Abstract
Delayed suprachoroidal hemorrhage (DSCH) is a rare but devastating complication of trabeculectomy, usually resulting in a poor visual prognosis. The typical presentation of DSCH includes acute visual loss, high intraocular pressure, a shallow anterior chamber, and choroidal elevation. We report a patient with hypertension who had DSCH following trabeculectomy, with an unusual presenting picture of a large blood clot hanging in a deep anterior chamber. Anterior chamber irrigation and choroidal taps were performed immediately. The intraocular pressure was soon controlled, and the visual acuity returned to 20/25 in 6 months.
Keywords: Delayed suprachoroidal hemorrhage, Hyphema, Intraocular pressure, Trabeculectomy
1. Introduction
Suprachoroidal hemorrhage is a rare but devastating complication which may occur in any type of intraocular surgery, especially when accompanied by a fluctuation in intraocular pressure (IOP). A suprachoroidal hemorrhage is called an expulsive hemorrhage when it occurs intraoperatively and the ocular contents prolapse through the wound. If it occurs postoperatively, it is called a delayed suprachoroidal hemorrhage (DSCH). Suprachoroidal hemorrhage usually presents with visual loss, a high IOP, shallow anterior chamber, and dark red dome-shaped or even appositional “kissing” choroidal elevation. Here we report a case of DSCH following trabeculectomy, with a presenting picture of a large blood clot hanging in the anterior chamber. Our management led to satisfactory results.
2. Case report
A 72-year-old man received a trabeculectomy in the right eye at another hospital. On the 1st postoperative day, a subtotal hyphema was noted, which was refractory to anterior chamber irrigation, and led to a refractory high IOP (up to 60 mm Hg under topical travoprost, timolol, and brimonidine, and oral acetazolamide). He was referred to our hospital on the 5th postoperative day. Syncope with temporary cardiac arrest occurred that night, and an electrocardiogram showed right branch bundle block with multiple premature ventricular complexes. Hypertension up to 153/96 mm Hg was noted and nifedipine was prescribed. Timolol was then discontinued. An anterior chamber paracentesis was performed daily to lower the IOP and to remove part of the hyphema. On the 13th postoperative day, anterior chamber irrigation and a pars plana vitrectomy were performed to remove the hyphema and the very dense vitreous hemorrhage. Abundant pigment on the posterior capsule and anterior hyaloid face was noted intraoperatively. On the 18th postoperative day, the patient underwent a trabeculectomy with mitomycin-C. No hyphema occurred this time and the IOP was 13 mm Hg postoperatively. The visual acuity returned to 20/25 in 3 months.
Two years later, a fornix-based trabeculectomy with mitomycin-C was performed smoothly in the left eye due to progressive visual field loss. On the 1st postoperative day, the patient had an IOP of 12 mm Hg with a diffuse bleb, a deep anterior chamber with no hyphema, and a patent peripheral iridectomy. However, he came to our emergency room with sudden painful loss of vision on the 3rd postoperative day. On examination, his visual acuity was limited to light perception, and the IOP was 49 mm Hg in his left eye. Slitlamp examination showed a round blood clot with an appearance like a nested cocoon hanging in the anterior chamber and obscuring the pupil (Fig. 1). The patient was not taking anticoagulants or antiplatelet medications. Immediate aspiration of the blood clot and irrigation of the anterior chamber were performed. The blood clot in the anterior chamber was found connected to a suprachoroidal hemorrhage. Two circumferential sclerotomies 4 mm from the limbus and 3 mm in length were performed in the superior nasal and superior temporal quadrants. The suprachoroidal hemorrhage was then drained from the two sclerotomies with constant irrigation pressure from the anterior chamber. His ocular pain subsided the next day. The IOP was 20 mm Hg. A B-scan showed mild residual suprachoroidal hemorrhage at the very peripheral area (Fig. 2). After 6 months, his visual acuity returned to 20/25. The IOP was 16 mm Hg.
Fig. 1.

Three days after trabeculectomy, this patient had a sudden painful loss of vision. A slit lamp examination reveals a large blood clot with an appearance like a nested cocoon hanging in the anterior chamber and obscuring the pupil.
Fig. 2.
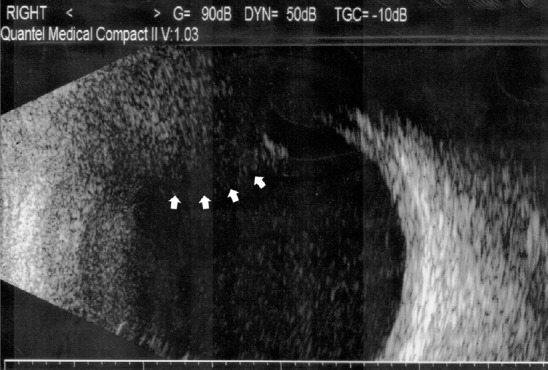
On the day after choroidal tap and anterior chamber irrigation, a B-scan image shows residual hemorrhage in the superior-peripheral area (arrows).
3. Discussion
DSCH typically occurs after uncomplicated glaucoma filtration surgery. The incidence of DSCH after glaucoma filtration procedures varies from 1.6% to 6.2% [1,2]. The risk factors include systemic conditions such as advanced age, atherosclerosis, hypertension, ischemic heart disease, and anticoagulant usage, and ocular conditions including myopia, aphakia, a high preoperative IOP, a drop in IOP, postoperative hypotony, and tube shunt implantation [3,4,5]. Our patient was 72 years old and was taking clopidogrel for ischemic heart disease before the second operation. Hyphema and vitreous hemorrhage occurred after a trabeculectomy in the right eye, and DSCH occurred after a trabeculectomy in the left eye. He had pseudophakia in both eyes, and there was no postoperative hypotony. His systemic risk factors might have played a major role in the development of DSCH.
