Abstract
Strengthening current surveillance systems for syphilis is important to track and monitor disease burden. We used routinely collected laboratory information to generate surveillance estimates for syphilis trends among women of reproductive age (12–49 years) in the Northern Cape Province, a high syphilis burden region (2003 [8.6%] to 2011 [3.8%]) in South Africa. We extracted records meeting inclusion criteria from the National Health Laboratory Service electronic database for the period 2003–2012. A total of 286,024 women were included in the analysis. Syphilis seropositivity decreased between 2003 (5.7%) and 2012 (1.8%); p trend = 0.001, which was largely consistent with findings reported in the annual national syphilis and HIV survey from 2003 (8.6%) to 2011 (3.8%). Annually for the period from 2003 to 2012 there was an approximate 14% reduction in the prevalence ratio of syphilis seroprevalence (PR = 0.86, 95% CI = 0.85–0.87, p <0.001). Three of five districts had significant decreases in syphilis seropositivity over this period. There were also declines in prevalence ratios for syphilis seropositivity for the various age groups for the period. This study shows that the national laboratory database in South Africa can be used as a complimentary surveillance tool to describe and understand trends in syphilis seroprevalence in South Africa.
Keywords: Congenital syphilis, antenatal clinics, prevalence, surveillance, laboratory, sexually transmitted infection
Introduction
Syphilis is a sexually transmitted infection (STI) and continues to be a major preventable global public health problem, with an estimated 12 million people infected each year.1 Syphilis continues to affect large numbers of pregnant women, causing substantial perinatal morbidity and mortality that could be prevented by early testing and treatment. Screening pregnant women for syphilis during routine antenatal care and then treating any detected infections with penicillin injections has been feasible for many years, even in low-resource settings.1 However, because coverage of testing and treatment of syphilis remains low in many countries, mother-to-child transmission (MTCT) of syphilis, commonly referred to as ‘congenital syphilis’ (CS) is still a global public health problem.2 National guidelines in South Africa have recommended universal syphilis testing for ANC attendees since 2002.3 In South Africa, three doses of benzathine penicillin 2.4 MU at weekly intervals are recommended for treating syphilis in pregnancy. However, limited information is available on compliance with the recommended regimen, in terms of starting treatment, number of doses, and timing of treatment. Pregnant women who are allergic to penicillin may be given alternative therapy with a two-week course of erythromycin.4 A study in two provinces (Northern Cape and Gauteng) in South Africa found that although 71% of pregnant women were tested for syphilis at first ANC visit, only 74% of women who tested positive for syphilis had treatment documented, and only 36% of seropositive women with documented treatment received the recommended three doses of intramuscular penicillin.5
In 2008, approximately 1.4 million pregnant women worldwide were estimated to have probable active syphilis infection and were at risk of transmitting the disease perinatally to their unborn children; of those, 80% had attended ANC.2 Worldwide, 520,000 adverse outcomes were estimated to be caused by maternal syphilis in 2008, including 215,000 stillbirths (>28 wk) or early foetal deaths (22 to 28 wk), 90,000 neonatal deaths, 65,000 preterm or low birth weight infants, and 150,000 infants with congenital disease. About 66% of these adverse effects occurred in ANC attendees who were not tested or were not treated for syphilis. Finally, in 2008, clinical services averted an estimated 26% of all adverse outcomes.2 In developing countries, approximately 3–15% of women of child-bearing age have syphilis, and about 30% of pregnant women with syphilis will have stillbirth, and another 30% will have a live baby with CS, a condition with mortality of up to 50%.6 CS results in deaths of more than one million babies a year worldwide.6
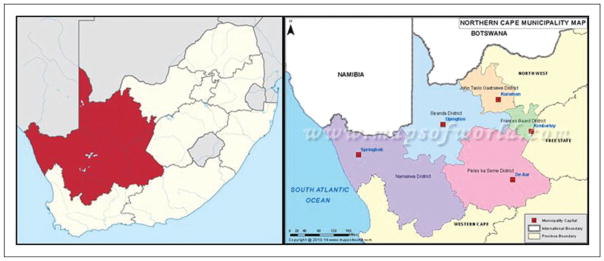
In 2007, the World Health Organization (WHO) launched its initiative for the Global Elimination of Congenital Syphilis, with the goal that at least 90% of pregnant women be tested for syphilis and at least 90% of seropositive pregnant women receive adequate treatment by 2015.1,7 In line with this global aim to eliminate CS as a public health problem, it is important to strengthen existing surveillance systems for syphilis in order to track and monitor disease burden. In South Africa, unlinked anonymous surveys in sentinel antenatal clinics have been conducted annually since 1990 to monitor syphilis seroprevalence among pregnant women. It is important to explore a complementary approach to understanding the syphilis burden in South Africa by utilizing routinely collected electronic laboratory data for surveillance, which provides efficient access to data, and has large-scale coverage. The Northern Cape Province is a region with high syphilis burden compared with other provinces in South Africa,8 see Figure 1. We set to determine whether the national electronic laboratory data repository also known as the Corporate Data Warehouse (CDW) can be employed as appropriate complimentary surveillance data source to track and monitor trends in syphilis seroprevalence in South Africa. Specifically, this paper describes trends in syphilis seroprevalence in women of reproductive age in Northern Cape Province, South Africa, between 2003 and 2012, using laboratory data routinely collected through South Africa’s National Health Laboratory Service (NHLS) CDW and compares the computed trends with findings from the National Antenatal Sentinel HIV & Syphilis Prevalence Surveys during the same period.
