Abstract
Background
This study compared the use of static cold storage versus continuous hypothermic machine perfusion in a cohort of kidney transplant recipients at high risk for delayed graft function (DGF).
Methods
In this national, multicenter, and controlled trial, 80 pairs of kidneys recovered from brain-dead deceased donors were randomized to cold storage or machine perfusion, transplanted, and followed up for 12 months. The primary endpoint was the incidence of DGF. Secondary endpoints included the duration of DGF, hospital stay, primary nonfunction, estimated glomerular filtration rate, acute rejection, and allograft and patient survivals.
Results
Mean cold ischemia time was high but not different between the 2 groups (25.6 ± 6.6 hours vs 25.05 ± 6.3 hours, 0.937). The incidence of DGF was lower in the machine perfusion compared with cold storage group (61% vs. 45%, P = 0.031). Machine perfusion was independently associated with a reduced risk of DGF (odds ratio, 0.49; 95% confidence interval, 0.26-0.95). Mean estimated glomerular filtration rate tended to be higher at day 28 (40.6 ± 19.9 mL/min per 1.73 m2 vs 49.0 ± 26.9 mL/min per 1.73 m2; P = 0.262) and 1 year (48.3 ± 19.8 mL/min per 1.73 m2 vs 54.4 ± 28.6 mL/min per 1.73 m2; P = 0.201) in the machine perfusion group. No differences in the incidence of acute rejection, primary nonfunction (0% vs 2.5%), graft loss (7.5% vs 10%), or death (8.8% vs 6.3%) were observed.
Conclusions
In this cohort of recipients of deceased donor kidneys with high mean cold ischemia time and high incidence of DGF, the use of continuous machine perfusion was associated with a reduced risk of DGF compared with the traditional cold storage preservation method.
Brazil is currently the second largest country in absolute number of kidney transplant. The number of kidney transplants with allografts recovered from deceased donors has steadily increased of the last 10 years. This has been a consequence of a well-organized public national transplant system funded by the government.1
While our national short term outcomes are comparable to many published reports of registry data, our long-term outcomes lag behind. Although several variables may concur to this finding, the remarkable high incidence of delayed graft function (DGF), which is at least 2 times higher than that observed in the United States and Europe, is perceived as the variable with highest relative risk associated with graft loss.2 Kidneys that develop DGF after transplantation have an increased risk of acute rejection, and are associated with prolonged hospitalization and overall increased costs.3,4 On the other hand, the influence of duration of DGF on graft outcomes is limited and controversial. In 1 cohort analysis including 1412 kidney transplant recipients, DGF lasted more than 15 days in 25% of patients and was independently associated with inferior allograft survival.5
Several factors beyond the traditional ones may account for this high incidence of DGF. First, organ procurement organizations (OPO) are restricted to a few university hospitals that cover large areas with over 50 regional hospitals. Late referral of a potential donor to the OPOs is perhaps 1 of the main reasons associated with the high incidence of DGF. Second, donor maintenance till organ recovery occurs at the expenses of these peripheral hospitals, which have limited financial and capacitated human resources. Third, the typical deceased kidney donor today is older and has more concomitant diseases than donors several years ago.6
Recent studies have suggested that machine perfusion could result in lower rates of DGF after transplantation of kidneys from all types of deceased donors.7 This could be particularly attractive in programs with high incidence of DGF. On the other hand, the effect of machine perfusion in kidneys recovered from unstable hemodynamic brain dead deceased donors is unknown. Additionally, machine perfusion allows access to perfusion parameters, as flow and renal resistance, variables that may assist in the decision to transplant or discard kidneys recovered from high risk donors.8-10 This study compared the incidence of DGF in recipients of kidneys recovered from brain dead deceased donors using machine perfusion or cold-storage preservation.
MATERIALS AND METHODS
Trial Design
This was a multicenter, prospective, randomized, and controlled trial comparing the influence of machine perfusion versus cold storage on the incidence of DGF after kidney transplantation. The study was approved by the local institutional review board. Because randomization was carried out right after organ recovery and intervention limited to the kidneys fulfilling the inclusion and exclusion criteria before allocation, no informed consent was required from recipients.
Donors
We screened all adult brain dead deceased donors referred to a single OPO during the enrollment period. To be included in the trial it was required the availability of the equipment and trained surgeons and sufficient time to recover the organs, considering the distance to travel at the time of referral. We excluded donors younger than 18 years, with unstable hemodynamic condition, and when combined transplants were anticipated.
Randomization and Preservation Methods
A randomization sequence identifying which kidney had to be place in the machine perfusion was generate using a Web-based program (www.randomization.com) and placed in opaque envelopes. After removal both kidneys were inspected to search for lesions or any other abnormalities. If both kidneys were considered suitable for transplantation, the randomization envelope was opened identifying treatment allocation (continuous machine perfusion or cold storage).
Machine Perfusion
Kidneys were initially flushed with 500 mL of Kidney Preservation Solution-1 and maintained in the machine perfusion at 1°C to 8°C (KPS-1, LifePort Kidney Transporter Machine; Organ Recovery Systems) from organ procurement until transplantation. None of the kidneys were discarded base on intravascular resistance and flow measurements.
Static Cold Storage
Kidneys were flushed with 500 mL and stored with Static Preservation Solution-1 (SPS-1, LifePort Kidney Transporter machine; Organ Recovery Systems) or with Celsior preservation solution (Genzyme) till transplantation.
