Abstract
Background
The relationship between inappropriate MPI and cardiovascular outcomes is poorly understood. We sought to systematically review the literature on appropriate use criteria (AUC) for MPI, including temporal trend of inappropriate testing and resulting cardiovascular outcomes.
Methods
We searched the MEDLINE database for studies related to AUC and MPI. The co-primary outcomes were abnormal test results and the presence of cardiac ischemia. Random effects odds ratios (OR) were constructed using DerSimonian-Laird method.
Results
A total of 22 studies with 23,443 patients were included. The prevalence of inappropriate testing was 14.8 % [95% confidence interval (CI) 11.6–18.7%]. Inappropriate MPI studies were less likely to be abnormal (OR 0.41 95% CI 0.35–0.49, p<0.0001) and to demonstrate ischemia (OR 0.40, 95% CI 0.24–0.67, p<0.0001) compared to appropriate testing. No difference in the rate of inappropriate tests was detected based on the midpoint of the enrollment year (p=0.54). The pattern of ordering inappropriate studies was not different between cardiology and non-cardiology providers (OR 0.74, 95% CI 0.51–1.06, p=0.10).
Conclusion
Inappropriate MPI studies are less likely to yield abnormal results or demonstrate myocardial ischemia. The rate of inappropriate MPI has not decreased over time.
Introduction
Myocardial perfusion imaging (MPI) remains a cornerstone for diagnosis and risk stratification in patients with coronary artery disease.1,2 The volume of MPI grew for the past 3 decades.3–5 Substantial growth in the use of MPI has generated concerns for overuse of this technology.6,7 To address this concern, the American College of Cardiology (ACC) and other specialty societies developed appropriate use criteria (AUC) for MPI in 2005, which was later revised in 2009.8,9
Since the development of the AUC for MPI, several studies have described the prevalence of inappropriate MPI. Most of these studies were conducted in single centers yielding variable rates of inappropriate MPI testing.10–19 The process of rating indications as “inappropriate” is supposed to account for low clinical utility in those scenarios; however, few studies have reported on the relationship between inappropriate MPI and cardiovascular outcomes.15,20–22 A recent analysis of appropriateness across imaging modalities showed a decrease in trans-thoracic echocardiography and computerized tomography angiography, but not with stress echocardiography or SPECT; however this study did not evaluate all studies in temporal sequence and did not address the relationship between inappropriate studies and cardiovascular outcomes.23
We conducted this systematic review and meta-analysis to demonstrate the relationship between inappropriate MPI and the frequency of abnormal test results and myocardial ischemia. Secondarily, we intended to test the hypothesis that inappropriate MPI testing is less common when ordered by cardiology providers.
Methods
Data sources
We performed a computerized literature search of the MEDLINE database without language restriction from January 2005 until December 2014 using the search strategy shown in Figure 1. To ensure that no potentially important studies were missed, the reference lists from the retrieved articles were also checked.
Figure 1.
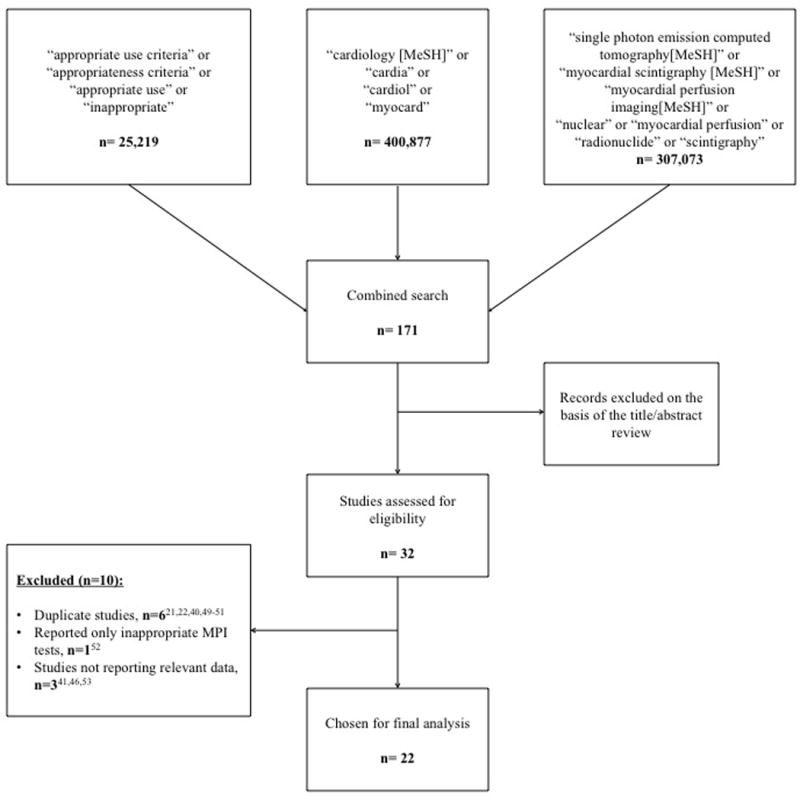
Study Selection Flow Diagram.
Summary of how the systematic search was conducted and eligible studies were identified.
Selection criteria
We selected studies that: 1) reported the prevalence of appropriate and inappropriate MPI testing according to either the 2005 or 2009 AUC for MPI, 2) described clinical outcomes among both groups, or 3) reported the variation among clinicians in ordering MPI tests. If the individual study used both criteria for evaluation of the MPI tests ordered, we utilized the data based on the 2009 AUC. We excluded studies that reported only a single arm (either appropriate or inappropriate MPI testing). If multiple reports were made from the same data, we preferentially used reports that included report of cardiovascular outcomes.