Figure 1.
Map of South Africa and the Northern Cape Province showing all the districts along with province boundary. (Source: www.mapsofworld.com)
Methods
Study design and setting
We analysed secondary data of longitudinally collected laboratory measurements from the CDW. The Northern Cape Province is a large and sparsely populated region in the west of South Africa, with an estimated population of 1.1 million.9 It is a high-burden syphilis region. It is administratively divided into five District Municipalities: Frances Baard, John Taolo Gaetsewe, Namakwa, Pixley Ka Seme, and Siyanda. Data from the public sector health facilities of the Northern Cape Province, where syphilis serology tests are conducted, were utilized in this study.
Study population
As the study objective was to explore if the analysis of electronic laboratory data from the CDW could estimate the trends from the National Antenatal Sentinel HIV & Syphilis Prevalence survey conducted annually in South Africa, we selected from the database females of reproductive age (12–49 years) identified from the Northern Cape Province. Other criteria for inclusion in the study were having tested for syphilis by serology between 2003 and 2012 (positive Rapid Plasma Reagin [RPR] confirmed by Treponema pallidum hemagglutination assay [TPHA]). The reasons for testing the women whose tests results ended up in the CDW were: (1) routine antenatal screening (the majority of syphilis tests are done routinely during ANC visits) and (2) when indicated for sexual assault, suspected secondary syphilis, suspected tertiary syphilis, and 6-month follow-up of early syphilis cases treated with doxycycline.10
Data sources and variables
The NHLS has a national network of 265 laboratories. Results of all tests performed in NHLS laboratories in the public sector health facilities in South Africa are sent to a central repository, the CDW, which contains archived test data from the countrywide laboratory information system. Each laboratory test data is captured onto an in-house laboratory information system which electronically feeds centrally to the CDW and are available for analysis in real time. The quality of the data in the CDW depends on accurate completion of the laboratory requisition form and data capturing.11 Whilst some tests may not be reported, this is not very common. Data for this study were obtained from the CDW between 2003 and 2012. Variables captured onto this electronic database include patient-identifying information, demographic information, name of health facility where test was performed, tests requested, date of test, and test result.
Laboratory testing
The syphilis serologic tests performed include the non-treponemal test (RPR) and treponemal test (TPHA). Blood specimens are collected by each public health facility (clinic) and sent to the nearest NHLS laboratory for testing. Women do not have to travel to access laboratories, there is easy clinic access. Though RPR measures disease activity, it is not specific for syphilis. The RPR test can distinguish between an active infection and a past infection.10 False RPR-positive reactions may occur, notably in patients with connective tissue disorders (false positive reactions are usually low titre <1:8). It is government/National Department of Health policy that the standard algorithm (RPR/TPHA) is used in every test. A non-treponemal test, RPR, is used for screening. If non-reactive then the result is deemed negative for syphilis; however, if positive, TPHA is done and if reactive – result is positive for syphilis.10,12
Statistical methods
As a unique identifier is not available in the CDW, identification fields were used together and a probabilistic record linkage technique was applied. In probabilistic record linkage, personal identifiers (e.g. name, sex, date of birth, area of residence) are used together in order to determine how likely a pair of records refers to the same individual. We extracted a total of 8,471,425 syphilis tests, covering the entire country, for the period 2003–2012. We limited analysis to the Northern Cape Province, which had a total of 310,730 tests meeting the inclusion criteria. The rationale of limiting the data to the Northern Cape region is that in South Africa while overall the prevalence of syphilis seropositivity among antenatal clinics attendees has decreased over the past 10–15 years, the Northern Cape Province has consistently showed a higher syphilis prevalence for each year from 2003 to 2011 than any other province, except for Western Cape Province in 2007 (5.6%) and Mpumalanga Province in 2011 (4.1%).8 So this region is currently the priority region in terms of strengthening syphilis surveillance in South Africa. This dataset was then de-duplicated resulting in a final number of 286,024. These were de-duplicated in order to have one single syphilis test record per person, i.e. the same testing episode may have been captured more than once on the database or a person may have had more than one syphilis testing episode within a year. If a person had more than one syphilis diagnostic testing episode during the year e.g. tested in January and then tested in August of the same year, the last record was retained in order to have one person record within a single year.
