Abstract
Background
Increases in patient needs can strain hospital resources, which may worsen care quality and outcomes. This systematic literature review sought to understand whether hospital capacity strain is associated with worse health outcomes for hospitalized patients and to evaluate benefits and harms of health system interventions to improve care quality during times of hospital capacity strain.
Methods
Parallel searches were conducted in MEDLINE, CINAHL, the Cochrane Library, and reference lists from 1999-2015. Two reviewers assessed study eligibility. We included English-language studies describing the association between capacity strain (high census, acuity, turnover, or an indirect measure of strain such as delayed admission) and health outcomes or intermediate outcomes for children and adults hospitalized in highly developed countries. We also included studies of health system interventions to improve care during times of capacity strain. Two reviewers extracted data and assessed risk of bias using the Newcastle-Ottawa Score for observational studies and the Cochrane Collaboration Risk of Bias Assessment Tool for experimental studies.
Results
Of 5,702 potentially relevant studies, we included 44 observational and 8 experimental studies. There was marked heterogeneity in the metrics used to define capacity strain, hospital settings, and overall study quality. Mortality increased during times of capacity strain in 18 of 30 studies and in 9 of 12 studies in intensive care unit settings. No experimental studies were randomized, and none demonstrated an improvement in health outcomes after implementing the intervention. The pediatric literature is very limited; only six observational studies included children. There was insufficient study homogeneity to perform meta-analyses.
Discussion
In highly developed countries, hospital capacity strain is associated with increased mortality and worsened health outcomes. Evidence-based solutions to improve outcomes during times of capacity strain are needed.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3936-3) contains supplementary material, which is available to authorized users.
Keywords: Hospital medicine, Patient safety, Systematic reviews, Quality assessment, Variations
INTRODUCTION
As hospitals strive to improve efficiency, increases in patient volume, acuity, and complexity can strain hospital resources. Strain can be defined as an “excessive demand on the strength, resources, or abilities”1 of a hospital, and any resource the hospital uses to provide care (e.g., beds, nurses, physicians, equipment) can experience strain. Resource strain resulting from a mismatch between supply and demand exists on a continuum from mild strain due to routine fluctuations in patient needs to severe strain resulting from patient surges during public health emergencies. Resource strain has been well studied in the emergency department (ED), often focusing on overcrowding due to high patient volume, and ED overcrowding is associated with delayed care and increased mortality.2 – 4 However, less is known about the relationship between resource strain in hospital inpatient units and patient health outcomes.
Capacity strain is a subset of resource strain originally described in the intensive care unit (ICU). There is no universally accepted definition of capacity strain, but it has been defined as increased patient census, acuity, and/or turnover affecting an ICU’s ability to provide high-quality care.5 This concept can also be applied to non-ICU settings. Expert groups recommend strategies to improve the ability of hospitals to provide care during times of strain, particularly in response to public health emergencies.6 The effect of these strategies on patient outcomes is not clear. To decide whether to institute and promote these strategies, hospital leaders and health policymakers need to understand the effects of inpatient capacity strain on outcomes and the effectiveness of interventions to address these effects.
We conducted this systematic review to (1) review the association between capacity strain and health outcomes for patients receiving inpatient care and (2) evaluate the benefits and harms of health system interventions to improve quality of inpatient care during times of capacity strain. As the US hospital system has significantly less capacity for children than for adults and thus may be at particularly high risk for severe pediatric capacity strain,7 our goal was to focus on hospitalized children; however, we expected to find limited pediatric literature and thus expanded our scope to include adult and pediatric patients.
METHODS
Study Protocol
The study protocol was created a priori based on PRISMA-P guidance8 and registered with the International Prospective Register of Systematic Reviews (available at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015024758). This study was deemed not human subjects research by our Institutional Review Board.
Data Sources
We searched Medline, the Cochrane Library, CINAHL, and ClinicalTrials.gov for relevant English-language studies from 1999 (the year the Institute of Medicine report To Err Is Human was published) until August 2015; we also manually identified studies from reference lists. Due to the lack of standard terms to define capacity strain, a wide variety of search terms was used (e.g., capacity strain, occupancy, surge capacity, hospital crowding). The complete search strategy can be found in the Online Appendix.
Study Selection
We included randomized and non-randomized trials, prospective and retrospective cohort studies, and case-control studies. Included studies described health outcomes or intermediate outcomes (i.e., outcomes such as length of stay or delay to emergent surgery, which are plausibly associated with health outcomes) for children and adults receiving inpatient care in acute non-psychiatric hospitals during times of inpatient capacity strain. The Online Appendix contains complete inclusion and exclusion criteria. We defined capacity strain as high patient census, acuity, or turnover5; we also accepted indirect measures reflecting changes in care due to inpatient capacity strain (admitted patients boarding in the ED, or patients refused ICU admission or admitted to alternate units due to lack of beds). Studies that primarily evaluated the effects of ED crowding or did not focus on outcomes of admitted patients were excluded. Included experimental studies described health system interventions to improve care for patients in either the hospital or the ED after the decision to admit to the hospital. Two reviewers assessed study eligibility (COE, RCS); disagreements were resolved through discussion and third-party review (JMG). We assessed risk of bias for experimental studies using the Cochrane Collaboration Risk of Bias Assessment Tool,9 summarizing risk of bias for each outcome as low, unclear, or high. For observational studies, we assessed risk of bias using the Newcastle-Ottawa Scale (NOS),10 which awards studies up to 9 total stars for participant selection (4 stars), comparability of participant groups (2 stars), and ascertainment of outcome or exposure (3 stars).
Data Abstraction and Synthesis
Two reviewers (COE, RCS) independently abstracted data on study design, patient and hospital characteristics, metrics to describe strain, outcomes, and interventions. Due to heterogeneity in measures of capacity strain, we qualitatively describe measures used to describe strain, the association between strain and health outcomes or intermediate outcomes, and the health effects of interventions to improve care during times of strain. There was insufficient study homogeneity to perform meta-analyses.