Data Extraction
Two authors (IYE and AM) independently extracted data on sample characteristics, sample size, intervention strategies, outcome measures, and other study characteristics from the included studies using a standardized form. Any discrepancies were resolved by consensus of the authors. For all clinical outcomes, we tabulated the number of events that occurred in each cohort within the study.
Outcomes and Definitions
The co-primary outcomes were the rate of abnormal test results and the presence of cardiac ischemia compared between inappropriate and appropriate or uncertain MPI. We used the definition of cardiac ischemia as reported in the individual studies. Other outcomes included all-cause mortality, non-fatal myocardial infarction (MI), the combined outcome of mortality or MI, cardiac catheterization, and revascularization.
Statistical Analysis
Since none of the studies had low event rates (arbitrarily defined as an expected event rate in any cell below 5.0), summary random effects odds ratio (OR) were constructed using the DerSimonian-Laird method.32 This meta-analysis was conducted based on the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines.33 An inverse variance weighted meta-regression for the rate of inappropriate testing versus the midpoint of the enrolment period in the individual studies was conducted. All p-values were 2-tailed, with statistical significance declared at P≤0.025. All overall estimates are accompanied by 95% confidence intervals (CI). All meta-analyses were performed using Comprehensive Meta-Analysis version 3.0 (Biostat; Englewood, New Jersey), and the meta-regression was conducted using SAS 9.3 (SAS Institute, Cary NC).
Results
A total of 22 studies with 23,443 patients were included in our analysis.10–20,34–44 The results of our search strategy are illustrated in Figure 1. The 2005 AUC were used by 6 studies,16,18,19,39,42,44 and the remainder used the 2009 AUC.10–15,17,20,34–38,40,41,43 Single-photon emission computed tomography (SPECT) was the modality utilized in most of the studies,13–20,34–36,38,39,41–44 one study reported using positron emission tomography (PET),12 while the remainder of the studies did not specify.10,11,37,40 Among the included studies, 5 were conducted outside the United States.11,17,34,38,41 Patients were recruited from the outpatient setting in 3 studies,20,35,37 from an inpatient setting in 1 study,10 and from both settings in 13 studies.11–16,19,34,36,38,40,42,43 Overall, the summary rate for inappropriate testing was 14.8% (95% CI 11.6–18.7%). The baseline characteristics and the percentage of inappropriate testing among the included studies are reported in Table 1. In Table 2, we summarize the quality of the studies included and report the most common reason for inappropriate MPI in the individual studies.
Table 1.
Baseline characteristics of the included studies
| Study (Ref#) | Year | AUC used | Patients, n | Age, years mean (SD) | DM, % | Obesity, % † | CAD, % | Inappropriate testing, % |
|---|---|---|---|---|---|---|---|---|
| Mahajan et al10 | 2014 | 2009 | 403 | 62 (14) | 31 | 50 | 27 | 29.3 |
| Medolago et al34 | 2014 | 2009 | 866 | 67 (10) | NR | NR | 49 | 17.2 |
| Oliveira et al11 | 2014 | 2009* | 367 | 65 (12) | 27 | 20 | NR | 5.2 |
| Johnson et al35 | 2014 | 2009 | 206 | NR | NR | NR | NR | 10.2 |
| Winchester et al12 | 2014 | 2009 | 582 | NR | 41 | 68 | 41 | 9.8 |
| Lalude et al13 | 2014 | 2009 | 420 | 56 | 39 | 51 | NR | 12.9 |
| Singh et al14 | 2014 | 2009 | 328 | 67 | 33 | NR | 38 | 5.5 |
| Khawaja et al36 | 2013 | 2009 | 280 | 67 (11) | 26 | NR | NR | 23.6 |
| Doukky et al20 | 2013 | 2009 | 1,511 | 59 (13) | 22 | NR | NR | 45.5 |
| Aldweib et al15 | 2013 | 2009 | 1,105 | 64 (13) | 28 | 45 | 18 | 18.0 |
| Lin et al37 | 2013 | 2009 | 338 | 57 (8) | 25 | NR | 49 | 13.0 |
| Moralidis et al38 | 2013 | 2009 | 3,032 | 66 (11) | NR | NR | 44 | 19.2 |
| Soine et al39 | 2012 | 2005 | 2,782 | 59 (12) | 28 | NR | NR | 9.2 |
| Nelson et al40 | 2012 | 2009 | 300 | 48 (11) | 28 | NR | NR | 19.3 |
| Gholamrezanezhad et al41 | 2011 | 2009* | 291 | 55 (10) | 22 | NR | NR | 16.8 |
| Gupta et al16 | 2011 | 2005 | 314 | 62 (14) | 24 | NR | 33 | 10.8 |
| Druz et al42 | 2011 | 2005 | 570 | 64 (13) | NR | NR | 28 | 14.7 |
| Koh et al17 | 2011 | 2009 | 1,623 | 61 (11) | 31 | NR | NR | 10.0 |
| Carryer et al43 | 2010 | 2009* | 281 | 67 (11) | 27 | 41 | NR | 24.2 |
| Hendel et al44 | 2010 | 2005 | 6,351 | 66 (12) | 23 | NR | NR | 13.4 |
| Mehta et al18 | 2008 | 2005 | 1,209 | 61 | NR | NR | NR | 12.7 |
| Gibbons et al19 | 2007 | 2005 | 284 | 67 (11) | 27 | 41 | NR | 14.1 |
Studies that utilized both the 2009 and 2005 AUC, data reported is for the 2009 AUC
Body mass index ≥ 30
AUC= appropriate use criteria, CAD= coronary artery disease, DM= diabetes mellitus, NR= not reported, SD= standard deviation
Table 2.