Endpoints
The primary end point was the incidence of DGF. Secondary end points included the duration of DGF, length of hospital stay, incidence of primary nonfunction (PNF) and treated acute rejection, renal function, and patient and allograft survival. All recipients were followed up for 1 year.
Study Definitions
DGF was defined as the need of dialysis within the first week after transplantation. Duration of DGF was calculated from the time of transplant till last dialysis section. PNF was defined as permanent absence of kidney function from the time after the transplant surgery. Biopsy-proven acute rejections (≥IA) were classified using the Banff 2009 scheme. Clinical acute rejection included borderline changes in biopsy treated with methylprednisolone bolus for at least 3 days. All treated rejections, confirmed or not by biopsy, were included in the analysis. Renal function was evaluated at days 7, 14, 21, 28, and 365.
Sample Size Calculation
The incidence of DGF in the regional kidney transplant population described previously has been stable around 60% over the last years.2 Assuming a 33% reduction in the incidence of DGF with machine perfusion, from 60% to 40%, with a significance level of 5% and power of 80%, 76 kidney transplants per group was required for the analysis of the primary endpoint. Assuming 30% drop out rate approximately 100 deceased donors would be randomized after kidney recovery.
Statistical Analysis
Continuous variables were summarized as mean values and standard deviations and compared using Student t test. Categorical variables were presented as percentages and compared using the χ2 test. For the primary endpoint (DGF), we used McNemar test for paired nominal data. Estimated glomerular filtration rate (eGFR) was compared using the general linear model for multiple comparisons in the intention to treat population (patients randomized who received at least 1 dose of study drug) and in the per protocol population (patients randomized who were receiving initial drug regimen at 12 months), with and without imputation using the last observation carried forward for patients who died and zero for those who lost the graft before 12 months. Patient and graft survivals were estimated using the Kaplan-Meier method and compared using the log rank test. Risk factors for DGF were identified using multivariable logistic regression analysis (donor variables: age, type of death, previous cardiac arrest, Kidney Donor Profile Index (KDPI), sodium, transaminases, creatinine phosphokinase, terminal creatinine; transplant variables: type of preservation, cold ischemia time; recipients variables: age, body mass index (BMI), time on dialysis, retransplant, panel-reactive antibody (PRA), HLA mismatches, rabbit antithymocyte globulin induction. Statistical tests were 2-sided and performed using SPSS version 22 (IBM Company, Chicago, IL) and differences with a P value less than 0.05 were considered statistically significant.
Support
Organ Recovery Systems provided the Lifeport kidney transporter machine, preservation solutions and perfusion kits, and training of the organ recovery team.
RESULTS
Enrollment occurred in 2 periods, from July 26, 2014, to August 22, 2014, and from January 26, 2015, to March 28, 2015, depending on the availability of machine, perfusion kit, and preservation solution. During both periods, the OPO screened 262 donors. Of 104 randomized donors, 39 were multiorgan donors and 65 kidney-only donors. These kidneys were initially flushed in situ immediately after aorta cross-clamping (warm ischemia time less than 1 minute) using different preservation solutions at the discretion of the surgical team (IGL, n = 8 pairs; Eurocollins, n = 49 pairs; SPS-1, n = 23 pairs; Celsior, n = 7 pairs; Custodiol, n = 17 pairs). Then, 104 kidneys were maintained in the machine perfusion and 104 were stored (SPS-1, n = 41; Celsior, n = 63) till transplantation.
Kidneys procured from 24 donors were not included in the analysis, 23 because both kidneys were not transplanted (biopsy findings [n = 10, both kidneys discarded], macroscopic evaluation [n = 5, 1 of the kidneys discarded], allocation of 1 kidney to combined transplant [n = 3], vascular lesions detected afterwards in 1 kidney [n = 2], positive Chagas serology [n = 1], lack of additional cannula to perfuse a kidney with 2 arteries [n = 1], and 1 pediatric donor), and 1 recipient was lost to follow-up. Therefore, 160 kidneys (80 preserved in cold storage and 80 in continuous machine perfusion) from 80 donors were randomized, transplanted, and followed up for 12 months in 14 different transplant centers in the state. The demographic characteristics of the donors are shown in Table 1. Mean age was 49 years, and 66% died due to cerebrovascular accident. The mean KDPI was 70% with a distribution shifted towards higher indexes (Figure 1). The inadequate hemodynamic condition of the donors is well characterized by the high percentage use of vasoactive drugs (96%), previous cardiac arrest (18%) and significant biochemical abnormalities. Importantly, mean terminal creatinine was 1.79 mg/dL and 51% had a terminal creatinine higher than 1.5 mg/dL (Table 1).
TABLE 1.
