Abstract
Although several surgical techniques have been described to perform meniscal allograft transplantation with good clinical results and although different methods of capsular stabilization can be found in the literature, there is no standard surgical technique to prevent a common complication in the most of series: the tendency to a radial displacement or extrusion of the transplanted menisci. We present a simple, reproducible, and implant-free technique to perform a lateral capsular fixation (capsulodesis) at the time of only the soft-tissue fixation technique of meniscal allograft transplantation in an effort to reduce or prevent the risk of graft extrusion. Using a minimum of two 2.4-mm tunnels drilled from the contralateral side of the tibia with the help of a regular tibial anterior cruciate ligament guide, a capsular attachment to the lateral tibial plateau is obtained.
In an attempt to replace the lost meniscal tissue as well as to prevent progressive deterioration of the joint, meniscal allograft transplantation (MAT) was introduced into clinical practice.1 Since then, several surgical techniques have been described for MAT with good short-, mid-, and even long-term clinical results in cases of painful meniscectomized compartments of the knee.2
However, most of the series found a tendency to a radial displacement or extrusion of the transplanted menisci.3 In the same way, meniscal transplants have been shown to extrude more than normal menisci.4 Extrusion is seen shortly after transplantation and tends to stabilize over time.5 From a biomechanical standpoint, an extruded meniscus results in decreased resistance to hoop strain. However, it has not been shown to have any clinical relevance. Although the final significance of extrusion is unknown, the anomalous position of those grafts causes concern among surgeons. In recent years, several technical steps have been implemented to limit or prevent allograft extrusion.
The aim of this study was to present a simple, reproducible, and implant-free technique to perform a lateral capsular fixation (capsulodesis) at the time of lateral MAT in an effort to reduce or prevent graft extrusion.
Surgical Technique
The arthroscopic lateral capsulodesis is performed in cases where a redundant capsule is observed or where extrusion of the midbody of the lateral meniscus has been identified with magnetic resonance imaging before MAT.
Fresh-frozen (−80°C), nonirradiated, bone-free, non–antigen-matched meniscal allografts were used in this series. Local authorized tissue banks supplied the allografts. Allograft sizing was performed in accordance with the method described by Pollard et al.6