RESULTS
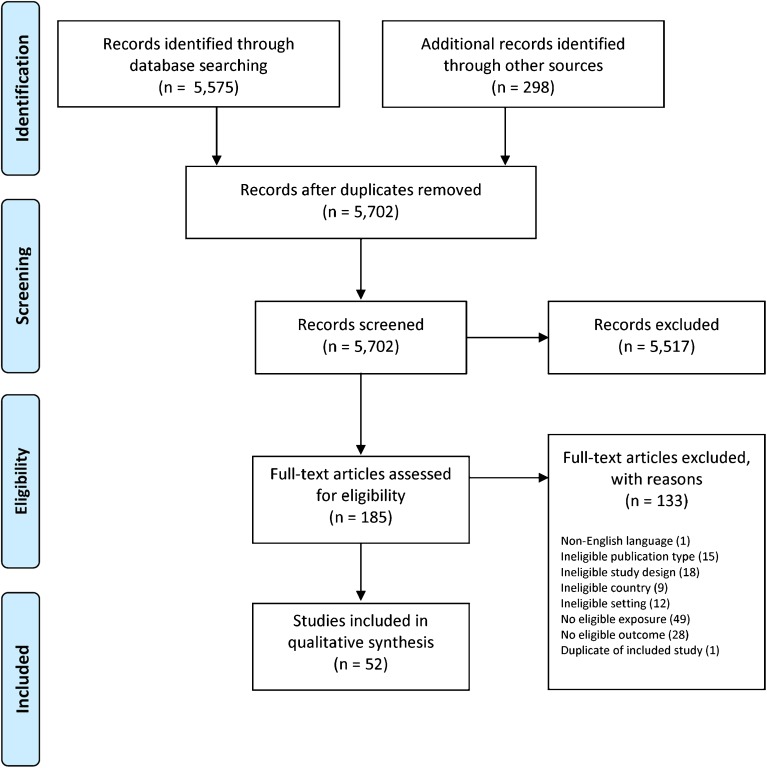
Of 5,702 potentially relevant studies, 52 were included for review (Fig. 1). Of 44 observational studies, 21 were performed in the US,11 – 31 16 in Europe,32 – 47 5 in Canada,48 – 52 and 2 in Australia.53 , 54 Thirty studies analyzed the association between capacity strain and mortality.11 – 25 , 32 – 43 , 48 , 49 , 53 All observational studies were cohort studies; all but four were retrospective.32 , 42 , 43 , 46 Eight studies described interventions to improve care during times of capacity strain,55 – 62 none using randomization to assign treatment category. Outcomes for children were separately analyzed in only six of the observational studies23 , 26 , 32 , 45 , 46 , 51 and none of the experimental studies. Characteristics of included studies are described in the Online Appendix.
Figure 1.
PRISMA flow diagram.
Measures and thresholds used to describe capacity strain varied widely (Online Appendix). One study used a composite measure that included components of census, acuity, and/or turnover13; a larger group used measures that included one of these concepts (most often census), often indexed to usual conditions. Other, often small studies used indirect measures of strain, most often ED boarding after the decision to admit to the hospital. Even among studies using similar concepts, there was great variation in specific measures to define strain. For example, some studies using census-based strain measures treated census as a continuous variable without a specific cutoff to define strain; other studies used cutoffs based on occupancy (e.g., >80% occupancy) or census percentiles (e.g., highest quartile of daily census). Timing of strain also varied: While most defined strain based on conditions on the day of admission, others used averages from the first 3 days or throughout the hospitalization, and one study evaluating the effect of strain on ICU readmission defined strain on the day of ICU discharge.14
NOS scores for included observational studies ranged from 3 to 8 of 9 possible stars (Online Appendix). The NOS does not include thresholds for distinguishing high- or low-quality studies. All experimental studies were assessed as having high risk of bias by the Cochrane Risk of Bias Tool because of high or unclear risk of bias for at least four of the tool’s eight criteria (Online Appendix).
Association Between Capacity Strain and Mortality
Of 30 studies examining mortality as an outcome, 12 were performed in ICU settings (Table 1). Thirteen were single-institution studies, while six included data from more than 100 hospitals; overall, mortality was analyzed for over 4 million hospitalizations. To define capacity strain, all but six of the multi-institution studies used hospital or unit census,12 , 13 , 16 , 19 , 20 , 36 often indexed to usual conditions (Online Appendix). Five multi-institution studies used measures of patient turnover (e.g., number of admissions) or acuity to define strain.12 – 15 , 19 Meanwhile, all but three of the single-institution studies used indirect measures of strain,24 , 41 , 49 such as time spent boarding in the ED after the decision to admit to the hospital. Most studies examined hospital mortality as the outcome of interest, while others used ICU14 , 22 , 40 or time-specific mortality.34 – 36 , 42 , 53
Table 1.
