Abstract
Objective:
This study aimed to investigate the characteristics and outcomes of patients with emergency department (ED) revisits within 72 hours and subsequent admission to the intensive care unit (ICU).
Materials and Methods:
The medical records of all adult patients revisiting the ED of a single tertiary referral medical center with ICU admissions between January 2012 and September 2014 were reviewed in terms of patient characteristics, clinical manifestations, diagnoses, triage according to the Taiwan Triage and Acuity Scale, causes of revisits, and mortality.
Results:
The majority of the 51 patients reviewed were male (64.7%). Their mean age was 62.9 ± 14.9 years. Most patients visited the ED during the evening shift (51%) and were categorized into triage Level III (76.5%) during their first ED visit. The causes of revisits were doctor-related (21/51, 41.1%), illness-related (18/51, 35.3%), and patient-related (12/51, 23.5%). Disease categories included the neurological (23.5%), digestive (23.5%), and cardiovascular systems (21.6%). Abdominal pain and vertigo/dizziness were the two most common initial manifestations. The mortality rate was 27.5%. Malignancy and hepatic diseases were the two most common underlying medical conditions for nonsurvivors. In addition, patients initially presenting to the ED with lower triage scores (III & IV) had a higher mortality rate than those with higher scores (I & II).
Conclusion:
Most of the patients who revisited the ED within 72 hours and were subsequently admitted to the ICU visited the ED during the evening shift and were categorized into triage Level III on their first visit. The most common chief complaint at the first visit was abdominal pain. The most common cause of revisits with ICU admission was doctor-related, while the most common underlying disease was hypertension. Significantly higher mortality was observed after ED revisits in patients with lower triage scores with underlying malignancy and liver cirrhosis.
Keywords: Emergency, ICU admission, Revisit
1. Introduction
The occurrence of unscheduled return visits to the emergency department (ED) is a widely known indicator of the quality of patient care, guiding the implementation of appropriate improvement strategies [1,2,3,4,5,6,7]. It is defined as a return ED visit within 72 hours at which the patient presents with the same chief complaint [5,6,7,8,9]. Previous studies have demonstrated a rate of ED revisits of approximately 3%, ranging from 1.9% to 5.47% [1,2,3,4,5,6,7,10]. These patients were considered to have a higher rate of morbidity and mortality than other ED patients, and analysis of the causes could help to establish guidelines to reinforce the quality of health care [2,7].
Although unscheduled return visits to the ED are regarded as an important quality indicator of patient safety, as well as the system responsible for the delivery of emergency care, the reasons for return visits to the ED are complicated and multifactorial. The type of disease, local culture, and psychosocial, medical, and health system issues are all involved. However, one retrospective cross-sectional study demonstrated the utilization of fewer resources, without higher hospital admission or mortality rates for patients with ED revisits within 72 hours, compared with first-time ED visitors. The authors suggested a more refined and reliable indicator, such as ED revisit-admission within 72 hours, be used to assess health care quality and patient safety [11]. A few studies have evaluated the causes of revisits, the characteristics of patients who return to the ED within 72 hours, and prognostic predictors of unplanned hospital admission within 72 hours after ED discharge in various time frames and hospital settings [5,6,7,12,13,14]. These studies demonstrated that 22% to 48% of patients with return visits were admitted to ordinary wards and 4.2% to 6.1% to the intensive care unit (ICU) [6,7,8,13,15,16].
Critical diseases may be overlooked because of initial atypical or trivial presentations, which may result in diagnostic or treatment delay or early release of patients from the ED, resulting in ED revisits shortly after discharge [17,18,19,20]. A revisit with ICU admission is a serious adverse event in ED management, therefore it is important to understand and analyze the underlying causes in order to improve patient safety [21,22]. Although previous studies have shown that the overall mortality rate ranged from 8% to 19% in ICUs in the United States [23,24,25] and was approximately 20.2% in Taiwan [26], the mortality rates of patients with ED visits and ICU admission have not been extensively investigated. To our knowledge, there have been few studies of unplanned revisits and subsequent ICU admission [10,27]. One retrospective single hospital study evaluated the characteristics and prognostic predictors of the patient subpopulation and showed a strong association with medical errors [27]. To further explore the precise characteristics of adult revisit patients with ICU admission, we conducted a study primarily aimed at identifying the causes of revisits, clinical manifestations, and outcomes of adult patients with ICU admission within 72 hours after ED discharge. The secondary aim was to evaluate the in-hospital mortality rate in this patient subpopulation.
