Abstract
Multiple ligament knee injuries are complex pathologies that often result from traumatic knee dislocations. Both a high level of suspicion and a thorough clinical and radiographic examination are mandatory to diagnose and identify all injured structures. Reconstruction of all injured ligaments is recommended to aid in early mobilization and to avoid joint stiffness or graft failure. For knee dislocations involving injury to the anterior cruciate ligament, posterior cruciate ligament, and medial-sided structures, a repair and augmentation of the medial collateral ligament, together with an anatomic reconstruction of the anterior cruciate ligament and double-bundle posterior cruciate ligament, is recommended. In the setting of these complex reconstructions, there are several technical aspects that require consideration to ensure concise and efficient treatment of these injuries. Graft choice, sequence of reconstruction, tunnel position and orientation, and graft tensioning all pose surgical challenges, and require dedicated preoperative preparation and planning. The purpose of this Technical Note is to report a safe, effective, and reproducible surgical technique for treatment of multiligament injuries in the setting of a knee dislocation with a medial-sided component (classified as KD-III-M in the Schenck classification system).
Multiligament knee injuries represent complex conditions that often occur as a result of traumatic knee dislocations. During these injury events 3 or more ligaments are often disrupted, including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and either the posteromedial corner or the posterolateral corner (PLC). A knee dislocation classification described by Schenck1 (Table 1) is commonly used, and may aid surgeons in diagnosis and decision making in treatment of these injuries.
Table 1.
Schenck Knee Dislocation Classification System
| Schenck Knee Dislocation (KD) Classification | Description |
|---|---|
| KD-I | Injury to a single ligament (ACL or PCL) |
| KD-II | Injury to both ACL and PCL |
| KD-III | Injury to ACL and PCL with additional medial (M) or lateral (L) injury: MCL (KD-III-M) or FCL (KD-III-L) |
| KD-IV | Injury to both cruciate and collateral ligaments (ACL, PCL, MCL, FCL) |
| KD-V | Knee fracture-dislocation |
ACL, anterior cruciate ligament; FCL, fibular colateral ligament; KD, knee dislocation; MCL, medial colateral ligament; PCL, posterior cruciate ligament.
Controversy exists within the literature regarding the optimal treatment of these complex injuries; however, reconstruction as opposed to repair of the cruciate ligaments is more widely accepted.2, 3 Furthermore, higher failure rates and inferior patient outcomes have been reported for repair of the collateral ligaments when compared with reconstruction.4, 5, 6 Thus, reconstruction of both the cruciate and collateral ligaments is recommended. To minimize the risk of postoperative stiffness and graft failure, it is also recommended that all injured structures be reconstructed concurrently and anatomically so that an early postoperative knee range of motion can be initiated.7, 8, 9, 10, 11, 12, 13, 14 Because of the complexity of these injuries, a thorough preoperative evaluation, detailed plan of surgery, a precise rehabilitation protocol, and a team that is familiar with this type of surgery are mandatory. Thorough knowledge of the anatomical attachment of the ligaments is required to perform anatomical reconstructions and optimize the tourniquet time, due to the number of concurrent procedures in a single surgery. The surgeon also must be familiar with the correct position for an atomic reduction of the knee, to avoid the fixation of the grafts in a suboptimal position, which can lead to failure of the reconstruction and inferior outcomes.
The purpose of this Technical Note is to explain, in detail, the technique for surgical treatment of KD-III-M injuries to the knee with anatomic reconstruction of the ACL using a bone–patellar tendon–bone allograft, double-bundle PCL reconstruction with Achilles and tibialis anterior allografts, and augmentation of the superficial medial collateral ligament (sMCL) with semitendinosus and gracilis autografts.
Evaluation
Indications
Acute Multiple Ligament Injuries
For high-energy injuries, advanced trauma life support principles apply. When an acute knee dislocation is diagnosed, pedal pulses and skin color should be monitored and compared with the uninjured side. Neurologic status should be assessed and recorded. Patients with an ankle-brachial index of <0.9 warrant angiography.2, 15 Although surgical management of all injured structures is recommended in the acute phase (<2-3 weeks),16, 17, 18 surgery of the ligaments can be delayed in patients with vascular and/or skin injuries.
Using a combination of stress radiographs and magnetic resonance imaging is recommended to objectively evaluate the extent of the injury and associated lesions. When both cruciate ligaments are torn, reconstruction should be planned if the patient is a surgical candidate and the injury should be approached as a knee dislocation in the acute phase with aims for early surgery and rehabilitation. Associated medial- or lateral-sided injuries may also require surgical treatment during the same surgical setting.16 Grade III PLC injuries should be reconstructed, because repair has been reported to yield less than optimal results.4, 19, 20 For grade III medial-sided injuries, surgical intervention with reconstruction or repair/augmentation is also warranted for the stability of the knee and early rehabilitation.
Chronic Injuries
Some patients may present in a chronic phase because of a missed diagnosis in the acute phase, or associated injuries that prevented definitive treatment in the acute phase. A comprehensive patient history, clinical examination supplemented with stress radiography, and magnetic resonance imaging evaluation should be performed. In addition to assessing ligamentous structures, these evaluations also assist in identification of concomitantly injured structures, including the articular cartilage or meniscus. Long leg standing coronal radiographs of the lower extremity should be obtained to assess alignment, and malalignment should be addressed with an osteotomy before ligament reconstruction for chronic injuries, because malalignment can lead to later graft failure.21
Surgical Technique
Patient Positioning and Anesthesia
When performing multiligament reconstructions, detailed planning, preparation of the operative suite, and surgical setup are crucial. After the induction of general anesthesia, the patient is placed in the supine position on the operating table (Video 1). A thorough physical examination is performed on both knees to confirm the knee instability on the symptomatic side. The following tests are used: varus/valgus stress test at full extension and 20° to 30° of knee flexion, anterior and posterior drawer at 90° of knee flexion, pivot shift, reverse pivot shift, external rotation recurvatum test, Lachman and posterior Lachman test at 30° of knee flexion, external rotation at 30° and 90° of knee flexion, and range of motion. A well-padded high-thigh tourniquet is subsequently placed around the proximal part of the operative leg and the leg is placed in a leg holder (Mizuho OSI, Union City, CA). The contralateral limb is placed in a well-padded abduction stirrup (BirkovaProduct LLC, Gothenburg, NE).
Graft Preparation
To perform this multiligament reconstruction technique, both autograft and allograft tissues are used. To perform the PCL double-bundle reconstruction, an 11-mm Achilles tendon allograft is used for reconstructing the anterolateral bundle (ALB), and a 7-mm anterior tibialis tendon allograft used for the posteromedial bundle (PMB) reconstruction. For the ACL reconstruction, a bone–patellar tendon–bone allograft or autograft is used. Medial augmentation of the sMCL is performed using the autogenous semitendinosus and gracilis tendons, which remain attached at their tibial insertion on the ipsilateral side of the injury.
Surgical Approach and Preparation for sMCL Augmentation
An open surgical approach is performed before arthroscopy to allow for improved soft tissue visualization and to limit fluid extravasation into the surgical site. The procedure begins with a focus on the medial structures. The adductor tubercle (AT), the medial aspect of the patella, and medial joint line are palpated. A skin incision is performed proximally between the AT and the patella, and extended 8 cm distally from the joint line to the medial part of the tibia (Fig 1). Blunt dissection is performed over the sartorius fascia and the injured structures are evaluated. The semitendinosus and gracilis tendons are isolated and an open-ended hamstring tendon stripper (Smith & Nephew, Andover, MA) is used to detach the tendons proximally. Care is taken to preserve their tibial insertion.