The surgical technique is completely arthroscopic and includes only soft-tissue fixation. Routine anterolateral and anteromedial portals are performed (Video 1). Two 5-mm bone tunnels are drilled at the anatomic sites of the lateral meniscal attachments, one at the anterior horn and the other at the posterior horn. In every case, No. 2 high-strength sutures (Hi-Fi, ConMed, Largo, FL) with a Krackow mattress are placed at both horns. One additional vertical mattress suture is placed at the junction between the posterior horn and the body of the meniscus. This suture will later help in introducing the graft into the joint.
Lateral Capsulodesis
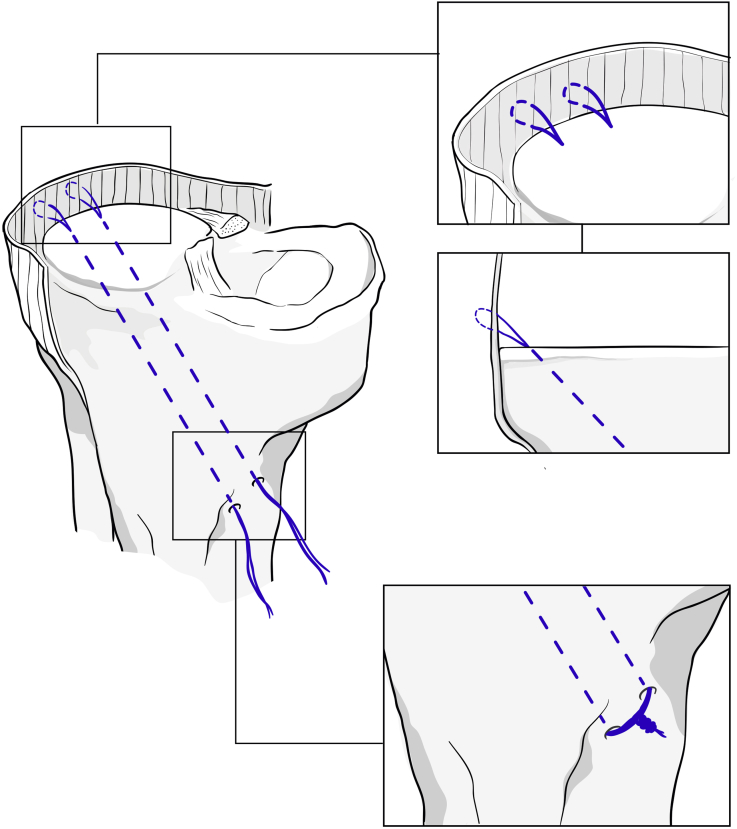
A motorized arthroscopy shaver is used to remove any marginal osteophyte on the lateral edge of the tibial plateau. The place where the lateral capsule is most displaced from the edge of the lateral tibial plateau is identified. In this area, a minimum of two 2.4-mm tibial tunnels are performed (Fig 1). The tunnels are drilled from the anteromedial aspect of the tibia with the help of an anterior cruciate ligament tibial guide (Pinn-ACL Guide, ConMed) with a distance of 1 cm between each one (Fig 2). Care should be taken to avoid tunnel collision. Using a suture passer, each tunnel is identified by a different colored thread, leaving a small loop inside the joint to retrieve the capsulodesis suture strand (Fig 3). Then, two 19-gauge spinal needles loaded with a No. 1 PDS (polydioxanone) suture are used to pierce the peripheral rim of the meniscus remnant or the capsule with an outside-in technique. This shuttle suture is substituted by a high-strength suture and retrieved through each tibial tunnel (Fig 4). The 2 limbs are then tied to each other on the anteromedial tibial cortex, bringing together the capsule to the tibial plateau (Fig 5). This step must always be performed before the meniscal graft introduction and fixation. A step-by-step summary of this technique is provided in Table 1.
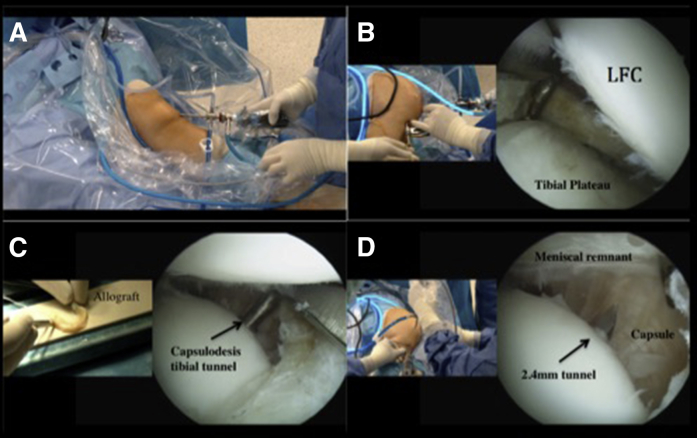
Fig 1.
Left knee image showing (A) patient positioning on the operating table. Arthroscopic image viewed through the anterolateral portal (B) drilling the posterior horn in the tibial plateau. (LFC, lateral femoral condyle.) Arthroscopic image through the anteromedial portal (C and D) showing the 2.4-mm tibial tunnel drilled from the anteromedial aspect of the tibia with the help of an anterior cruciate ligament tibial guide.