Studies Describing the Association Between Hospital Capacity Strain and Mortality
| Metrics to describe strain | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author, year | Number of hospitals | Number of admissions | Census | Admissions | Acuity | Indirect measure* | Mortality | ICU study | Children included | Key finding(s) |
| Rubinson, 2013 | 661 | NR | ● | ↑ | Increased hospital mortality for patients with stroke (15% increase) and acute myocardial infarction (20%) at hospitals experiencing high surge during the influenza pandemic compared with no-surge hospitals | |||||
| Evans, 2006 | ∼400 | 28,561+ | ● | ↔ | No association between a high number of admissions on Friday and Saturday following a Thursday admission and hospital mortality | |||||
| Tucker, 2002 | 186 | 13,334 | ● | ↑ | ● | ● | For each 10% increase in percentage of maximum occupancy on day of admission, odds of hospital mortality increased 9%; infants admitted at 50% maximum occupancy had about 50% lower odds of mortality compared to maximum occupancy | |||
| Jenkins, 2015 | 156 | 230,621 | ● | ● | ↑ | Two-fold increase in hospital mortality for patients admitted during times of high trauma surge (composite of admissions and acuity), 7-fold increase in mortality for patients with firearm injuries | ||||
| Gabler, 2013 | 107 | 264,401 | ● | ● | ● | ↑ | ● | 2% increase in odds of in-hospital death for each standard deviation increase in ICU census. 2% decrease in odds of in-hospital death for each 10% increase in number of admissions. No effect of ICU acuity on mortality | ||
| Wagner, 2013 | 107 | 200,730 | ● | ● | ● | ↔ | ● | Capacity strain on day of ICU discharge not associated with increased odds of subsequent in-hospital death; discharge on days with increased admissions associated with 3% lower odds of in-hospital death | ||
| Chalfin, 2007 | 90 | 50,332 | ● | ↑ | ● | 29% lower odds of hospital survival among patients with delayed admission to ICU | ||||
| Iapichino, 2004 | 89 | 12,615 | ● | ↑ | ● | Admission to an ICU with average occupancy >80% was associated with 32–35% increase in odds of hospital mortality compared to ICUs with average occupancy ≤80% | ||||
| Schwierz, 2011 | 72 | NR | ● | ↔ | No increase in 24-h mortality among patients admitted on days with unexpectedly high census (after adjusting for changes in unobserved risk characteristics on high-census days) | |||||
| Madsen, 2014 | 72 | 2,651,021 | ● | ↑ | 1.2% increase in relative risk of inpatient and 30-day mortality per 10% increase in median bed occupancy rate. Occupancy rates ≥110% associated with a 9% increase in mortality compared to occupancy rate <80% | |||||
| Iwashyna, 2009 | 48 | 200,499 | ● | ↔ | ● | No difference in hospital mortality with increasing census on the day of admission | ||||
| Schilling, 2010 | 39 | 166,920 | ● | ↑ | 6% increase in hospital mortality among patients admitted on high occupancy days. 12% increase in mortality among patients admitted during widespread or regional influenza activity | |||||
| Marcin, 2004 | 39 | 102,008 | ● | ↔ | No association between high annual, quarterly, or monthly number of trauma admissions and hospital mortality | |||||
| Derose, 2014 | 13 | 136,740 | ● | ↔ | No association between increased ED boarding time and inpatient mortality | |||||
| Robert, 2012 | 10 | 1,332 | ● | ↑ | ● | 1.8-fold increased adjusted odds of 60-day mortality in patients admitted to ICU after subsequent referral compared to patients admitted immediately; no significant effect on 28-day mortality | ||||
| Sprivulis, 2006 | 3 | 62,495 | ● | ↑ | Compared to patients admitted while hospital occupancy was <90%, patients admitted while occupancy was ≥100% had 30% increase in 7-day mortality hazard | |||||
| Yergens, 2015 | 3 | 1,036 | ● | ↑ | Compared to patients admitted to the hospital when ICU occupancy was <80%, patients admitted when ICU occupancy was ≥90% had 72% increased odds of hospital mortality | |||||
| Singer, 2011 | 1 | 41,256 | ● | ↑ | Compared to patients who did not board in the ED, patients who boarded ≥12 h had 23–43% increased hospital mortality | |||||
| Plunkett, 2011 | 1 | 23,114 | ● | ↑ | Compared to patients who waited <1 h between admission team referral and ward bed placement, each category of increasing delay (1–2.5 h, 2.5–6 h, 6–14 h, >14 h) was associated with an additional 7% increase in 30-day hospital mortality | |||||
| Gilligan, 2008 | 1 | 13,357 | ● | ↔ | No association between number of ED boarders at 9 a.m. and hospital mortality | |||||
| Pascual, 2014 | 1 | 8,626 | ● | ↔ | ● | No difference in ICU mortality between patients boarding in an overflow ICU and non-boarded patients | ||||
| Serafini, 2015 | 1 | 3,828 | ● | ↑ | Among medical patients boarding in surgical wards, 1.8-fold increased adjusted odds of hospital mortality | |||||
| Bekmezian, 2012 | 1 | 1,792 | ● | ↔ | ● | No association between ED boarding time and hospital mortality | ||||
| O’Callaghan, 2012 | 1 | 1,609 | ● | ↔ | Delay in admission to the ICU from the ED was not associated with ICU mortality | |||||
| Clark, 2012 | 1 | 1,433 | ● | ↑ | ● | 9% increase in hospital mortality for every unit increase in ICU occupancy | ||||
| Clark, 2007 | 1 | 1,200 | ● | ↑ | ● | 1.5% increase in hospital mortality for every 10% increase in time between decision to admit and ICU admission | ||||
| Tarnow-Mordi, 2000 | 1 | 1,050 | ● | ● | ↑ | ● | Highest quartile of each workload measure (initial occupancy, initial workload, peak occupancy, average occupancy, average workload, average acuity) associated with 90-130% increased odds of hospital mortality | |||
| Ball, 2006 | 1 | 861 | ● | ↔ | Patients treated during mass casualty incidents did not have higher hospital mortality than trauma patients admitted during other times | |||||
| Stowell, 2013 | 1 | 483 | ● | ↔ | No association between admission to outlying wards instead of usual specialty ward and unadjusted mortality at 24 h, 28 days, and 90 days | |||||
| Intas, 2012 | 1 | 200 | ● | ↑ | ● | Patients with ED boarding times >6 h had 5.7 times higher hospital mortality than those with shorter boarding time | ||||
*Examples of indirect measures include boarding in the emergency department after decision to admit, admission to alternate unit because of full usual unit, and refused ICU admission due to full ICU
ED: Emergency department. h: hours. ICU: Intensive care unit. NR: Not reported
There was a statistically significant increase in mortality during times of capacity strain in 18 of 30 studies and in 9 of 12 studies in ICU settings (Table 1). While two studies reported over five-fold mortality associated with capacity strain,13 , 43 several studies found more modest 50–150% increases in mortality.32 , 36 , 39 , 41 , 48 Only two studies included children: a multi-institution UK study that found a doubling in mortality odds for patients admitted at maximum compared to 50% occupancy32 and a single-institution US study that found no significant association between ED boarding time and subsequent hospital mortality.23 Study quality did not appear to affect the likelihood of reporting a positive relationship between strain and mortality. While most studies measured strain daily or more often, one study measured monthly, quarterly, and annual variation in strain and did not find a significant association with hospital mortality19; as conditions in acute care hospitals change rapidly, it is possible that measuring strain monthly may be too infrequent to detect strain-associated changes in outcomes. The only study finding a statistically significant decrease in mortality during strained times reported decreased mortality for patients discharged on days with increased ICU admissions, but no change in mortality using other measures of strain; this was also the only study to measure strain at ICU discharge.15
While almost all studies adjusted for risk of patient mortality in multivariable analyses (Online Appendix), two studies specifically analyzed mortality for patients who had diagnoses that were likely unrelated to the cause of strain.11 , 49 In a large study comparing US hospitals with an increased number of admissions during the 2009 Influenza H1N1 pandemic (“strained” hospitals) to hospitals with no increased admissions, Rubinson et al. reported an approximately 15–20% increase in the odds of hospital mortality for patients admitted to strained hospitals with stroke or acute myocardial infarction.11
