Abstract
Isolated posterolateral corner injury is an uncommon injury that could be a source of unexplained knee pain and dysfunction. Most of these patients present instability caused by concomitant ligament injuries. Numerous studies have shown open approach posterolateral repair or reconstruction surgeries to restore posterolateral rotational stability. Still, there is a certain population of patients who present posterolateral rotation instability without significant injury to the fibular collateral ligament, popliteal fibular ligament, and popliteus tendon. The posterolateral capsular ligament is critical to provide posterolateral rotation stability. In this Technical Note, with video, we show a completely arthroscopic approach to stabilize the posterolateral corner, by stabilizing the posterior lateral joint capsule with the lateral meniscus attached to the rim of the lateral tibial plateau.
Injury to the lateral and posterolateral region of the knee requires particular attention because the sequelae can generate considerable morbidity.1 The posterolateral corner (PLC) injury induces posterolateral rotatory instability (PLRI) of the knee, which is a pathological instability resulting from posterolateral tibial subluxation when an external rotational force is applied to the knee.2
PLC injury is an increasingly recognized entity, commonly associated with concomitant ligament injuries including posterior cruciate ligament (PCL) injury and/or anterior cruciate ligament (ACL) injury. Indeed, when injured, the PLC is one of the most complex areas to both accurately diagnose and surgically treat.3 Missed PLC injuries associated with ACL and PCL can account for clinical failures after ACL and PCL reconstruction surgeries.4, 5 Since the past decade, the anatomy and biomechanics of the PLC lesion has been better defined, which makes it possible to detail the different lesions more precisely. Untreated PLC injury results in functional instability such as posterior subluxation and lateral rotation of the lateral tibial plateau due to the failure of one of or several structures of the PLC.6
A number of various surgical techniques for treating PLRI have been described, showing the complexities involved in reconstruction of the PLC structure.1 However, the clinical results after these published PLC surgeries vary greatly. There is no gold standard approach to the treatment of PLRI. Recent anatomical studies showed that there are different kinds of PLC structures, including the popliteofibular ligament (PFL), arcuate ligament complex, and capsular ligament. The posterolateral capsular ligament has an important role in stabilizing posterolateral rotation.7
This Technical Note describes an arthroscopic technique to stabilize the PLC, by stabilizing the posterior lateral joint capsule with lateral meniscus attached to the rim of the lateral tibial plateau in patients with PLRI without significant injury to the fibular collateral ligament (FCL), PFL, and populates tendon.
Surgical Technique
Centralization and stabilization of the posterior lateral joint capsule is performed on a patient with isolated PLRI of the knee. The most commonly used diagnostic methods for PLC injuries are comprehensive physical examinations, including the dial test, the reverse pivot-shift test, the external rotational recurvatum test, and the posterolateral drawer test.8 Physical examination is performed with the patient under anesthesia, before performing surgery, which confirms that there are no main PLC failures, including the popliteus tendon, FCL, and PFL by the magnetic resonance imaging study (Fig 1, Video 1).
Fig 1.
(A) Proton density weighted image. Sagittal view of the right knee. The arrow shows the posterior cruciate ligament. (B) Proton density weighted image. Sagittal view of the right knee. The arrow shows a high-intensity area at the meniscocapsular junction. (C) Proton density weighted image of the right knee. Coronal view of the knee. The arrow shows a high-intensity area at the meniscocapsular junction.