Donor demographic characteristics (n = 80)
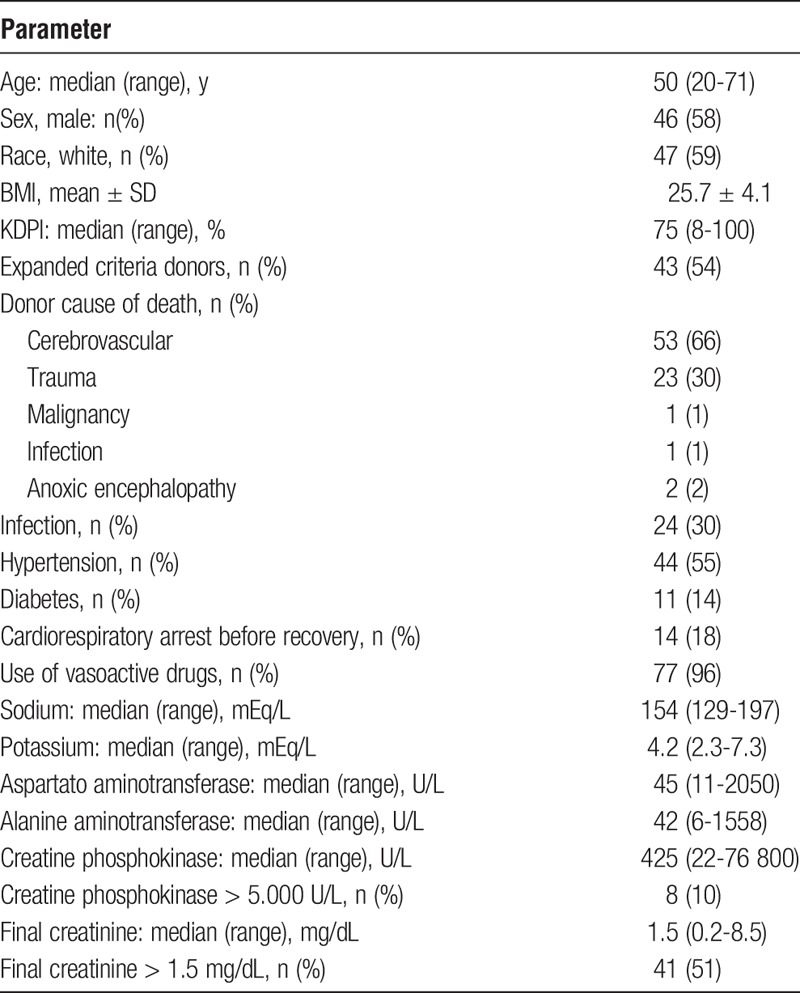
FIGURE 1.
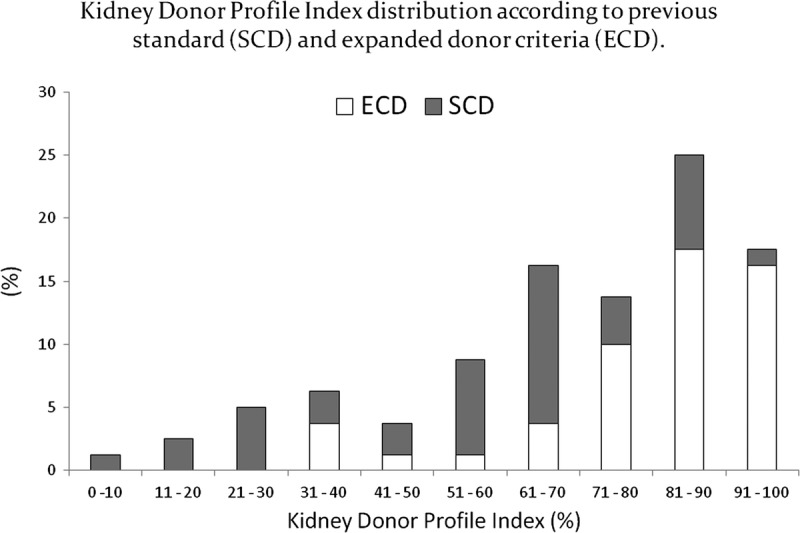
KDPI distribution according to previous standard (SCD) and expanded donor criteria (ECD).
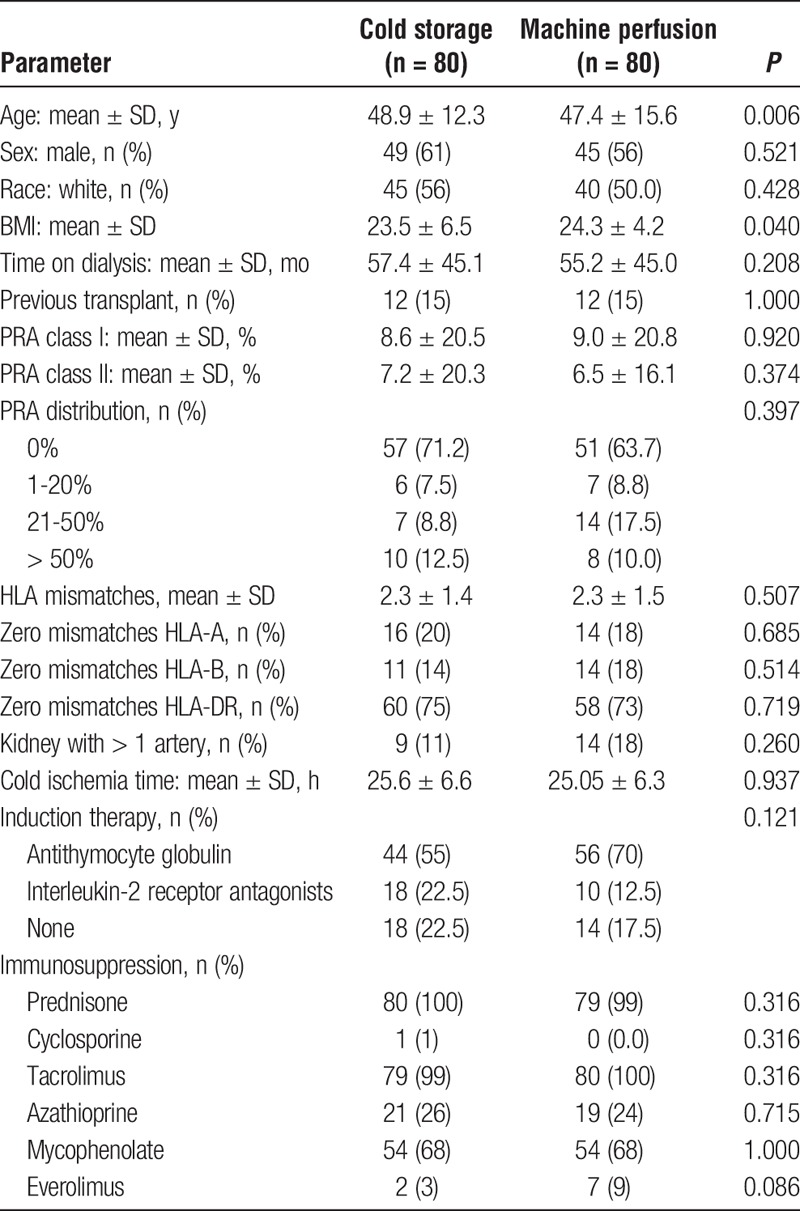
Recipients and Transplant Characteristics
The demographic characteristics of the study population well represent the general kidney transplant population of the state. Mean age was about 48 years and predominantly nonobese white men on dialysis for over 2 years median time. Low/moderate immunological risk is characterized by low prevalence of previous transplant, low mean class I or class II PRAs, and good HLA match. The proportion of kidneys with more than 1 artery was low in both groups. Mean cold ischemia time was 25 hours in both groups. The majority of patients received induction therapy with rabbit antithymocyte globulin followed by tacrolimus, mycophenolate, and prednisone (Table 2).