Association Between Capacity Strain and Other Outcomes
Eight studies examined the association between capacity strain and nonlethal adverse events,22 , 30 – 32 , 38 , 44 , 45 , 47 with five of eight identifying a statistically significant association between strain and aspiration pneumonia,22 methicillin-resistant Staphylococcus aureus infection,44 Clostridium difficile infection,47 or adverse events in general.31 , 45 Of two studies including children, one described an almost doubling in patient-related adverse events during times of high pediatric ICU occupancy,45 while one found no significant association between neonatal ICU occupancy immediately before admission and development of nosocomial bacteremia.32
Of 15 studies examining the relationship between capacity strain and hospital, ICU, or postoperative length of stay (LOS), 10 reported a significant association between strain and increased LOS16 , 20 , 21 , 23 , 26 , 27 , 34 , 42 , 49 , 54; both pediatric studies reported an association between strain and increased LOS.23 , 26 The magnitude of increase in LOS ranged from 1 h23 to more than 1 day27; the greatest increases in LOS were reported in studies that examined strain during mass casualty incidents.27 , 49 The previously described study that measured capacity strain at ICU discharge reported that patients discharged from the ICU on days with high ICU census, acuity, and admissions had shorter ICU and post-ICU LOS.15
Seventeen studies examined the relationship between capacity strain and additional outcomes, such as ICU or hospital readmission,12 , 15 , 19 , 23 , 26 , 28 , 29 , 34 , 42 representation to the ED,52 ICU admission,21 , 46 delayed testing or treatment,30 , 54 low Apgar scores,46 and composite measures including morbidity and mortality.32 , 50 , 51 All but six of these studies reported significant associations between capacity strain and outcomes.23 , 29 , 32 , 34 , 46 , 52
Benefits and Harms of Interventions to Improve Care During Times of Capacity Strain
We did not find any randomized studies of interventions to improve care during times of capacity strain; all but one of the eight experimental studies utilized historical controls only60 (Table 2). Types of interventions varied greatly and included interventions to increase bed availability,55 , 58 , 59 , 62 decrease inefficiency and improve patient flow in busy hospitals,57 , 61 coordinate care during mass casualty incidents,56 and limit spread of an emerging infectious illness during an epidemic.60 Interventions were not associated with improved health outcomes in any studies; seven studies described post-intervention improvements in time-based measures (e.g., hospital LOS, time to surgery), ambulance diversion, or use of non-trauma ICUs for trauma patients.55 – 59 , 61 , 62 None of the studies separately analyzed outcomes for children.
Table 2.
Studies Describing Interventions to Improve Care During Times of Capacity Strain
| Author, year of publication, country | Study years | Number of patients. Hospital characteristics, Patient diagnoses | Metric to define capacity strain | Intervention | Key results |
|---|---|---|---|---|---|
| Bhakta, 2013, USA | 2009-2011 | 529 adults Urban trauma center with 3 trauma ICUs Trauma |
Trauma patients boarded in ED or admitted to a non-trauma ICU bed due to no available Trauma ICU bed. Analysis not restricted to times of capacity strain | Implementation of 24/7 open trauma bed protocol in designated trauma ICUs to facilitate rapid admission | No change in mortality, ICU and hospital LOS, and ICU readmissions. Mean ED LOS decreased from 4.2 to 3.1 h, percentage of ICU patients admitted to trauma ICU increased from 83 to 93% |
| Einav, 2009, Israel | 2001-2006 | 531 adults Urban trauma center Victims of MCIs |
MCI (terrorist attack sufficient in size to activate district emergency medical system) and ≥10 casualties or ≥4 severely injured casualties in a brief period of time | Assignment of a physician or nurse case manager to each MCI patient to guide workup, treatment, and transfer decisions | No change in mortality. Several time-based measures improved: Time to first chest x-ray decreased 24 min, time from admission to OR decreased >3 h, and hospital LOS for patients with severe injuries decreased by ≥50% |
| Howell, 2010, USA | 2005-2007 | 33,721 adults Urban trauma center None specified |
Hours on ambulance diversion due to “yellow alert” (ED experiencing temporary overwhelming overload) or “red alert” (no critical care beds available). Analysis not restricted to times of capacity strain | Implementation of active bed management: Hospitalist physician assigned as bed manager, makes triage decisions collaboratively with ED physicians, proactively assesses bed availability | No change in ICU mortality, ICU LOS, ICU admissions after original admission to non-ICU, or ICU readmissions. ED LOS decreased for patients admitted to ICUs. Yellow alert status hours decreased 6% and red alert status hours decreased 27% |
| Kastrup, 2012, Germany | 2008-2011 | 9,286 adults & children Urban teaching hospital Post-surgical patients needing intensive or intermediate care |
None. Analysis not restricted to times of capacity strain | Institution of 24-h staffing of PACU by ICU nurse and in-house critical care physician to allocate postoperative patients to ICU, intermediate care unit, or PACU | No change in mortality for ICU patients. Mean hospital LOS (includes additional post-surgical patients) decreased (8.3 to 7.7 days), mean time from admit to surgery for all operative patients decreased |
| Lo, 2014, Hong Kong | 2009 | 1,834 adults Regional hospital None specified |
None. Analysis not restricted to times of capacity strain | Institution of emergency medicine ward (similar to short-stay unit) | Decrease in mean hospital LOS from 5.2 to 4.1 days. No change in ED LOS |
| Stukel, 2008, Canada | 2000-2003 | Not reported 7 urban hospitals in 3 cities 7 common diagnoses |
Toronto SARS epidemic (defined by dates). Compared pre-SARS to SARS for Toronto and 2 other cities | Restricted medical admissions during SARS outbreak to limit nosocomial spread | No change in mortality. No systematic change in hospital readmission |
| Toomath, 2014, New Zealand | 2009-2013 | 49,319 adults Urban regional hospital None specified |
None. Analysis not restricted to times of capacity strain | Redesign of medical inpatient service: Geographically based teams, daily patient redistribution, less uneven staffing | Mean hospital LOS decreased from 3.5 to 3.1 days. No change in 7-day readmission rates |
| Wertheimer, 2014, USA | 2011-2013 | 5,812 adults 2 acute care units in urban academic hospital None specified |
None. Analysis not restricted to times of capacity strain | Intervention to increase discharges before noon: Interdisciplinary rounds, pre-discharge checklists, communication to stakeholders, daily leadership meetings, real-time feedback | Decrease in standardized hospital LOS by 10%. No change in 30-day readmission rates |
ED: Emergency department. ICU: Intensive care unit. LOS: Length of stay. MCI: Mass casualty incident. OR: Operating room. SARS: Severe acute respiratory syndrome
DISCUSSION
This systematic review found that hospital capacity strain in highly developed countries was associated with increased patient mortality in 9 of 12 studies in ICU settings and in 18 of 30 studies overall. Only 5 of 41 included observational studies did not find a statistically significant association between strain and worsened patient health outcomes or intermediate outcomes.15 , 17 , 29 , 38 , 40 , 52 The pediatric literature is very limited, with only four observational studies and no experimental studies separately analyzing outcomes for children.23 , 26 , 32 , 45 There was marked heterogeneity in study methods, including the metrics used to define capacity strain, hospital settings, patient populations, outcomes examined, and study quality. We found only eight reports of the health effects of interventions to improve care during times of capacity strain, none of which were randomized studies. Though seven of these eight studies described improvements in process measures, none reported an improvement in patient health outcomes after implementing the intervention.