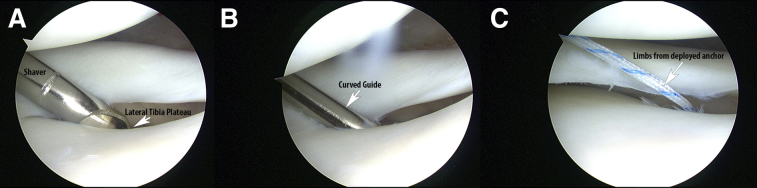
A standard arthroscopic examination is performed through the anteromedial and anterolateral portals (Video 1). Other injuries, including osteochondral lesions and meniscus tears, are managed according to the status of the injury. The drive-through sign, on the lateral compartment, is used to assess the possibility of PLC injury9 by measuring the displacement of the lateral meniscus using a probe (Fig 2A). A midlateral portal is then created through the anterolateral view at the rim of the tibia plateau, posterior to the lateral collateral ligament and 1 cm anterior to the popliteal hiatus (Fig 2B). Then a shaver is introduced under direct visualization through the midlateral portal. The rim is abraded at the lateral tibial plateau by a motorized shaver to remove the cartilage and prepared for anchor placement. A JuggerKnot Soft Anchor (Biomet, Warsaw, IN), loaded with a MaxBraid suture (Zimmer-Biomet), is introduced through the midlateral portal and is placed on the lateral edge of the lateral tibial plateau, just posterior to the popliteal hiatus using the curved drill guide (Fig 3). Next, a 45° left or right ACCU-PASS suture shuttle (Smith & Nephew, Andover, MA) is inserted through the midlateral portal. The tip of the ACCU-PASS suture shuttle penetrates the posterolateral joint capsule from superior to inferior performing the tightening of the capsule. Next, a wire loop is advanced sufficiently into the knee joint. A suture grasper is then inserted through the anterolateral portal, and the wire loop and 1 strand of MaxBraid are retrieved through the anterolateral portal. The retrieved MaxBraid suture is passed into the wire loop, and then retrieved and pulled from the midlateral portal allowing us to pass the MaxBraid suture from inferior to superior. The same procedure is repeated for other strands of the MaxBraid suture (Fig 4).
Fig 2.
Right knee, visualization from the anterolateral portal. (A) Note the drive-through sign in the lateral femoral compartment. (B) The midlateral portal is created under direct visualization.
Fig 3.
Right knee, visualization from the anteromedial portal. (A) Shaver introduced through the midlateral portal and used to prepare a footprint for the anchor, (B) curved drill guide, and (C) soft anchor deployed.
Fig 4.
Right knee, visualization from the anteromedial portal. (A) The ACCU-PASS already penetrated the posterolateral capsule and (B) the wire loop released in the joint.
Then a SUTUREFIX ULTRA (Smith & Nephew), loaded with 2 ULTRABRAIDs (Smith & Nephew), is inserted in the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus through the midlateral portal. A 45° upbend ACCU-PASS suture shuttle (Smith & Nephew) is inserted through the midlateral portal. The same penetration and retrieval procedure is repeated as described above. Finally, the MaxBraid suture and the ULTRABRAIDs are tied in a mattress fashion through the midlateral portal (Fig 5).
Fig 5.
Right knee, visualization from the anteromedial portal. (A) Sutures from the first anchor were retrieved from the midlateral portal. The second anchor was drilled and sutures are evident in the joint. (B) Using an ACCU-PASS the sutures from the second anchor were retrieved through the midlateral portal and (C) knot tied in a mattress fashion.
After surgery, it should be confirmed that there is no PLRI by physical examination (Video 1). The patient undergoes a routine postoperative protocol. Range of motion exercise without restriction is initiated immediately after surgery. Non–weight-bearing exercise with crutches is continued for 2 weeks. After 4 weeks, full weight-bearing exercise is permitted as tolerated. Deep squatting is allowed at 3 months after surgery.
Discussion
This Technical Note presents the success of an arthroscopic technique to stabilize the posterolateral capsule with the lateral meniscus to treat a PLC entity in isolated PLRI. This minimally invasive approach can be used to stabilize the posterior lateral joint capsule combined with the lateral meniscus attached onto the rim of the lateral tibial plateau to restore the posterolateral rotational stability in patients without definitive tear PLC entities, such as the popliteus tendon, FCL, and PFL.
Several surgical treatments for PLC, such as reefing, shortening, and reconstruction, have been reported.1 Recently, Stannard et al.10 reported a prospective Level II study comparing treatment in a series of 64 patients. The results were poor, with 15 failures requiring secondary ligament reconstruction, ultimately with relatively less satisfactory objective results. There has been an increasing awareness of the importance of PLRI reconstruction surgery.1 However, conventional reconstruction surgeries are invasive and need an autologous graft. Feng et al.11 have shown arthroscopic reconstruction for treating PLRI. It is meticulous, invasive, and appears likely to be widely spread.