We used frequencies, proportions, and the Chi square test for trend to examine the changes in syphilis seroprevalence from 2003 to 2012. We applied the modified-Poisson regression approach (with robust error variance) to estimate prevalence ratios (PR) and 95% CIs of syphilis seroprevalence over time. Syphilis seroprevalence was the dependent variable and calendar year was the main independent variable controlling for age and geographical location. Separate analyses by age group and geographical location were also performed. We used the simple linear regression analysis of differences in annual prevalences over time to test for the significance of the difference in trend between the NHLS data and the antenatal survey data. We found no significant differences between the slopes of CDW and ANSUR prevalences (slope = −0.013, 95% CI: −0.277 to 0.250, p = 0.982). All analyses were conducted in STATA version 13 (Stata Corp., College Station, TX, US).
Ethical clearance
Permission to analyse the laboratory data was obtained from the NHLS. Ethical clearance to conduct the study was obtained from the Faculty of Health Sciences Research Ethics Committee of the University of Pretoria. We ensured that the dataset was secured and kept confidential by separating patient-identifying details from the laboratory data and storing the master list that links patient-identifying details to study patient identifiers in a separate, secured location. The dataset was password-protected and was only accessible to the three supervisors and the investigator.
Results
A total number of 286,024 women were included in the study after applying the inclusion criteria and de-duplication. Table 1 shows the characteristics of the study population per year from 2003 to 2012. The mean (standard deviation [SD]) age ranged from 25.7 (6.9) years in 2003 to 27.9 (8.1) years in 2012. The majority of women were in the 26–49 years age group (45.4% in 2003 to 55.4% in 2012).
Table 1.
Characteristics of females of reproductive age tested for syphilis in the Northern Cape Province, South Africa, 2003–2012.
| Characteristic | Year
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2003 (N = 14 514) | 2004 (N = 23 935) | 2005 (N = 25 726) | 2006 (N = 31 006) | 2007 (N = 31 449) | 2008 (N = 34 639) | 2009 (N = 34 937) | 2010 (N = 34 851) | 2011 (N = 35 175) | 2012 (N = 19 792) | |
| Age group (years), n (%) | ||||||||||
| 12–17 | 1 312 (9.0) | 2 386 (10.0) | 2 522 (9.8) | 2 742 (8.8) | 2 693 (8.6) | 2 937 (8.5) | 2 879 (8.3) | 2 800 (8.0) | 2 921 (8.3) | 1 455 (7.4) |
| 18–25 | 6 624 (45.7) | 10 841 (45.3) | 11 328 (44.0) | 12 777 (41.2) | 12 380 (39.3) | 13 559 (39.1) | 13 261 (38.0) | 13 097 (37.6) | 13 143 (37.4) | 7 363 (37.2) |
| 26–49 | 6 578 (45.3) | 10 708 (44.7) | 11 876 (46.2) | 15 487 (50.0) | 16 376 (52.1) | 18 143 (52.4) | 18 779 (53.7) | 18 954 (54.4) | 19 111 (54.3) | 10 974 (55.4) |
| Age, mean (SD) | 25.7 (6.9) | 25.6 (7.0) | 25.9 (7.2) | 26.7 (7.6) | 27.1 (7.3) | 27.2 (7.9) | 27.5 (8.0) | 27.6 (8.1) | 27.5 (8.0) | 27.9 (8.1) |
| District, n (%) | ||||||||||
| Frances Baard | 5 248 (36.2) | 8 433 (35.2) | 8 997 (35.0) | 11 623 (37.5) | 11 601 (36.9) | 12 875 (37.2) | 12 267 (35.1) | 11 716 (33.6) | 12 689 (36.1) | 11 565 (58.4) |
| John Taolo Gaetsewe | 1 591 (11.0) | 4 390 (18.3) | 5 521 (21.5) | 6 249 (20.1) | 6 784 (21.6) | 7 927 (22.9) | 7 908 (22.6) | 8 315 (23.9) | 7 832 (22.3) | 3 115 (15.7) |
| Namakwa | 1 354 (9.3) | 1 998 (8.4) | 2 127 (8.2) | 2 271 (7.3) | 2 172 (6.9) | 2 187 (6.3) | 2 134 (6.1) | 2 210 (6.3) | 2 254 (6.4) | 1 078 (5.5) |
| Pixley Ka Seme | 2 859 (19.7) | 4 117 (17.2) | 4 086 (15.9) | 5 130 (16.6) | 5 145 (16.3) | 5 715 (16.5) | 6 342 (18.2) | 6 241 (17.9) | 5 952 (16.9) | 1 427 (7.2) |
| Siyanda | 3 462 (23.8) | 4 997 (20.9) | 4 995 (19.4) | 5 733 (18.5) | 5 747 (18.3) | 5 935 (17.1) | 6 286 (18.0) | 6 369 (18.3) | 6 448 (18.3) | 2 607 (13.2) |
There was an overall decline in syphilis seroprevalence between 2003 (5.7%) and 2012 (1.8%); p trend: 0.001. This decline was consistent with findings published from the National Antenatal Sentinel HIV & Syphilis Prevalence Surveys from 2003 (8.6%) to 2011 (3.8%),8 as shown in Table 2. Annually for the period from 2003 to 2012 there was an approximate 14% reduction in the prevalence ratio of syphilis seroprevalence (PR = 0.86, 95% CI = 0.85–0.87, p <0.001).