A key challenge to understanding the health effects of hospital capacity strain is the lack of standard terminology and classification to define strain. Studies included in this review used very different terms to describe capacity strain, from general descriptions (e.g., “strained,”14 “busy,”15 or high “workload”31 , 32 , 41) to descriptions based on the number of admitted patients (e.g., “crowding” or “overcrowding,”26 , 53 high “census” or “occupancy,”17 , 18 , 24 , 35 , 41 , 44 , 47 , 50) to descriptions based on the number of new patients (e.g., “admission volume”19). A subset of studies used terms often found in trauma or public health emergency literature (e.g., “surge,”11 “mass casualty incident,”27 or “multiple casualty incident”49); others used sequelae of high inpatient census to define strain (e.g., “ED boarding”16 , 20 , 21 , 23 , 30 , 38 , 43 or “time from receiving the order for a bed and leaving the ED,”25 “lack of beds”42 or “refused admission due to full unit,”36 “delayed admission,”40 “boarding”22 or “outlying”42 or “bedspacing”52 in non-primary units). This lack of standard terminology contributed to differences in how strain was conceptualized by study authors, i.e., whether it was based on changing patient occupancy, acuity, or turnover or whether it was measured indirectly (Online Appendix). Even studies that used similar underlying terminology (e.g., occupancy) varied greatly in strain classification; while some studies examined the effect of occupancy as a continuous variable, others classified strain based on a threshold in percentage occupancy, and others chose occupancy thresholds indexed to a hospital’s or unit’s usual occupancy as reflected by deviation from mean or median occupancy. One study examined strain at the time of ICU discharge, and the finding that ICU and post-ICU length of stay decreased for patients discharged from the ICU during strained times raises the possibility that strain may have led to improved care efficiency, though at the cost of increased ICU readmissions.15 The resulting heterogeneity in strain classification precluded meta-analysis and limited more detailed qualitative assessments of the relationship between strain and health outcomes. To improve individual study quality and between-study consistency, we suggest that future studies (1) use direct measures of capacity strain based on patient census, acuity, and turnover rather than indirect measures, (2) index strain to usual conditions, such as median and interquartile range, (3) explore non-linear relationships between strain and outcomes, and (4) measure strain over a short enough time interval (minutes to days) to avoid contamination of “strained” vs. “non-strained” groups.
A second key challenge to understanding the relationship between hospital strain and outcomes is the lack of a consistent conceptual approach. Hospitals must consistently provide high-quality care in spite of relatively fixed resources and significant fluctuations in patient needs. An imbalance between patient needs and available resources creates resource strain, but such an imbalance may be due to either increased needs or decreased resources and may be acute or chronic. Chronic resource strain may result from lack of any essential resource and may compromise a hospital’s ability to provide safe care. Adequate staffing may be the single most critical resource to maintaining care quality, and shortfalls in nurse or physician staffing have been linked to increased patient mortality and decreased care efficiency.63 – 68 We focused on a subset of resource strain called “capacity strain,” applying a conceptual model that defines the cause of capacity strain as the temporal variation in patient needs as defined by census, acuity, and turnover.5 Thus, the purpose behind the concept of capacity strain, and the focus of this review, is not to assess a hospital’s inherent ability to provide high-quality care, but rather its ability to provide high-quality care when patient needs rise. Even within a hospital, individual units may face strain resulting from increased patient needs at different times; it is unclear to what extent strain and its relationship to care quality are localized to specific areas within a hospital and to what extent this localization varies. A coherent theoretical framework for hospital resource strain, which includes both hospital- and patient-driven factors and accounts for both temporal variation in supply and demand as well as the interdependence of different settings (e.g., EDs, inpatient units, nearby hospitals) would provide essential context when planning and interpreting studies of strain.
A third challenge to understanding the relationship between strain and outcomes is that variation in settings is likely to influence the relationship. Some settings may have high baseline levels of strain and thus have less reserve to cope with increases in patient needs. While quality of care may degrade gradually and linearly as patient needs increase, we agree with prior authors that it is more likely that the system is resilient to changing patient needs up to a certain “tipping point,” after which care may degrade rapidly.5 , 69 Thus, chronically high hospital census in Denmark (almost 40% of patient days were spent in hospitals with over 100% bed occupancy) may partly explain the association between high occupancy at the time of hospital admission and a 9% increase in mortality.35 It is possible that patient risk is dependent on the timing of capacity strain relative to an individual patient’s hospitalization or even on the total amount of time above a threshold level of strain; these concepts are not well addressed in the existing literature. In addition, more fundamental differences in care delivery systems may affect the relationship between strain and outcomes. For example, the finding by Intas et al. of an almost six-fold increase in hospital mortality among patients with >6 h of ED boarding prior to ICU admission may be due in part to the inability of Greek EDs to initiate ICU treatments at the time of the study,43 and may not be generalizable to settings where ICU-level care is routinely provided in the ED. Lastly, some hospitals may be more resilient than others to the potentially negative effects of strain, which may have contributed to heterogeneity in findings among studies included in this review. While factors influencing such resilience were not reported in these studies, understanding and replicating practices employed by resilient hospitals is an important area of future research.