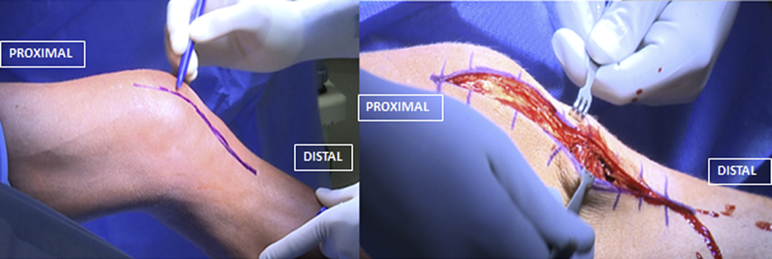
Fig 1.
Multiligament reconstruction performed in a left knee, with the patient in a supine position and the limb secured in a leg holder (Mizuho OSI). To avoid liquid extravasation due to the arthroscopic part of the procedure, which can jeopardize the correct identification of the medial structures landmarks, this technique starts with the medial collateral ligament (MCL) identification. The skin incision is performed with the knee in approximately 45° of flexion, proximally between the adductor tubercle and the patella, and extended 8 cm distally from the joint line to the medial part of the tibia to perform the MCL augmentation. Blunt dissection is performed over the sartorius fascia and the injured structures are evaluated.
The posteromedial aspect of the tibia is identified at this point and 2 double-loaded suture anchors (Mitek, Westwood, MA) are placed at the tibial insertion of the sMCL, 6 cm distal to the joint line. The first anchor is placed at the posterior insertion and then used as a reference for the second anchor, which is placed slightly anterior and proximal (Fig 2). The semitendinosus and gracilis tendons are now sutured to the tibia, along with the remnant sMCL, to reconstitute the distal sMCL tibial attachment. Once the hamstring grafts are secured distally, attention is directed proximally and the AT is identified using the adductor magnus tendon as a reference. The adductor magnus tendon is considered to be the “lighthouse” on the medial aspect of the knee because it serves as a consistent point of reference for the medial structure femoral attachment sites.
Fig 2.
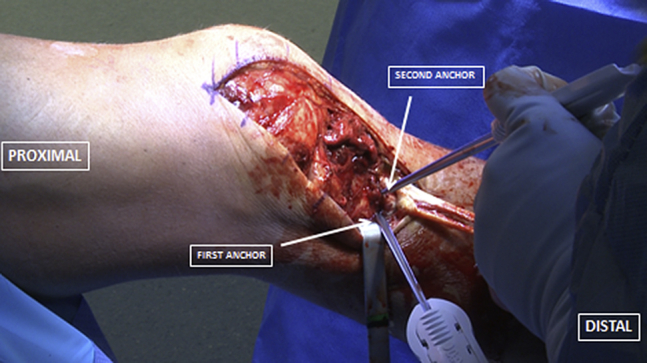
Open reconstruction of the medial collateral ligament in a left knee with multiligament injury. After the exposition of the superficial medial collateral ligament, a ruler is used to identify the point situated 6 cm below the medial femorotibial joint line, which will be used to mark the level of the first anchor. The first double-loaded suture anchor (Mitek) is placed at the posteriomedial part of the tibial shaft and then used as reference for the second anchor, which is placed slightly anterior and proximal. This technique allows the correct position of the graft to recreate the medial collateral ligament anatomy and biomechanics.
The sMCL proximal attachment is 12 mm distal and 8 mm anterior to the AT (Fig 3).22 A sharp dissection is performed on the sMCL proximal attachment to define it and an eyelet pin is placed through its center with an aiming guide (Arthrex, Naples, FL) anteriorly and proximally, avoiding the trochlea and the PCL reconstruction tunnels. A 35-mm deep tunnel is reamed using a 7-mm acorn reamer (Arthrex) (Fig 4). Both tendon grafts are then passed through deep to the sartorial fascia along the native course of the sMCL (Fig 5). A guide pin is placed in the femoral reconstruction tunnel and the graft is then measured from this point such that 30 mm of graft is whipstitched for later passage into the tunnel. The excess graft length is removed. A passing suture is then pulled through the tunnel. The grafts remain unsecured to the femoral side at this juncture to allow for preparation of the remaining reconstructions.
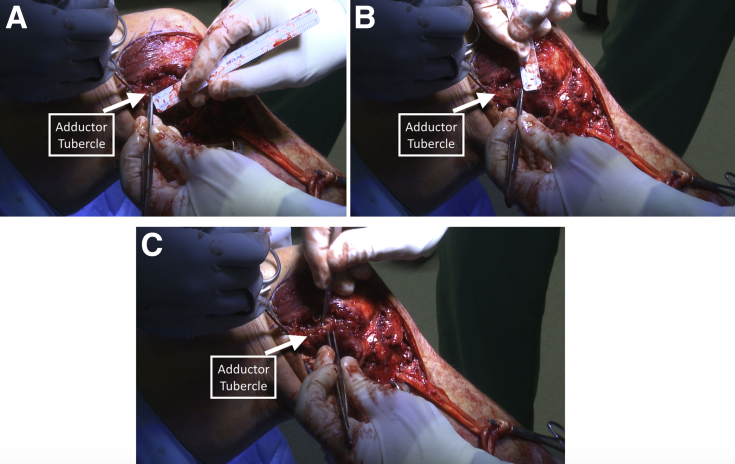
Fig 3.
Superficial medial collateral ligament (sMCL) reconstruction performed in a left knee. To identify the correct position of the proximal attachment of the sMCL, the adductor tubercle (AT) is identified. The adductor magnus tendon can be used as a reference to find the correct position of the AT if necessary. Once identified and with the use of a ruler, the proximal insertion of the sMCL will be located 12 mm distal (A) and 8 mm anterior (B) to the adductor tubercle. Sharp dissection is performed to identify the attachment in a small depression posterior and proximal to the medial epicondyle (C).
Fig 4.
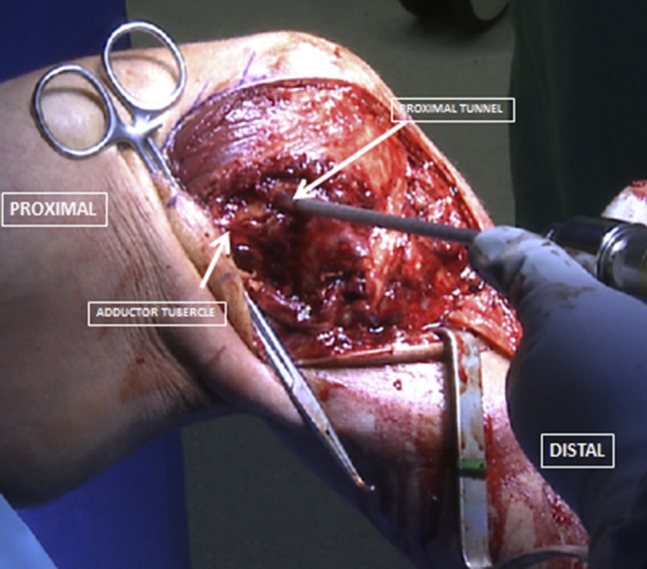
Superficial medial collateral ligament (sMCL) reconstruction performed in a left knee in a setting of a multiligament injury. To perform the correct identification of the proximal attachment of the medial collateral in the femur, anatomic landmarks are used as a reference. The adductor tendon is used to identify the adductor tubercle. Once the adductor tubercle (AT) is found, a ruler is used to identify the point 12 mm distal to the AT. Sharp dissection is performed 8 mm anterior to this point, which will be the proximal sMCL attachment, situated in a small depression posterior and proximal to the medial epicondyle. A 35-mm deep tunnel is reamed using a 7-mm acorn reamer (Arthrex) and care must be taken to avoid damage to the trochlea and the posterior cruciate ligament reconstruction tunnels.
