Abstract
Background
In acute respiratory respiratory distress syndrome (ARDS) a sustained mismatch of alveolar ventilation and perfusion (VA/Q) impairs the pulmonary gas exchange. Measurement of endexpiratory lung volume (EELV) by multiple breath-nitrogen washout/washin is a non-invasive, bedside technology to assess pulmonary function in mechanically ventilated patients. The present study examines the association between EELV changes and VA/Q distribution and the possibility to predict VA/Q normalization by means of EELV in a porcine model.
Methods
After approval of the state and institutional animal care committee 12 anesthetized pigs were randomized to ARDS either by bronchoalveolar lavage (n = 6) or oleic acid injection (n = 6). EELV, VA/Q ratios by multiple inert gas elimination and ventilation distribution by electrical impedance tomography were assessed at healthy state and at five different positive endexpiratory pressure (PEEP) steps in ARDS (0, 20, 15, 10, 5 cmH2O; each maintained for 30 min).
Results
VA/Q, EELV and tidal volume distribution all displayed the PEEP-induced recruitment in ARDS. We found a close correlation between VA/Q < 0.1 (representing shunt and low VA/Q units) and changes in EELV (spearman correlation coefficient −0.79). Logistic regression reveals the potential to predict VA/Q normalization (VA/Q < 0.1 less than 5%) from changes in EELV with an area under the curve of 0.89 with a 95%-CI of 0.81–0.96 in the receiver operating characteristic. Different lung injury models and recruitment characteristics did not influence these findings.
Conclusion
In a porcine ARDS model EELV measurement depicts PEEP-induced lung recruitment and is strongly associated with normalization of the VA/Q distribution in a model-independent fashion. Determination of EELV could be an intriguing addition in the context of lung protection strategies.
Keywords: ARDS, Endexpiratory lung volume, Ventilation/perfusion mismatch, Pig model
Background
Within the lung adequate matching of alveolar ventilation and perfusion determines sufficient gas exchange. In healthy subjects the ventilation/perfusion ratio (VA/Q) is widely normally distributed with small physiological shunt and low VA/Q fractions. Development of an acute respiratory distress syndrome (ARDS) causes high amounts of atelectatic or poorly ventilated lung areas going along with an altered perfusion [1, 2], which leads to a sustained VA/Q mismatch and consecutive gas exchange impairment. VA/Q ratios can hardly be measured in the clinical routine, and can only be estimated from conventional blood gas analysis or shunt calculation. Sophisticated imaging technologies like single photon emission tomography or positron emission tomography lack feasibility in critically ill patients [3]. The multiple inert gas elimination technique (MIGET) is regarded as experimental gold standard for VA/Q measurement, though also has feasibility concerns despite advances in technology, automatization and time requirements [4]. Another novel, non-invasive technique for evaluation of lung aeration without radiation exposition is the assessment of the functional residual capacity or, if a positive end-expiratory pressure (PEEP) is applied, the end-expiratory lung volume (EELV) based on multiple breath nitrogen washout/washin developed by Olegard et al. [5]. This technique provides a reliable EELV measurement in vivo and correlates well to computer tomography-based volumetric assessment (r 2 = 0.89) [6].
EELV measurement does not distinguish between distinct VA/Q fractions and addresses primarily the ventilatory pattern, but not alterations of pulmonary perfusion. Hence, it is not known, if EELV measurement can predict VA/Q normalization. Hence, we sought to further analyze the association between EELV and VA/Q ratio in porcine ARDS models. We hypothesized that (1) EELV changes in different lung injury models reflect PEEP-induced recruitment and (2) EELV measurement indirectly predicts normalization of VA/Q.
Methods
After approval of the institutional and state animal care committee (Landesuntersuchungsamt Rheinland-Pfalz, Koblenz, Germany; approval number G12-1-059) we performed this prospective randomized animal study in accordance with the international guidelines for the care and use of laboratory animals. This manuscript adheres to the applicable EQUATOR guidelines.
Anesthesia and instrumentation
Twelve healthy male pigs (sus scrofa domestica, weight: 26–33 kg) were sedated (ketamine 4 mg kg−1, azaperon 8 mg kg−1 intramuscular) and delivered by a local breeder. After establishing an intravenous line anesthesia was induced and maintained by propofol (8–12 mg kg−1 h−1) and fentanyl (0.1–0.2 mg kg−1 h−1). A single dose atracurium (0.5 mg kg−1) was administered to facilitate orotracheal intubation. Ventilation (Respirator: Engström Carestation®, GE Healthcare, Germany) was started in pressure-controlled mode with a tidal volume (Vt) of 7 ml kg−1, PEEP of 5 cmH2O, fraction of inspired oxygen (FiO2) of 0.4 and a variable respiratory rate to maintain normocapnia. A balanced electrolyte solution (Sterofundin iso, B. Braun, Germany) was continuously infused at a rate of 5 ml kg−1 h−1. Vascular catheters were placed ultrasound-guided: an arterial line, a pulse contour cardiac output catheter (PiCCO, Pulsion Medical Systems, Germany), a central venous line and a 7.5-French introducer for a pulmonary arterial catheter were inserted via femoral vascular access. Esophageal pressure was measured by a balloon-catheter to enable transpulmonary pressure calculation. Respiratory and extended hemodynamic parameters were recorded continuously (Datex S/5, GE Healthcare, Germany). Further respiratory parameters and measurements were recorded by the respirator. Normothermia was maintained by body surface warming.