Assessment of study components
| Study (Ref#) | Study design | Outpatient/ inpatient | Institution | Single/ multi-center | Restrictive inclusion criteria | Commonest reason for inappropriate testing |
|---|---|---|---|---|---|---|
| Mahajan et al10 | Retrospective | Inpatient | Academic | Single | No | Non acute chest pain |
| Medolago et al34 | Prospective | Both | Academic | Multi | No | Non acute chest pain |
| Oliveira et al11 | Retrospective | Both | Academic | Single | No | Asymptomatic patient until 1 year after revascularization |
| Johnson et al35 | Prospective | Outpatient | Community | Multi | No | Low risk symptomatic patients |
| Winchester et al12 | Retrospective | Both | Academic | Single | No | Low risk asymptomatic patients |
| Lalude et al13 | Retrospective | Both | Academic | Single | No | Low pretest probability of CAD, ECG interpretable, and able to exercise |
| Singh et al14 | Retrospective | Both | Academic | Single | No | Pre-operative assessment |
| Khawaja et al36 | Retrospective | Both | Academic | Single | Yes | NR |
| Doukky et al20 | Prospective | Outpatient | Community | Multi | No | NR |
| Aldweib et al15 | Retrospective | Both | Academic | Single | No | Pre-operative assessment |
| Lin et al37 | Prospective | Outpatient | Community | Multi | Yes | Low risk asymptomatic patients |
| Moralidis et al38 | Prospective | Both | Academic | Multi | No | Pre-operative assessment |
| Soine et al39 | Retrospective | NR | Academic | Multi | No | NR |
| Nelson et al40 | Retrospective | Both | Academic | Multi | No | Asymptomatic patients < 2 years after PCI |
| Gholamrezanezhad et al41 | Prospective | NR | Community | Multi | No | NR |
| Gupta et al16 | Retrospective | Both | Community | Single | No | NR |
| Druz et al42 | Prospective | Both | Academic | Single | No | Low risk asymptomatic patients |
| Koh et al17 | Prospective | NR | Academic | Single | No | Pre-operative assessment |
| Carryer et al43 | Retrospective | Both | Academic | Single | No | Low risk asymptomatic patients |
| Hendel et al44 | Prospective | NR | Academic | Multi | No | Low risk asymptomatic patients |
| Mehta et al18 | Retrospective | NR | Academic | Single | No | Low risk symptomatic patients |
| Gibbons et al19 | Retrospective | Both | Academic | Single | No | Low risk asymptomatic patients |
CAD= coronary artery disease
ECG= electrocardiogram
NR= not reported
PCI= percutaneous coronary intervention
Primary outcomes
The relationship between inappropriate MPI and abnormal test results were reported by 8 studies reported the incidence of abnormal test results,10,12,17,18,20,34,40,41 while 6 studies described on myocardial ischemia.10,12,20,34,36,40 Individual study definitions for ischemia are supplied in supplemental Table 1. Inappropriate MPI studies were less likely to be abnormal 15.6% vs 42.0% (OR 0.41 95% CI 0.35–0.49, p<0.0001) compared to appropriate tests (Figure 2). Additionally, inappropriate MPI testing was less likely to demonstrate cardiac ischemia 6.1% vs 18.5 % (OR 0.40, 95% CI 0.24–0.67, p<0.0001) when compared to appropriate testing (Figure 3).
Figure 2.
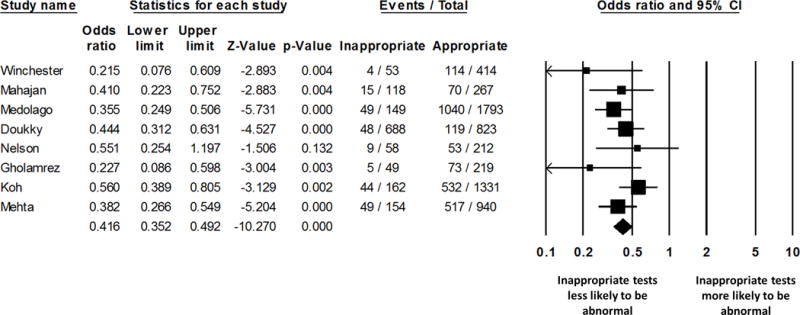
Summary plot for abnormal test results.
The relative size of the data markers indicates the weight of the sample size from each study.
CI = confidence interval
Figure 3.
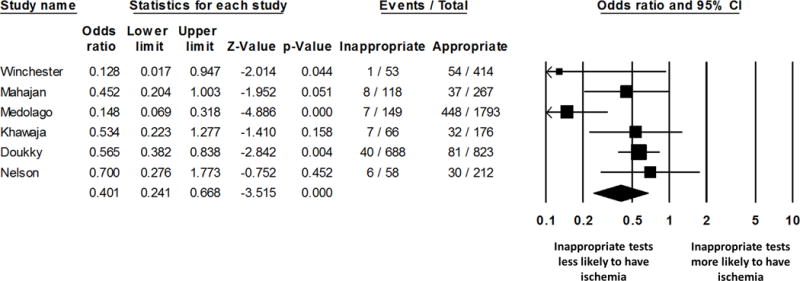
Summary plot for detection of cardiac ischemia.