Table 2.
Comparing syphilis seroprevalence for Northern Cape Province, South Africa, using Corporate Data Warehouse data (2003–2012) and National Antenatal Sentinel HIV & Syphilis Prevalence Surveys (2003–2011).
| Syphilis prevalence (%) | Year
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
| ANSUR | 8.6 | 7.0 | 8.5 | 6.9 | 5.6 | 6.8 | 5.6 | 3.6 | 3.8 | – |
| Study | 5.7 | 6.4 | 5.8 | 5.9 | 4.5 | 4.4 | 3.3 | 2.0 | 2.0 | 1.8 |
Decline in syphilis seroprevalence was also seen across all age groups from 2003 to 2012: 12–17 years (4.2% to 2.2%), 18–25 years (5.7% to 1.8%), and 26–49 years (5.9% to 1.7%), p trend = 0.001. There was heterogeneity in changes of syphilis seroprevalence over time by geographical location/region in the Northern Cape Province. Three out of five districts, Frances Baard (6.9% to 0.9%), John Taolo Gaetsewe (7.4% to 0.7%), and Namakwa district (3.3% to 1.7%) experienced significant decreases in syphilis seroprevalence over the 10-year period. Pixley Ka Seme district had an increase in syphilis seroprevalence from 2003 to 2004 (5.4% to 6.4%); largely similar from 2004 to 2008 (6.4%, 6.1%, 7.0%, 6.3%, 6.5%); experienced a decrease from 2008 to 2011 (6.5% to 4.3%), and another increase from 2011 to 2012 (4.3% to 6.9%). Siyanda district had an increase from 2003 to 2004 (4.2% to 9.0%) and decrease from 2004 to 2012 (9.0% to 4.1%). Table 3 below illustrates the overall syphilis seroprevalence by year, age group, and geographic location (districts). A similar pattern to that of the prevalence was reflected when the prevalence ratios were computed and this decrease was statistically significant across all age groups and geographic location (p trend: <0.001). See Tables 4 and 5.
Table 3.
Syphilis seroprevalence among females of reproductive age tested for syphilis in the Northern Cape Province, South Africa, by age and district using data from the Corporate Data Warehouse: 2003–2012.