2. Materials and methods
2.1. Study design
This study was conducted at a 1251-bed, tertiary referral hospital in southern Taiwan which receives approximately 66,000 emergency visits per year. From January 1, 2012 to September 30, 2014, the electronic medical records of all adult patients who revisited the ED within 72 hours after initial discharge with subsequent admission to the ICU were extracted from our ED administrative database and retrospectively reviewed in terms of patient information, arrival and discharge time, underlying diseases, triage level according to the Taiwan Triage and Acuity Scale, and disease category. The causes and timing of initial ED visits and revisits, characteristics of presentations, and patient outcomes including their in-hospital mortality rate were also analyzed and compared. The Institutional Review Board of our institution approved the protocol of the present study. The study was a retrospective review of the hospital database and all patients were unidentifiable before the study, therefore the Institutional Review Board waived the need for informed consent.
2.2. Study population
All adult patients aged 18 years or older fitting the criteria of ED revisit within 72 hours with subsequent admission to the ICU were included in the current study. Pediatric patients were excluded from the present study because the causes and characteristics of their return visits to the ED are different to those of adult and elderly patients [28,29]. In addition, patients who revisited the ED within 72 hours of initial discharge for unrelated medical problems were also excluded (Fig. 1).
Fig. 1.
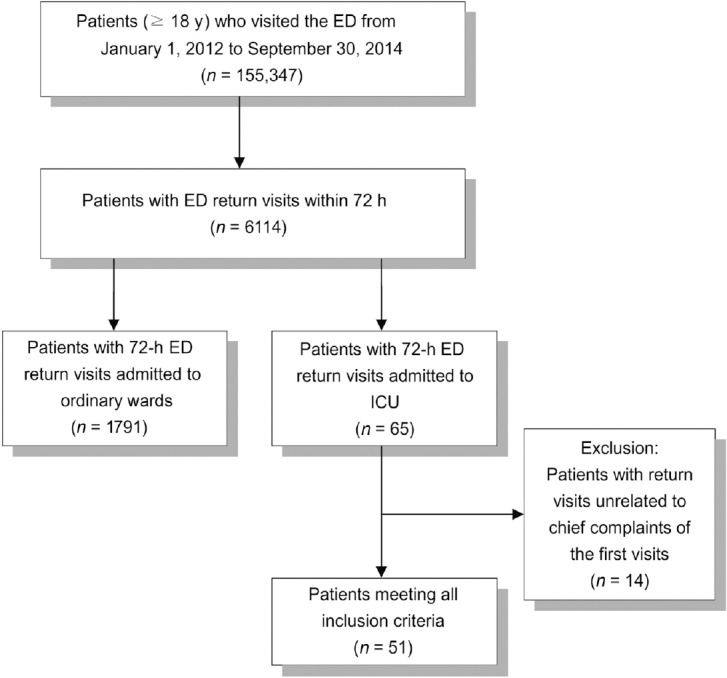
Protocol for patient recruitment.
During the study period, a total of 155,347 adult patients visited the ED, of whom 6114 (4%) made a return visit within 72 hours (Fig. 1). Among these 6114 patients, 1856 (30%) were admitted to the hospital; 1791 (29%) to the wards and 65 (1%) to the ICU. The mean age of all 1856 patients was 55 ± 24.1 years and 59% were male. Of the 65 patients subsequently admitted to the ICU, 51 fulfilled the enrollment criteria and were recruited for the present study. The remaining 14 made unrelated revisits and were excluded. The mean age of these 51 patients was 62.9 ± 14.9 years (range, 26–89 years) and 64.7% were male.