Extended respiratory monitoring
The EELV was determined semi-automatically through the Engström Carestation by means of the nitrogen washout/washin method with a FiO2 change of 0.1 as described by Olegard and co-workers [5]. All measurements were done twice and the mean value was used. All EELV measurements were referenced to the animals’ individual baseline value in a healthy state (EELV/EELVBaseline [%]). The VA/Q-distribution was determined using micropore membrane inlet mass spectrometry-MIGET (MMIMS-MIGET, Oscillogy LLC, Folsom, PA, USA). After steady-state infusion of a saline solution containing six inert gases (sulphur hexafluoride, krypton, desfluran, enfluran diethyl ether and acetone) in subclinical and non-toxic dosage for 30 min, synchronous mixed-venous and arterial blood samples were taken. Following ARDS induction the saline solution was infused continuously to guarantee a steady state of inert gas retention and elimination. Sampling procedure and data processing were carried out according to previously reported protocols [7]. Hypoventilated compartments (VA/Q < 0.1) representing the sum of true shunt (VA/Q < 0.05) and low VA/Q areas, normal and hyperventilated compartments (high VA/Q) are reported as fraction of cardiac output [7, 8]. To analyze the regional ventilation distribution we used an electrical impedance tomography device (EIT; Goe-MF II, CareFusion, San Diego, CA, USA) that records thoracic bioimpedance variations associated with tidal ventilation. The electrodes were placed on a transverse lung section just below the axilla. The regional ventilation distribution was examined for the non-dependent, central, and dependent lung regions (Levels L1-L3) as percentage of the global tidal amplitude [9].
Study protocol
Following instrumentation, we set the FiO2 to 1.0 and conducted a lung recruitment maneuver (plateau pressure 40 cmH2O for 10 s). Then baseline parameters were assessed at healthy state. Afterwards the pigs were randomized to ARDS induction by either lung lavage (LAV, n = 6) followed by 1 h of high tidal volume ventilation [7] or by central venous oleic acid injection (OAI, n = 6) to depict different etiologies and kinetics of ARDS. For LAV the endotracheal tube was clamped in inspiration. Then 30 ml kg−1 of warmed balanced saline solution were instilled and directly drained by gravity. Lavage procedures were repeated within 10 min intervals until a PaO2/FiO2 ratio ≤ 250 mmHg was achieved. Afterwards animals were ventilated for 1 h in pressure-controlled mode with the following settings: Vt of 15 ml kg−1, PEEP 0, FiO2 1.0, and respiratory rate to maintain normocapnia. After this hour Vt was reduced to 7 ml kg−1. For OAI 0.1 ml kg−1 of oleic acid (cis-9-octadecenoic acid) were solved in 20 ml saline solution and injected via the central venous line in fractions of 2 ml every 3 min. The procedure was repeated with another 0.1 ml kg−1 after 15 min, if the PaO2/FiO2 was higher than 200 mmHg. After ARDS criteria were fulfilled respirator settings were adapted: Vt 7 ml kg−1, FiO2 1.0. We used five different PEEP steps throughout the experiment (0, 20, 15, 10, 5 [cmH2O]), whereby each step was maintained for 30 min to achieve stable conditions. If necessary to warrant stable hemodynamics during the experiments (mean arterial pressure > 60 mmHg), norepinephrine was administered. After finishing all measurements, the animals were killed in deep general anesthesia by injection of 200 mg propofol and 40 mmol potassium.
Statistics
Physiological parameters are displayed as mean and standard deviations. A repeated measurement ANOVA was performed to compare the parameters between the different PEEP levels using the F-test for least squares means and Bonferroni-adjusted post-hoc t-tests for the pairwise comparisons. To investigate the influence of PEEP and injury model on the relative change in EELV from baseline, PaO2 and tidal volume distribution per level linear mixed models were fitted with PEEP level and lung injury model as fixed factors and a random intercept to account for intra-subject correlations. For PaO2 an interaction term PEEP *injury model was included. F-tests and t-tests for least squares means (LS-means) differences were calculated for the fixed effects and pairwise comparisons, respectively. In the interaction model for PaO2 the pairwise comparisons between PEEP steps were derived from the average LS-means over the two injury models and the comparison between the two injury models was derived from the average LS-means over the PEEP steps. The changes in VA/Q between the different PEEP levels and baseline are evaluated by Wilcoxon signed rank tests. Correlation between the relative change in EELV and VA/Q is described by a scatter plot and the spearman rank correlation coefficient. Further associations between EELV respectively VA/Q < 0.1 and PaO2, lung compliance, and airway driving pressure were analyzed. The discriminating ability of relative change in EELV to distinguish between VA/Q fractions < 0.1 above or below 5, 10, 15 and 30% is described by receiver operating characteristic (ROC) curves as derived from logistic regression. As this is an explorative study no adjustments for multiple testing have been done. P-values are given for descriptive reasons only and must be interpreted with caution due to the large number of tests.