| Characteristic | Seroprevalence by Year
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Overall prevalence (%) | 823/14 | 1 | 1 | 1 | 1 | 1 | 1 | 681/34 | 722/35 | 353/19 |
| 514 (5.7) | 534/23 | 501/25 | 841/31 | 416/31 | 536/34 | 138/34 | 851 (2.0) | 175 (2.0) | 792 (1.8) | |
| 935 (6.4) | 726 (5.8) | 006 (5.9) | 449 (4.5) | 639 (4.4) | 937 (3.3) | |||||
| Age group (years) | ||||||||||
| 12–17 | 55/1 | 149/2 | 115/2 | 132/2 | 92/2 | 130/2 | 99/2 | 56/2 | 69/2 | 32/1 |
| 312 (4.2) | 386 (6.2) | 522 (4.6) | 742 (4.8) | 693 (3.4) | 937 (4.4) | 897 (3.4) | 921 (2.0) | 921 (2.4) | 455 (2.2) | |
| 18–25 | 3776 | 699/10 | 625/11 | 747/12 | 525/12 | 526/13 | 453/13 | 294/13 | 27913 | 134/7 |
| 624 (5.7) | 841 (6.5) | 328 (5.5) | 777 (5.9) | 380 (4.2) | 559 (3.9) | 261 (3.4) | 097 (2.2) | 143 (2.1) | 363 (1.8) | |
| 26–49 | 391/6 | 686/10 | 761/11 | 962/15 | 799/16 | 880/18 | 586/18 | 331/18 | 374/19 | 187/10 |
| 578 (5.9) | 708 (6.4) | 876 (6.4) | 487 (6.2) | 376 (4.9) | 143 (4.9) | 779 (3.1) | 954 (1.8) | 111 (2.0) | 974 (1.7) | |
| District | ||||||||||
| Frances Baard | 362/5 | 547/8 | 578/8 | 611/11 | 554/11 | 621/12 | 402/12 | 187/11 | 146/12 | 107/11 |
| 248 (6.9) | 433 (6.5) | 997 (6.4) | 623 (5.3) | 601 (4.8) | 875 (4.8) | 267 (3.3) | 716 (1.6) | 689 (1.2) | 565 (0.9) | |
| John Taolo Gaetsewe | 117/1 | 205/4 | 225/5 | 226/6 | 166/6 | 184/7 | 123/7 | 50/8 | 75/7 | 23/3 |
| 591 (7.4) | 390 (4.7) | 521 (4.1) | 249 (3.6) | 784 (2.5) | 927 (2.3) | 908 (1.6) | 315 (0.6) | 832 (1.0) | 115 (0.7) | |
| Namakwa | 44/1 | 70/1 | 61/2 | 82/2 | 58/2 | 40/2 | 36/2 | 44/2 | 28/2 | 18/1 |
| 354 (3.3) | 998 (3.5) | 127 (2.9) | 271 (3.6) | 172 (2.7) | 187 (1.8) | 134 (1.7) | 210 (2.0) | 254 (1.2) | 078 (1.7) | |
| Pixley Ka Seme | 155/2 | 264/4 | 248/4 | 359/5 | 323/5 | 369/5 | 319/6 | 225/6 | 253/5 | 99/1 |
| 859 (5.4) | 117 (6.4) | 086 (6.1) | 130 (7.0) | 145 (6.3) | 715 (6.5) | 342 (5.0) | 241 (3.6) | 952 (4.3) | 427 (6.9) | |
| Siyanda | 145/3 | 448/4 | 389/4 | 563/5 | 315/5 | 322/5 | 258/6 | 175/6 | 220/6 | 106/2 |
| 462 (4.2) | 997 (9.0) | 995 (7.8) | 733 (9.8) | 747 (5.5) | 935 (5.4) | 286 (4.1) | 369 (2.8) | 448 (3.4) | 607 (4.1) | |
Table 4.
Prevalence ratios by age group among females of reproductive age tested for syphilis in the Northern Cape Province, South Africa, using data from the Corporate Data Warehouse, 2003–2012.
| Year | Age group
|
|||||
|---|---|---|---|---|---|---|
| 12–17 years*
|
18–25 years*
|
26–49 years*
|
||||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| 2003 | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| 2004 | 1.49 | 1.10–2.01 | 1.13 | 1.0–1.28 | 1.08 | 0.96–1.22 |
| 2005 | 1.09 | 0.79–1.49 | 0.97 | 0.86–1.10 | 1.08 | 0.96–1.21 |
| 2006 | 1.15 | 0.84–1.56 | 1.03 | 0.91–1.16 | 1.05 | 0.93–1.17 |
| 2007 | 0.81 | 0.59–1.13 | 0.75 | 0.65–0.85 | 0.82 | 0.73–0.92 |
| 2008 | 1.06 | 0.78–1.44 | 0.68 | 0.60–0.78 | 0.82 | 0.73–0.92 |
| 2009 | 0.82 | 0.59–1.13 | 0.60 | 0.53–0.69 | 0.52 | 0.46–0.59 |
| 2010 | 0.48 | 0.33–0.60 | 0.39 | 0.34–0.46 | 0.29 | 0.25–0.34 |
| 2011 | 0.56 | 0.40–0.80 | 0.37 | 0.32–0.43 | 0.33 | 0.29–0.38 |
| 2012 | 0.52 | 0.34–0.81 | 0.32 | 0.26–0.39 | 0.29 | 0.24–0.34 |
p Trend <0.001 across all age-groups.
Table 5.
