure 2). A test of interaction by antihypertensive use was statistically significant (p<0.0001).
Discussion
Our results show that among adolescent girls with overweight/obesity, self-perception as normal weight is associated with lower blood pressure in adulthood. To our knowledge, this is the first study examining the relationship between weight self-perception and blood pressure. On average, female under-perceivers had a systolic blood pressure 4.33 mmHg and a diastolic blood pressure 2.84 mmHg lower than women who perceived themselves as overweight. This association was independent of the previously-described association between weight under perception and lower weight gain. These blood pressure differences are of clinically significant magnitude, comparable to the pooled effect of antihypertensive medications in clinical trials of mild-to-moderate hypertension (which, on average, reduce diastolic blood pressure by 5.6 mmHg.)[30] Overall, our findings suggest that weight under-perception may be associated with better long-term health, particularly in women. Conversely, public health efforts to encourage self-perception as overweight (e.g. through BMI report cards) may backfire.
We hypothesize that stress and social stigma, and their psychological effects, mediate this relationship. Numerous studies have shown that adolescents with overweight and obesity are subject to discrimination, teasing, negative comments from peers and family, and other harmful social effects.[5,6,21,31] These social consequences of overweight and obesity increase stress, depression, and other psychological disorders among affected youth and adults. [6,32,33] Weight self-perception is likely closely tied to weight stigma and discrimination; adolescents who perceive themselves as overweight may do so in part because they receive pervasive, shaming messages from their peers and family members about their weight. Adolescents may also be more sensitive to such teasing if they perceive it to be true; one study showed that holding anti-fat personal beliefs worsened the negative psychological effects of weight-based stigma.[34] Thus, we expect that adolescents who perceive themselves as overweight will experience greater psychosocial harm than those who under-perceive their weight. Although the mechanism is not fully understood, reviews of the literature have concluded that such psychosocial stress increases the risk of elevated blood pressure.[20,35]
Access to healthcare – which, itself, may be mediated by stress and stigma – may also be a relevant mediator. Several studies have shown that individuals with overweight/obesity, especially women, commonly experience stigma and discrimination in healthcare settings, increasing the likelihood that they will delay or avoid medical care.[31,33] Those who perceive themselves to be overweight might thus be less likely to receive preventive medical care, increasing their risk of uncontrolled hypertension.
The gender differences seen in our results are consistent with past research showing that girls and women face more weight-based stigma and have higher rates of body dissatisfaction than boys and men.[21,36] Given this, perceiving oneself to be overweight may be particularly stressful and detrimental to health outcomes in women. The racial differences are likely more complicated, and it is difficult to draw conclusions given the small sample sizes of non-White groups in our study. One possible explanation is racial variation in sociocultural norms around weight; although rates of weight discrimination are higher among Black than White women, Black women have moderately lower rates of body dissatisfaction.[21,22] An alternative explanation is that Black women already experience increased blood pressure due to the stress of racial discrimination.[37] Black women may therefore be functioning at higher baseline stress levels than White women; if psychosocial stress is not purely additive, weight self-perception may have a smaller impact.
Our analysis has several strengths. We used a nationally-representative data set with a directly measured biomarker, rather than self-reported health behavior, as our outcome. This avoids the bias inherent in self-report – particularly concerning with a topic, like weight control, that is laden with social pressure – and provides a more accurate picture of participants’ cardiovascular risk. We must also note our study’s limitations: although we controlled for multiple factors known or suspected to affect blood pressure, our model explained only about 8% of the variation in adult blood pressure; we lacked data on other potential confounders and mediators, such as stress, coping resources, and personality. Our analyses were also underpowered to test associations among non-White youth, which may be particularly important given racial/ethnic differences in body weight norms.
We made substantial effort to reduce bias in our study. As with any study where an arbitrary cut-off is used to define the population, it is possible that some individuals at the margin were misclassified. By controlling for BMI, we eliminated the worst effects of this potential misclassification bias; we know that the results are not driven mainly by individuals with marginal BMIs. However, our sensitivity analysis suggests that the results may be less pronounced in girls with higher BMIs; since we were underpowered to determine whether there was a significant difference, further study is needed. Another potential source of bias is selection bias: since we only studied adolescents with overweight/obesity, we may have excluded people who perceived themselves to be overweight but responded by losing weight prior to Wave II, thereby never entering our sample. Although we cannot absolutely disprove the possibility that this occurred prior to Wave II, the data on switching into the normal weight category between Waves II and IV suggests that it is very unlikely. Only about 5% of our population fell into the normal weight category by Wave IV, and those who perceived themselves as overweight were far less likely to do so. This suggests that, if any selection bias is present, it would actually work to minimize our results – not make our results spurious.