Fig 5.
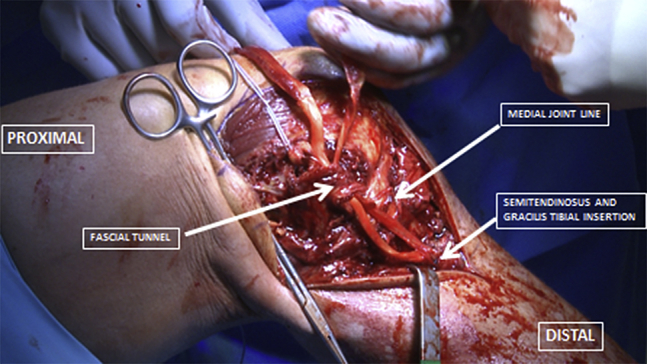
Superficial medial collateral ligament reconstruction in a left knee with the gracilis and semitendinosus tendon grafts. After the distal fixation using 2 double-loaded suture anchors (Mitek), both grafts are passed through a small incision made in line with the sartorial fascia, and the distance between the grafts and the proximal tunnel must be measured to reach 30 mm proximal to the tunnel entrance.
Diagnostic Arthroscopy and Preparation of the ACL and PCL Tunnels
Routine arthroscopy is performed through standard anterolateral and anteromedial portals. All of the compartments are evaluated for associated lesions. With the use of an arthroscopic shaver (Smith & Nephew) and an arthroscopic coagulator (Smith & Nephew) the medial wall of the lateral femoral condyle is prepared for ACL reconstruction tunnel reaming (Fig 6). The femoral footprint of the ACL is evaluated using the lateral intercondylar ridge as a reference, and an accessory medial portal is established first by using a spinal needle with the knee flexed to approximately 80° to 90°. With the knee flexed to 120°, an eyelet guide pin is then inserted in the femoral footprint, midway between the anteromedial and posterolateral bundles, through the accessory medial portal. A 10-mm low-profile reamer (Arthrex) is used to create a 25-mm deep closed socket tunnel with the knee in 120° of flexion while maintaining a 1- to 2-mm back wall. A passing suture is pulled through the femoral ACL tunnel.
Fig 6.
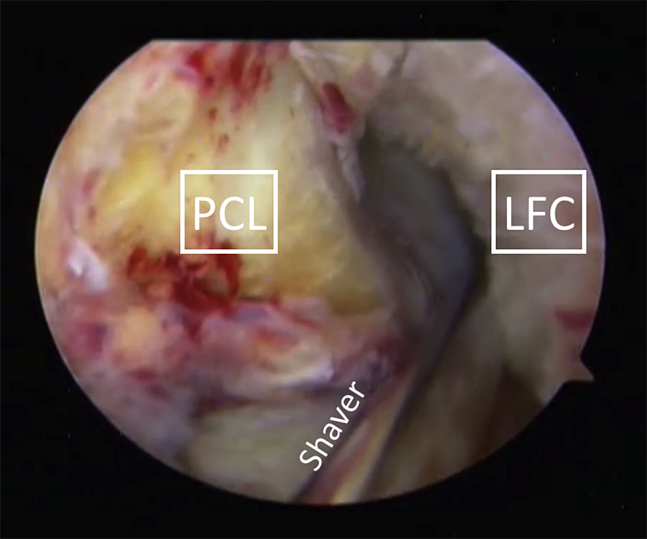
Arthroscopic visualization of a left knee joint in a setting of multiligament injury. A 30° arthroscope is positioned in the anterolateral portal and an arthroscopic shaver (Smith & Nephew) and an arthroscopic coagulator (Smith & Nephew) are positioned in the anteromedial portal. After evaluation of all the compartments of the knee, the anterior cruciate femoral tunnel is prepared first. The intercondylar area is evaluated and the medial wall of the lateral condyle is prepared. The lateral intercondylar ridge is used as a reference to find the correct insertion point of the anterior cruciate ligament femoral tunnel, which will be performed through a medial accessory portal. (LFC, lateral femoral condyle; PCL, posterior cruciate ligament.)
Then attention is then turned to preparing the femoral insertion of the PCL. The femoral attachments of the ALB and PMB are identified, using the trochlear point and the medial arch point, and then outlined with an arthroscopic coagulator (Smith & Nephew). For the ALB, an 11-mm-diameter acorn reamer (Arthrex) is used, which is placed through the anterolateral portal. The reamer is placed abutting the cartilage (Fig 7), at the ALB footprint, and a pin is drilled at the center of the footprint, using the reamer as a guide. A 25-mm deep closed socket tunnel is then reamed, and a passing suture is placed in the tunnel. A 25-mm deep tunnel is reamed to reconstruct the PMB using a 7-mm-diameter acorn reamer (Arthrex), with the center of the tunnel approximately 8 to 9 mm posterior to the edge of the articular cartilage of the medial femoral condyle and placed slightly posterior to the ALB tunnel previously prepared. These 2 tunnels are divergent with a 1- to 2-mm bone bridge at the aperture (Fig 8).23
Fig 7.
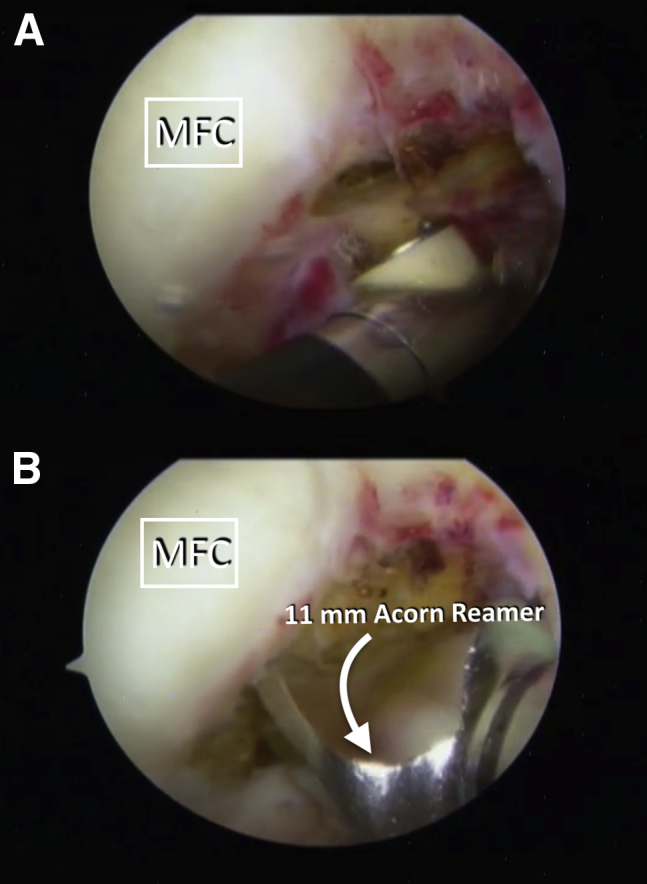
An arthroscopic view of the left knee using a 30° arthroscope through the anterolateral portal. To perform the double-bundle posterior cruciate ligament reconstruction in the femur, the attachment of the anterolateral bundle (ALB) and posteromedial bundle (PMB) is identified. With the use of an arthroscopic coagulator (A) the anterolateral attachment is identified using the trochlear point and medial arch point as a reference. The femoral attachment of the ALB is then removed and an 11-mm-diameter acorn reamer is placed against the cartilage (B). This allows the correct position of the tunnel and avoids damage to the cartilage. A guide pin is inserted through the acorn reamer and a 25-mm deep closed socket is performed. The first tunnel will be the reference to perform the PMB reconstruction. (MFC, medial femoral condyle.)