The relative size of the data markers indicates the weight of the sample size from each study.
CI = confidence interval
Additional analyses
No significant difference was observed in the pattern of ordering inappropriate tests between cardiology and non-cardiology providers (OR 0.74, 95% CI 0.51–1.06, p=0.10) (Figure 4). No significant correlation was observed between the rate of inappropriate testing and the midpoint of the enrollment year (0.52%, 95% CI -1.16% to -2.20% per year, p=0.54) (Figure 5). Meta-analysis could not be performed for the risk of all-cause mortality, MI, the combined outcome of mortality or MI, cardiac catheterization, or revascularization due to the limited number of studies reporting these outcomes. In Table 3, we summarize the rate of all-cause mortality, MI, the combined outcome of mortality or MI, cardiac catheterization, and revascularization in the individual studies. The study by Doukky et al was both large and had a notably different point estimate for inappropriate MPI.20 To evaluate the impact of this study on our investigation, we excluded it in a sensitivity analysis. Doing this, the summary estimate of inappropriate testing was 14.0% (95% CI 12.1% to 16.2%) and estimates for the co-primary outcomes were not changed; (OR 0.41, 95% CI 0.33–0.50, p< 0.0001) for abnormal test results, and (OR 0.35, 95% CI 0.18–0.62, p=0.002) for ischemia.
Figure 4.
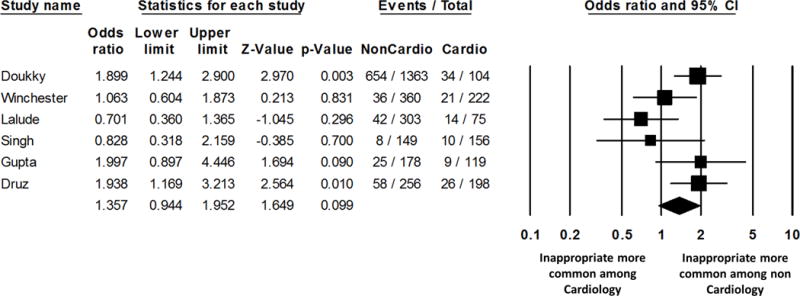
Summary plot for the rate of inappropriate testing according to provider.
The relative size of the data markers indicates the weight of the sample size from each study.
CI = confidence interval; MPI= myocardial perfusion imaging
Figure 5.
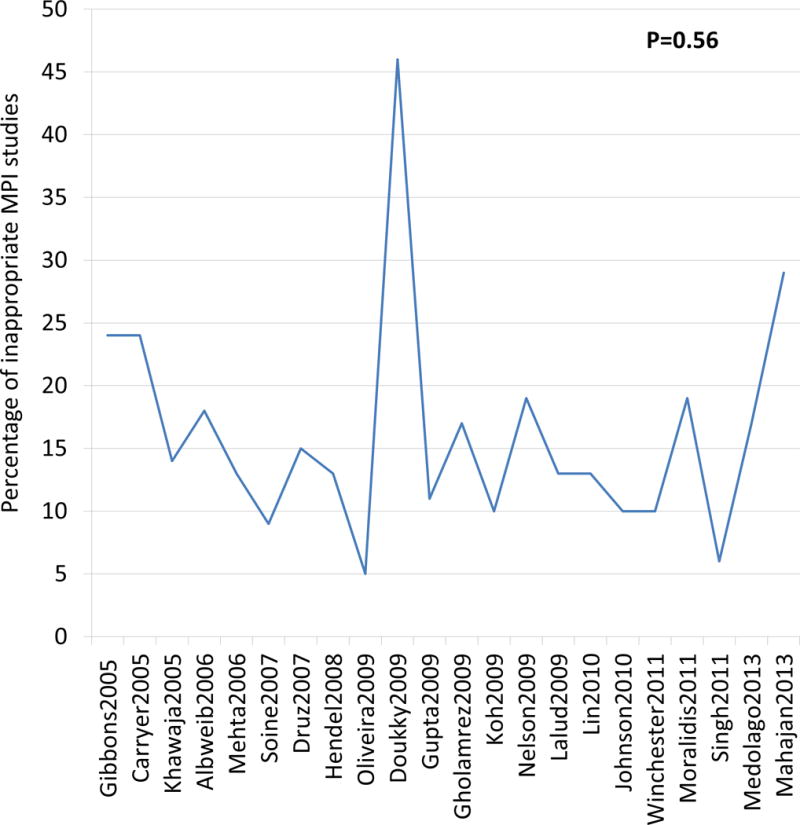
Rate of inappropriate studies over time
On the X-axis, studies were arranged chronologically based on the midpoint of patient enrollment for their study.
MPI= myocardial perfusion imaging
Table 3.