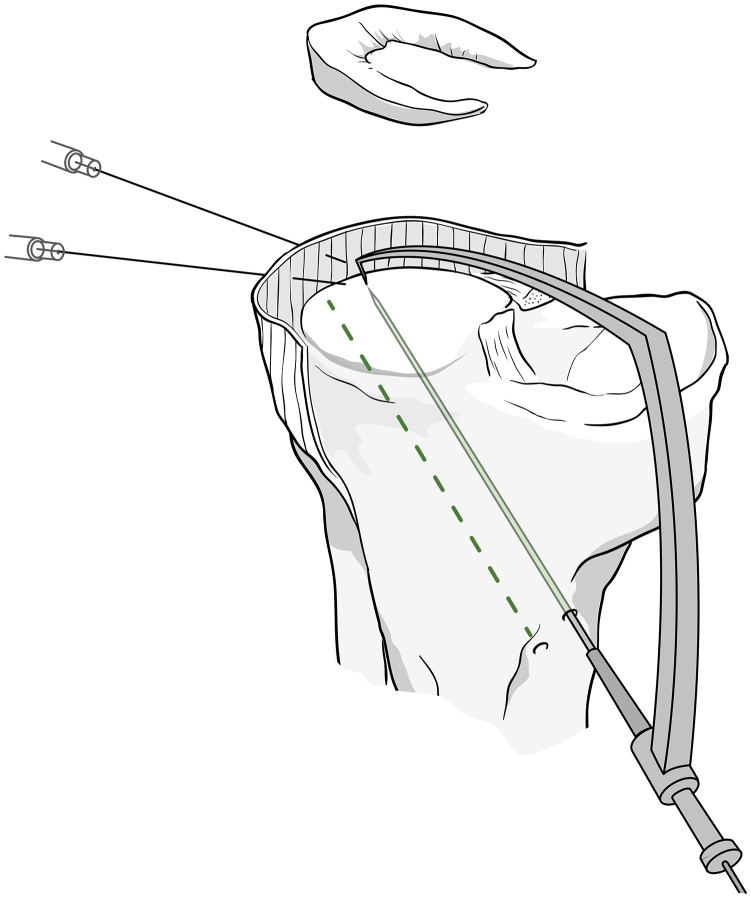
Fig 2.
Right knee, anteromedial view. Lateral capsulodesis tunnel placement using the anterior cruciate ligament tibial guide through the anteromedial portal.
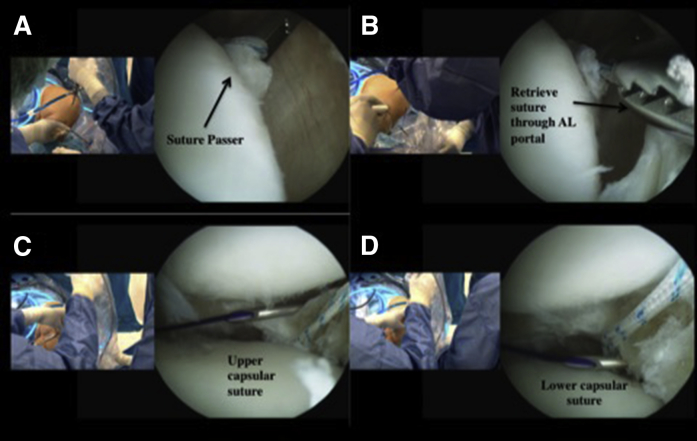
Fig 3.
Left knee, arthroscopic image through the anteromedial portal. Using a suture passer, (A) identify the tunnel leaving a small loop inside the joint (B) to retrieve the capsulodesis suture strand. Then use two 19-gauge spinal needles (C and D) loaded with No. 1 polydioxanone suture to pierce the peripheral rim of the meniscus remnant or the capsule with an outside-in technique. (AL, anterolateral.)
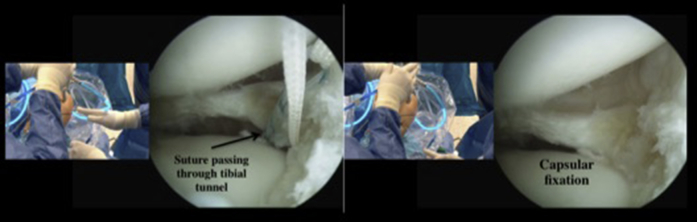
Fig 4.
Shuttle suture replaced by a high-strength strand and retrieved through the tibial tunnel. Tie the 2 suture ends together on the anteromedial tibial cortex to secure the capsulodesis.
Fig 5.
Capsular fixation suture passed through each transtibial tunnel and tied to each other on the anteromedial cortex fixing the capsule to the tibial plateau.
Table 1.