Change in prevalence ratio of syphilis seroprevalence among females of reproductive age by district in the Northern Cape Province, South Africa, using data from Corporate Data Warehouse, 2003–2012.
| District
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Namakwa*
|
JT Gaetsewe*
|
Frances Baard*
|
Pixley Ka Seme*
|
Siyanda*
|
||||||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| 2003 | 1.00 | reference | 1.00 | reference | 1.00 | Reference | 1.00 | reference | 1.00 | reference |
| 2004 | 1.08 | 0.74–1.56 | 0.63 | 0.51–0.79 | 0.94 | 0.83–1.07 | 1.18 | 0.98–1.43 | 2.14 | 1.78–2.57 |
| 2005 | 0.88 | 0.60–1.29 | 0.55 | 0.45–0.69 | 0.93 | 0.82–1.06 | 1.12 | 0.92–1.36 | 1.86 | 1.54–2.24 |
| 2006 | 1.11 | 0.78–1.59 | 0.49 | 0.40–0.61 | 0.76 | 0.67–0.86 | 1.29 | 1.08–1.55 | 2.34 | 1.95–2.80 |
| 2007 | 0.82 | 0.56–1.21 | 0.33 | 0.26–0.42 | 0.69 | 0.61–0.79 | 1.16 | 0.96–1.39 | 1.31 | 1.08–1.59 |
| 2008 | 0.56 | 0.37–0.86 | 0.32 | 0.25–0.40 | 0.70 | 0.62–0.79 | 1.19 | 0.99–1.43 | 1.30 | 1.07–1.57 |
| 2009 | 0.52 | 0.34–0.80 | 0.21 | 0.17–0.27 | 0.48 | 0.41–0.55 | 0.93 | 0.77–1.12 | 0.98 | 0.80–1.20 |
| 2010 | 0.61 | 0.41–0.93 | 0.08 | 0.06–0.11 | 0.23 | 0.19–0.28 | 0.66 | 0.54–0.81 | 0.66 | 0.53–0.81 |
| 2011 | 0.38 | 0.24–0.61 | 0.13 | 0.10–0.17 | 0.17 | 0.14–0.20 | 0.78 | 0.65–0.95 | 0.81 | 0.66–1.00 |
| 2012 | 0.51 | 0.30–0.88 | 0.10 | 0.06–0.16 | 0.13 | 0.11–0.17 | 1.28 | 1.00–1.63 | 0.97 | 0.76–1.24 |
p Trend <0.001 across all districts.
Discussion
This study explored the utility of routinely collected laboratory information in the Northern Cape Province, South Africa, as a supplemental source of surveillance data to monitor syphilis trends among women of reproductive age. Overall, syphilis seroprevalence showed statistically significant decreases between 2003 and 2012. Our estimates are largely consistent with previously published data from the National Antenatal Sentinel HIV & Syphilis Prevalence Survey from 2003 to 2011.8 Although three of the five districts of the Northern Cape Province had statistically significant decreases in syphilis seroprevalence, there were variations in trend pattern among the other two districts over the 10-year period. The key strength of our study is that it demonstrated that routinely collected electronic laboratory data can accurately portray the trends in the prevalence of syphilis in South Africa. The implications of our study findings are that laboratory-based estimates of the burden of disease at national and provincial levels serve as a useful tool in surveillance. Laboratory data can be a good indicator of trend, while understanding that it may not be as representative of the population. For over two decades, conventional methods of surveillance (ANC prevalence surveys), which have been largely paper-based records, have been used to monitor trends in syphilis seropositivity in South Africa.13
The Northern Cape Province is a region of high syphilis burden compared with other provinces in South Africa, with syphilis seroprevalence for each year from 2003 to 2011 being higher than any other province, except for Western Cape Province in 2007 (5.6%) and Mpumalanga Province in 2011 (4.1%).8 Our data showed that syphilis seroprevalence in the Northern Cape Province has decreased significantly over the study period. Other South African studies have also suggested declines in Syphilis seroprevalence in the Northern Cape Province.5,8,14 As other studies have shown, this decrease may be attributable to a number of factors such as the implementation of syndromic management of STIs in most limited resource settings, improved access to healthcare and widespread use of antibiotics, reduction in risky sexual behaviours in a population, and mortality due to HIV/AIDS.15,16 A South African study suggests that increased condom use, improved treatment of STIs, and mortality due to HIV/AIDS collectively led to significant reduction in syphilis prevalence between 1990 and 2005.17 Improved ANC visits (more women attending ANC for first visit with better services) and increased awareness and health education of women and girls about the consequences of syphilis by healthcare providers during ANC visits are factors that also contribute to the downward trend in the prevalence of syphilis in pregnant women.15,17 The WHO recommends a minimum of four ANC visits, starting in the first 12 weeks of pregnancy.18 ANC is provided free of charge in the South African public health system and nearly all pregnant women and girls attend ANC at least once during their pregnancy (between 90 to 100% of pregnant women attend a health facility at least once for ANC).19
The highest decrease in syphilis seroprevalence for the period among the various age groups was recorded in the 26–49 years (15%), followed by the 18–25 years (13%), and then 12–17 years (10%) age groups. Future trends in syphilis seroprevalence in the overall population may be predicted by trends in the youngest pregnant women, as syphilis infection in the 12–17 years age group (4.2% [2003] to 2.2% [2012]) are likely to be more recent and may best reflect incidence of disease.20 Though Pixley Ka Seme and Siyanda districts showed variations in terms of decreases there was, however, an overall marginal decrease. Pixley Ka Seme district falls in the second socio-economic quintile (out of five quintiles, the first quintile is the most deprived and the fifth quintile is the least deprived), among the poorer districts, whereas Siyanda district falls in the third socioeconomic quintile. John Taolo Gaetsewe, Namakwa, and Frances Baard districts fall in the fourth socioeconomic quintile, among the wealthier districts.21 Findings from studies in Malawi, Tanzania, and Zambia suggest that syphilis seroprevalence rates are highest among people in areas with high crowding and high levels of economic deprivation, as measured by poverty, and that there is positive association with lower syphilis prevalence among higher socio-economic status and education.22 These findings are likely to apply to South Africa.