Cardiac events
| Study (ref#) | Appropriate, n | Event, n (%) | Inappropriate, n | Event, n (%) | Follow-up duration, m |
|---|---|---|---|---|---|
| All-cause mortality | |||||
| Winchester et al12 | 414 | 13 (3.1) | 53 | 0 (0) | 12 |
| Doukky et al20 | 823 | 29 (3.5) | 688 | 5 (0.7) | 27* |
| Aldweib et al15 | 685 | 68 (9.9) | 199 | 10 (5.0) | 100 |
| Koh et al17 | 106 | 3 (2.8) | 70 | 0 (0) | 3 |
|
| |||||
| Death or MI | |||||
| Winchester et al12 | 414 | 15 (3.6) | 53 | 1 (1.9) | 12 |
| Doukky et al20 | 823 | 37 (4.5) | 688 | 7 (1.0) | 27* |
|
| |||||
| MI | |||||
| Winchester et al12 | 414 | 3 (0.7) | 53 | 1 (1.9) | 12 |
| Koh et al17 | 106 | 6 (5.7) | 70 | 1 (1.4) | 3 |
|
| |||||
| Cardiac catheterization | |||||
| Mahajan et al10 | 267 | NR | 118 | 11 (9.3) | 4 |
| Winchester et al12 | 414 | 68 (16.4) | 53 | 1 (1.9) | 12 |
| Singh et al14 | 287 | NR | 18 | 6 (33.3) | 6 |
| Khawaja et al36 | 176 | 25 (14) | 66 | 2 (0.3) | 6 |
| Doukky et al20 | 823 | 72 (8.7) | 688 | 34 (4.9) | 27* |
|
| |||||
| Revascularization | |||||
| Mahajan et al10 | 267 | NR | 118 | 6 (5.1) | 4 |
| Winchester et al12 | 414 | 31 (7.5) | 53 | 1 (1.9) | 12 |
| Singh et al14 | 287 | NR | 18 | 3 (16.7) | 6 |
| Khawaja et al36 | 176 | NR | 66 | 0 (0) | 6 |
| Doukky et al20 | 823 | 40 (4.9) | 688 | 21 (3.1) | 27* |
| Druz et al42 | 359 | 13 (3.6) | 84 | NR | 12 |
mean is reported
MI= myocardial infarction, NR= not reported
Discussion
AUC are based on the premise that MPI testing for inappropriate indications will not benefit patients. In this meta-analysis of 22 studies including 23,443 patients, inappropriate MPI are consistently less likely to be abnormal or demonstrate ischemia as compared to appropriate studies. Using currently available data, we were unable to analyze relationship between inappropriate MPI and more substantial cardiovascular outcomes, such as catheterization, MI, and death. While the data for these outcomes were not sufficient to meta-analyze, individual studies demonstrated a substantial effect.20,21 Doukky et al showed a dramatic difference in cardiac events despite having a notably higher rate of inappropriate MPI as compared to other studies.20 Our analysis suggests that systems such as the AUC are valid strategies for focusing limited health care resources on those patients with the most to benefit from testing. It is important to mention that the 2013 AUC for stable ischemic heart disease now uses the term rarely appropriate as opposed to inappropriate”; 18 out of 80 indications are rated as “rarely appropriate”.45
Since the first AUC for MPI were published 10 years ago, a reasonable assumption is that growing awareness of recommendations about inappropriate testing might alter patterns of care. Although Fonseca et al analyzed the temporal trends in AUC for SPECT,23 our analysis included 7 additional studies.10,11,13,14,34–36 Using meta-regression, we analyzed our data for any change in the rate of inappropriate testing over time. If any change has occurred, the magnitude of change (0.52%, 95% CI -1.16% to -2.20 in our analysis). Larger scale real world data from programs such as FOCUS and ImageGuide™ may make it possible to ascertain such temporal trends in the future.46,47 We observed a wide range of rates of inappropriate MPI. In one study with the highest inappropriate rate, the patient population was based on multiple community practices, in contrast to the vast majority of the studies included in this analysis which were conducted in single-tertiary care centers. Differences in patient populations and behavior of ordering physicians may have contributed to this difference. In our sensitivity analysis excluding this study, our results did not change.20
Compared with non-cardiology providers, cardiology providers did not order significantly fewer inappropriate MPI in our analysis. The publications addressing this question have shown mixed results with some finding a difference,16,42 and other with no difference.12,24 Doukky et al were able to demonstrate that if a difference does exist, the likely explanation relates to the patient population being tested and not to an enhanced knowledge base by cardiology providers.24 The data were insufficient to make other comparisons about practice setting, such as geographic differences, US versus non-US investigations, academic versus community institutions, and inpatient versus outpatient setting. This last comparison may become more challenging as the next iteration of AUC shift away from modality based rating systems to multimodality ratings based on patient presentations.
Few studies on interventions to reduce inappropriate testing have been published. Some of the heterogeneous approaches attempted include education, peer review and feedback, and point-of-care decision support systems.19,29,35 Among these studies, education alone appeared insufficient to reduce inappropriate MPI while the addition of other system changes resulted in a decrease. These findings are in accord with recent investigations and systematic reviews, which demonstrate that decision support systems can reduce unnecessary imaging.48–50 Another strategy that has been considered is prior authorization, although a recent analysis on this strategy suggests no effect on the rate of inappropriate MPI among patients insured by private carriers as compared to Medicare which does not implement prior authorization measures.51
Meta-analysis of AUC is subject to a number of limitations. We relied on the AUC classification systems used by the original authors. Multiple studies have demonstrated that inter-rater and intra-rater variation is not negligible; however, we could not ascertain in which direction this might bias our results.19,30 One study showed the AUC inter-rater variation for non-cardiologists raters was modest compared to cardiologists (κ= 0.51).52 As noted previously, we could not comment on the risk of cardiac events due to the limited number of studies reporting these outcomes. Because we lacked access to patient level data, we could not analyze appropriateness of MPI based on patient characteristics such as sex, obesity, or diabetes since this has been described to increase the risk of bias.53 Publication bias is a potential limitation to meta-analyses. Finally, we included studies that used 2 different AUC (2005 & 2009), however; only one study utilizing the 2005 AUC was included in the analysis of the co-primary outcomes.18
New Knowledge Gained
Inappropriate MPI are less likely to yield abnormal results or determine myocardial ischemia. There has not been a significant reduction in the rates of inappropriate MPI testing with time. No differences were observed in the pattern of ordering inappropriate MPI between cardiology and non-cardiology providers.