TABLE 2.
Demographic characteristics of the recipients and transplants
Outcomes
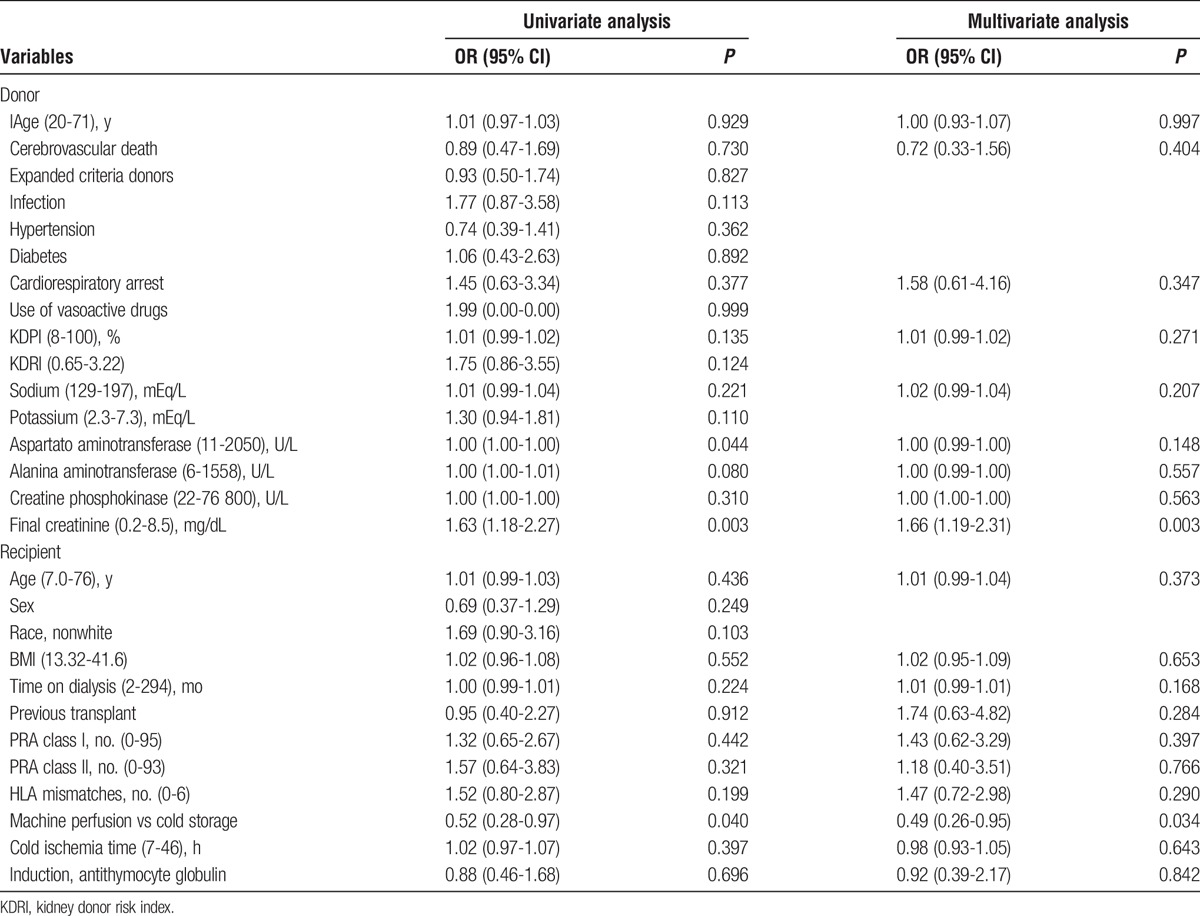
The incidence of DGF was lower in the continuous machine perfusion group (61% vs 45%, p = 0.039). There were no differences in the incidence of PNF, and in the duration of DGF or hospital stay (Table 3). Renal function recovery occurred earlier among recipients receiving kidneys preserved with continuous machine perfusion (Figure 2). Mean eGFR tended to be higher at day 28 (40.6 ± 19.9 mL/min per 1.73 m2 vs 49.0 ± 26.9 mL/min per 1.73 m2; P = 0.262) and 1 year (48.3 ± 19.8 mL/min per 1.73 m2 vs 54.4 ± 28.6 mL/min per 1.73 m2; P = 0.201) in the machine perfusion group (Table 3). Similar trends were observed comparing patients with or without DGF (data not shown). The incidence of treated acute rejection during the first month was 16.3% in the cold storage and 8.8% in the continuous machine perfusion group (P = 0.151). There were also no differences in the incidence of treated acute rejection, graft loss, or death (Table 4). One year patient and death-censored graft survivals were not different between the 2 groups and were not influenced by the incidence of DGF or acute rejection (Figure 3). Finally, using multivariable logistic regression analysis, only continuous machine perfusion was independently associated with reduced incidence of DGF (odds ratio [OR], 0.49; 95% confidence interval [CI], 0.26-0.95; P = 0.034), whereas terminal donor creatinine above 1.5 mg/dL was independently associated with higher incidence of DGF (OR, 1.66; 95% CI, 1.19-2.31; P = 0.03; Table 5).