Fig 8.
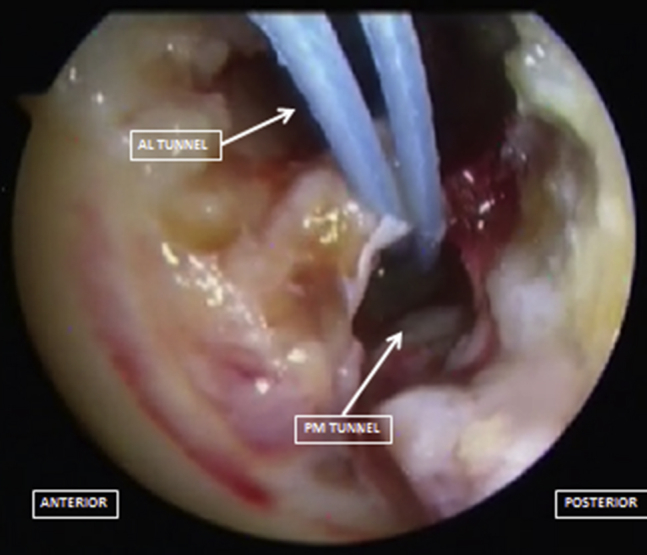
To correctly perform the double-bundle technique for the reconstruction of the posterior cruciate ligament, an 11-mm-diameter acorn reamer is placed against the cartilage and after that a 25-mm deep socket tunnel is performed to recreate the anterolateral bundle. The first tunnel will be used as a reference for the reconstruction of the posteromedial bundle tunnel, which will be performed using a 7-mm acorn reamer, placed approximately 8 to 9 mm posterior to the edge of the articular cartilage of the medial femoral condyle and slightly posterior to the anterolateral bundle. These 2 tunnels are divergent with a 1- to 2-mm bone bridge at the aperture. (AL, anterolateral; PM, posteromedial.)
To access the tibial attachment of the PCL, a posteromedial portal and a 70° arthroscope (Smith & Nephew) may be required. The tibial PCL footprint is identified. The shiny white fibers of the posterior root attachment of the medial meniscus are used as a reference for the proximal debridement and the lateral articular cartilage is used as a lateral reference. The distal debridement is performed until the popliteus muscle fibers are visualized and the champagne-glass drop-off of the posterior tibia is identified. After the debridement, the tibial PCL guide (Arthrex) is placed 5.5 mm proximal to the champagne-glass drop-off of the posterior tibia to place the PCL tibial tunnel guide pin. The entry point of the PCL guide pin is placed 6 cm distal to the joint line on the anteromedial aspect of the tibia. Fluoroscopy is used to verify that the tibial pin is placed in the desired anatomic location (Fig 9). If there is a meniscal tear present, it is repaired at this time.
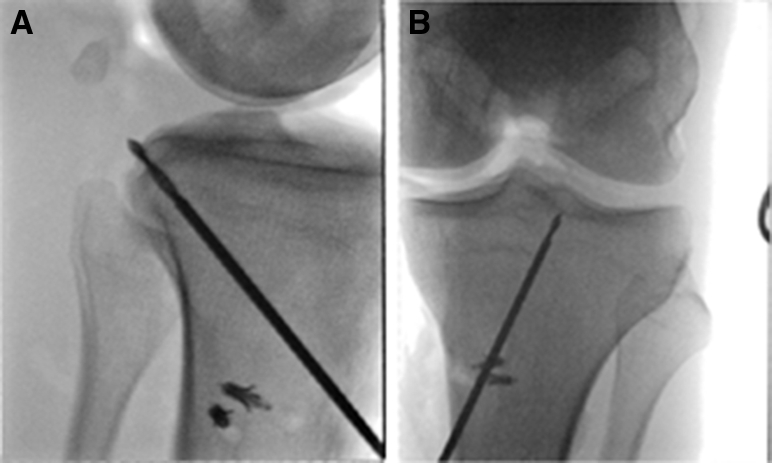
Fig 9.
Transoperative fluoroscopic lateral (A) and anteroposterior (B) views of a left knee in a setting of multiligament injury, showing the correct placement of the posterior cruciate ligament tibial guide pin. In the lateral view, the guide pin must be 5.5 mm proximal to the champagne-glass drop-off on the posterior aspect of the tibia. In the anteroposterior view, the correct position of the guide pin must be identified at the medial aspect of the lateral tibial eminence. Care must be taken to avoid pin extrusion and neurovascular damage to the posterior structures of the knee.
With the correct placement, a curette is used to protect against guide pin protrusion and to retract the posterior capsule, while a 12-mm acorn reamer (Arthrex) over-reams the tibial guide pin. A smoother (Gore Smoother Crucial Tool, Smith & Nephew) is used to avoid laceration of the graft by bone spicules at the tibial tunnel aperture, but care must be taken to avoid an iatrogenic medial meniscal root injury. The closed loop tip of the smoother is passed out through the anterolateral arthroscopic portal.
The tibial footprint of ACL is then identified and a tibial ACL guide (Arthrex) is placed in the center of the ACL tibial attachment, adjacent to the anterior root of the lateral meniscus, and a guide pin is passed. A 10-mm acorn reamer (Arthrex) is used to ream the tibial tunnel over the guide pin. To perform the graft passage, the passing sutures are used.
Fixation of the PCL and ACL Grafts
The PMB PCL graft is passed through the anterolateral portal into its femoral tunnel with the aid of a passing suture and fixed with a 7 × 23 mm bioabsorbable interference screw (Arthrex) at the posteroinferior aspect of the femoral tunnel. The ALB PCL graft is then passed into the femoral tunnel, with the cortical side of the bone plug placed into the anterior portion of the tunnel and fixed with a 7 × 20 mm titanium interference screw (Arthrex) at the anterosuperior aspect of the tunnel. Then, the sutures in the end of both grafts are passed through with the loop tip of the smoother and pulled distal down the tibial tunnel and cycled several times, while traction is applied to remove any slack in the grafts. The ACL graft is passed through the tibia into the femoral ACL tunnel and then fixed in the femur with a 7 × 20 mm titanium interference screw (Arthrex).
Once all cruciate grafts are fixed in their femoral tunnels and are shuttled down the anterior tibia, the PCL grafts are secured first. The rationale for this maneuver is to reduce the knee to an anatomic position with normal tibial step-off similar to the contralateral side before restoring rotational and valgus stability. With the knee flexed to 90° and in neutral rotation, the joint line is palped to ensure the correct position and the normal tibiofemoral step-off is verified while applying an anterior reduction force, and the PCL ALB graft is secured to the tibia with a fully threaded bicortical 6.5-mm cannulated cancellous screw (Arthrex) and an 18-mm spiked washer (Arthrex). Then, the knee is placed in full extension and the PCL PMB graft is secured to the tibia with a similar screw and washer that were used for the other bundle, while distal traction applied to the graft (Fig 10). The excess portions of the grafts are removed. Distal traction is then applied to the ACL graft, and the knee is cycled several times. The tibial ACL graft fixation is performed with a 9 × 20 mm titanium interference screw (Arthrex) with the knee in full extension.