DSCH usually presents with a sudden onset of painful visual loss, an elevated IOP, a shallow anterior chamber, and peripheral large choroidal elevations with dark coloration. However, instead of a shallow anterior chamber, our patient had a deep anterior chamber with an overhanging cocoon-like blood clot, which has never been described before in literature. Our initial impression was ordinary bleeding from the peripheral iridectomy. After the blood clot was found connected to the suprachoroidal hemorrhage, DSCH was diagnosed as the underlying etiology. A suprachoroidal hemorrhage through the angle to the anterior chamber transferred the pressure to the anterior chamber. The iris-lens diaphragm was therefore not pushed forward, and the anterior chamber depth was maintained. The overall IOP was still high. The connection to the suprachoroidal hemorrhage also explained why and how the large blood clot was hanging from the superior angle.
The timing of surgical intervention and the optimal procedure remain unclear. A wait of 7 days to 14 days to allow liquefaction of the blood clot is usually recommended [6,7]. But this delay in intervention may increase inflammation, leading to irreversible damage such as retinal adhesions or cyclitic membrane formation. This would require complex vitreoretinal surgery, and thus a poor final prognosis [8]. Early surgical intervention after the diagnosis of DSCH has been suggested [9,10]. Pakravan et al [9] recommended an immediate choroidal tap and anterior chamber reformation after diagnosis of DSCH. They suggested two scleral incisions 4 mm in length and a 1 mm sclerectomy in both inferior quadrants. After massage to remove the serosanguinous fluid, they created a para-centesis to reform the anterior chamber with a balanced salt solution. We also performed surgical drainage in our patient immediately after the diagnosis of DSCH. However, we performed scleral incisions in two superior quadrants, instead of inferior quadrants. We believed that the DSCH would be located more superiorly in this patient because the large blood clot in the anterior chamber was connected to the DSCH at the 12 o’clock area. We also did not massage the fluid in our patient so as not to stretch or distort the weakened, previously ruptured vessels and induce secondary hemorrhage. Fortunately, the blood was evacuated smoothly. The IOP returned to normal limits the next day and the visual acuity returned to 20/25 in 6 months.
In conclusion, we report a blood clot hanging in a deep anterior chamber as an unusual presentation of DSCH after trabeculectomy. Immediate choroidal tap and anterior chamber irrigation without massage led to a satisfactory visual result.
Footnotes
Conflict of interest: none.
References
- [1].Givens K, Shields MB. Suprachoroidal hemorrhage after glaucoma filtering surgery. Am J Ophthalmol. 1987;15:689–94. doi: 10.1016/s0002-9394(14)74331-4. [DOI] [PubMed] [Google Scholar]
- [2].Paysse E, Lee PP, Lloyd MA, Sidoti PA, Fellenbaum PS, Baerveldt G, et al. Suprachoroidal hemorrhage after Molteno implantation. J Glaucoma. 1996;5:170–5. [PubMed] [Google Scholar]
- [3].Chu TG, Green RL. Suprachoroidal hemorrhage. SurvOphthalmol. 1999;43:471–86. doi: 10.1016/s0039-6257(99)00037-5. [DOI] [PubMed] [Google Scholar]
- [4].Tuli SS, WuDunn D, Ciulla TA, Cantor LB. Delayed suprachoroidal hemorrhage after glaucoma filtration procedures. Ophthalmology. 2001;108:1808–11. doi: 10.1016/s0161-6420(01)00763-1. [DOI] [PubMed] [Google Scholar]
- [5].Jeganathan VS, Ghosh S, Ruddle JB, Gupta V, Coote MA, Crowston JG. Risk factors for delayed suprachoroidal hemorrhage following glaucoma surgery. Br J Ophthalmol. 2008;92:1393–6. doi: 10.1136/bjo.2008.141689. [DOI] [PubMed] [Google Scholar]
- [6].Stamper RL, Lieberman MF, Drake MV. Becker-Shaffer's diagnosis and therapy of the glaucomas. USA: Mosby; 2009. pp. 514–5. [Google Scholar]
- [7].Allingham RR, Damji KF, Freedman SF. Shield textbook of glaucoma. Philadelphia: Lippincott Williams & Wilkins; 2011. pp. 504–5. [Google Scholar]
- [8].Weinberg DV, Rosenberg LI. Retina to retina adhesions following suprachoroidal hemorrhage. Br J Ophthalmol. 1996;80:674. doi: 10.1136/bjo.80.7.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pakravan M, Yazdani S, Afroozifar M, Kouhestani N, Ghassami M, Shahshahan M. An alternative approach for management of delayed suprachoroidal hemorrhage after glaucoma procedures. J Glaucoma. 2014;23:37–40. doi: 10.1097/IJG.0b013e31825afb25. [DOI] [PubMed] [Google Scholar]
- [10].Jin W, Xing Y, Xu Y, Wang W, Yang A. Management of delayed suprachoriodal haemorrhage after intraocular surgery and trauma. Graefes Arch Clin Exp Ophthalmol. 2014;252:1189–93. doi: 10.1007/s00417-013-2550-x. [DOI] [PubMed] [Google Scholar]