Limitations
The lack of consistent terminology, classification, and theoretical model in this field makes study selection very challenging. While we consistently applied inclusion and exclusion criteria based on a clear construct and clearly defined outcomes, we acknowledge that no inclusion strategy is perfect when the divisions between related fields are blurred. This may be particularly true for experimental studies; many types of interventions implemented for different reasons (e.g., reorganizing care processes to decrease inefficiencies or improving bed utilization data capture) could lead to improved care quality during times of capacity strain, regardless of their intent. Though almost all included observational studies analyzed the association between strain and outcomes adjusted for patient-level factors, unmeasured differences in patient risk characteristics may have been partly responsible for worsened outcomes during times of strain.
Quality assessment is subject to limitations of the assessment tools. The NOS was not specifically designed to assess risk of bias for hospital-based studies of mortality and thus may not have been an ideal tool; similarly, the Cochrane Risk of Bias Tool was not primarily designed to assess risk of bias in pre-post experimental studies. The significant heterogeneity among included studies, particularly in study settings and strain classification, precluded meta-analysis and limited the ability to draw more precise conclusions regarding the relationship between strain and health outcomes. Lastly, findings of studies performed in highly developed countries may not apply in resource-restricted settings; even in highly developed countries, there may be significant variation in the relationship between strain and outcomes in different hospital settings.
CONCLUSIONS
Hospital capacity strain is likely associated with increased patient mortality and worsening of other health outcomes in highly developed countries, indicating that care quality may degrade during times of strain. There are no interventions that have been shown to improve patient outcomes during times of capacity strain. Understanding the relationship between strain and outcomes is challenged by lack of consistent terminology, classification, and theoretical framework, and by variation in study settings. It is likely that some hospitals are more resilient than others during times of strain, and understanding and replicating practices employed by resilient hospitals are essential to improving care in busy hospitals.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 80 kb)
Acknowledgments
We are indebted to reference librarians Andrew Hamilton, MS, and Robyn Painter, MA-LIS, for their assistance creating search strategies, and to Marian McDonough, PharmD, Benjamin Sun, MD, MPP, and K. John McConnell, PhD, for general guidance.
Compliance with Ethical Standards
Conflict of Interest
Carl Eriksson and Craig Newgard received funding from the US Agency for Healthcare Research and Quality (AHRQ) during the conduct of the study. All other authors declare no conflicts of interest.
Funding Source
US Agency for Healthcare Research and Quality, 1 K12 HS022981 01. The funding agency played no role in the design or conduct of this research.
Footnotes
Registration: International Prospective Register of Systematic Reviews (PROSPERO), Registration No. CRD42015024758
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3936-3) contains supplementary material, which is available to authorized users.
References
- 1.Oxford University Press. “strain”. Oxford Dictionaries.
- 2.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 4.Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106–15. doi: 10.1111/jnu.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halpern SD. ICU capacity strain and the quality and allocation of critical care. Curr Opin Crit Care. 2011;17(6):648–57. doi: 10.1097/MCC.0b013e32834c7a53. [DOI] [PubMed] [Google Scholar]
- 6.Christian MD, Devereaux AV, Dichter JR, Rubinson L, Kissoon N. Introduction and executive summary: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 Suppl):8s–34. doi: 10.1378/chest.14-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanter RK, Moran JR. Hospital emergency surge capacity: an empiric New York statewide study. Ann Emerg Med. 2007;50(3):314–9. doi: 10.1016/j.annemergmed.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed June 23 2016.
- 11.Rubinson L, Mutter R, Viboud C, Hupert N, Uyeki T, Creanga A, et al. Impact of the fall 2009 influenza A(H1N1)pdm09 pandemic on US hospitals. Med Care. 2013;51(3):259–65. doi: 10.1097/MLR.0b013e31827da8ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evans WN, Kim B. Patient outcomes when hospitals experience a surge in admissions. J Health Econ. 2006;25(2):365–88. doi: 10.1016/j.jhealeco.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Jenkins PC, Richardson CR, Norton EC, Cooke CR, Banerjee M, Nathens AB, et al. Trauma surge index: advancing the measurement of trauma surges and their influence on mortality. J Am Coll Surg. 2015;221(3):729–38.e1. doi:10.1016/j.jamcollsurg.2015.05.016. [DOI] [PubMed]
- 14.Gabler NB, Ratcliffe SJ, Wagner J, Asch DA, Rubenfeld GD, Angus DC, et al. Mortality among patients admitted to strained intensive care units. Am J Respirat Critic Care Med. 2013;188(7):800–6. doi: 10.1164/rccm.201304-0622OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159(7):447–55. doi: 10.7326/0003-4819-159-7-201310010-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, Delay-Ed study group Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477–83. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 17.Iwashyna TJ, Kramer AA, Kahn JM. Intensive care unit occupancy and patient outcomes. Crit Care Med. 2009;37(5):1545–57. doi: 10.1097/CCM.0b013e31819fe8f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schilling PL, Campbell DA, Jr, Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care. 2010;48(3):224–32. doi: 10.1097/MLR.0b013e3181c162c0. [DOI] [PubMed] [Google Scholar]