The findings of this study should be interpreted with caution in light of several limitations. First, all the tests from the National Antenatal Sentinel HIV & Syphilis Prevalence Survey end up in the CDW (there is partially a comparison of the same tests). However, numbers from the survey represent <5% of the total female population that had syphilis tests, i.e. for 2011. For 2011, the antenatal survey had a sample size of 1128 for the Northern Cape Province and the CDW had a sample size of 35,175 for the Northern Cape Province, representing 3.2% (1 128/35 175). Second, this is a secondary dataset analysis and the CDW dataset is limited by the variables that are stored and quality of the data, which depend on accurate completion of the laboratory requisition form and data capturing. Since record linkage techniques were used, only records with complete information and therefore better chance of linkage are included in the study, leading to potential selection bias. Also, the linkage may not have been good enough in truly identifying unique people, thus resulting in multiple records for the same individual going unmatched or mismatched records that reduce the number of real individuals. Third, since the de-duplication approach retains the last testing episode done in order to achieve a single record per person within that year, this could underestimate the actual syphilis prevalence. Where follow-up testing of early syphilis was not confirmed with TPHA, there will be an initial true positive result with a negative follow-up test, thus resulting in a negative result being retained. Fourth, we only used one of the nine provinces of South Africa to compare with available data, which makes our sample not representative and findings not generalizable to South Africa as a whole. Finally, participants of the study included only women who attended public health facilities, leaving out those who attended private health facilities and those who do not access health services, also leading to potential overestimation of the syphilis burden. Our study aim was to compare the estimates from the electronic laboratory data with those of the National Antenatal Sentinel HIV & Syphilis Prevalence Survey. Though the objective of determining the utility of the electronic laboratory data may have been achieved, we may have overestimated the burden of syphilis in Northern Cape Province.
Conclusions
There was significant decline in syphilis seroprevalence in the Northern Cape Province, which was largely consistent with findings from the National Antenatal Sentinel HIV & Syphilis Prevalence Surveys. We have shown that a national electronic laboratory database with high coverage can be used to assess trends in syphilis seropositivity in South Africa. This highlights that completeness and quality of routine electronic laboratory data should be strengthened in order to enhance the quality of this simple, inexpensive disease surveillance approach.
Acknowledgments
We gratefully recognize the invaluable role played by the hardworking staff of the Centre for HIV and Sexually Transmitted Infections (STI section) of the National Institute for Communicable Diseases (NICD), particularly the guidance and expertise of Prof. David A. Lewis (Former Head) in conceiving this project. We also sincerely appreciate the enormous contributions of the South African Field Epidemiology Training Programme (SA FETP), particularly Drs Carl Reddy and Patience Kweza. We also thank Ms Dorothy Southern of the US Centers for Disease Control and Prevention, South Africa, for editing the manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Diseases Control and Prevention under the terms of 5U2GPS001328-05.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Diseases Control and Prevention, the National Institute for Communicable Diseases, National Health Laboratory Service, the University of the Witwatersrand and the University of Pretoria.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.The global elimination of congenital syphilis: rationale and strategy for action. Geneva: World Health Organization; 2007. [accessed 25 June 2015]. http://www.who.int/reproductivehealth/publications/rtis/9789241595858/index.htmi. [Google Scholar]
- 2.Newman L, Kamb M, Hawkes S, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. Plos Med. 2013;10:e1001396. doi: 10.1371/journal.pmed.1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health Guidelines for Maternity Care in South Africa. [accessed 10 November 2015];A Manual for Clinics, Community Health Centres and District Hospitals. (2). 2002 http://healthweb.kznhealth.gov.za/maternityguidelines.pdf.