2.3. Definitions
Patients were categorized in terms of disease severity according to the Taiwan Triage and Acuity Scale which was modified from the Canadian Triage and Acuity Scale and officially adopted by the Taiwanese emergency health care system in 2010: Level I, resuscitation; Level II, emergency; Level III, urgent; Level IV, less urgent; and Level V, nonurgent. Additionally, the present study classified the nature of the return visits in accordance with the causes based on the method proposed in a previous study by Pierce et al [2] with minor modifications. Briefly, return visits were divided into three groups: doctor-related (i.e., diagnostic errors and inadequate treatment); illness-related (i.e., disease progression, recurrent disease process, and expected medical complications); and patient-related (i.e., discharge against medical advice and noncompliance). Two senior emergency physicians then determined the classification for each return visit. If the classifications of the two physicians were inconsistent, the final decision was made by a third expert. If more than one cause was identified, the doctor-related cause took priority over all other causes and the illness-related cause took priority over the patient-related cause.
Patients were divided into survivors and nonsurvivors for further comparisons.
2.4. Statistical analysis
All analyses were performed using SPSS (Version 15.0, Chicago, IL, USA). A two-sided p < 0.05 was considered to be significant. Differences between survivors and nonsurvivors with ED return visits and admission to the ICU were compared using Fisher's exact test for categorical variables.
3. Results
3.1. Characteristics of patients revisiting the ED with subsequent ICU admission
Most of the 51 patients visited the ED during the evening shift (51%) and were categorized into triage Level III (76.5%) in their first ED visit. The causes of revisits with ICU admission were judged to be doctor-related (21/51, 41.1%), illness-related (18/51, 35.3%), or patient-related (12/51, 23.5%), while the common underlying diseases were hypertension (39.2%), diabetes mellitus (27.5%), and malignancy (27.5%) (Table 1). The neurological (23.5%), digestive (23.5%), and cardiovascular systems (21.6%) were most commonly involved.
Table 1.
Demographic factors and characteristics of patients returning to the ED within 72 hours with admission to the ICU (n = 51).
| Variables | n | % | |
|---|---|---|---|
| Sex | Male | 33 | 64.7 |
| Female | 18 | 35.7 | |
| Age (y) | ≥60 | 31 | 60.8 |
| <60 | 20 | 39.2 | |
| Shift | Day | 12 | 23.5 |
| Evening | 26 | 51.0 | |
| Night | 13 | 25.5 | |
| First triage | Level I | 2 | 3.9 |
| Level II | 8 | 15.7 | |
| Level III | 39 | 76.5 | |
| Level IV | 2 | 3.9 | |
| Return visit justification | Doctor-related | 21 | 41.2 |
| Illness-related | 18 | 35.3 | |
| Patient-related | 12 | 23.5 | |
| Diagnostic category | Neurological system | 12 | 23.5 |
| Digestive system | 12 | 23.5 | |
| Cardiovascular system | 11 | 21.6 | |
| Respiratory system | 9 | 17.6 | |
| Trauma | 4 | 7.8 | |
| Others | 3 | 5.8 | |
| Underlying disease | Hypertension | 20 | 39.2 |
| Malignancy | 14 | 27.5 | |
| Diabetic mellitus | 14 | 27.5 | |
| Stroke | 10 | 19.6 | |
| Liver cirrhosis | 7 | 13.7 | |
| COPD | 6 | 11.8 | |
| Congestive heart failure | 4 | 7.8 | |
| Coronary artery disease | 3 | 5.9 | |
| Uremia | 2 | 3.9 |
COPD = chronic obstructive pulmonary disease; ED = emergency department; ICU = intensive care unit.
The most common chief complaints of the 39 patients admitted for doctor-related or illness-related factors were abdominal pain (13/39, 33.3%) and vertigo/dizziness (4/39, 10.3%) with the neurological (35.9%) and digestive (23.1%) systems most commonly involved (Table 2).
Table 2.