- 19.Marcin JP, Romano PS. Impact of between-hospital volume and within-hospital volume on mortality and readmission rates for trauma patients in California. Crit Care Med. 2004;32(7):1477–83. doi: 10.1097/01.CCM.0000127781.08985.03. [DOI] [PubMed] [Google Scholar]
- 20.Derose SF, Gabayan GZ, Chiu VY, Yiu SC, Sun BC. Emergency department crowding predicts admission length-of-stay but not mortality in a large health system. Med Care. 2014;52(7):602–11. doi: 10.1097/MLR.0000000000000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singer AJ, Thode HC, Jr, Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18(12):1324–9. doi: 10.1111/j.1553-2712.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 22.Pascual JL, Blank NW, Holena DN, Robertson MP, Diop M, Allen SR, et al. There’s no place like home: boarding surgical ICU patients in other ICUs and the effect of distances from the home unit. J Trauma Acute Care Surg. 2014;76(4):1096–102. doi: 10.1097/TA.0000000000000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bekmezian A, Chung PJ. Boarding admitted children in the emergency department impacts inpatient outcomes. Pediatr Emerg Care. 2012;28(3):236–42. doi: 10.1097/PEC.0b013e3182494b94. [DOI] [PubMed] [Google Scholar]
- 24.Clark K, Normile L. Nursing informatics and data collection from the electronic medical record: study of characteristics, factors and occupancy impacting outcomes of critical care admissions from the emergency department. Health Inform J. 2012;18(4):309–19. doi: 10.1177/1460458212454023. [DOI] [PubMed] [Google Scholar]
- 25.Clark K, Normile LB. Influence of time-to-interventions for emergency department critical care patients on hospital mortality. J Emerg Nurs. 2007;33(1):6–13. doi: 10.1016/j.jen.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Lorch SA, Millman AM, Zhang X, Even-Shoshan O, Silber JH. Impact of admission-day crowding on the length of stay of pediatric hospitalizations. Pediatrics. 2008;121(4):e718–30. doi: 10.1542/peds.2007-1280. [DOI] [PubMed] [Google Scholar]
- 27.Abir M, Choi H, Cooke CR, Wang SC, Davis MM. Effect of a mass casualty incident: clinical outcomes and hospital charges for casualty patients versus concurrent inpatients. Acad Emerg Med. 2012;19(3):280–6. doi: 10.1111/j.1553-2712.2011.01278.x. [DOI] [PubMed] [Google Scholar]
- 28.Baker DR, Pronovost PJ, Morlock LL, Geocadin RG, Holzmueller CG. Patient flow variability and unplanned readmissions to an intensive care unit. Crit Care Med. 2009;37(11):2882–7. doi: 10.1097/CCM.0b013e3181b01caf. [DOI] [PubMed] [Google Scholar]
- 29.Elliott DJ, Young RS, Brice J, Aguiar R, Kolm P. Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786–93. doi: 10.1001/jamainternmed.2014.300. [DOI] [PubMed] [Google Scholar]
- 30.Liu SW, Chang Y, Weissman JS, Griffey RT, Thomas J, Nergui S, et al. An empirical assessment of boarding and quality of care: delays in care among chest pain, pneumonia, and cellulitis patients. Acad Emerg Med. 2011;18(12):1339–48. doi: 10.1111/j.1553-2712.2011.01082.x. [DOI] [PubMed] [Google Scholar]
- 31.Weissman JS, Rothschild JM, Bendavid E, Sprivulis P, Cook EF, Evans RS, et al. Hospital workload and adverse events. Med Care. 2007;45(5):448–55. doi: 10.1097/01.mlr.0000257231.86368.09. [DOI] [PubMed] [Google Scholar]
- 32.Tucker J, Group UKNSS. Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet. 2002;359(9301):99–107. doi: 10.1016/S0140-6736(02)07366-X. [DOI] [PubMed] [Google Scholar]
- 33.Iapichino G, Gattinoni L, Radrizzani D, Simini B, Bertolini G, Ferla L, et al. Volume of activity and occupancy rate in intensive care units. association with mortality. Intensive Care Med. 2004;30(2):290–7. doi: 10.1007/s00134-003-2113-4. [DOI] [PubMed] [Google Scholar]
- 34.Schwierz C, Augurzky B, Focke A, Wasem J. Demand, selection and patient outcomes in German acute care hospitals. Health Econ. 2012;21(3):209–21. doi: 10.1002/hec.1706. [DOI] [PubMed] [Google Scholar]
- 35.Madsen F, Ladelund S, Linneberg A. High levels of bed occupancy associated with increased inpatient and thirty-day hospital mortality in Denmark. Health Aff. 2014;33(7):1236–44. doi: 10.1377/hlthaff.2013.1303. [DOI] [PubMed] [Google Scholar]
- 36.Robert R, Reignier J, Tournoux-Facon C, Boulain T, Lesieur O, Gissot V, et al. Refusal of intensive care unit admission due to a full unit: impact on mortality. Am J Respirat Critic Care Med. 2012;185(10):1081–7. doi: 10.1164/rccm.201104-0729OC. [DOI] [PubMed] [Google Scholar]
- 37.Plunkett PK, Byrne DG, Breslin T, Bennett K, Silke B. Increasing wait times predict increasing mortality for emergency medical admissions. European J Emerg Med. 2011;18(4):192–6. doi: 10.1097/MEJ.0b013e328344917e. [DOI] [PubMed] [Google Scholar]
- 38.Gilligan P, Winder S, Singh I, Gupta V, Kelly PO, Hegarty D. The Boarders in the Emergency Department (BED) study. Emerg Med J. 2008;25(5):265–9. doi: 10.1136/emj.2007.048173. [DOI] [PubMed] [Google Scholar]
- 39.Serafini F, Fantin G, Brugiolo R, Lamanna O, Aprile A, Presotto F. Outlier admissions of medical patients: prognostic implications of outlying patients. The experience of the Hospital of Mestre. Italian J Med. 2015;9(3):299–302. [Google Scholar]
- 40.O’Callaghan DJP, Jayia P, Vaughan-Huxley E, Gribbon M, Templeton M, Skipworth JRA, et al. An observational study to determine the effect of delayed admission to the intensive care unit on patient outcome. Crit Care. 2012;16(5). doi:10.1186/cc11650. [DOI] [PMC free article] [PubMed]
- 41.Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356(9225):185–9. doi: 10.1016/S0140-6736(00)02478-8. [DOI] [PubMed] [Google Scholar]
- 42.Stowell A, Claret PG, Sebbane M, Bobbia X, Boyard C, Genre Grandpierre R. Hospital out-lying through lack of beds and its impact on care and patient outcome. Scandinavian J Trauma, Resuscitation Emerg Med. 2013;21:17. doi: 10.1186/1757-7241-21-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Intas G, Stergiannis P, Chalari E, Tsoumakas K, Fildissis G. The impact of ED boarding time, severity of illness, and discharge destination on outcomes of critically ill ED patients. Adv Emerg Nursing J. 2012;34(2):164–9. doi: 10.1097/TME.0b013e318251515f. [DOI] [PubMed] [Google Scholar]