Results
A total of 12 animal experiments were included in this study. One animal didn’t tolerate the zero PEEP setting after induction of ARDS, so we applied a PEEP of 5 cmH2O for the initial step. Another animal died following the last drop to PEEP 5 cmH2O in ARDS. Lung injury induction led to sustained gas exchange impairment, increase of the extravascular lung water content and pulmonary arterial hypertension. The physiological parameters are summarized in Table 1.
Table 1.
Physiological parameters
| Baseline | P0 | P20 | P15 | P10 | P5 | |
|---|---|---|---|---|---|---|
| MAP [mmHg] | 82 ± 8 | 81 ± 17 | 69 ± 12a, b | 76 ± 13 | 75 ± 12 | 74 ± 12 |
| CVP [mmHg] | 7 ± 1 | 6 ± 2 | 9 ± 2 | 9 ± 2 | 8 ± 2 | 6 ± 2 |
| MPAP [mmHg] | 17 ± 2 | 35 ± 5a | 32 ± 5a | 29 ± 6a | 30 ± 9a | 28 ± 6a |
| CO [l min−1] | 3.8 ± 0.6b, c | 5.2 ± 1.6 | 3.7 ± 0.9b, c | 3.8 ± 0.8b, c | 4.2 ± 1.0c | 5.6 ± 1.5 |
| EVLWI [ml kg−1] | 13 ± 4 | 25 ± 10a | 22 ± 9a | 22 ± 9a | 23 ± 9a | 24 ± 10a |
| Vt [ml kg−1] | 6.6 ± 0.4 | 6.9 ± 0.4 | 6.9 ± 0.5 | 6.9 ± 0.4 | 6.9 ± 0.4 | 7.0 ± 0.4 |
| RR [min−1] | 36 ± 4 | 35 ± 3 | 44 ± 3a, b | 44 ± 3a, b | 43 ± 3a, b | 41 ± 4a, b |
| etCO2 [mmHg] | 39 ± 2 | 40 ± 6c | 46 ± 4a, b, d, c | 42 ± 3d, c | 38 ± 2 | 36 ± 3 |
| Ppeak [cmH2O] | 15 ± 2 | 29 ± 8a | 40 ± 3a, b, e, d, c | 32 ± 4a | 29 ± 6a | 28 ± 7a |
| PEEP [cmH2O] | 5 ± 1 | 1 ± 1a, e, d, c | 21 ± 1a, b, e, d, c | 16 ± 1a, d, c | 10 ± 1a, c | 5 ± 1 |
| PTP [cmH2O] | 5 ± 3 | 18 ± 6a | 25 ± 3a, b, e, d, c | 19 ± 4a | 17 ± 6a | 17 ± 9a |
| ∆P [cmH2O] | 8 ± 2 | 25 ± 5a, e, c | 18 ± 3a, b | 15 ± 4a | 18 ± 7a | 22 ± 7a, e, d |
| Cdyn [ml cmH2O−1] | 22 ± 7 | 8 ± 2a | 12 ± 3a, b | 14 ± 4a, b, c | 13 ± 5a, b | 10 ± 3a |
MAP mean arterial pressure, CVP central venous pressure, MPAP mean pulmonal arterial pressure, CO cardiac output, EVLWI extravascular lung water index, V t tidaL volume, RR respiratory rate, etCO 2 endtidal carbon dioxide, P peak peak inspiratory pressure, PEEP positive endexpiratory pressure, P TP transpulmonary pressure, ∆P dynamically calculated airway driving pressure (Ppeak-PEEP), C dyn dynamic lung compliance
P < 0.05
a vs. BLH
b vs. P0
c vs. P5
d vs. P10
e vs P15
Figure 1 shows the PEEP-related changes of VA/Q distribution (upper graph) and regional tidal ventilation (lower graph): shunt values were significantly higher at PEEP 0 (p < 0.001), PEEP 10 (p < 0.05) and PEEP 5 (p < 0.05) compared to baseline. Low VA/Q was significantly higher at PEEP 0 (p < 0.05) compared to baseline, at PEEP 5 significance was marginally missed (p = 0.058). No relevant high VA/Q ratios developed despite the PEEP changes. The regional ventilation distribution shows a PEEP dependency in ARDS with reduced tidal ventilation in the dependent lung areas and a corresponding increase in the central and non-dependent regions. The non-dependent region exhibits decent, but significant (each p < 0.05) changes in tidal ventilation between PEEP 0 and all other PEEP levels. Tidal ventilation in the dependent lung area also responds to the PEEP-induced recruitment with significant difference between all PEEP steps except PEEP 15 versus PEEP 20 (p = 0.76). Induction of ARDS significantly reduced the EELV in both groups (Fig. 2). Considerable alterations occurred in response to the consecutive PEEP escalation (p < 0.001) without difference between the two lung injury models (p = 0.19). The PaO2 significantly changed with each PEEP step as compared to baseline (p < 0.001). Furthermore, there revealed to be a model-dependent influence in the resulting PaO2 (p < 0.001).
Fig. 1.