Initial presentations and final diagnoses of return visits caused by doctor-related and disease-related factors.
| Final diagnostic categorizations (n) | Initial presentations of first visit (n) |
|---|---|
| Neurological system (14) | |
| Acute ischemic stroke (4) | Vertigo (3); Transient slurred speech (1) |
| Subarachnoid hemorrhage (4) | Trauma (1); Headache (1); |
| Neck pain (1); Insomnia (1) | |
| Subdural hemorrhage (2) | Vertigo (1); Trauma (1) |
| Intracerebral hemorrhage (1) | Trauma |
| Epidural abscess (1) | Back pain |
| Cerebral venous thrombosis (1) | Headache |
| Status epilepticus (1) | Convulsion |
| Digestive system (9) | |
| Gallbladder rupture (1) | Abdominal pain |
| Obstructive ileus (1) | Abdominal bloating |
| Inguinal hernia incarceration (1) | Abdominal pain |
| Intraabdominal infection (2) | Abdominal pain (2) |
| Hollow organ perforation (2) | Abdominal pain (2) |
| Ischemic bowel (1) | Abdominal pain |
| Liver cirrhosis with hepatic coma (1) | Abdominal bloating |
| Cardiovascular system (7) | |
| Acute coronary syndrome (4) | Chest pain (2); Syncope (1); |
| Abdominal pain (1) | |
| Abdominal aortic aneurysm (2) | Abdominal pain (1); |
| Back pain (1) | |
| Congestive heart failure (1) | Dyspnea |
| Respiratory system (6) | |
| Pneumonia (4) | Fever (2); Malaise (1); |
| Abdominal pain (1) | |
| Upper airway obstruction (2) | Dyspnea (2) |
| Oncology (3) | |
| Tumor bleeding (2) | Abdominal pain (1); |
| Oral bleeding (1) | |
| Brain tumor | Headache |
3.2. Characteristics of survivors and nonsurvivors
Patient characteristics were compared between the survival and nonsurvival groups (Table 3). Fourteen of the 51 patients died during hospitalization giving a mortality rate of 27.5%. There were no fatalities in the 10 patients with higher triage scores [emergency severity index (ESI) I & II]. Significantly higher mortality, however, was observed in patients with lower triage scores (ESI III & IV) (p = 0.045) with underlying malignancy and liver cirrhosis (p = 0.038 and 0.013, respectively).
Table 3.
The characteristics of survivors and nonsurvivors with ED return visit and admission to ICU.
| Variables | Survive (72.5%) | Death (27.5%) | Total (100%) | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Sex | 0.744 | |||||
| Female | 14 | 77.8 | 4 | 22.2 | 18 | |
| Male | 23 | 69.7 | 10 | 30.3 | 33 | |
| Age (y) | 0.758 | |||||
| <60 | 14 | 70.0 | 6 | 30.0 | 20 | |
| ≥60 | 23 | 74.2 | 8 | 25.8 | 31 | |
| Shift | 0.601 | |||||
| Day | 8 | 66.7 | 4 | 33.3 | 12 | |
| Evening | 18 | 69.2 | 8 | 30.8 | 26 | |
| Night | 11 | 84.6 | 2 | 15.4 | 13 | |
| First triage | 0.045* | |||||
| High level (I, II) | 10 | 100.0 | 0 | 0.0 | 10 | |
| Low level (III, IV) | 27 | 65.9 | 14 | 34.1 | 41 | |
| Revisited triage | 0.334 | |||||
| High level (I, II) | 25 | 78.1 | 7 | 21.9 | 32 | |
| Low level (III, IV) | 12 | 63.2 | 7 | 36.8 | 19 | |
| Return visit justification | 0.399 | |||||
| Doctor-related | 16 | 76.2 | 5 | 23.8 | 21 | |
| Illness-related | 13 | 72.2 | 5 | 27.8 | 18 | |
| Patient-related | 8 | 66.7 | 4 | 33.3 | 12 | |
| Underlying disease | ||||||
| Hypertension | 14 | 70.0 | 6 | 30.0 | 20 | 0.758 |
| Malignancy | 7 | 50.0 | 7 | 50.0 | 14 | 0.038* |
| Diabetic mellitus | 13 | 92.9 | 1 | 7.1 | 14 | 0.077 |
| Stroke | 9 | 90.0 | 1 | 10.0 | 10 | 0.250 |
| Liver cirrhosis | 2 | 28.6 | 5 | 71.4 | 7 | 0.013* |
| COPD | 4 | 66.7 | 2 | 33.3 | 6 | 0.661 |
| Congestive heart failure | 3 | 75.0 | 1 | 25.0 | 4 | >0.99 |
| Coronary artery disease | 3 | 100.0 | 0 | 0.0 | 3 | 0.552 |
| Uremia | 2 | 100.0 | 0 | 0.0 | 2 | >0.99 |
* Significance of difference determined by Chi-square test.