Conclusions
We observed a wide range of inappropriate MPI rates, and estimate the overall rate among published studies to be 14.8%. Inappropriate MPI tests are consistently less likely to be abnormal or demonstrate ischemia than appropriate MPI, thus limiting their clinical utility. Currently available literature is insufficient to meta-analyze the relationship between death, MI, and inappropriate MPI. The rate of inappropriate MPI does not appear to have changed significantly over the time.
Supplementary Material
Acknowledgments
Funding source: This work was partially supported by NIH grant 1UL1TR000064 from the National Center for Advancing Translational Sciences
Abbreviations
- ACC
American College of Cardiology
- AUC
appropriate use criteria
- CI
confidence interval
- MI
myocardial infarction
- MPI
myocardial perfusion imaging
- MOOSE
Meta-analysis Of Observational Studies in Epidemiology
- OR
odds ratio
- PET
positron emission tomography
- SPECT
single-photon emission computed tomography
Footnotes
Disclosure: None
References
- 1.Salerno M, Beller GA. Noninvasive assessment of myocardial perfusion. Circ Cardiovasc Imaging. 2009;2:412–24. doi: 10.1161/CIRCIMAGING.109.854893. [DOI] [PubMed] [Google Scholar]
- 2.Loong CY, Anagnostopoulos C. Diagnosis of coronary artery disease by radionuclide myocardial perfusion imaging. Heart. 2004;90(Suppl 5):v2–9. doi: 10.1136/hrt.2003.013581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levin DC, Rao VM, Parker L, Frangos AJ, Intenzo CM. Recent payment and utilization trends in radionuclide myocardial perfusion imaging: comparison between self-referral and referral to radiologists. J Am Coll Radiol. 2009;6:437–41. doi: 10.1016/j.jacr.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–9. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McNulty EJ, Hung Y, Almers LM, Go AS, Yeh RW. Population Trends From 2000–2011 in Nuclear Myocardial Perfusion Imaging Use. JAMA. 2014;311:1248–9. doi: 10.1001/jama.2014.472. [DOI] [PubMed] [Google Scholar]
- 6.Hendel RC. Utilization management of cardiovascular imaging: pre-certification and appropriateness. JACC Cardiovasc Imaging. 2008;1:241–8. doi: 10.1016/j.jcmg.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Iglehart JK. The new era of medical imaging—Progress and pitfalls. N Engl J Med. 2009;360:1030–7. doi: 10.1056/NEJMhpr061219. [DOI] [PubMed] [Google Scholar]
- 8.Brindis RG, Douglas PS, Hendel RC, Peterson ED, Wolk MJ, Allen JM, et al. ACCF/ASNC appropriateness criteria for single-photon emission computed tomography myocardial perfusion imaging (SPECT MPI): a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group and the American Society of Nuclear Cardiology endorsed by the American Heart Association. J Am Coll Cardiol. 2005;46:1587–605. doi: 10.1016/j.jacc.2005.08.029. [DOI] [PubMed] [Google Scholar]
- 9.Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119:e561–87. doi: 10.1161/CIRCULATIONAHA.109.192519. [DOI] [PubMed] [Google Scholar]
- 10.Mahajan A, Bal S, Hahn H. Myocardial perfusion imaging determination using an appropriate use smartphone application. J Nucl Cardiol. 2015;22:66–71. doi: 10.1007/s12350-014-9995-0. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira AD, Rezende MF, Corrêa R, Mousinho R, Azevedo JC, Miranda SM, et al. Applicability of the Appropriate use Criteria for Myocardial Perfusion Scintigraphy. Arq Bras Cardiol. 2014;103:375–81. doi: 10.5935/abc.20140140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winchester DE, Hymas J, Meral R, Nguyen D, Dusaj R, Shaw LJ, et al. Clinician-dependent variations in inappropriate use of myocardial perfusion imaging: training, specialty, and location. J Nucl Cardiol. 2014;21:598–604. doi: 10.1007/s12350-014-9887-3. [DOI] [PubMed] [Google Scholar]
- 13.Lalude OO, Gutarra MF, Pollono EN, Lee S, Tarwater PM. Inappropriate utilization of SPECT myocardial perfusion imaging on the USA-Mexico border. J Nucl Cardiol. 2014;21:544–52. doi: 10.1007/s12350-014-9881-9. [DOI] [PubMed] [Google Scholar]
- 14.Singh M, Babayan Z, Harjai KJ, Dedhia P, Sattur S, Jagasia DH. Utilization patterns of single-photon emission cardiac tomography myocardial perfusion imaging studies in a rural tertiary care setting. Clin Cardiol. 2014;37:67–72. doi: 10.1002/clc.22240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aldweib N, Negishi K, Seicean S, Jaber WA, Hachamovitch R, Cerqueira M, et al. Appropriate test selection for single-photon emission computed tomography imaging: association with clinical risk, posttest management, and outcomes. Am Heart J. 2013;166:581–8. doi: 10.1016/j.ahj.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Gupta A, Tsiaras SV, Dunsiger SI, Tilkemeier PL. Gender disparity and the appropriateness of myocardial perfusion imaging. J Nucl Cardiol. 2011;18:588–94. doi: 10.1007/s12350-011-9368-x. [DOI] [PubMed] [Google Scholar]