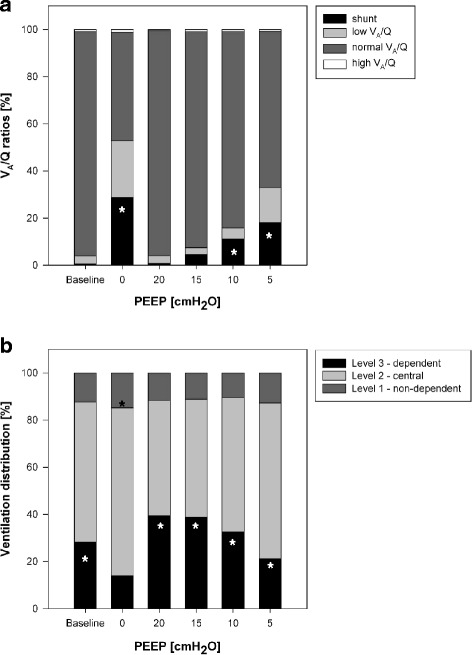
Influence of PEEP-induced lung recruitment on VA/Q distribution and ventilation distribution. The VA/Q distribution was measured by multiple inert gas elimination (upper graph) and the ventilation distribution by electrical impedance tomography (lower graph). Key statistical findings (p < 0.05) are marked by *
Fig. 2.
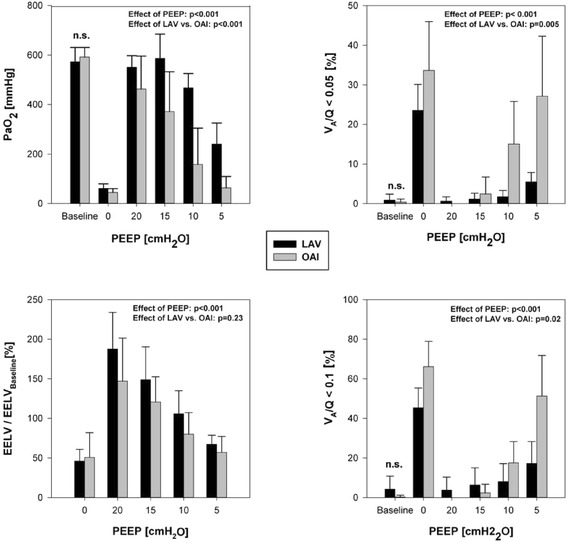
Model-dependent effect of PEEP-induced lung recruitment in bronchoalveolar lavage (LAV)-induced versus oleic acid injection (OAI)-ARDS. Impact on PaO2 and EELV (upper/lower left) and VA/Q fractions < 0.05 (shunt; upper right) and < 0.1 (all hypoventilated areas; lower right). n.s. non-significant
Despite differences in response to PEEP-induced recruitment the EELV is highly correlated to VA/Q ratios < 0.1 with a spearman rank correlation coefficient of −0.79 (Fig. 3). The separate coefficients for the two ARDS models were −0.71 (LAV) and −0.81 (OAI). Logistic regression showed a ROC curve with an area under the curve (AUC) of 0.89 with a 95%-CI of [0.81; 0.96] (Fig. 4) when discriminating between VA/Q fractions < 0.1 above or below 5%. A Youden index of 0.77 is observed when applying a threshold of 96.8% for the relative change in EELV from baseline. The same threshold applied to discriminate between VA/Q fractions < 0.1 above or below 10 and 15% results in a Youden index of 0.73, respectively. For VA/Q fractions < 0.1 below 30% the best Youden index of 0.7 is observed when defining a threshold for the EELV-change of 57.5%. Additional analyses revealed that changes in EELV are associated with changes in PaO2(Spearman correlation coefficient 0.74, p < 0.001), in lung compliance (Spearman correlation coefficient 0.48, p < 0.001) and dynamically calculated driving pressure (peak pressure – PEEP; Spearman correlation coefficient −0.46, p < 0.001). VA/Q ratios < 0.1 are also correlated with lung compliance (Spearman correlation coefficient −0.65, p < 0.001) and airway driving pressure (Spearman correlation coefficient 0.66, p < 0.001).
Fig. 3.
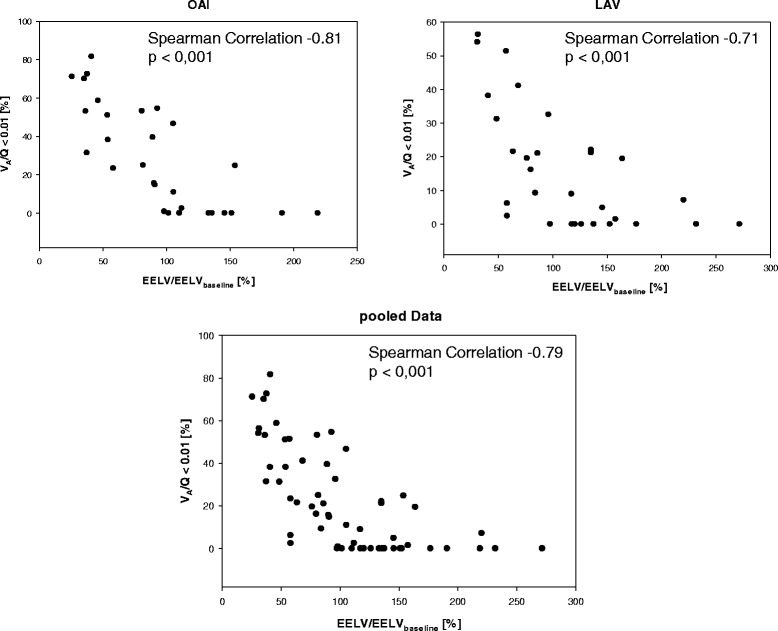
Correlation between VA/Q <0.1 and EELV. Separate correlations for oleic-acid injection (OAI)-ARDS (upper left), bronchoalveolar lavage (LAV)-ARDS (upper right) and the pooled data (lower graph)
Fig. 4.