- 4.Mullick S, Beksinksa M, Msomi S. [accessed 20 September 2013];Treatment for syphilis in antenatal care: compliance with the three dose standard regimen. doi: 10.1136/sti.2004.011999. http://www.sti.bmjjournals.com. [DOI] [PMC free article] [PubMed]
- 5.Dinh TH, Lewis D, Trege L, et al. Prevalence of and adherence to HIV prophylaxis and syphilis treatment regimenin pregnant women receiving antenatal care services in public facilities in Northern Cape and Gauteng Provinces, South Africa, 2004–2006. [Poster Presentation]. HIV/AIDS Implementers’ Meeting; 3–7 June 2008; Kampala, Uganda. [Google Scholar]
- 6.The use of rapid syphilis tests. The sexually transmitted diseases diagnostic Initiative/World Health Organization, 2006.
- 7.Kamb ML, Newman Lori M, Riley PL, et al. A road map for global elimination of congenital syphilis. Obstet Gynecol Int. 2010;2010:312798. doi: 10.1155/2010/312798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Department of Health SA. The 2011 National Antenatal Sentinel HIV and Syphilis Prevalence Survey in South Africa. National Department of Health; South Africa: 2012. [Google Scholar]
- 9.Census 2011: Census in brief. Statistics South Africa; Pretoria: 2012. [Google Scholar]
- 10.Sexually Transmitted Infections Management Guidelines. Adapted from: Standard Treatment Guidelines and Essential Drug List PHC. National Department of Health; South Africa: 2015. [Google Scholar]
- 11.Sherman GG, Lilian R, Bhardwa S, et al. Laboratory information system data demonstrate successful implementation of the mother-to-child transmission programme in South Africa. South African Med J. 2014;104:235–238. doi: 10.7196/samj.7598. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Sexually transmitted infection disease surveillance, 2012. Atlanta, GA: US Department of Human Services; 2014. [Google Scholar]
- 13.Goga AE, Dinh T, Jackson DJ for the SAPMTCTE study group. Evaluation of the Effectiveness of the National Prevention of Mother-To-Child Transmission (PMTCT) Programme Measured at Six Weeks Postpartum in South Africa, 2010. South African Medical Research Council, National Department of Health of South Africa and PEPFAR/US Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 14.Dihn TH, Kamb M, Msimang V, et al. Integration of preventing mother-to-child transmission of HIV and syphilis testing and treatment in antenatal catre services in the Northern Cape and Gauteng Provinces, South Africa. Sex Transmitted Dis. 2013;40:846–851. doi: 10.1097/OLQ.0000000000000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Creek TL, Thuku H, Kolou B, et al. Declining syphilis prevalence in pregnant women in northern Botswana: an encouraging sign for HIV prevention? Sex Transm Infect. 2005;81:453–455. doi: 10.1136/sti.2004.014068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Temmerman M, Fonck K, Bashir F, et al. Declining syphilis prevalence in pregnant women in Nairobi since 1995: another sucess story in the STD field? Int J STD AIDS. 1999;10:405–408. [PubMed] [Google Scholar]
- 17.Johnson LF, Dorrington R, Bradshaw D, et al. The effect of syndromic management interventions on the prevalence of sexually transmitted infections in South Africa. Sex Reprod Health. 2011;2:13–20. doi: 10.1016/j.srhc.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Abou-Zahr CH, Wardlaw TM. Analysis of trends, levels and differentials, 1990–2001. Geneva: World Health Organization; 2003. Antenatal care in developing countries: promises, achievements and missed opportunities. [Google Scholar]
- 19.National Department of Health, Medical Research Council. South African Demographic and Health Survey 2003. Pretoria: 2007. [Google Scholar]
- 20.Podgor M, Leske C. Estimating incidence from age-specific prevalence for irreversible disease with differential mortality. Stats Med. 1986;5:573–758. doi: 10.1002/sim.4780050604. [DOI] [PubMed] [Google Scholar]
- 21.Massyn N, Day C, Peer N, et al. District Health Barometer 2013/14. Durban: Health Systems Trust; 2014. [Google Scholar]
- 22.Potter D, Goldenberg R, Read JS, et al. Correlates of syphilis seropositivity among pregnant women: The HIVNET 024 Trial in Malawi, Tanzania and Zambia. Sex Transm Dis. 2006;33:604–609. doi: 10.1097/01.olq.0000216029.00424.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]