Fig 10.
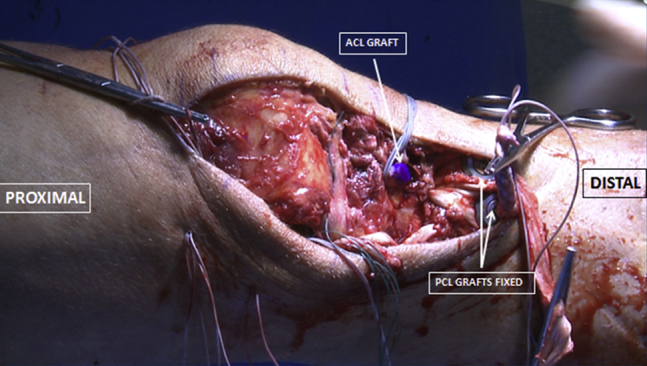
Multiligament reconstruction in a left knee. After drilling the intra-articular tunnels, the anterior cruciate ligament (ACL) graft is the first to be secured in the femur, followed by the posterior cruciate ligament (PCL) grafts. Attention is then turned to the PCL grafts fixation in the tibia, which are secured using screws and a spike washer. The anterolateral bundle graft is fixed to the tibia with the knee flexed to 90° and in neutral rotation while applying the anterior force. Then, the knee is placed in full extension and the posterior medial bundle graft is fixed, while distal traction is applied to the graft.
Fixation of the sMCL Grafts
After fixation of the central ligaments (Fig 11), which restores the normal anatomic position of the tibiofemoral joint, attention is turned back to the medial side of the knee through the prior open incision. The semitendinosus and gracilis grafts are pulled into the femoral tunnel using the previously placed shuttle suture. The knee is positioned at 20° of flexion in neutral rotation, a gentle varus force reduction is applied, and the grafts are fixed with a 7 × 23 mm bioabsorbable screw (Arthrex). A spinal needle is used to define the joint line and the last double-loaded suture anchor (Mitek) is inserted 12 mm distal to the joint line and the sutures are tied to the grafts with the knee positioned at 20° of knee flexion and in neutral rotation to reconstitute the sMCL proximal tibial attachment. The “safe zone” range of motion is determined to guide the postoperative rehabilitation. The skin and subcutaneous tissues are closed and the procedure is complete. The pearls and pitfalls of this procedure are summarized in Table 2.
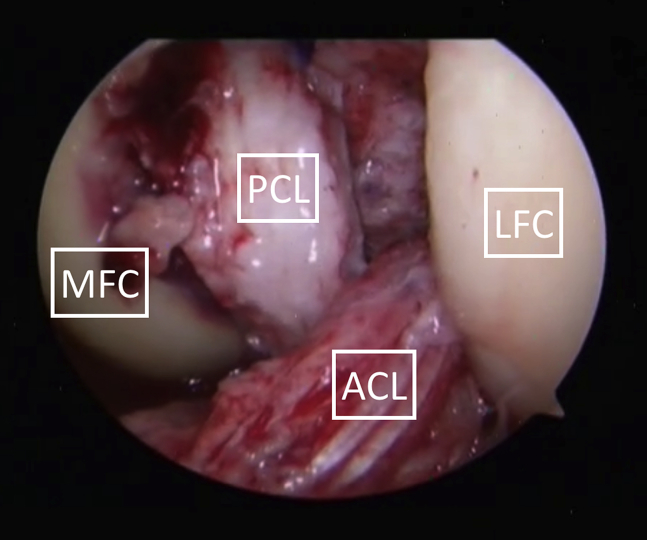
Fig 11.
An arthroscopic view of a left knee using a 30° arthroscope inserted in the anterolateral portal. After the fixation of the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) in the tibia and with the lack of saline solution in the joint, an arthroscopic visualization of the reconstruction is performed. The ACL and the double-bundle PCL reconstruction on the left knee can be visualized, showing the anatomic position of the anterolateral and posteromedial bundle of the PCL as well as the ACL graft. (LFC, lateral femoral condyle; MFC, medial femoral condyle.)
Table 2.
Pearls and Pitfalls of Multiligament Reconstruction
| Pearls | Pitfalls |
|---|---|
| These lesions should be treated in the acute setting whenever possible. | To avoid the increased risk of failure the MCL graft tibial insertion should be posteriorized to better resemble the anatomy of the sMCL. |
| A comprehensive physical examination, stress radiographs, and MRI are key to fully diagnose associated lesions. | Nonanatomic placement of the tunnels can jeopardize the reconstruction; thus only ream the tunnels after verifying that the guide pins are in the correct place. Medial-sided tunnels should be created aiming anteriorly and proximally in the femur. |
| Leaving passing sutures after drilling each tunnel facilitates later graft passage. | Not using a screw protector during screw placement on the femur for cruciate ligament grafts can lead to graft damage. |
| If feasible, address all the pathology during a single surgery. | If the tunnels are not properly cleared of all soft tissue, passage of the grafts can be difficult. |
| In chronic cases, assess the limb alignment so it can be addressed before or concurrent with the reconstruction. | Too long of a graft for the sMCL can result in a lax graft because the graft fills the tunnel prematurely. |
MCL, medial colateral ligament; MRI, magnetic resonance imaging.
Postoperative Rehabilitation
Postoperative recovery after a multiligament reconstruction procedure typically requires 9 to 12 months of rehabilitation before returning to full activities. This allows proper time for the grafts to incorporate and to heal to prevent reconstruction graft failure. Furthermore, a thorough rehabilitation protocol helps allay fatigue and endurance issues that can cause reinjury to the operative knee or the contralateral side.
A well-guided rehabilitation protocol after a multiligament reconstruction should focus on graft protection and functional outcomes including regaining motion, strength, and function. Full range of motion is especially vital to long-term outcomes, and patients should aim to obtain 0° to 90° of knee flexion within the first 2 weeks after surgery. Further range of motion should be achieved between weeks 2 and 6. Further goals of the first 6 weeks include limiting joint effusion and improving patellar mobility.
After week 6, the patients may initiate partial weight bearing. Physical therapy should focus on achieving control on a single leg stance and normalizing gait. This can progress to exercises that include step up/down, squats, and partial lunges. Once the patients have developed good dynamic neuromuscular control without any pain, they can progress to their functional sport-specific exercises.
Discussion
The multiple ligament injured knee remains a complex surgical problem given the increased risk of neurovascular injury, articular cartilage damage, and meniscus tears when compared with single ligament injuries.24, 25, 26 This Technical Note details our preferred surgical approach for multiple ligament reconstruction in the setting of KD-III-M injuries. Table 3 summarizes the advantages and limitations of these anatomic reconstruction techniques. Although these injuries can be devastating to patients and surgeons alike, a systematic and evidence-based approach allows for improved surgical efficiency and improved patient outcomes.
Table 3.