TABLE 3.
Clinical outcomes after transplantation
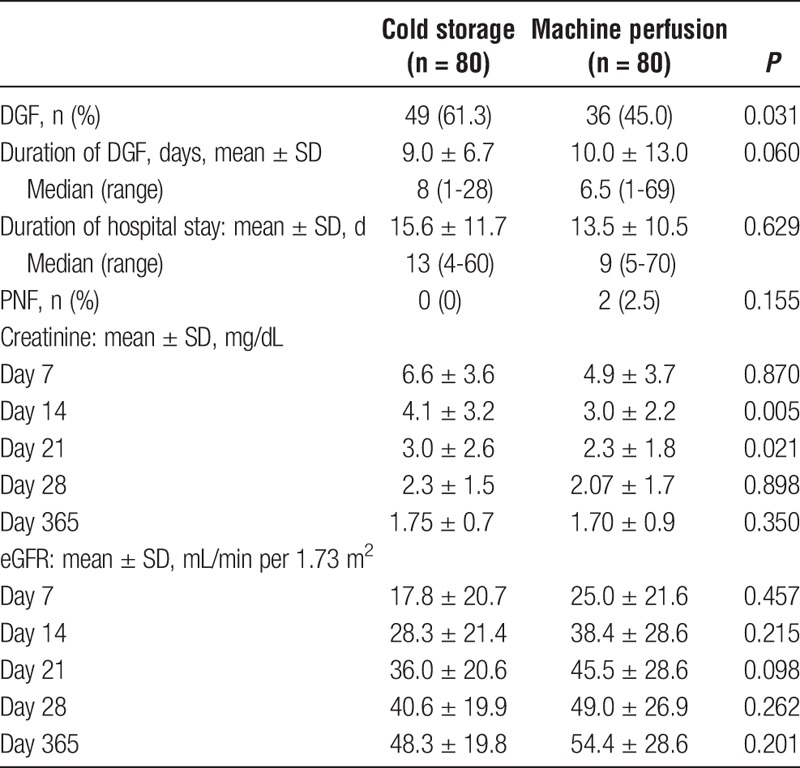
FIGURE 2.
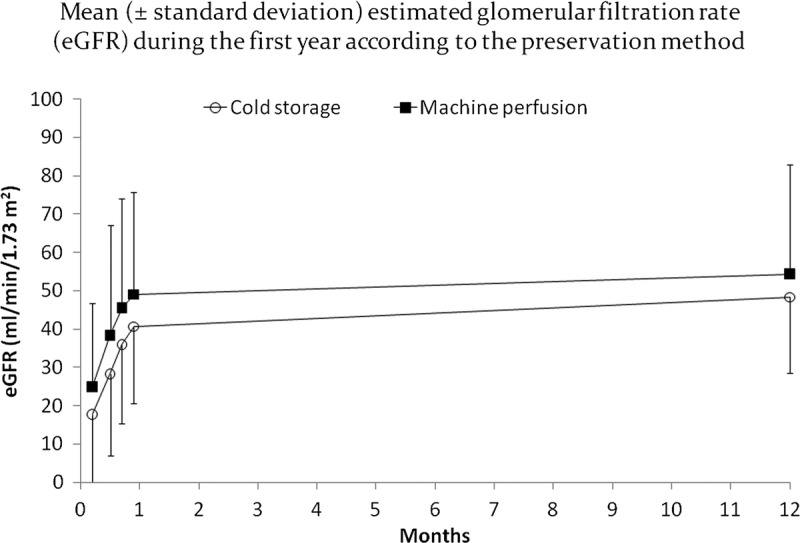
Mean (± SD) eGFR during the first year according to the preservation method.
TABLE 4.