There are several studies looking at the anatomical and biomechanical importance of the posterolateral capsule in all PLC entities. Lerat et al.12 described tightening of posterolateral structures by transposing the head of the fibula and tightening of the posterolateral capsule. However, this type of ligament tightening cannot prevent rotational subluxation of the tibia in the extension of the knee because the isometry differs from that of the original anatomical structure. The popliteus tendon and the PFL are the primary restraints to external rotation.13 The popliteus tendon has a strong attachment to the lateral meniscus at the posterior knee joint capsule.14 In addition to its attachment on the femur and tibia, the popliteus contains popliteomeniscal fascicles that extend to the lateral meniscus, as well as attachments to the posterior capsule.15 These reports suggest that stabilizing the posterior capsule on the tibia by the proposed procedure is a more anatomically correct repair that would improve PLRI. The suggested procedure induces stabilization of the PLC by stabilizing the lateral meniscus through centralization and stabilization of the posterolateral joint capsule.
In PLRI, there is an abnormal popliteomeniscal motion distinguished by the displacement of the lateral meniscus.16 Simonian et al.17, 18 first showed that the PFL plays an important role in lateral meniscus stability. They observed a significant increase in lateral meniscus mobility after arthroscopic sectioning of the PFL. In the popliteal hiatus, the popliteal tendon is joined to the lateral meniscus by 3 bands.19 Considered together, the proposed procedure seems to induce stabilization of the PFL, which is quite important in the control of PLRI by posterolateral capsular stabilization to the rim of the lateral tibia. The stabilization of the posterolateral joint capsule using a similar procedure to lateral meniscus centralization seems to be a useful technique for PLRI injuries.
Our technique has several pearls and pitfalls as well as advantages and some disadvantages (Tables 1 and 2). The advantages of this arthroscopic technique include small incisions, such as a midlateral portal that is away from the common peroneal nerve. There appears to be a short recovery time, which is especially beneficial for athletes who must quickly recover to the preinjury activity level. The disadvantage of this arthroscopic technique is that the PLC is not anatomically reconstructed and that the lateral meniscus is limited in normal motion.
Table 1.
Tips/Pearls and Pitfalls
| Tips and pearls: |
| Confirm PLRI without PCL, popliteus tendon, fibular collateral ligament, and popliteofibular ligament injuries by special tests, such as the dial test, the reverse pivot-shift test, the external rotational recurvatum test, and posterolateral drawer test, as well as magnetic resonance imaging study |
| During surgery, confirm PLRI by the drive-through sign with a probe |
| Make a midlateral portal with an arthroscopic view from the anterolateral portal 1 cm anterior to the popliteal hiatus |
| The first suture anchor should be inserted on the lateral edge of the lateral tibial plateau, posterior to the popliteal hiatus. The second anchor is inserted anterior to the popliteal hiatus |
| Use an ACCU-PASS suture shuttle to penetrate the posterior lateral joint capsule from superior to inferior to create a mattress suture configuration |
| Pitfalls: |
| Caution is needed for PLRI with obvious PLC injury and complex injury |
| Confirm the orientation of the knee to avoid the departure of the anchors |
PCL, posterior cruciate ligament; PLC, posterolateral corner; PLRI, posterolateral rotator instability.
Table 2.
Advantages and Disadvantages
| Advantages: |
| Minimally invasive |
| Reduced possibility of nerve injury, such as at the peroneal nerve |
| Quicker recovery |
| Especially beneficial treatment for the athletes |
| Disadvantages: |
| Posterolateral corner is not anatomically reconstructed |
| Lateral meniscus is limited in normal motion |
There are also some pitfalls in our technique. This technique is not suitable for PLRI with obvious PLC injury and complex injury because there is a possibility that the instability cannot be entirely controlled. The orientation of the knee must be confirmed to avoid the departure of the anchors to the posterior of the tibia (Table 1). Indications and contraindications are described in Table 3.