Advantages and Disadvantages of Multiligament Reconstruction
| Advantages | Disadvantages |
|---|---|
| If acute, assess for range and motion and delay surgery with preoperative rehabilitation if flexion is less than 90°. Prompt surgery avoids fibrotic tissues and facilitates visualization. | Limited range of motion before the surgery can result in higher rates of arthrofibrosis and poorer outcomes. |
| This technique allows for an unstaged reconstruction of the structures that will ultimately result in a faster recovery. | A skilled surgeon is advocated to attempt this reconstruction at one setting because it might result in a prolonged operative time otherwise. |
| Anatomic reconstructions facilitate early range of motion without compromising the grafts integrity. | A mix of autografts and allografts are recommended due to the quantity of structures to reconstruct. |
Reconstructive techniques using a combination of autografts and allografts to reconstruct multiligament-deficient knees have shown good to excellent outcomes in prior studies.27 However, the decision for repair or augmentation and/or reconstruction of medial-sided knee injuries has only recently been studied. For grade III injuries, reconstruction has shown improved longer term results,28, 29, 30 and King et al.6 reported that MCL repair in the setting of KD-III-M injuries was inferior to MCL reconstruction. We therefore recommend reconstruction of both the central ligaments and medial-sided injuries when present in the setting of KD-III-M injuries.
Although several nonanatomic-based knee ligament reconstructions are used, anatomical reconstructions are preferred because they restore near native knee biomechanics and have also been validated to improve patient outcomes. When several ligaments are injured, restoration of knee kinematics to near preinjury levels is paramount.19, 31, 32, 33 Tunnel orientation to avoid convergence and tensioning sequence are potential problems; however, there is a paucity of literature on techniques to avert such issues. Gelber et al.34 reported in a cadaveric study that an sMCL tunnel oriented 30° anteriorly and proximally avoided tunnel convergence between the double-bundle PCL and sMCL tunnels. However, in their study, the PCL tunnels were smaller than the ones used in this technique. Camarda et al.35 reported that proximal orientation of the sMCL tunnel avoided convergence with the PCL tunnel in single-bundle PCL reconstruction with concurrent MCL reconstruction.
The PCL is routinely tensioned first to restore tibiofemoral articulation, and the tibial step-off. The normal knee is used as a reference for tibial step-off, and fluoroscopy may be used to aid during the reduction of the tibia. It is important to restore the tibial step-off because not doing so will result in the tibia being fixed posteriorly, thereby overconstraining the knee when the other grafts are tensioned. This error will lead to changes in joint biomechanics and loading, potentially causing graft stretching or failure. When the ACL is tensioned first, the tibia has a tendency to be displaced posteriorly. In a biomechanical study of ACL and PCL reconstruction tensioning by Markolf et al.,36 the PCL had to be tensioned first to consistently restore normal knee laxities and graft forces. The tensioning sequence used in this technique has been previously reported by other authors.2, 27, 29 Wentorf et al.37 reported that the tibia was externally rotated if the ACL was tensioned in PLC-deficient knees. Because of this, both graft tensioning and order of graft fixation play important roles in surgical planning for the dislocated knee.
Despite the challenging nature of these cases, good patient-reported outcomes after multiple ligament knee reconstructions are reported after surgical treatment. Several studies reported mean Tegner scores of 4 to 5 and Lysholm scores of 83 to 84.27, 38, 39, 40, 41, 42 Medium- to long-term prevalence of knee osteoarthritis is reported in the range of 23% to 87%. Most studies however had few patient cohorts, and the patient population was heterogeneous in regard to ligaments involved.27, 38, 39, 40, 41, 42
Knee dislocation is a serious injury with significant potential for associated injury, and as such, a high index of suspicion combined with appropriate physical and radiographic examination is of utmost importance in the diagnosis of these potentially limb-threatening injuries. Early and complete surgical intervention leads to improved outcomes, and should be performed by surgeons familiar with these complex cases. Although we recommend the above technique, future long-term studies with larger samples are necessary to assess the efficacy and patient-reported outcome measures after multiple ligament reconstruction.
Footnotes
The authors report the following potential conflict of interest or source of funding: G.M. receives research grants from Health South East, Norway, and Arthrex. R.F.L. receives support from Smith & Nephew Endoscopy, Ossur Americas, Arthrex, Siemens Medical Solutions, Small Bone Innovations, ConMed Linvatec, and Opedix; he is on the editorial/governing board for AJSM and KSSTA, and has member/committee appointments with AOSSM, ISAKOS, AANA, and ESSKA.
Supplementary Data
After induction of general anesthesia, the patient is placed in the supine position on the operating table. After sterile preparation and draping, the medial knee structures are approached first to identify structures before structure extravasation. A hockey stick incision is performed proximally between the adductor tubercle and the patella. The incision is extended 8 cm distally over the joint line along the anteromedial tibia. A combination of blunt and sharp dissection is used to expose the subcutaneous structures and to identify the hamstring tendons. The semitendinosus and gracilis tendons are harvested proximally for the medial collateral ligament (sMCL) augmentation procedure. Of note, their tibial insertion should remain attached at the pes anserine. A spinal needle is used to identify the joint line and a ruler is then used to measure 6 cm distal to the medial joint line to identify the distal tibial attachment of the sMCL. Two double-loaded suture anchors are placed at the posteromedial aspect of the tibia posteriorizing the attachment of the grafts to recreate the anatomic distal insertion of the sMCL. Attention is then directed proximally. Using the adductor magnus tendon and subsequently the adductor tubercle as a landmark, the sMCL proximal attachment is identified 12 mm distal and 8 mm anterior. Sharp dissection is performed to identify the attachment in a small depression posterior and proximal to the medial epicondyle. An eyelet pin is drilled through the sMCL femoral attachment. A 7-mm reamer is reamed over the guide pin to a depth of 35 mm for the proximal femoral reconstruction tunnel. A passing suture is then placed through the tunnel for the later graft passage. Both tendon grafts are then passed proximally along the native course of the sMCL deep to the sartorial fascia. The graft length is measured and it is whipstitched 30 mm proximal to the femoral tunnel entrance. Afterward, the excess graft length is removed. The sMCL grafts remain unfixed until later in the procedure. Routine arthroscopy is then performed. The femoral attachment site of the anterior cruciate ligament (ACL) on the medial wall of the lateral femoral condyle is prepared. An accessory medial portal is established first by using a spinal needle. A 10-mm low-profile reamer is used to create a 25-mm closed socket tunnel for the ACL reconstruction. Initially, the reamer is advanced 4-5 mm to confirm maintenance of a 1- to 2-mm back wall. After the tunnel is reamed, a passing suture is placed to allow for the later ACL graft passage. Then, attention is then turned to preparing the tunnels for the femoral attachments of the posterior cruciate ligament (PCL). For the anterolateral bundle (ALB), an 11-mm-diameter acorn reamer is placed against the cartilage and a guide pin is inserted through it. Then a 25-mm deep closed socket tunnel is reamed. Next, the posteromedial bundle (PMB) tunnel is prepared using the same technique with a 7-mm-diameter acorn reamer to a depth of 25 mm. These 2 tunnels should diverge and must have at least 1-2 mm of bony bridge at the entrances. Passing sutures are placed in each tunnel to allow for the later PCL graft passage. To prepare the tibial attachment of the PCL, a 70° arthroscope is used and a posteromedial portal can be created if needed. The posterior capsule is carefully resected with the aid of a shaver and a radiofrequency device until the popliteus muscle fibers are observed. The shiny white fibers, lateral articular cartilage, bundle ridge, and the champagne drop-off are used as references to locate the PCL tibial attachment. The guide pin is them drilled using a PCL aiming device located at the bundle ridge. The tibial footprint of ACL is then identified and a tibial ACL guide pin is drilled at this point. A 10-mm acorn reamer is used to antegrade ream the tunnel. The PCL grafts are passed first to allow appropriate reduction of the tibiofemoral joint. The posteromedial bundle PCL graft is passed first into its femoral tunnel and fixed with a 7 × 23 mm bioabsorbable interference screw. The bone plug for the ALB PCL graft is then passed into its femoral reconstruction tunnel and secured with a 7 × 20 mm titanium interference screw. The ACL graft is then passed into the femoral tunnel using the passing suture and fixed in the femur with a 7 × 20 mm titanium interference screw. Once all grafts are shuttled through the anterior tibia, the PCL grafts are secured first. With the knee flexed to 90° of knee flexion, the ALB graft is split in line with its fibers and fixed using a 6.5-mm cancellous screw and a spiked washer. Then, the PMB graft is fixed to the tibia in full extension. Next, the ACL graft tibial fixation is performed with the knee in full extension, traction applied to the graft sutures, and with a 9 × 20 mm titanium interference screw after cycling the grafts several times to remove any slack on the grafts. The cruciate ligament grafts are then arthroscopically visualized to confirm restoration of the tibiofemoral position. The semitendinosus and gracilis grafts are pulled into the femoral tunnel and fixed with a 7 × 25 mm PEEK (polyether ether ketone) interference screw. A double-loaded suture anchor is then inserted 12-15 mm distal to the medial joint line to reconstitute the proximal tibial attachment of the sMCL. The tourniquet is released and the excess portions of the grafts are removed. The “safe zone” range of motion is determined to guide the initial amount of knee motion allowed for postoperative rehabilitation. Hemostasis is performed, the subcutaneous and skin tissues are closed, and the procedure is complete.