- 17.Koh AS, Flores JL, Keng FY, Tan RS, Chua TS. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging in an Asian tertiary cardiac center. J Nucl Cardiol. 2011;18:324–30. doi: 10.1007/s12350-010-9317-0. [DOI] [PubMed] [Google Scholar]
- 18.Mehta R, Ward RP, Chandra S, Agarwal R, Williams KA. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging. J Nucl Cardiol. 2008;15:337–44. doi: 10.1016/j.nuclcard.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Gibbons RJ, Miller TD, Hodge D, Urban L, Araoz PA, Pellikka P, et al. Application of appropriateness criteria to stress single-photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol. 2008;51:1283–9. doi: 10.1016/j.jacc.2007.10.064. [DOI] [PubMed] [Google Scholar]
- 20.Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation. 2013;128:1634–43. doi: 10.1161/CIRCULATIONAHA.113.002744. [DOI] [PubMed] [Google Scholar]
- 21.Winchester DE, Chauffe RJ, Meral R, Nguyen D, Ryals S, Dusaj R, et al. Clinical utility of inappropriate positron emission tomography myocardial perfusion imaging: Test results and cardiovascular events. J Nucl Cardiol. 2015;22:9–15. doi: 10.1007/s12350-014-9925-1. [DOI] [PubMed] [Google Scholar]
- 22.Koh AS, Flores JL, Keng FY, Tan RS, Chua TS. Correlation between clinical outcomes and appropriateness grading for referral to myocardial perfusion imaging for preoperative evaluation prior to non-cardiac surgery. J Nucl Cardiol. 2012;19:277–84. doi: 10.1007/s12350-011-9462-0. [DOI] [PubMed] [Google Scholar]
- 23.Fonseca R, Negishi K, Otahal P, Marwick TH. Temporal changes in appropriateness of cardiac imaging. J Am Coll Cardiol. 2015;65:763–73. doi: 10.1016/j.jacc.2014.11.057. [DOI] [PubMed] [Google Scholar]
- 24.Doukky R, Hayes K, Frogge N. Are cardiologists truly better at appropriately selecting patients for stress myocardial perfusion imaging? Int J Cardiol. 2014;176:285–6. doi: 10.1016/j.ijcard.2014.06.087. [DOI] [PubMed] [Google Scholar]
- 25.Winchester DE, Meral R, Ryals S, Beyth RJ, Shaw LJ. Appropriate use of myocardial perfusion imaging in a veteran population: profit motives and professional liability concerns. JAMA Intern Med. 2013;173:1381–3. doi: 10.1001/jamainternmed.2013.953. [DOI] [PubMed] [Google Scholar]
- 26.Gibbons RJ, Askew JW, Hodge D, Kaping B, Carryer DJ, Miller T. Appropriate use criteria for stress single-photon emission computed tomography sestamibi studies: a quality improvement project. Circulation. 2011;123:499–503. doi: 10.1161/CIRCULATIONAHA.110.975995. [DOI] [PubMed] [Google Scholar]
- 27.Gibbons RJ, Askew JW, Hodge D, Miller TD. Temporal trends in compliance with appropriateness criteria for stress single-photon emission computed tomography sestamibi studies in an academic medical center. Am Heart J. 2010;159:484–9. doi: 10.1016/j.ahj.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Gertz ZM, O’Donnell W, Raina A, Litwack AJ, Balderston JR, Goldberg LR. Application of appropriate use criteria to cardiac stress testing in the hospital setting: limitations of the criteria and areas for improved practice. Clin Cardiol. 2015;38:8–12. doi: 10.1002/clc.22340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin FY, Rosenbaum LR, Gebow D, Kim RJ, Wolk MJ, Patel MR, et al. Cardiologist concordance with the American College of Cardiology appropriate use criteria for cardiac testing in patients with coronary artery disease. Am J Cardiol. 2012;110:337–44. doi: 10.1016/j.amjcard.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 30.McCully RB, Pellikka PA, Hodge DO, Araoz PA, Miller TD, Gibbons RJ. Applicability of appropriateness criteria for stress imaging: similarities and differences between stress echocardiography and single-photon emission computed tomography myocardial perfusion imaging criteria. Circ Cardiovasc Imaging. 2009;2:213–8. doi: 10.1161/CIRCIMAGING.108.798082. [DOI] [PubMed] [Google Scholar]
- 31.Levin DC, Intenzo CM, Rao VM, Frangos AJ, Parker L, Sunshine JH. Comparison of recent utilization trends in radionuclide myocardial perfusion imaging among radiologists and cardiologists. J Am Coll Radiol. 2005;2:821–4. doi: 10.1016/j.jacr.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 32.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 33.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 34.Medolago G, Marcassa C, Alkraisheh A, Campini R, Ghilardi A, Giubbini R. Applicability of the appropriate use criteria for SPECT myocardial perfusion imaging in Italy: preliminary results. Eur J Nucl Med Mol Imaging. 2014;41:1695–700. doi: 10.1007/s00259-014-2743-5. [DOI] [PubMed] [Google Scholar]
- 35.Johnson TV, Rose GA, Fenner DJ, Rozario NL. Improving appropriate use of echocardiography and single-photon emission computed tomographic myocardial perfusion imaging: a continuous quality improvement initiative. J Am Soc Echocardiogr. 2014;27:749–57. doi: 10.1016/j.echo.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Khawaja FJ, Jouni H, Miller TD, Hodge DO, Gibbons RJ. Downstream clinical implications of abnormal myocardial perfusion single-photon emission computed tomography based on appropriate use criteria. J Nucl Cardiol. 2013;20:1041–8. doi: 10.1007/s12350-013-9794-z. [DOI] [PubMed] [Google Scholar]