Step-by-Step Arthroscopic Lateral Capsular Fixation to Prevent Meniscal Allograft Extrusion
| Step | Description |
|---|---|
| 1 | The patient is placed in the supine position on the operating table. A well-padded high-thigh tourniquet is subsequently placed on the operative leg. |
| 2 | Standard anterolateral and anteromedial portals are created and the joint is visualized with a 30° arthroscope. |
| 3 | Perform joint evaluation to confirm the diagnosis and the absence of significant chondral lesions. |
| 4 | An arthroscopic shaver is inserted into the knee, and the remnants of the meniscal tissue are debrided to a bleeding rim. |
| 5 | Drill two 5-mm bone tunnels at the anatomic sites of the lateral meniscal horns attachments. |
| 6 | Use a shaver to remove any marginal osteophyte on the lateral edge of the tibial plateau and identify the place where the lateral capsule is most displaced. |
| 7 | Perform a minimum of two 2.4-mm tibial tunnels from the anteromedial aspect of the tibia with the help of an anterior cruciate ligament tibial guide with a distance of 1 cm between them. |
| 8 | Identify each tunnel with a different colored thread, leaving a small loop inside the joint to retrieve the capsulodesis suture strand. |
| 9 | Use two 19-gauge spinal needles loaded with a No. 1 polydioxanone suture to pierce the peripheral rim of the meniscus remnant or the capsule with an outside-in technique. |
| 10 | Replace this shuttle suture by a high-strength strand and retrieve it through each tibial tunnel. |
| 11 | Tie the 2 suture ends to each other on the anteromedial tibial cortex, and secure the capsulodesis. |
Graft Placement
Once the capsulodesis has been secured and the anterolateral portal enlarged, the posterior-horn suture is used to pull the meniscal allograft in place. The vertical stitch placed between the posterior horn and the body of the meniscus helps to accommodate the graft in the proper position by pulling the sutures from the posterolateral corner. The allograft is then fixed to the rim by combining all-inside meniscal repair implants (FasT-Fix, Smith & Nephew, Andover, MA) in the posterior horn and the meniscal body and an outside-in technique in the anterior horn. Finally, the sutures placed in the anterior and posterior horns are tied together over the tibial cortex. Pearls and pitfalls to performing this surgical procedure are listed in Table 2.
Table 2.
Pearls, Pitfalls, and Risks
| Pearls: |
| • The arthroscopic lateral capsulodesis is performed in cases where a redundant capsule is observed or where extrusion of the midbody of the lateral meniscus has been identified with magnetic resonance imaging before meniscal allograft transplantation (MAT). |
| • Remove any marginal osteophyte on the lateral edge of the tibial plateau. |
| • Perform a minimum of two 2.4-mm tibial tunnels from the anteromedial aspect of the tibia with the help of an anterior cruciate ligament tibial guide with a distance of 1 cm in between. |
| • Identify each tunnel to avoid tunnel collision. |
| • Using a suture passer, leave a small suture loop inside the joint to retrieve the capsulodesis suture strand. |
| • Use No. 1 polydioxanone as a shuttle suture, replace it by a high-strength strand, and retrieve it through each tibial tunnel. |
| • Tie the 2 suture ends on the anteromedial tibial cortex always before the meniscal graft introduction and fixation. |
| Pitfalls and risks: |
| • Failure to address concomitant conditions such as chondral lesions or instability will lead to poor results. |
| • An error in the sequence of tying the sutures, after graft introduction and fixation, can lead to poor results and MAT extrusion. |
| • To avoid tunnel collision, make sure to identify each tunnel and place the guide with a minimum of 1 cm of distance between them. |
| • Stiffness can occur if the patient is not able to follow the established rehabilitation protocol. Partial weight bearing with a knee immobilizer is allowed at 3 wk and progressed to full weight bearing at approximately 6 wk. Progressive range of motion without exceeding 90° of flexion until the fourth week is followed by unrestricted progression per tolerance. |
Rehabilitation Protocol
Partial weight bearing with a knee immobilizer is allowed at 3 weeks and progressed to full weight bearing at approximately 6 weeks. Progressive range of motion without exceeding 90° of flexion until the fourth week is followed by unrestricted progression per tolerance. Patients may return to a normal workload by the fourth month after surgery.
Discussion
Because MAT is carried out with the hope of preventing the progression of osteoarthritis, the presence of graft extrusion is a matter of concern for the surgeon. To avoid meniscal extrusion, a simple, implant-free capsulodesis technique is presented in this Technical Note.
Several factors have been related to an extruded meniscal allograft. They are the fixation method, the type of allograft (medial or lateral), the investigated meniscal area, and the graft size.