- 44.Howie AJ, Ridley SA. Bed occupancy and incidence of Methicillin-resistant Staphylococcus aureus infection in an intensive care unit. Anaesthesia. 2008;63(10):1070–3. doi: 10.1111/j.1365-2044.2008.05575.x. [DOI] [PubMed] [Google Scholar]
- 45.Tibby SM, Correa-West J, Durward A, Ferguson L, Murdoch IA. Adverse events in a paediatric intensive care unit: relationship to workload, skill mix and staff supervision. Intensive Care Med. 2004;30(6):1160–6. doi: 10.1007/s00134-004-2256-y. [DOI] [PubMed] [Google Scholar]
- 46.Tucker J, Parry G, Penney G, Page M, Hundley V. Is midwife workload associated with quality of process of care (continuous electronic fetal monitoring [CEFM]) and neonatal outcome indicators? a prospective study in consultant-led labour wards in Scotland. Paediatr Perinat Epidemiol. 2003;17(4):369–77. doi: 10.1046/j.1365-3016.2003.00524.x. [DOI] [PubMed] [Google Scholar]
- 47.Ahyow LC, Lambert PC, Jenkins DR, Neal KR, Tobin M. Bed occupancy rates and hospital-acquired Clostridium difficile infection: a cohort study. Infect Contrl Hospital Epidemiol. 2013;34(10):1062–9. doi: 10.1086/673156. [DOI] [PubMed] [Google Scholar]
- 48.Yergens DW, Ghali WA, Faris PD, Quan H, Jolley RJ, Doig CJ. Assessing the association between occupancy and outcome in critically Ill hospitalized patients with sepsis. BMC Emergency Med. 2015;15(1). doi:10.1186/s12873-015-0049-y. [DOI] [PMC free article] [PubMed]
- 49.Ball CG, Kirkpatrick AW, Mulloy RH, Gmora S, Findlay C, Hameed SM. The impact of multiple casualty incidents on clinical outcomes. J Trauma-Injury Infect Critic Care. 2006;61(5):1036–9. doi: 10.1097/01.ta.0000231764.00067.54. [DOI] [PubMed] [Google Scholar]
- 50.Chrusch CA, Olafson KP, McMillan PM, Roberts DE, Gray PR. High occupancy increases the risk of early death or readmission after transfer from intensive care. Crit Care Med. 2009;37(10):2753–8. doi: 10.1097/CCM.0b013e3181a57b0c. [DOI] [PubMed] [Google Scholar]
- 51.Shah PS, Mirea L, Ng E, Solimano A, Lee SK. Association of unit size, resource utilization and occupancy with outcomes of preterm infants. J Perinatol. 2015;35(7):522–9. doi: 10.1038/jp.2015.4. [DOI] [PubMed] [Google Scholar]
- 52.Liu J, Griesman J, Nisenbaum R, Bell CM. Quality of care of hospitalized internal medicine patients bedspaced to non-internal medicine inpatient units. PLoS ONE. 2014;9(9). doi:10.1371/journal.pone.0106763. [DOI] [PMC free article] [PubMed]
- 53.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184(5):208–12. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 54.Richardson D, McMahon KL. Emergency Department access block occupancy predicts delay to surgery in patients with fractured neck of femur. Emerg Med Austral. 2009;21(4):304–8. doi: 10.1111/j.1742-6723.2009.01201.x. [DOI] [PubMed] [Google Scholar]
- 55.Bhakta A, Bloom M, Warren H, Shah N, Casas T, Ewing T, et al. The impact of implementing a 24/7 open trauma bed protocol in the surgical intensive care unit on throughput and outcomes. J Trauma Acute Care Surg. 2013;75(1):97–101. doi: 10.1097/TA.0b013e31829849e5. [DOI] [PubMed] [Google Scholar]
- 56.Einav S, Schecter WP, Matot I, Horn JK, Hersch M, Reissman P, et al. Case managers in mass casualty incidents. Ann Surg. 2009;249(3):496–501. doi: 10.1097/SLA.0b013e31819a6f17. [DOI] [PubMed] [Google Scholar]
- 57.Howell E, Bessman E, Marshall R, Wright S. Hospitalist bed management effecting throughput from the emergency department to the intensive care unit. J Crit Care. 2010;25(2):184–9. doi: 10.1016/j.jcrc.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 58.Kastrup M, Seeling M, Barthel S, Bloch A, le Claire M, Spies C. Effects of intensivist coverage in a post-anaesthesia care unit on surgical patients’ case mix and characteristics of the intensive care unit. Critic Care (London, England). 2012;16(4):R126. doi:10.1186/cc11428. [DOI] [PMC free article] [PubMed]
- 59.Lo SM, Choi KTY, Wong EML, Lee LLY, Yeung RSD, Chan JTS, et al. Effectiveness of Emergency Medicine Wards in reducing length of stay and overcrowding in emergency departments. Int Emerg Nursing. 2014;22(2):116–20. doi: 10.1016/j.ienj.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 60.Stukel TA, Schull MJ, Guttmann A, Alter DA, Li P, Vermeulen MJ, et al. Health impact of hospital restrictions on seriously ill hospitalized patients: lessons from the Toronto SARS outbreak. Med Care. 2008;46(9):991–7. doi: 10.1097/MLR.0b013e3181792525. [DOI] [PubMed] [Google Scholar]
- 61.Toomath R, Szecket N, Nahill A, Denison T, Spriggs D, Lay C, et al. Medical service redesign shares the load saving 6000 bed days and improving morale. Intern Med J. 2014;44(8):785–90. doi:10.1111/imj.12477. [DOI] [PubMed]
- 62.Wertheimer B, Jacobs RE, Bailey M, Holstein S, Chatfield S, Ohta B, et al. Discharge before noon: an achievable hospital goal. J Hospital Med (Online) 2014;9(4):210–4. doi: 10.1002/jhm.2154. [DOI] [PubMed] [Google Scholar]
- 63.Shekelle PG. Nurse-patient ratios as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 PART 2):404–9. doi:10.7326/0003-4819-158-5-201303051-00007. [DOI] [PubMed]
- 64.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007;45(12):1195–204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 65.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically III patients: a systematic review. J Am Med Assoc. 2002;288(17):2151–62. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 66.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 67.Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–45. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 68.Michtalik HJ, Yeh HC, Pronovost PJ, Brotman DJ. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–7. doi: 10.1001/jamainternmed.2013.1864. [DOI] [PubMed] [Google Scholar]
- 69.Kuntz L, Mennicken R, Scholtes S. Stress on the ward: evidence of safety tipping points in hospitals. Manag Sci. 2015;61(4):754–71. doi: 10.1287/mnsc.2014.1917. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 80 kb)