Our findings have implications for clinical practice. Clinicians and public health professionals often assume that making adolescents with overweight/obesity aware of their weight status will improve their health.[11–13] This assumption has led many states to implement in-school screening programs to measure children’s BMI and report the results to their parents. [4,38] At the same time, fat rights advocates have long argued that labeling people as clinically overweight or obese is harmful and increases social stigma, poor self-image, negative psychological outcomes, and distrust of the healthcare system.[33,39,40] This study suggests that encouraging youth to perceive themselves as overweight may, in fact, have unintended negative health consequences.
In conclusion, adolescent girls with overweight/obesity who perceive themselves to be normal weight have lower blood pressure in adulthood than those who perceive themselves to be overweight. This lower blood pressure noted is clinically significant, and suggests that clinical and public health interventions designed to correct weight misperception may not be helping young women. Further research should re-assess such interventions, with a focus on long-term health outcomes.
Supplementary Material
Acknowledgments
Funding sources played no role in the study design; the collection, analysis and interpretation of data; the writing of the report; or in the decision to submit the article for publication. Emily Unger wrote the first draft of this paper, and no form of payment was provided to any of the authors to produce this paper.
This work was supported by the National Institute on Aging [grant number T32AG051108J]. It uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. No direct support was received from grant P01-HD31921 for this analysis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Abbreviations
- BMI
body mass index
- Add Health
National Longitudinal Study of Adolescent to Adult Health
- BP
blood pressure
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- FPL
federal poverty line
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare no conflict of interest.
Implications and Contributions: It’s widely assumed that knowing your weight is essential to weight control and good health. But might under-perceiving your weight actually benefit your health? This study shows that adolescent girls with overweight and obesity who perceive themselves as normal weight end up with lower blood pressure as adults.
Contributor Information
Emily S Unger, Harvard Medical School, 25 Shattuck St., Boston, MA 02115, USA.
Ichiro Kawachi, Department of Social and Behavioral Sciences, Harvard School of Public Health, 677 Huntington Ave. 7th Floor, Boston, MA 02115, USA
Carly E Milliren, Division of Adolescent/Young Adult Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School, 300 Longwood Ave., Boston, MA 02115, USA.
Kendrin R Sonneville, Division of Adolescent/Young Adult Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School and Department of Nutritional Sciences, University of Michigan School of Public Health, 3855 SPH I, 1415 Washington Heights, Ann Arbor, MI 48109, USA.
Idia B Thurston, Department of Psychology, University of Memphis, 310 Psychology Building, Dept. of Psychology, Memphis, TN 38152.
Holly C Gooding, Division of Adolescent/Young Adult Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School, 300 Longwood Ave., Boston, MA 02115, USA.
Tracy K Richmond, Division of Adolescent/Young Adult Medicine, Department of Medicine, Boston Children’s Hospital and Harvard Medical School, 333 Longwood Ave., Boston, MA 02115, USA.
References
- 1.Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385:2510–2520. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150 doi: 10.1016/j.jpeds.2006.08.042. 12–2. [DOI] [PubMed] [Google Scholar]
- 3.US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125:361–367. doi: 10.1542/peds.2009-2037. [DOI] [PubMed] [Google Scholar]
- 4.Nihiser AJ, Lee SM, Wechsler H, et al. BMI measurement in schools. Pediatrics. 2009;124:S89–S97. doi: 10.1542/peds.2008-3586L. [DOI] [PubMed] [Google Scholar]
- 5.Puhl RM, King KM. Weight discrimination and bullying. Best Pract Res Clin Endocrinol Metab. 2013;27:117–127. doi: 10.1016/j.beem.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Arch Pediatr Adolesc Med. 2003;157:733–738. doi: 10.1001/archpedi.157.8.733. [DOI] [PubMed] [Google Scholar]
- 7.Sonneville KR, Calzo JP, Horton NJ, et al. Body satisfaction, weight gain and binge eating among overweight adolescent girls. Int J Obes (Lond) 2012;36:944–949. doi: 10.1038/ijo.2012.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van den Berg P, Neumark-Sztainer D. Fat 'n happy 5 years later: is it bad for overweight girls to like their bodies? J Adolesc Health. 2007;41:415–417. doi: 10.1016/j.jadohealth.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self-perception of weight in overweight adolescents. Pediatrics. 2010;125:e452–e458. doi: 10.1542/peds.2009-0185. [DOI] [PubMed] [Google Scholar]
- 10.Richmond TK, Thurston I, Sonneville K, et al. Racial/ethnic differences in accuracy of body mass index reporting in a diverse cohort of young adults. Int J Obes (Lond) 2015;39:546–548. doi: 10.1038/ijo.2014.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali MM, Amialchuk A, Renna F. Social network and weight misperception among adolescents. Southern Economic Journal. 2011;77:827–842. [Google Scholar]