MAT fixation is crucial to preventing short- and mid-term complications due to altered knee kinematics. Although peripheral fixation is achieved with sutures in any of the available techniques, the fixation of meniscal horns may be achieved through either sutures or a bone plug or a bone bridge. In general, bone plugs are preferred for the medial meniscus when using bone-to-bone fixation and a bone bridge for the lateral meniscus. Some in vitro studies have shown that fixation with bone plugs is better compared with graft fixation without bone plugs in terms of the restoration of the normal contact mechanics of the knee.7, 8 Nonetheless, other biomechanical in vitro studies have shown no differences in the mean pull-out strength of the medial meniscus allograft between the 2 fixation methods.9 Moreover, MAT without bone plugs has shown good and excellent results in terms of pain relief and clinical and functional outcomes.10, 11, 12 Clinical studies comparing both fixation methods have shown no differences in clinical, functional, or radiographic outcomes.13 However, because suture-only fixation has shown a higher degree of meniscal extrusion,14 this capsulodesis technique was developed to prevent or decrease this lateral displacement.
Several technical recommendations have been made to limit or prevent allograft extrusion. Jang et al.15 reported that reducing the graft size by 5% decreases the percentage of extrusion without any adverse outcome either clinically or radiographically. Other studies showed that in the bone bridge technique, the risk of graft extrusion increases as the angle of the trough on the axial plane increases.16 Jeon et al.17 suggested that the excision of a peripheral osteophyte larger than 2 mm in the proximal tibial plateau was associated with less MAT extrusion. Some surgeons fix the meniscus body to the tibial plateau in an attempt to control graft extrusion. However, this maneuver may present the risk of limiting the normal mobility of the meniscus during knee motion.
A recent investigation showed that peripheral fixation in an adequate remnant meniscal rim is not only important to promoting healing of the graft but also crucial to prevent peripheral extrusion.18 In that sense, we are currently exploring the role that a capsule fixation to the tibial plateau might play. A list of advantages and limitations of our procedure can be found in Table 3.
Table 3.
Advantages and Limitations
| Advantages: |
| • Simple, reproducible, and implant-free technique |
| • Reduces and prevents the risk of graft extrusion |
| • Allows for versatility in terms of number of fixation points and locations |
| • No significant bone loss in the tibial plateau because the diameters of the drill holes are only 2.4 mm |
| • It does not interfere with subsequent magnetic resonance imaging and adds no additional costs |
| Limitations: |
| • Risk of tunnel collision |
| • Requirement for an outside-in technique with small incisions to perform the capsular suture |
Although different methods of capsular stabilization have been described, the present technique based on an implant-free lateral capsulodesis seems to be a valid, reliable, and easy method to prevent or decrease lateral MAT extrusion. It allows for versatility in terms of number of fixation points and locations, without a significant bone loss in the tibial plateau because the diameters of the drill holes are only 2.4 mm. It does not interfere with subsequent magnetic resonance imaging (Fig 6) and adds no additional costs.
Fig 6.

Coronal view of magnetic resonance imaging at 6 months postoperatively. We see the midbody position of the lateral meniscus allograft and the lateral capsulodesis tibial tunnel placement (arrows) with no extrusion of the graft.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C.M. receives support from ConMed Linvatec, Smith & Nephew, Surgival, BioIberica, Spanish Arthroscopy Association, and Spanish Ministry of Health, Social Service and Equality. He is also a board member of ESSKA. P.E.G. receives support from Spanish Arthroscopic Association, ConMed, and Hospital de Sant Pau, Barcelona, Spain.