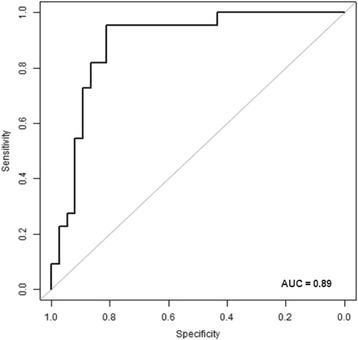
Receiver operating characteristic curve for the prediction of VA/Q normalization by EELV measurements. AUC: area under the curve
Discussion
The present study examines the association EELV and VA/Q in lung injured pigs: a close correlation (R = −0.79) and a ROC with an AUC of 0.89 were found. The ROC curve is a tool to evaluate the predictive potency of a parameter by examining sensitivity and specificity, whereby the AUC is regarded a quality marker [10]. Regarding this, our data show the possibility to predict changes in VA/Q ratios < 0.1 with high accuracy by measuring EELV in pigs. Our results retrieve a strong association, that even in ARDS if the EELV is close to the individuals’ baseline, VA/Q fractions < 0.1 are smaller than 5%. The ability of EELV to discriminate VA/Q fractions < 0.1 smaller than 10 or 15% showed similar results. Additional, but less considerable associations were found between EELV and lung compliance respectively dynamic driving pressure.
Measurement of EELV by means of nitrogen washout/washin is a novel technique that has been made available for bedside use due to integration in intensive care respirators. The technique was successfully validated against computer tomography and helium dilution technique [6]. EELV measurements show a good correlation to PEEP-induced lung volume changes, if leakage-related artefacts are prevented (r 2 = 0.80) [11]. The ratio of PEEP-induced changes in EELV and the baseline functional residual capacity can be used to differentiate patients with a high or low recruitment potential [12]. In pigs, EELV significantly correlates but underestimates the computer tomography-based volumetry with an AUC of at least 0.73 for EELV changes larger than 150 ml [13]. ARDS induces a shift towards hypoventilated areas (low VA/Q) and shunt [7]. The MIGET-derived VA/Q is able to depict ventilation [4, 14] as well as perfusion impairment [8, 15]. Our data reveal that during PEEP-induced recruitment measurement of EELV reliably predicts the occurring VA/Q normalization. Theoretically, derecruitment and atelectasis formation subsequently leading to EELV decrease is inherent to VA/Q mismatch and shunt increase. This simplified model, however, neither considers poorly ventilated but non-atelectatic lung tissue nor altered perfusion that is capable to affect VA/Q independently of lung recruitment. Though, the hemodynamic response to PEEP escalation in our data does not suggest the latter. Considerable low VA/Q fractions occur not only in our data (Fig. 1) but also in patients suffering from ARDS [16] and substantially influence VA/Q mismatch. Conversion of low to normal VA/Q areas may not be fully reflected by EELV increase, which explains that PaO2 can increase despite constant EELV [17]. This highlights the need for differentiation between mere anatomical and functional recruitment [18]. To our knowledge, the present study is the first to approve a direct predictive value of EELV on VA/Q despite this complex underlying pathophysiology. Several factors that alter pulmonary perfusion like hypovolemia or impaired hypoxic pulmonary vasoconstriction (HPV) may also influence the reported correlation. In lipopolysaccharide-induced sepsis HPV is blunted [19], which contributes significantly to VA/Q mismatch and may interfere with the VA/Q-EELV association. Pigs, in this context, exhibit a high degree of HPV [20], which is not compromised by LAV-induced ARDS, but may be reduced by OAI to a certain degree [21]. Accordingly, the predictive value of EELV needs to be interpreted in the individual context.