Incidence and characteristics of acute rejection, graft loss, and deaths
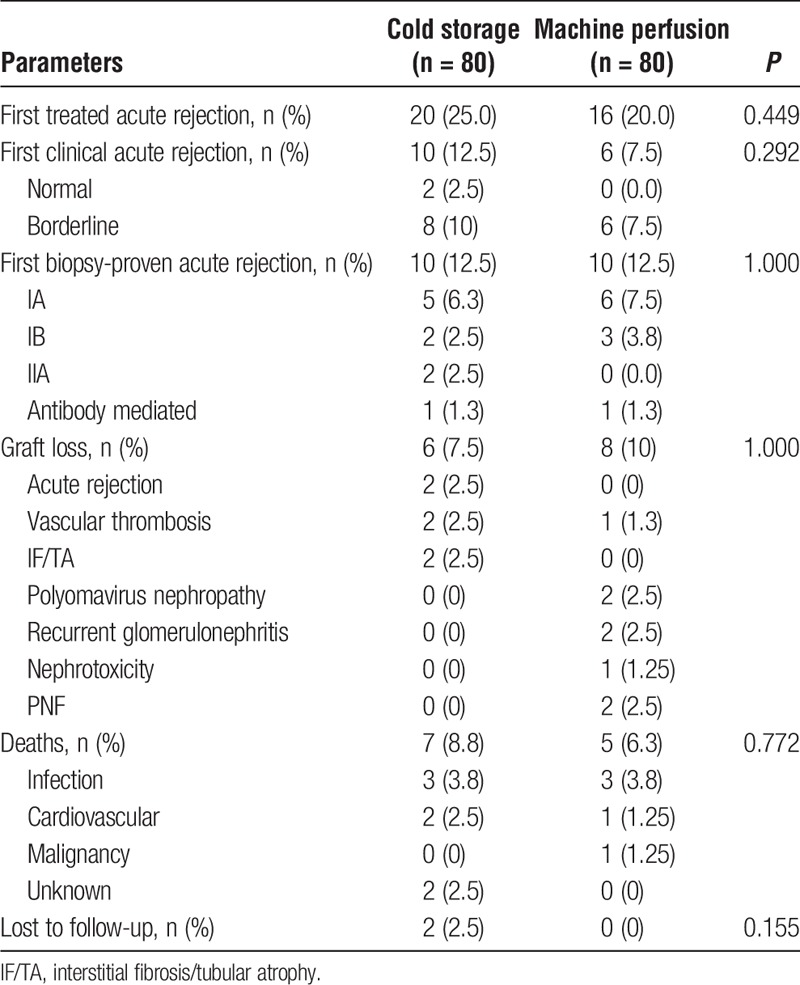
FIGURE 3.
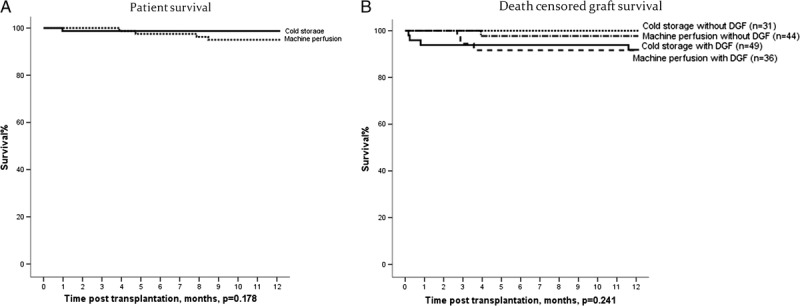
A, Patient survival. B, Death-censored graft survival.
TABLE 5.
Multivariate analysis for DGF
DISCUSSION
The use of machine perfusion in kidney transplantation is still widely debated.11,12 The benefit of this treatment modality is primarily observed in high-risk transplants, being kidneys recovered from brain-dead expanded-criteria donors13 or from donation after cardiac death14 as 2 good examples. The wide differences in our organ procurement and allocation system, including the late identification and severe hemodynamic compromise of the donors, long cold ischemia time and high incidence of DGF, preclude immediate extrapolation of the benefits of machine perfusion observed in other trials to our transplant population without a prospective trial. This study demonstrated that continuous hypothermic machine perfusion reduces the incidence of DGF compared with cold storage in recipients of kidneys recovered from high-risk deceased brain-dead donors.7 This result is in line with the larger European multicenter study.15 Importantly, in the cold storage group, our incidence of DGF was 61% compared with 26.5% in the European study. This higher incidence of DGF is associated with the hemodynamic instability, high terminal creatinine, and longer cold ischemia time. Also, the magnitude of reduction in DGF with machine perfusion was higher (30%) in our study compared with the European multicenter trial (21%). The benefit was observed among recipients of kidneys recovered from standard as well as expanded criteria donors, as donor type was not independently associated with development of DGF. In 2 large United Network for Organ Sharing registry analysis similar benefit was observed among recipients of kidneys from standard or expanded donor criteria.16,17 The only risk factor associated with DGF was the final donor creatinine, which perhaps reflects the overall hemodynamic instability of the donor and is a variable included in the majority of DGF prediction models.18 Hemodynamic instability as a risk factor for DGF has also been described using more sophisticated analysis in a cohort of kidney transplants from donors after cardiac death.19 On the other hand, continuous machine perfusion was the only variable independently associated with reduced risk of DGF. Interestingly, considering the high risk donor population, the incidence of PNF was relatively low and not influenced by the preservation method. In 2 studies in recipients of kidneys recovered from expanded criteria donors after brain death, the use of machine perfusion was associated with a reduction in the incidence of PNF compared with cold storage.13,20
There were no detectable differences in the duration of DGF and hospital stay. In the European study, machine perfusion was associated with a small but significant reduction in DGF duration (10 vs 13 days; P = 0.04). Considering this small difference, the lack of difference in our study may be due to the use of different criteria for stopping dialysis and discharging the patients among the transplant centers.
Of course, efforts to reduce the incidence of DGF should not be restricted to universal use of continuous machine perfusion. Several educational measures have been developed and implemented primarily aiming earlier identification of potential donors, which perhaps will allow earlier and better donor management by the OPOs after donation consent.