Table 3.
Indications and Contraindications
| Indications | Contraindications |
|---|---|
| Patient with PLRI with no associated FCL, PFL, and populate tendon tear | Patients with PLRI caused by severe damage of the FCL, PFL, and populate tendon |
| Patients with associated with lower extremity compartment | |
| Infection |
FCL, fibular collateral ligament; PFL, popliteofibular ligament; PLRI, posterolateral rotational instability.
The proposed procedure is routinely used in our practice, and it continues to show promise. Long-term clinical outcomes from a larger number of case series will be required, but we believe that this approach will prove to be especially beneficial in high-demand athletes with PLRI.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Y.O., C.P-G., and H.K. receive support from Biomet. S.U. receives support from BioMed, Depuy Synthesis, Smith & Nephew, BioMet, Stryker, and Dai-Ichi Sankyo.
Supplementary Data
Centralization and stabilization of the posterior lateral joint capsule is performed in a patient with isolated posterolateral rotatory instability of the right knee. Visualization is performed through the anterolateral portal. First, a lateral midlateral portal is performed under direct visualization. Then a shaver is introduced through the midlateral portal and used to create a footprint at the rim of the lateral plateau. A JuggerKnot Soft Anchor (Biomet, Warsaw, IN) loaded with a MaxBraid suture is deployed at the prepared footprint. Then, using an ACCU-PASS introduced through the midlateral portal and performing the tightening of the capsule, the wire loop is pushed to the joint. A suture grasper is then inserted through the anterolateral portal, and the wire loop and 1 strand of MaxBraid (corresponding to the first soft anchor) are retrieved through the anterolateral portal. The retrieved MaxBraid suture is passed into the wire loop, and then retrieved and pulled from the midlateral portal allowing us to pass the MaxBraid suture from inferior to superior. The same procedure is repeated for other strands of the MaxBraid suture. Then a second anchor, SUTUREFIX ULTRA (Smith & Nephew, Andover, MA), loaded with 2 ULTRABRAIDs (Smith & Nephew), is inserted in the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus through the midlateral portal. Then, a 45° upbend ACCU-PASS suture shuttle (Smith & Nephew) is inserted through the midlateral portal. The same penetration and retrieval procedure is repeated as described above. Finally, the MaxBraid suture and the ULTRABRAIDs are tied in a mattress fashion through the midlateral portal.
References
- 1.Djian P. Posterolateral knee reconstruction. Orthop Traumatol Surg Res. 2015;101:S159–S170. doi: 10.1016/j.otsr.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 2.Albright J.P., Brown A.W. Management of chronic posterolateral rotatory instability of the knee: Surgical technique for the posterolateral corner sling procedure. Instr Course Lect. 1998;47:369–378. [PubMed] [Google Scholar]
- 3.Covey D.C. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83:106–118. doi: 10.2106/00004623-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 5.Wentorf F.A., LaPrade R.F., Lewis J.L., Resig S. The influence of the integrity of posterolateral structures on tibiofemoral orientation when an anterior cruciate ligament graft is tensioned. Am J Sports Med. 2002;30:796–799. doi: 10.1177/03635465020300060701. [DOI] [PubMed] [Google Scholar]
- 6.Raheem O., Philpott J., Ryan W., O'Brien M. Anatomical variations in the anatomy of the posterolateral corner of the knee. Knee Surg Sports Traumatol Arthrosc. 2007;15:895–900. doi: 10.1007/s00167-007-0301-4. [DOI] [PubMed] [Google Scholar]
- 7.Terry G.C., LaPrade R.F. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996;24:732–739. doi: 10.1177/036354659602400606. [DOI] [PubMed] [Google Scholar]
- 8.Lee S.H., Jung Y.B., Jung H.J., Song K.S., Ko Y.B. Combined reconstruction for posterolateral rotatory instability with anterior cruciate ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:1219–1225. doi: 10.1007/s00167-010-1078-4. [DOI] [PubMed] [Google Scholar]