References
- 1.Schenck R.C., Jr. The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 2.Levy B.A., Fanelli G.C., Whelan D.B. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197–206. doi: 10.5435/00124635-200904000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Frosch K.H., Preiss A., Heider S. Primary ligament sutures as a treatment option of knee dislocations: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1502–1509. doi: 10.1007/s00167-012-2154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy B.A., Dajani K.A., Morgan J.A., Shah J.P., Dahm D.L., Stuart M.J. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 5.Levy B.A., Dajani K.A., Whelan D.B. Decision making in the multiligament-injured knee: An evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 6.King A.H., Krych A.J., Prince M.R., Pareek A., Stuart M.J., Levy B.A. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy. 2016;32:1814–1819. doi: 10.1016/j.arthro.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 7.House C.V., Connell D.A., Saifuddin A. Posteromedial corner injuries of the knee. Clin Radiol. 2007;62:539–546. doi: 10.1016/j.crad.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 8.Sims W.F., Jacobson K.E. The posteromedial corner of the knee: Medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 9.Robinson J.R., Bull A.M., Thomas R.R., Amis A.A. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med. 2006;34:1815–1823. doi: 10.1177/0363546506289433. [DOI] [PubMed] [Google Scholar]
- 10.Lundquist R.B., Matcuk G.R., Jr., Schein A.J. Posteromedial corner of the knee: The neglected corner. Radiographics. 2015;35:1123–1137. doi: 10.1148/rg.2015140166. [DOI] [PubMed] [Google Scholar]
- 11.Geeslin A.G., LaPrade R.F. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: A prospective case series and surgical technique. J Bone Joint Surg Am. 2011;93:1672–1683. doi: 10.2106/JBJS.J.01639. [DOI] [PubMed] [Google Scholar]
- 12.Harner C.D., Vogrin T.M., Hoher J., Ma C.B., Woo S.L. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med. 2000;28:32–39. doi: 10.1177/03635465000280011801. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade R.F., Muench C., Wentorf F., Lewis J.L. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: A biomechanical study. Am J Sports Med. 2002;30:233–238. doi: 10.1177/03635465020300021501. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 15.Kendall R.W., Taylor D.C., Salvian A.J., O'Brien P.J. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35:875–878. doi: 10.1097/00005373-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 16.McKee L., Ibrahim M.S., Lawrence T., Pengas I.P., Khan W.S. Current concepts in acute knee dislocation: The missed diagnosis? Open Orthop J. 2014;8:162–167. doi: 10.2174/1874325001408010162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fanelli G.C., Fanelli D.G. Knee dislocations and PCL-based multiligament knee injuries in patients aged 18 years and younger: Surgical technique and outcomes. J Knee Surg. 2016;29:269–277. doi: 10.1055/s-0036-1571427. [DOI] [PubMed] [Google Scholar]
- 18.Levy N.M., Krych A.J., Hevesi M. Does age predict outcome after multiligament knee reconstruction for the dislocated knee? 2- to 22-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2015;23:3003–3007. doi: 10.1007/s00167-015-3750-1. [DOI] [PubMed] [Google Scholar]
- 19.Geeslin A.G., Moulton S.G., LaPrade R.F. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: Surgical treatment of acute injuries. Am J Sports Med. 2016;44:1336–1342. doi: 10.1177/0363546515592828. [DOI] [PubMed] [Google Scholar]
- 20.Stannard J.P., Brown S.L., Farris R.C., McGwin G., Jr., Volgas D.A. The posterolateral corner of the knee: Repair versus reconstruction. Am J Sports Med. 2005;33:881–888. doi: 10.1177/0363546504271208. [DOI] [PubMed] [Google Scholar]
- 21.Noyes F.R., Barber-Westin S.D. Posterior cruciate ligament revision reconstruction, part 1: Causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33:646–654. doi: 10.1177/0363546504271210. [DOI] [PubMed] [Google Scholar]
- 22.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 23.Chahla J., Nitri M., Civitarese D., Dean C.S., Moulton S.G., LaPrade R.F. Anatomic double-bundle posterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e149–e156. doi: 10.1016/j.eats.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Badlani J.T., Borrero C., Golla S., Harner C.D., Irrgang J.J. The effects of meniscus injury on the development of knee osteoarthritis: Data from the osteoarthritis initiative. Am J Sports Med. 2013;41:1238–1244. doi: 10.1177/0363546513490276. [DOI] [PubMed] [Google Scholar]
- 25.Krych A.J., Sousa P.L., King A.H., Engasser W.M., Stuart M.J., Levy B.A. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3019–3025. doi: 10.1007/s00167-015-3540-9. [DOI] [PubMed] [Google Scholar]
- 26.Liow R.Y., McNicholas M.J., Keating J.F., Nutton R.W. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845–851. [PubMed] [Google Scholar]
- 27.Engebretsen L., Risberg M.A., Robertson B., Ludvigsen T.C., Johansen S. Outcome after knee dislocations: A 2-9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026. doi: 10.1007/s00167-009-0869-y. [DOI] [PubMed] [Google Scholar]
- 28.Stannard J.P., Black B.S., Azbell C., Volgas D.A. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25:429–434. doi: 10.1055/s-0032-1322605. [DOI] [PubMed] [Google Scholar]
- 29.Fanelli G.C., Edson C.J. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 30.Werner B.C., Hadeed M.M., Gwathmey F.W., Jr., Gaskin C.M., Hart J.M., Miller M.D. Medial injury in knee dislocations: What are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472:2658–2666. doi: 10.1007/s11999-014-3483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moulton S.G., Geeslin A.G., LaPrade R.F. A systematic review of the outcomes of posterolateral corner knee injuries, part 2: Surgical treatment of chronic injuries. Am J Sports Med. 2016;44:1616–1623. doi: 10.1177/0363546515593950. [DOI] [PubMed] [Google Scholar]
- 32.McCarthy M., Camarda L., Wijdicks C.A., Johansen S., Engebretsen L., Laprade R.F. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38:1674–1681. doi: 10.1177/0363546510361220. [DOI] [PubMed] [Google Scholar]
- 33.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 34.Gelber P.E., Masferrer-Pino A., Erquicia J.I. Femoral tunnel drilling angles for posteromedial corner reconstructions of the knee. Arthroscopy. 2015;31:1764–1771. doi: 10.1016/j.arthro.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 35.Camarda L., Grassedonio E., Lauria M., Midiri M., D'Arienzo M. How to avoid collision between PCL and MCL femoral tunnels during a simultaneous reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2767–2772. doi: 10.1007/s00167-014-3446-y. [DOI] [PubMed] [Google Scholar]