The use of new preservation solutions is another potential strategy to reduce the incidence of DGF.21 We did not investigate systematically the effect of new solutions compared with the Eurocollins in our kidney transplant population. Certainly, a pharmacoeconomic analysis would be needed considering that the new preservation solutions are at least 6 times more expensive than Eurocollins solution. Nevertheless, the incidence of DGF in the cold storage group (61%) using these new solutions (SPS-1 or Celsior) was similar to our historical incidence among 1508 kidneys over more than 10 years period preserved with Eurocollins solution.2 Also, in 1 small cohort analysis, initial flushing with Eurocollins followed by Belzer preservation solution did not influence the outcomes of combined pancreas and kidney transplantation compared with Belzer solution alone.22
The reduction of the cold ischemia time is also important though several obstacles still exist. First, within the region this study was conducted (São Paulo City, 12.04 million inhabitants) there are 230 hospitals where organ procurement takes place, all coordinated by only 4 OPOs. There are over 9000 patients on the waiting list, all managed by only 2 immunogenetics laboratories. After formal consent for organ donation, peripheral blood is sent to the immunogenetics laboratory for donor HLA typing. This information is sent to the State Health Secretary where a list of potential recipients is generated based on ABO blood type and HLA compatibility. The immunogenetics laboratories then perform the CDC crossmatches (each laboratory tests about 15 potential recipients) using lymphocytes isolated from lymph nodes obtained during organ recovery due to concerns of cell viability in the peripheral blood. Both laboratories send final crossmatch results to the State Secretary that begins calling transplant centers to offer the kidneys to recipients with highest HLA compatibility and a negative crossmatch. The size of the waiting list hampers the ability to maintain it updated, leading to longer times to locate the potential recipient and furthers delays for them to arrive at the transplant center, depending on the distance, where occasionally the clinical condition of the patient precludes transplantation. As a consequence, there is no predefined time to decline the offer. This process is repeated until both kidneys are transplanted. This is further complicated for the allocation of kidneys recovered from the expanded criteria donors, where final acceptance only occurs after several declinations because there is still no dedicated wait list. Among measures in development to reduce the cold ischemia time are the use of lymphocytes from peripheral blood to perform the CDC crossmatch and initial organ allocation based on virtual crossmatch. These measures will allow earlier localization and arrival of a potential recipient at the transplant center while we wait for the final CDC crossmatch. Under the current system 80% of kidney transplants are performed with full DR match.
The incidence of acute rejection is higher among patients with DGF. Although patients receiving kidneys preserved in cold storage solution presented almost a 2-fold higher incidence of treated acute rejection during the first month compared with those receiving kidneys preserved with continuous machine perfusion, this difference was not statistically significant, perhaps due to the use of anti-thymocyte globulin induction and the small sample size for this particular endpoint. Nevertheless, this difference in acute rejection rates disappeared towards the end of first year. As expected, no differences in graft loss or deaths were observed between the 2 groups. Two recent meta-analysis did not reveal any difference in the incidence of PNF, graft loss, or patient death at 1 year after transplantation.11,12
Contrasting with the European trial, renal function recovery was faster in the continuous machine perfusion group but the differences in eGFR reduced on average from 10 mL/min at month 1 to 6 mL/min at 12 months. Patients receiving kidneys preserved with continuous machine perfusion tended to show faster renal function recovery and superior renal function at the end of first year, both in those who developed or not DGF.
The major limitations of our study is the lack of power to detect differences in secondary key endpoints such as renal function and graft survival at the end of first year. Also, because of the multicenter open label design, no uniformed criteria for indicating or stopping dialysis and for hospital discharge were used, precluding definitive conclusion regarding these important outcomes. It is not possible to anticipate whether similar results would be observed if cold ischemia times were lower, comparable to those observed in the United States and Europe. Finally, a pharmacoeconomic analysis is ongoing to evaluate the cost-effectiveness of this strategy and to identify potential deceased donors in which this procedure is dominant compared with cold storage preservation.
In summary, in this cohort of recipients of deceased donor kidneys with high incidence of DGF, the use of continuous machine perfusion was associated with a reduced risk of DGF compared with the traditional cold storage preservation method. Nevertheless, the beneficial effects of machine perfusion were modest and temporary and should be balanced against other strategies to reduce the incidence of DGF such as shorter cold ischemia times and use of better preservation solutions.
Footnotes
Published online 18 April, 2017.
The authors declare no funding or conflicts of interest.
H.T-S.Jr, J.C.M.O., V.A.C., M.I.d.P., W.F.A., J.M.P. participated in research design. H.T-S.Jr., J.C.M.O., V.A.C., M.I.d.P., W.F.A., J.M.P. participated in data analysis. H.T-S.Jr., J.C.M.O., V.A.C., M.I.d.P., E.D.N., F.B.C.L., L.R.R.M., A.P.e.S.F., M.d.F.d.M.C., E.F.d.S., L.A.M., D.P.D., P.S.L., W.T.d.S.L., S.A.B., L.M.k., I.L.N., S.L.B., R.C.B., J.C.M.M., I.M.M.F-C., M.A-F., L.G.M.d.A., P.D.G., L.T.S.S., A.F.L., P.R.C., A.L.C.N., J.A.Z., A.J.D.d.A.S.F., W.F.A., J.M.P. participated in the performance of the research. H.T-S.Jr., J.C.M.O., V.A.C., M.I.d.P., E.D.N., F.B.C.L., L.R.R.M., A.P.e.S.F., M.d.F.d.M.C., E.F.d.S., L.A.M., D.P.D., P.S.L., W.T.d.S.L., S.A.B., L.M.k., I.L.N., S.L.B., R.C.B., J.C.M.M., I.M.M.F-C., M.A-F., L.G.M.d.A., P.D.G., L.T.S.S., A.F.L., P.R.C., A.L.C.N., J.A.Z., A.J.D.d.A.S.F., W.F.A., J.M.P. participated in the writing of the article.