- 37.Lin FY, Dunning AM, Narula J, Shaw LJ, Gransar H, Berman DS, et al. Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. J Am Coll Cardiol. 2013;62:308–16. doi: 10.1016/j.jacc.2013.04.059. [DOI] [PubMed] [Google Scholar]
- 38.Moralidis E, Papadimitriou N, Stathaki M, Xourgia X, Spyridonidis T, Fotopoulos A, et al. A multicenter evaluation of the appropriate use of single-photon emission tomography myocardial perfusion imaging in Greece. J Nucl Cardiol. 2013;20:275–83. doi: 10.1007/s12350-012-9664-0. [DOI] [PubMed] [Google Scholar]
- 39.Soine LA, Cunningham SL, Motzer SA, Inoue LY, Caldwell JH. Application of appropriate use criteria for stress myocardial perfusion imaging at two academic medical centers: compliance and association with image findings. J Am Acad Nurse Pract. 2012;24:200–8. doi: 10.1111/j.1745-7599.2011.00679.x. [DOI] [PubMed] [Google Scholar]
- 40.Nelson KH, Willens HJ, Hendel RC. Utilization of radionuclide myocardial perfusion imaging in two health care systems: assessment with the 2009 ACCF/ASNC/AHA appropriateness use criteria. J Nucl Cardiol. 2012;19:37–42. doi: 10.1007/s12350-011-9467-8. [DOI] [PubMed] [Google Scholar]
- 41.Gholamrezanezhad A, Shirafkan A, Mirpour S, Rayatnavaz M, Alborzi A, Mogharrabi M, et al. Appropriateness of referrals for single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) in a developing community: a comparison between 2005 and 2009 versions of ACCF/ASNC appropriateness criteria. J Nucl Cardiol. 2011;18:1044–52. doi: 10.1007/s12350-011-9419-3. [DOI] [PubMed] [Google Scholar]
- 42.Druz RS, Phillips LM, Sharifova G. Clinical evaluation of the appropriateness use criteria for single-photon emission-computed tomography: differences by patient population, physician specialty, and patient outcomes. ISRN Cardiol. 2011;2011:798318. doi: 10.5402/2011/798318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carryer DJ, Hodge DO, Miller TD, Askew JW, Gibbons RJ. Application of appropriateness criteria to stress single photon emission computed tomography sestamibi studies: a comparison of the 2009 revised appropriateness criteria to the 2005 original criteria. Am Heart J. 2010;160:244–9. doi: 10.1016/j.ahj.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 44.Hendel RC, Cerqueira M, Douglas PS, Caruth KC, Allen JM, Jensen NC, et al. A multicenter assessment of the use of single-photon emission computed tomography myocardial perfusion imaging with appropriateness criteria. J Am Coll Cardiol. 2010;55:156–62. doi: 10.1016/j.jacc.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 45.Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Nucl Cardiol. 2014;21:192–220. doi: 10.1007/s12350-013-9841-9. [DOI] [PubMed] [Google Scholar]
- 46.FOCUS Initiative. http://www.cardiosource.org/Science-And-Quality/Quality-Programs/Imaging-in-FOCUS/. Accessed March 4, 2015.
- 47.Tilkemeier P, Wang TY, Lytle BL, Denton EA. ASNC ImageGuide™: cardiovascular imaging data registry. J Nucl Cardiol. 2013;20:1186–7. doi: 10.1007/s12350-013-9789-9. [DOI] [PubMed] [Google Scholar]
- 48.Dunne RM, Ip IK, Abbett S, Gershanik EF, Raja AS, Hunsaker A, et al. Effect of evidence-based clinical decision support on the use and yield of CT pulmonary angiographic imaging in hospitalized patients. Radiology. 2015:141208. doi: 10.1148/radiol.15141208. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moriarity AK, Klochko C, O’Brien M, Halabi S. The effect of clinical decision support for advanced inpatient imaging. J Am Coll Radiol. 2015;12:358–63. doi: 10.1016/j.jacr.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 50.Jenkins HJ, Hancock MJ, French SD, Maher CG, Engel RM, Magnussen JS. Effectiveness of interventions designed to reduce the use of imaging for low-back pain: a systematic review. CMAJ. 2015;187:401–408. doi: 10.1503/cmaj.141183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doukky R, Hayes K, Frogge N, Nazir NT, Collado FM, Williams KA. Impact of insurance carrier, prior authorization and socioeconomic status on appropriate use of SPECT myocardial perfusion imaging in private community-based office practice. Clin Cardiol. 2015 doi: 10.1002/clc.22382. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ye S, Rabbani LE, Kelly CR, Kelly MR, Lewis M, Paz Y, et al. Can physicians identify inappropriate nuclear stress tests? An examination of inter-rater reliability for the 2009 appropriate use criteria for radionuclide imaging. Circ Cardiovasc Qual Outcomes. 2015;8:23–9. doi: 10.1161/CIRCOUTCOMES.114.001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hernán MA, Clayton D, Keiding N. The Simpson’s paradox unraveled. Int J Epidemiol. 2011;40:780–5. doi: 10.1093/ije/dyr041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