Our results further explain the findings of Krause et al. [22]: they showed an optimal effect of inhaled nitric oxide in lung injured pigs when EELV was similar to the pre-injury state. This is associated with an intact VA/Q distribution and may provide ideal conditions for drug inhalation. The declining effect with further increase in PEEP and EELV on the other hand should be related to a shift from normal to high VA/Q areas and impaired perfusion. The complex combination of several pathomechanisms in ARDS can hardly by mimicked in full extent by experimental models [23]. Assessment of lung recruitability is crucial in ARDS patients: the individual recruitability may influence the ventilatory management, PEEP requirement, and even survival [24]. In experimental research the response to ventilatory interventions may very well depend on the chosen model and its underlying pathomechanism [9]. To reduce the probability of a mere model-dependent effect, we chose to examine two common but different models of ARDS with LAV and OAI, which represent surfactant depletion-related alveolar collapse and atelectasis respectively capillary leakage-induced edema and alveolar flooding [25]. Based on these considerations LAV-injured lungs respond well to PEEP or recruitment maneuvers [2]. The OAI model, however, is characterized by a need for higher PEEP to improve oxygenation [26]. Low VA/Q areas are considerably larger in OAI and less recruitable [2]. Furthermore, an only moderate correlation of PEEP-induced EELV or with PaO2 (r 2 = 0.53) was found in a previous study [27], which may be caused by delayed recruitment from low to normal VA/Q ratios that contribute to the gas exchange to a lesser degree than directly recruited atelectasis. Consistent with this data, we found a significantly higher PaO2 and decrease of shunt and low VA/Q ratios at lower PEEP in lung LAV-injured pigs, but no model-dependent differences in EELV. This may be caused higher variances and the smaller EELV changes between the PEEP steps as assumed by Richard et al. [13]. In both models, though, EELV and VA/Q < 0.1 are separately correlated despite different response in the PEEP trial. Hence given a positive PEEP response, EELV referenced to its individual baseline reliably predicts VA/Q normalization independent from the model related recruitment characteristics.
The present study has some limitations. PEEP-induced EELV normalization is not necessarily lung protective by itself. A forced PEEP raise may lead to injurious hyperinflation of the persisting healthy lung tissue even without achieving a fully recruited lung [28]. In our model sustained hyperinflation is unlikely due to only minimal occurrence of high VA/Q ratios going along with decent changes of tidal ventilation in the non-dependent lung areas. Nevertheless, we cannot fully rule out overdistension, but this was not the main focus of this study and may be addressed in further examinations. Increased endtidal CO2 levels in the high PEEP settings may point towards increasing dead space to which we cannot provide sufficient physiological explanations from the present data. Recent data highlight the role of the driving pressure (plateau pressure – PEEP) to determine the meaningfulness of respiratory modifications [29]. Instead, the present protocol only allowed for calculation of the dynamic, but yet less validated, variant of airway driving pressure (peak pressure – PEEP) [30]. If below harmful thresholds, patients might benefit from VA/Q optimization without the risk of sustained further injury. Hence, EELV measurement can represent only one cornerstone to optimize lung recruitment and gas exchange in a lung protective ventilation strategy, if severe hyperinflation is prevented by additional monitoring methods [31]. We found a good discriminating ability for VA/Q fractions < 0.1 below 5, 10 and 15 when applying a threshold of 96.8% of baseline EELV and a slightly minor discriminating ability for VA/Q fractions < 0.1 below 30% when applying a threshold of 57.5% for the EELV change. 96.8% of the baseline EELV revealed to be the optimum cut-off. But the individual amounts of VA/Q < 0.1, which is just tolerable to ensure sufficient oxygenation in ARDS patients, needs to be confirmed in clinical studies. We referenced the EELV to the individual baseline value rather than comparing the absolute EELV. This concept has been previously assumed [22] and prevents variances due to different individual conditions. Dellamonica et al. developed a method to determine this baseline even in ARDS patients by using a prolonged exhalation without direct measurements at zero PEEP or derecruitment [12].
Conclusion
In porcine ARDS models measurement of EELV by nitrogen washout/washin retraces PEEP-induced recruitment, VA/Q normalization and ventilation distribution. The EELV is strongly associated with the extent of VA/Q ratios < 0.1. An EELV close to the individual baseline value predicts normalization of the VA/Q with a high sensitivity.
Automatized nitrogen washout/washin is an interesting bedside tool for EELV measurement and even indirect assessment of the VA/Q mismatch in ARDS. Implementation of EELV in lung protection strategies could facilitate the decision, if patients benefit from further recruitment.
Acknowledgements
The authors thank Dagmar Dirvonskis for technical assistance.
Funding
The study was supported in part by a Stage 1 grant of the Johannes Gutenberg-University Mainz to JK and the German Research Council (DFG DA 842/2-2).
Availability of data and materials
The datasets generated and/or analysed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
JK, AGB, BD and TL conducted the experiments. JK, AJE and EKH performed the data analysis. JK and EKH drafted the manuscript. FH revised the manuscript. MD and EKH participated in the study design, supervision of laboratory, data interpretation and revision of the manuscript. All authors edited and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval
The study was approved by the institutional and state animal care committee (Landesuntersuchungsamt Rheinland-Pfalz, Koblenz, Germany; approval number G12-1-059).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ANOVA
Analysis of variance
- ARDS
Acute respiratory distress syndrome
- AUC
Area under the Curve
- EELV
Endexpiratory lung volume
- EIT
Electrical impedance tomography
- etCO2
endtidal CO2
- FiO2
Fraction of inspired oxygen
- HPV
Hypoxic pulmonary vasoconstriction
- LAV
ARDS induced by bronchoalveolar lavage
- LS
Least squares
- MAP
Mean arterial pressure
- MMIMS-MIGET
Micropore membrane inlet mass spectrometry - multiple inert gas elimination technique
- OAI
ARDS induced by central-venous injection of oleic acid
- PaO2
Arterial partial pressure of oxygen
- PEEP
Positive end-expiratory pressure
- ROC
Receiver operating characteristic
- VA/Q
Ventilation/perfusion distribution
- Vt
Tidal volume
Contributor Information
Jens Kamuf, Email: kamuf@uni-mainz.de.