REFERENCES
- 1.Silva HT, Jr, Felipe CR, Abbud-Filho M, et al. The emerging role of Brazil in clinical trial conduct for transplantation. Am J Transplant. 2011;11:1368–1375. [DOI] [PubMed] [Google Scholar]
- 2.Klein R, Galante NZ, de Sandes-Freitas TV, et al. Transplantation with kidneys retrieved from deceased donors with acute renal failure. Transplantation. 2013;95:611–616. [DOI] [PubMed] [Google Scholar]
- 3.Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011;11:2279–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yarlagadda SG, Coca SG, Formica RN, Jr, et al. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transplant. 2009;24:1039–1047. [DOI] [PubMed] [Google Scholar]
- 5.de Sandes-Freitas TV, Felipe CR, Aguiar WF, et al. Prolonged delayed graft function is associated with inferior patient and kidney allograft survivals. PLoS One. 2015;10:e0144188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baptista AP, Silva HT, Jr, Pestana JO. Influence of deceased donor hemodynamic factors in transplant recipients renal function. J Bras Nefrol. 2013;35:289–298. [DOI] [PubMed] [Google Scholar]
- 7.Jochmans I, O'Callaghan JM, Pirenne J, et al. Hypothermic machine perfusion of kidneys retrieved from standard and high-risk donors. Transpl Int. 2015;28:665–676. [DOI] [PubMed] [Google Scholar]
- 8.Yushkov YY, Stern J, Ying A, et al. Identifying risk factors in renal allografts before transplant: machine-measured renal resistance and posttransplant allograft survival. Prog Transplant. 2012;22:175–182. [DOI] [PubMed] [Google Scholar]
- 9.Sung RS, Christensen LL, Leichtman AB, et al. Determinants of discard of expanded criteria donor kidneys: impact of biopsy and machine perfusion. Am J Transplant. 2008;8:783–792. [DOI] [PubMed] [Google Scholar]
- 10.Jochmans I, Moers C, Smits JM, et al. The prognostic value of renal resistance during hypothermic machine perfusion of deceased donor kidneys. Am J Transplant. 2011;11:2214–2220. [DOI] [PubMed] [Google Scholar]
- 11.Lam VW, Laurence JM, Richardson AJ, et al. Hypothermic machine perfusion in deceased donor kidney transplantation: a systematic review. J Surg Res. 2013;180:176–182. [DOI] [PubMed] [Google Scholar]
- 12.O'Callaghan JM, Morgan RD, Knight SR, et al. Systematic review and meta-analysis of hypothermic machine perfusion versus static cold storage of kidney allografts on transplant outcomes. Br J Surg. 2013;100:991–1001. [DOI] [PubMed] [Google Scholar]
- 13.Treckmann J, Moers C, Smits JM, et al. Machine perfusion versus cold storage for preservation of kidneys from expanded criteria donors after brain death. Transpl Int. 2011;24:548–554. [DOI] [PubMed] [Google Scholar]
- 14.Morrissey PE, Monaco AP. Donation after circulatory death: current practices, ongoing challenges, and potential improvements. Transplantation. 2014;97:258–264. [DOI] [PubMed] [Google Scholar]
- 15.Moers C, Smits JM, Maathuis MH, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2009;360:7–19. [DOI] [PubMed] [Google Scholar]
- 16.Cannon RM, Brock GN, Garrison RN, et al. Machine perfusion: not just for marginal kidney donors. Am Surg. 2015;81:550–556. [PubMed] [Google Scholar]
- 17.Gill J, Dong J, Eng M, et al. Pulsatile perfusion reduces the risk of delayed graft function in deceased donor kidney transplants, irrespective of donor type and cold ischemic time. Transplantation. 2014;97:668–674. [DOI] [PubMed] [Google Scholar]
- 18.Nashan B, Abbud-Filho M, Citterio F. Prediction, prevention, and management of delayed graft function: where are we now? Clin Transplant. 2016;30:1198–1208. [DOI] [PubMed] [Google Scholar]
- 19.Allen MB, Billig E, Reese PP, et al. Donor hemodynamics as a predictor of outcomes after kidney transplantation from donors after cardiac death. Am J Transplant. 2016;16:181–193. [DOI] [PubMed] [Google Scholar]
- 20.Gallinat A, Moers C, Treckmann J, et al. Machine perfusion versus cold storage for the preservation of kidneys from donors >/= 65 years allocated in the Eurotransplant Senior Programme. Nephrol Dial Transplant. 2012;27:4458–4463. [DOI] [PubMed] [Google Scholar]
- 21.O'Callaghan JM, Knight SR, Morgan RD, et al. Preservation solutions for static cold storage of kidney allografts: a systematic review and meta-analysis. Am J Transplant. 2012;12:896–906. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez AM, Filho GJ, Pestana JO, et al. Effects of Eurocollins solution as aortic flush for the procurement of human pancreas. Transplantation. 2005;80:1269–1274. [DOI] [PubMed] [Google Scholar]