COPD = chronic obstructive pulmonary disease; ED = emergency department; ICU = intensive care unit.
4. Discussion
Previous studies have elucidated that unscheduled 72-hour ED return may be an insufficient quality indicator due to a lack of evidence of higher resource utilization or higher admission rates in these patients compared with first-time ED visitors. Indeed, the mortality rate of these patients has been reported to be as low as 0% to 1% [8,11,12] which hampers its role as a sensitive indicator of health care quality [11]. In contrast, other studies reported the mortality rate of patients with revisit-admission was relatively high, ranging from 4.1% to 10% [6,7,16]. Accordingly, hospital admission was shown to be a critical indicator of the severity of disease and represents the most serious adverse event in patients discharged from the ED [1,2,3,25]. The present study, which investigated patients with ED revisits and ICU admissions, explored the clinical implications of an even more differentiating parameter and showed a mortality of up to 27% in this setting. Moreover, medical quality is more likely to be reflected in the prevalence of doctor-related causes of revisits than that of patient- or disease-related causes. The prevalence of doctor-related causes for 72-hour ED revisits, 72-hour ED revisits with admissions, and 72-hour revisits with ICU admissions were 7.8% to 17% [5,6,10], 12% to 32% [5,6,7], and between 29% and 41% in the present study [27], respectively, which further underscores the possibility of utilizing 72-hour revisits with ICU admissions as an indicator of emergency health care quality.
The 4% incidence of ED revisits in this study was similar to that reported by most studies [5,6,7]. In the present study, 29% of patients with return visits were admitted to ordinary wards and 1% to the ICU, resembling the proportions of 22% and 0.8% in a study by Wu et al [5] and 33% and 2% in the study by Hu et al [6], respectively. The mean age of the patients with ED revisits within 72 hours and ordinary ward admission in this study was 55 years, which is similar to the ages of 59 years in the study by Hu et al [6] and 56 years in the study by Cheng et al [7]. In contrast, the mean age of revisit patients with ICU admission in this study was 63 years, higher than that of those with ordinary admission. Age has been shown to be a risk factor for admission after return visits [6]. The results of the current study further strengthen the assumption that the condition of elderly patients with return visits is likely to be more severe than that in younger patients. Their atypical disease presentations and complex medical conditions may delay timely intervention and require multidisciplinary management and more advanced care than younger patients [30,31].
In accordance with a slight male predominance (51 –54%) among patients with ED revisits within 72 hours, the present study showed an even higher prevalence of 64.7% for patients with subsequent ICU admissions (Table 1). The finding could probably be explained by poorer medical compliance for male ED patients compared with their female counterparts [32]. This is supported by the results of the current study, demonstrating that up to eight of the 12 revisits with ICU admissions were due to patient-related factors.
The quality of medical attention that a patient receives in the ED has also been reported as a significant factor in the incidence of return visits [6]. Indeed, previous studies have revealed an association between ED crowding and an increased rate of medication errors [33,34]. In this study, the highest prevalence of patients with return visits and ICU admissions visited during the evening shift on their first visit (51%) compared with 23.5% for the day shift and 25.5% for the night shift (Table 1). This highlights the impact of ED crowding and the number of available physicians. Further investigation in the present study demonstrated that physicians treated 2.48, 2.67, and 1.55 patients per hour in the ED for on the day, evening, and night shifts, respectively.