Andreas Garcia-Bardon, Email: a.garciabardon@uni-mainz.de.
Bastian Duenges, Email: duenges@anaesthesie.klinik.uni-mainz.de.
Tanghua Liu, Email: smile_liuth@hotmail.com.
Antje Jahn-Eimermacher, Email: jahna@uni-mainz.de.
Florian Heid, Email: heid@uni-mainz.de.
Matthias David, Email: david@uni-mainz.de.
Erik K. Hartmann, Email: hartmane@uni-mainz.de
References
- 1.Dakin J, Jones AT, Hansell DM, Hoffman EA, Evans TW. Changes in lung composition and regional perfusion and tissue distribution in patients with ARDS. Respirology. 2011;16:1265–1272. doi: 10.1111/j.1440-1843.2011.02048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karmrodt J, Bletz C, Yuan S, David M, Heussel CP, Markstaller K. Quantification of atelectatic lung volumes in two different porcine models of ARDS. Br J Anaesth. 2006;97:883–895. doi: 10.1093/bja/ael275. [DOI] [PubMed] [Google Scholar]
- 3.Hopkins SR, Wielputz MO, Kauczor HU. Imaging lung perfusion. J Appl Physiol (1985) 2012;113:328–339. doi: 10.1152/japplphysiol.00320.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kretzschmar M, Schilling T, Vogt A, Rothen HU, Borges JB, Hachenberg T, Larsson A, Baumgardner JE, Hedenstierna G. Multiple inert gas elimination technique by micropore membrane inlet mass spectrometry--a comparison with reference gas chromatography. J Appl Physiol (1985) 2013;115:1107–1118. doi: 10.1152/japplphysiol.00072.2013. [DOI] [PubMed] [Google Scholar]
- 5.Olegard C, Sondergaard S, Houltz E, Lundin S, Stenqvist O. Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg. 2005;101:206–212. doi: 10.1213/01.ANE.0000165823.90368.55. [DOI] [PubMed] [Google Scholar]
- 6.Chiumello D, Cressoni M, Chierichetti M, Tallarini F, Botticelli M, Berto V, Mietto C, Gattinoni L. Nitrogen washout/washin, helium dilution and computed tomography in the assessment of end expiratory lung volume. Crit Care. 2008;12:R150. doi: 10.1186/cc7139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartmann EK, Duenges B, Baumgardner JE, Markstaller K, David M. Correlation of thermodilution-derived extravascular lung water and ventilation/perfusion-compartments in a porcine model. Intensive Care Med. 2013;39:1313–1317. doi: 10.1007/s00134-013-2915-y. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann EK, Duenges B, Boehme S, Szczyrba M, Liu T, Klein KU, Baumgardner JE, Markstaller K, David M. Ventilation/perfusion ratios measured by multiple inert gas elimination during experimental cardiopulmonary resuscitation. Acta Anaesthesiol Scand. 2014;58:1032–1039. doi: 10.1111/aas.12378. [DOI] [PubMed] [Google Scholar]
- 9.Ziebart A, Hartmann EK, Thomas R, Liu T, Duenges B, Schad A, Bodenstein M, Thal SC, David M. Low tidal volume pressure support versus controlled ventilation in early experimental sepsis in pigs. Respir Res. 2014;15:101. doi: 10.1186/s12931-014-0101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou KH, O’Malley AJ, Mauri L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation. 2007;115:654–657. doi: 10.1161/CIRCULATIONAHA.105.594929. [DOI] [PubMed] [Google Scholar]
- 11.Dellamonica J, Lerolle N, Sargentini C, Beduneau G, Di Marco F, Mercat A, Richard JC, Diehl JL, Mancebo J, Rouby JJ, et al. Accuracy and precision of end-expiratory lung-volume measurements by automated nitrogen washout/washin technique in patients with acute respiratory distress syndrome. Crit Care. 2011;15:R294. doi: 10.1186/cc10587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dellamonica J, Lerolle N, Sargentini C, Beduneau G, Di Marco F, Mercat A, Richard JC, Diehl JL, Mancebo J, Rouby JJ, et al. PEEP-induced changes in lung volume in acute respiratory distress syndrome. Two methods to estimate alveolar recruitment. Intensive Care Med. 2011;37:1595–1604. doi: 10.1007/s00134-011-2333-y. [DOI] [PubMed] [Google Scholar]
- 13.Richard JC, Pouzot C, Pinzon AM, Gonzalez JS, Orkisz M, Neyran B, Hoyos MH, Lavenne F, Guerin C. Reliability of the nitrogen washin-washout technique to assess end-expiratory lung volume at variable PEEP and tidal volumes. Intensive Care Med Exp. 2014;2:10. doi: 10.1186/2197-425X-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartmann EK, Boehme S, Bentley A, Duenges B, Klein KU, Elsaesser A, Baumgardner JE, David M, Markstaller K. Influence of respiratory rate and end-expiratory pressure variation on cyclic alveolar recruitment in an experimental lung injury model. Crit Care. 2012;16:R8. doi: 10.1186/cc11147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson NB, Chi EY, Robertson HT. Ventilation-perfusion relationships after hemorrhage and resuscitation: an inert gas analysis. J Appl Physiol Respir Environ Exerc Physiol. 1983;54:1131–1140. doi: 10.1152/jappl.1983.54.4.1131. [DOI] [PubMed] [Google Scholar]