- 12.Park E. Overestimation and underestimation: adolescents' weight perception in comparison to BMI-based weight status and how it varies across socio-demographic factors. J Sch Health. 2011;81:57–64. doi: 10.1111/j.1746-1561.2010.00561.x. [DOI] [PubMed] [Google Scholar]
- 13.Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009;17:790–795. doi: 10.1038/oby.2008.603. [DOI] [PubMed] [Google Scholar]
- 14.Skinner AC, Weinberger M, Mulvaney S, et al. Accuracy of perceptions of overweight and relation to self-care behaviors among adolescents with type 2 diabetes and their parents. Diabetes Care. 2008;31:227–229. doi: 10.2337/dc07-1214. [DOI] [PubMed] [Google Scholar]
- 15.Jones M, Grilo CM, Masheb RM, et al. Psychological and behavioral correlates of excess weight: misperception of obese status among persons with Class II obesity. Int J Eat Disord. 2010;43:628–632. doi: 10.1002/eat.20746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hadland SE, Austin SB, Goodenow CS, et al. Weight misperception and unhealthy weight control behaviors among sexual minorities in the general adolescent population. J Adolesc Health. 2014;54:296–303. doi: 10.1016/j.jadohealth.2013.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sonneville KR, Thurston IB, Milliren CE, et al. Helpful or harmful? Prospective association between weight misperception and weight gain among overweight and obese adolescents and young adults. Int J Obes (Lond) 2016;40:328–332. doi: 10.1038/ijo.2015.166. [DOI] [PubMed] [Google Scholar]
- 18.Robinson E, Hunger JM, Daly M. Perceived weight status and risk of weight gain across life in US and UK adults. Int J Obes (Lond) 2015;39:1721–1726. doi: 10.1038/ijo.2015.143. [DOI] [PubMed] [Google Scholar]
- 19.Effects of Weight Loss and Sodium Reduction Intervention on Blood Pressure and Hypertension Incidence in Overweight People With High-Normal Blood Pressure: The Trials of Hypertension Prevention, Phase II. Arch Intern Med. 1997;157:657–667. [PubMed] [Google Scholar]
- 20.Kaplan MS, Nunes A. The psychosocial determinants of hypertension. Nutr Metab Cardiovasc Dis. 2003;13:52–59. doi: 10.1016/s0939-4753(03)80168-0. [DOI] [PubMed] [Google Scholar]
- 21.Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes (Lond) 2008;32:992–1000. doi: 10.1038/ijo.2008.22. [DOI] [PubMed] [Google Scholar]
- 22.Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: a meta-analysis. Psychol Bull. 2006;132:622–640. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]
- 23.Duncan DT, Wolin KY, Scharoun-Lee M, et al. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011;8:20. doi: 10.1186/1479-5868-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The National Longitudinal Survey of Adolescent to Adult Health. [Accessed September 1, 2016];Study Design. Available at http://www.cpc.unc.edu/projects/addhealth/design. [Google Scholar]
- 25.Harris KM. The Add Health Study: Design and Accomplishments. [Accessed August 24, 2015]; Available at: http://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWIIV.pdf. [Google Scholar]
- 26.National Center for Health Statistics. 2000 CDC growth charts: United States. [Accessed December 11, 2015]; Available at: http://www.cdc.gov/growthcharts/
- 27.Chen P, Chantala K. Guidelines for analyzing Add Health data. Carolina Population Center. 2014:1–53. [Google Scholar]
- 28.Nguyen QC, Tabor JW, Entzel PP, et al. Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22:532–541. doi: 10.1097/EDE.0b013e31821c79d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.VanderWeele T. Explanation in Causal Inference. Oxford: Oxford University Press; 2015. [Google Scholar]
- 30.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 31.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 32.Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity (Silver Spring) 2009;17:2033–2039. doi: 10.1038/oby.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. American Journal of Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedman KE, Reichmann SK, Costanzo PR, et al. Weight stigmatization and ideological beliefs: relation to psychological functioning in obese adults. Obes Res. 2005;13:907–916. doi: 10.1038/oby.2005.105. [DOI] [PubMed] [Google Scholar]
- 35.Rozanski A, Blumenthal JA, Davidson KW, et al. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice. Journal of the American College of Cardiology. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 36.Feingold A, Mazzella R. Gender Differences in Body Image Are Increasing. Psychological Science. 1998;9:190–195. [Google Scholar]
- 37.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86:1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Evans EW, Sonneville KR. BMI report cards: will they pass or fail in the fight against pediatric obesity? Curr Opin Pediatr. 2009;21:431–436. doi: 10.1097/MOP.0b013e32832ce04c. [DOI] [PubMed] [Google Scholar]
- 39.Kwan S. Framing the Fat Body: Contested Meanings between Government, Activists, and Industry. Sociological Inquiry. 2009;79:25–50. [Google Scholar]
- 40.Lewis E. Why there's no point telling me to lose weight. Bmj. 2015;350:g6845. doi: 10.1136/bmj.g6845. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.