- 36.Markolf K.L., O'Neill G., Jackson S.R., McAllister D.R. Reconstruction of knees with combined cruciate deficiencies: A biomechanical study. J Bone Joint Surg Am. 2003;85:1768–1774. doi: 10.2106/00004623-200309000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Wentorf F.A., LaPrade R.F., Lewis J.L., Resig S. The influence of the integrity of posterolateral structures on tibiofemoral orientation when an anterior cruciate ligament graft is tensioned. Am J Sports Med. 2002;30:796–799. doi: 10.1177/03635465020300060701. [DOI] [PubMed] [Google Scholar]
- 38.Ibrahim S.A., Ahmad F.H., Salah M., Al Misfer A.R., Ghaffer S.A., Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24:178–187. doi: 10.1016/j.arthro.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 39.Bin S.I., Nam T.S. Early results of high-flex total knee arthroplasty: Comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–355. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 40.Dedmond B.T., Almekinders L.C. Operative versus nonoperative treatment of knee dislocations: A meta-analysis. Am J Knee Surg. 2001;14:33–38. [PubMed] [Google Scholar]
- 41.Owens B.D., Neault M., Benson E., Busconi B.D. Primary repair of knee dislocations: Results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma. 2007;21:92–96. doi: 10.1097/BOT.0b013e3180321318. [DOI] [PubMed] [Google Scholar]
- 42.Shelbourne K.D., Haro M.S., Gray T. Knee dislocation with lateral side injury: Results of an en masse surgical repair technique of the lateral side. Am J Sports Med. 2007;35:1105–1116. doi: 10.1177/0363546507299444. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
After induction of general anesthesia, the patient is placed in the supine position on the operating table. After sterile preparation and draping, the medial knee structures are approached first to identify structures before structure extravasation. A hockey stick incision is performed proximally between the adductor tubercle and the patella. The incision is extended 8 cm distally over the joint line along the anteromedial tibia. A combination of blunt and sharp dissection is used to expose the subcutaneous structures and to identify the hamstring tendons. The semitendinosus and gracilis tendons are harvested proximally for the medial collateral ligament (sMCL) augmentation procedure. Of note, their tibial insertion should remain attached at the pes anserine. A spinal needle is used to identify the joint line and a ruler is then used to measure 6 cm distal to the medial joint line to identify the distal tibial attachment of the sMCL. Two double-loaded suture anchors are placed at the posteromedial aspect of the tibia posteriorizing the attachment of the grafts to recreate the anatomic distal insertion of the sMCL. Attention is then directed proximally. Using the adductor magnus tendon and subsequently the adductor tubercle as a landmark, the sMCL proximal attachment is identified 12 mm distal and 8 mm anterior. Sharp dissection is performed to identify the attachment in a small depression posterior and proximal to the medial epicondyle. An eyelet pin is drilled through the sMCL femoral attachment. A 7-mm reamer is reamed over the guide pin to a depth of 35 mm for the proximal femoral reconstruction tunnel. A passing suture is then placed through the tunnel for the later graft passage. Both tendon grafts are then passed proximally along the native course of the sMCL deep to the sartorial fascia. The graft length is measured and it is whipstitched 30 mm proximal to the femoral tunnel entrance. Afterward, the excess graft length is removed. The sMCL grafts remain unfixed until later in the procedure. Routine arthroscopy is then performed. The femoral attachment site of the anterior cruciate ligament (ACL) on the medial wall of the lateral femoral condyle is prepared. An accessory medial portal is established first by using a spinal needle. A 10-mm low-profile reamer is used to create a 25-mm closed socket tunnel for the ACL reconstruction. Initially, the reamer is advanced 4-5 mm to confirm maintenance of a 1- to 2-mm back wall. After the tunnel is reamed, a passing suture is placed to allow for the later ACL graft passage. Then, attention is then turned to preparing the tunnels for the femoral attachments of the posterior cruciate ligament (PCL). For the anterolateral bundle (ALB), an 11-mm-diameter acorn reamer is placed against the cartilage and a guide pin is inserted through it. Then a 25-mm deep closed socket tunnel is reamed. Next, the posteromedial bundle (PMB) tunnel is prepared using the same technique with a 7-mm-diameter acorn reamer to a depth of 25 mm. These 2 tunnels should diverge and must have at least 1-2 mm of bony bridge at the entrances. Passing sutures are placed in each tunnel to allow for the later PCL graft passage. To prepare the tibial attachment of the PCL, a 70° arthroscope is used and a posteromedial portal can be created if needed. The posterior capsule is carefully resected with the aid of a shaver and a radiofrequency device until the popliteus muscle fibers are observed. The shiny white fibers, lateral articular cartilage, bundle ridge, and the champagne drop-off are used as references to locate the PCL tibial attachment. The guide pin is them drilled using a PCL aiming device located at the bundle ridge. The tibial footprint of ACL is then identified and a tibial ACL guide pin is drilled at this point. A 10-mm acorn reamer is used to antegrade ream the tunnel. The PCL grafts are passed first to allow appropriate reduction of the tibiofemoral joint. The posteromedial bundle PCL graft is passed first into its femoral tunnel and fixed with a 7 × 23 mm bioabsorbable interference screw. The bone plug for the ALB PCL graft is then passed into its femoral reconstruction tunnel and secured with a 7 × 20 mm titanium interference screw. The ACL graft is then passed into the femoral tunnel using the passing suture and fixed in the femur with a 7 × 20 mm titanium interference screw. Once all grafts are shuttled through the anterior tibia, the PCL grafts are secured first. With the knee flexed to 90° of knee flexion, the ALB graft is split in line with its fibers and fixed using a 6.5-mm cancellous screw and a spiked washer. Then, the PMB graft is fixed to the tibia in full extension. Next, the ACL graft tibial fixation is performed with the knee in full extension, traction applied to the graft sutures, and with a 9 × 20 mm titanium interference screw after cycling the grafts several times to remove any slack on the grafts. The cruciate ligament grafts are then arthroscopically visualized to confirm restoration of the tibiofemoral position. The semitendinosus and gracilis grafts are pulled into the femoral tunnel and fixed with a 7 × 25 mm PEEK (polyether ether ketone) interference screw. A double-loaded suture anchor is then inserted 12-15 mm distal to the medial joint line to reconstitute the proximal tibial attachment of the sMCL. The tourniquet is released and the excess portions of the grafts are removed. The “safe zone” range of motion is determined to guide the initial amount of knee motion allowed for postoperative rehabilitation. Hemostasis is performed, the subcutaneous and skin tissues are closed, and the procedure is complete.