- 16.Retamal J, Libuy J, Jimenez M, Delgado M, Besa C, Bugedo G, Bruhn A. Preliminary study of ventilation with 4 ml/kg tidal volume in acute respiratory distress syndrome: feasibility and effects on cyclic recruitment - derecruitment and hyperinflation. Crit Care. 2013;17:R16. doi: 10.1186/cc12487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanch L, Van der Kloot TE, Youngblood AM, Murias G, Naveira A, Adams AB, Romero PV, Nahum A. Application of tracheal gas insufflation to acute unilateral lung injury in an experimental model. Am J Respir Crit Care Med. 2001;164:642–647. doi: 10.1164/ajrccm.164.4.2005127. [DOI] [PubMed] [Google Scholar]
- 18.Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–1786. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 19.Easley RB, Mulreany DG, Lancaster CT, Custer JW, Fernandez-Bustamante A, Colantuoni E, Simon BA. Redistribution of pulmonary blood flow impacts thermodilution-based extravascular lung water measurements in a model of acute lung injury. Anesthesiology. 2009;111:1065–1074. doi: 10.1097/ALN.0b013e3181bc99cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maggiorini M, Brimioulle S, De Canniere D, Delcroix M, Naeije R. Effects of pulmonary embolism on pulmonary vascular impedance in dogs and minipigs. J Appl Physiol (1985) 1998;84:815–821. doi: 10.1152/jappl.1998.84.3.815. [DOI] [PubMed] [Google Scholar]
- 21.Leeman M, Delcroix M, Vachiery JL, Melot C, Naeije R. Blunted hypoxic vasoconstriction in oleic acid lung injury: effect of cyclooxygenase inhibitors. J Appl Physiol (1985) 1992;72:251–258. doi: 10.1152/jappl.1992.72.1.251. [DOI] [PubMed] [Google Scholar]
- 22.Krause MF, Jakel C, Haberstroh J, Schulte-Monting J, Hoehn T. Functional residual capacity determines the effect of inhaled nitric oxide on intrapulmonary shunt and gas exchange in a piglet model of lung injury. Pediatr Crit Care Med. 2001;2:82–87. doi: 10.1097/00130478-200101000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Ballard-Croft C, Wang D, Sumpter LR, Zhou X, Zwischenberger JB. Large-animal models of acute respiratory distress syndrome. Ann Thorac Surg. 2012;93:1331–1339. doi: 10.1016/j.athoracsur.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 24.Caironi P, Cressoni M, Chiumello D, Ranieri M, Quintel M, Russo SG, Cornejo R, Bugedo G, Carlesso E, Russo R, et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181:578–586. doi: 10.1164/rccm.200905-0787OC. [DOI] [PubMed] [Google Scholar]
- 25.Wang HM, Bodenstein M, Markstaller K. Overview of the pathology of three widely used animal models of acute lung injury. Eur Surg Res. 2008;40:305–316. doi: 10.1159/000121471. [DOI] [PubMed] [Google Scholar]
- 26.Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ. Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med. 2001;164:122–130. doi: 10.1164/ajrccm.164.1.2007010. [DOI] [PubMed] [Google Scholar]
- 27.Lambermont B, Ghuysen A, Janssen N, Morimont P, Hartstein G, Gerard P, D’Orio V. Comparison of functional residual capacity and static compliance of the respiratory system during a positive end-expiratory pressure (PEEP) ramp procedure in an experimental model of acute respiratory distress syndrome. Crit Care. 2008;12:R91. doi: 10.1186/cc6961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Retamal J, Bugedo G, Larsson A, Bruhn A. High PEEP levels are associated with overdistension and tidal recruitment/derecruitment in ARDS patients. Acta Anaesthesiol Scand. 2015;59:1161–1169. doi: 10.1111/aas.12563. [DOI] [PubMed] [Google Scholar]
- 29.Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 30.Chiu LC, Hu HC, Hung CY, Chang CH, Tsai FC, Yang CT, Huang CC, Wu HP, Kao KC. Dynamic driving pressure associated mortality in acute respiratory distress syndrome with extracorporeal membrane oxygenation. Ann Intensive Care. 2017;7:12. doi: 10.1186/s13613-017-0236-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa EL, Borges JB, Melo A, Suarez-Sipmann F, Toufen C, Jr, Bohm SH, Amato MB. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35:1132–1137. doi: 10.1007/s00134-009-1447-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study available from the corresponding author on reasonable request.