Supplementary Data
0:00-0:04: Lateral capsular fixation: A reliable implant-free technique to prevent meniscal allograft extrusion. 0:04-0:11: The surgical technique was completely arthroscopic. Routine anterolateral and anteromedial portals were used. 0:12-0:21: This arthroscopic lateral capsulodesis for meniscal allograft transplantation is performed in cases where a redundant capsule is observed or where extrusion of the midbody of the meniscus has been identified with magnetic resonance imaging before meniscal transplantation. 0:22-0:29: Two 5-mm bone tunnels were drilled at the anatomic sites of meniscal attachment, one at the anterior horn and the other at the posterior horn. 0:30-0:45: Once the place where the lateral capsule is most displaced from the edge of the lateral tibial plateau is identified, stabilization is performed using a minimum of two 2.5-mm tunnels. The tunnels were drilled from the contralateral side of the tibia with the help of a regular tibial anterior cruciate ligament guide with a distance of 1 cm between those. Care should be taken to avoid tunnel collision. 0:46-1:05: Using a suture passer, each tunnel is identified, leaving a small loop inside the joint to retrieve the capsulodesis suture strand. 1:06-1:26: Then, 2 spinal needles loaded with a No. 2 polydioxanone suture are used to capture the peripheral rim of the meniscus with an outside-in technique or, alternatively, the capsule when the previous does not exist. This shuttle suture is substituted by a high-strength suture and recovered through each tibial tunnel. The 2 limbs are tied to each other on the medial tibial cortex, fixing the capsule to the tibial plateau. This step must always be performed before meniscal graft introduction and fixation. 1:27-1:39: The anterior tunnel is drilled at the anatomic site of meniscal insertion and a shuttle suture is recovered through the anterolateral portal to pass the sutures of the anterior horn of the meniscal allograft. 1:40-1:46: With an outside-in technique, a shuttle suture is placed in the posterolateral corner. 1:47-1:54: Once the capsulodesis has been secured, the posterior-horn suture is used to pull the meniscal allograft in place. The additional vertical stitch helps to accommodate the graft in the right position as it pulls the graft from the posterolateral corner. 1:55-2:03: The allograft is then fixed to the rim by combining an all-inside technique in the posterior horn and meniscal body and an outside-in technique in the anterior horn. 2:04-2:13: Finally, the sutures placed in the anterior and posterior horns are tied together over the tibial cortex.
References
- 1.Milachowski K.A., Weismeier K., Wirth C.J. Homologous meniscus transplantation: Experimental and clinical results. Int Orthop. 1989;13:1–11. doi: 10.1007/BF00266715. [DOI] [PubMed] [Google Scholar]
- 2.Rosso F., Bisicchia S., Bonasia D.E., Amendola A. Meniscal allograft transplantation: A systematic review. Am J Sports Med. 2015;43:998–1007. doi: 10.1177/0363546514536021. [DOI] [PubMed] [Google Scholar]
- 3.Samitier G., Alentorn-Geli E., Taylor D.C. Meniscal allograft transplantation. Part 1: Systematic review of graft biology, graft shrinkage, graft extrusion, graft sizing, and graft fixation. Knee Surg Sports Traumatol Arthrosc. 2015;23:310–322. doi: 10.1007/s00167-014-3334-5. [DOI] [PubMed] [Google Scholar]
- 4.Verdonk P., Depaepe Y., Desmyter S. Normal and transplanted lateral knee menisci: Evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc. 2004;12:411–419. doi: 10.1007/s00167-004-0500-1. [DOI] [PubMed] [Google Scholar]
- 5.Lee D.H., Kim T.H., Lee S.H., Kim C.W., Kim J.M., Bin S. Evaluation of meniscus allograft transplantation with serial magnetic resonance imaging during the first postoperative year: Focus on graft extrusion. Arthroscopy. 2008;24:1115–1121. doi: 10.1016/j.arthro.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–687. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 7.Paletta G.A., Manning T., Snell E., Parker R., Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. Am J Sports Med. 1997;25:692. doi: 10.1177/036354659702500519. [DOI] [PubMed] [Google Scholar]
- 8.Alhalki M.M., Howell S.M., Hull M.L. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27:320–328. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 9.Hunt S., Kaplan K., Ishak C., Kummer F.J., Meislin R. Bone plug versus suture fixation of the posterior horn in medial meniscal allograft transplantation: A biomechanical study. Bull NYU Hosp Jt Dis. 2008;66:22–26. [PubMed] [Google Scholar]