- 9.LaPrade R.F. Arthroscopic evaluation of the lateral compartment of knees with grade 3 posterolateral knee complex injuries. Am J Sports Med. 1997;25:596–602. doi: 10.1177/036354659702500502. [DOI] [PubMed] [Google Scholar]
- 10.Stannard J.P., Stannard J.T., Cook J.L. Repair or reconstruction in acute posterolateral instability of the knee: Decision making and surgical technique introduction. J Knee Surg. 2015;28:450–454. doi: 10.1055/s-0035-1563403. [DOI] [PubMed] [Google Scholar]
- 11.Feng H., Hong L., Geng X.S., Zhang H., Wang X.S., Zhang J. Posterolateral sling reconstruction of the popliteus tendon: An all-arthroscopic technique. Arthroscopy. 2009;25:800–805. doi: 10.1016/j.arthro.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Lerat J.L., Dejour H., Trillat A. [Treatment problems in old and recent rupture of the lateral knee ligament] Rev Chir Orthop Reparatrice Appar Mot. 1978;64:231–241. [in French] [PubMed] [Google Scholar]
- 13.Pasque C., Noyes F.R., Gibbons M., Levy M., Grood E. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br. 2003;85:292–298. doi: 10.1302/0301-620x.85b2.12857. [DOI] [PubMed] [Google Scholar]
- 14.Diamantopoulos A., Tokis A., Tzurbakis M., Patsopoulos I., Georgoulis A. The posterolateral corner of the knee: Evaluation under microsurgical dissection. Arthroscopy. 2005;21:826–833. doi: 10.1016/j.arthro.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 16.Staubli H.U., Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: Gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy. 1990;6:209–220. doi: 10.1016/0749-8063(90)90077-q. [DOI] [PubMed] [Google Scholar]
- 17.Simonian P.T., Sussmann P.S., van Trommel M., Wickiewicz T.L., Warren R.F. Popliteomeniscal fasciculi and lateral meniscal stability. Am J Sports Med. 1997;25:849–853. doi: 10.1177/036354659702500620. [DOI] [PubMed] [Google Scholar]
- 18.Simonian P.T., Sussmann P.S., Wickiewicz T.L. Popliteomeniscal fasciculi and the unstable lateral meniscus: Clinical correlation and magnetic resonance diagnosis. Arthroscopy. 1997;13:590–596. doi: 10.1016/s0749-8063(97)90185-7. [DOI] [PubMed] [Google Scholar]
- 19.LaPrade R.F., Muench C., Wentorf F., Lewis J.L. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30:233–238. doi: 10.1177/03635465020300021501. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Centralization and stabilization of the posterior lateral joint capsule is performed in a patient with isolated posterolateral rotatory instability of the right knee. Visualization is performed through the anterolateral portal. First, a lateral midlateral portal is performed under direct visualization. Then a shaver is introduced through the midlateral portal and used to create a footprint at the rim of the lateral plateau. A JuggerKnot Soft Anchor (Biomet, Warsaw, IN) loaded with a MaxBraid suture is deployed at the prepared footprint. Then, using an ACCU-PASS introduced through the midlateral portal and performing the tightening of the capsule, the wire loop is pushed to the joint. A suture grasper is then inserted through the anterolateral portal, and the wire loop and 1 strand of MaxBraid (corresponding to the first soft anchor) are retrieved through the anterolateral portal. The retrieved MaxBraid suture is passed into the wire loop, and then retrieved and pulled from the midlateral portal allowing us to pass the MaxBraid suture from inferior to superior. The same procedure is repeated for other strands of the MaxBraid suture. Then a second anchor, SUTUREFIX ULTRA (Smith & Nephew, Andover, MA), loaded with 2 ULTRABRAIDs (Smith & Nephew), is inserted in the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus through the midlateral portal. Then, a 45° upbend ACCU-PASS suture shuttle (Smith & Nephew) is inserted through the midlateral portal. The same penetration and retrieval procedure is repeated as described above. Finally, the MaxBraid suture and the ULTRABRAIDs are tied in a mattress fashion through the midlateral portal.