- 10.Alentorn-Geli E., Seijas R., García M. Arthroscopic meniscal allograft transplantation without bone plugs. Knee Surg Sports Traumatol Arthrosc. 2011;19:174–182. doi: 10.1007/s00167-010-1123-3. [DOI] [PubMed] [Google Scholar]
- 11.González-Lucena G., Gelber P.E., Pelfort X., Tey M., Monllau J.C. Meniscal allograft transplantation without bone blocks: A 5- to 8-year follow-up of 33 patients. Arthroscopy. 2010;26:1633–1640. doi: 10.1016/j.arthro.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Verdonk P.C., Demurie A., Almqvist K.F., Veys E.M., Verbruggen G., Verdonk R. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87:715–724. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 13.Abat F., Gelber P.E., Erquicia J.I., Tey M., Gonzalez-Lucena G., Monllau J.C. Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1516–1522. doi: 10.1007/s00167-012-2032-4. [DOI] [PubMed] [Google Scholar]
- 14.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Gonzalez-Lucena G., Monllau J.C. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40:1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 15.Jang S.H., Kim J.G., Ha J.G., Shim J.C. Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy. 2011;27:914–922. doi: 10.1016/j.arthro.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Lee D.H., Kim J.M., Lee B.S., Kim K.A., Bin S.I. Greater axial trough obliquity increases the risk of graft extrusion in lateral meniscus allograft transplantation. Am J Sports Med. 2012;40:1597–1605. doi: 10.1177/0363546512447932. [DOI] [PubMed] [Google Scholar]
- 17.Jeon B., Kim J.M., Kim J.M., Lee C.R., Kim K.A., Bin S.I. An osteophyte in the tibial plateau is a risk factor for allograft extrusion after meniscus allograft transplantation. Am J Sports Med. 2015;43:1215–1221. doi: 10.1177/0363546515570462. [DOI] [PubMed] [Google Scholar]
- 18.Matava M.J. Meniscal allograft transplantation: A systematic review. Clin Orthop Relat Res. 2007;455:142–157. doi: 10.1097/BLO.0b013e318030c24e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
0:00-0:04: Lateral capsular fixation: A reliable implant-free technique to prevent meniscal allograft extrusion. 0:04-0:11: The surgical technique was completely arthroscopic. Routine anterolateral and anteromedial portals were used. 0:12-0:21: This arthroscopic lateral capsulodesis for meniscal allograft transplantation is performed in cases where a redundant capsule is observed or where extrusion of the midbody of the meniscus has been identified with magnetic resonance imaging before meniscal transplantation. 0:22-0:29: Two 5-mm bone tunnels were drilled at the anatomic sites of meniscal attachment, one at the anterior horn and the other at the posterior horn. 0:30-0:45: Once the place where the lateral capsule is most displaced from the edge of the lateral tibial plateau is identified, stabilization is performed using a minimum of two 2.5-mm tunnels. The tunnels were drilled from the contralateral side of the tibia with the help of a regular tibial anterior cruciate ligament guide with a distance of 1 cm between those. Care should be taken to avoid tunnel collision. 0:46-1:05: Using a suture passer, each tunnel is identified, leaving a small loop inside the joint to retrieve the capsulodesis suture strand. 1:06-1:26: Then, 2 spinal needles loaded with a No. 2 polydioxanone suture are used to capture the peripheral rim of the meniscus with an outside-in technique or, alternatively, the capsule when the previous does not exist. This shuttle suture is substituted by a high-strength suture and recovered through each tibial tunnel. The 2 limbs are tied to each other on the medial tibial cortex, fixing the capsule to the tibial plateau. This step must always be performed before meniscal graft introduction and fixation. 1:27-1:39: The anterior tunnel is drilled at the anatomic site of meniscal insertion and a shuttle suture is recovered through the anterolateral portal to pass the sutures of the anterior horn of the meniscal allograft. 1:40-1:46: With an outside-in technique, a shuttle suture is placed in the posterolateral corner. 1:47-1:54: Once the capsulodesis has been secured, the posterior-horn suture is used to pull the meniscal allograft in place. The additional vertical stitch helps to accommodate the graft in the right position as it pulls the graft from the posterolateral corner. 1:55-2:03: The allograft is then fixed to the rim by combining an all-inside technique in the posterior horn and meniscal body and an outside-in technique in the anterior horn. 2:04-2:13: Finally, the sutures placed in the anterior and posterior horns are tied together over the tibial cortex.