Although the current study demonstrated that ED revisits within 72 hours with subsequent admission to the ICU may be a useful indicator of emergency care quality, studies focusing on ED revisits with ICU admissions are rare. The overall ICU mortality rate in Taiwan between 2004 and 2009 was 20.2% [26]. A previous Taiwanese study which investigated the risk factors and prognostic indicators of unexpected ICU admission within 3 days after ED discharge demonstrated a mortality rate of 20% in this patient subpopulation [27]. The percentage was lower than that in the present study (27%). This discrepancy may be attributable to differences in the study designs of the two studies. Firstly, while the current investigation recruited only adult patients, previous studies included patients of all ages [26,27]. The overall mortality rate in the pediatric ICU has been reported to be 8.17% in Taiwan which is substantially lower than that for adult ICU patients (20%) [20,35]. This explains the lower mortality rate in the previous study [27]. Secondly, the present study included only patients with related complaints on the two visits as previously described [5,6,7,8,9], whereas the definition was unclear in the previous Taiwanese study [27]. Recruitment of patients with diseases of an unrelated nature during their first visits may include those who presented to the ED with severe diseases for the first time during their second visits, thereby eliminating the adverse impact of delay in diagnosis and treatment that contributed to the prevalence of ICU admissions. This proposal is also supported by the markedly lower prevalence of physician-related causes in the previous study (29%) [27] compared with that in the current study (41.2%). Furthermore, variations in patient characteristics and criteria for ICU admission may also contribute to the difference in the ICU mortality rates in the two studies.
The present study also demonstrated a notable impact of underlying diseases on the mortality of patients with ED revisits and ICU admissions. In particular, malignancy and liver disease were significant contributors to mortality in this patient population. One previous study also identified these two disease entities as significant risk factors for mortality after hospitalization in patients with ED return visits [7]. One paradoxical finding in the current study is that patients who initially presented with lower triage scores (ESI III & IV) had a notably higher mortality rate than those with higher scores (ESI I & II). One possible explanation may be the lack of vigilance of emergency physicians when encountering patients with seemingly trivial initial presentations.
Abdominal pain, fever, and vertigo were the most commonly reported initial manifestations in patients with ED revisits and hospitalization in previous studies [5,7]. The present study, which focused on patients with ED revisits and subsequent ICU admissions, also identified abdominal pain (13/39, 33.3%) and vertigo/dizziness (4/39, 10.3%) as the two most common initial manifestations. Although most abdominal pain in the current study had an alimentary origin (9/12, 66.7%), three patients (33%) had abdominal pain as an initial atypical presentation of cardiovascular (i.e., acute coronary syndrome and abdominal aortic aneurysm) and respiratory (i.e., pneumonia) diseases. Therefore, other than having a high level of vigilance, physicians should make use of convenient, noninvasive diagnostic tools such as sonography in the early diagnosis of potentially life-threatening conditions [36].
4.1. Limitations
The present study has limitations. Firstly, the number of patients was relatively small, not only because this was a single center retrospective study rather than a nationwide investigation, but also because the proportion of patients with ED revisits and admission to the ICU is very small compared with the total number of ED patients. Secondly, important details regarding the natural course of a disease may be missed through a mere review of the medical records, so it could not be accurately determined whether the causes of revisits were illness-related or doctor-related. To minimize the impact of this issue, three experts acted as reviewers to categorize the nature of the revisits. Thirdly, it is possible that some patients who developed more serious conditions after their initial ED visits sought medical attention at other institutions. Nevertheless, this is unlikely because our institution is located in a suburb with no other major medical facilities.
5. Conclusion
The present study demonstrated higher rates of patient mortality and doctor-related causes of admission than previous studies of 72-hour ED revisits and revisit-admission. Malignancy and hepatic diseases were the two most common underlying medical conditions positively associated with increased ICU mortality. This study also highlights the paradoxical observation of higher mortality for patients initially presenting to the ED with lower triage scores than those with higher scores. This finding underscores the importance of a high degree of vigilance when encountering patients with apparently trivial manifestations such as abdominal pain and vertigo.
Footnotes
Conflicts of interest: none.
References
- [1].Keith KD, Bocka JJ, Kobernick MS, Krome RL, Ross MA. Emergency department revisits. Ann Emerg Med. 1989;18:964–8. doi: 10.1016/s0196-0644(89)80461-5. [DOI] [PubMed] [Google Scholar]
- [2].Pierce JM, Kellerman AL, Oster C. “Bounces”: an analysis of short-term return visits to a public hospital emergency department. Ann Emerg Med. 1990;19:752–7. doi: 10.1016/s0196-0644(05)81698-1. [DOI] [PubMed] [Google Scholar]
- [3].Hu SC. Analysis of patient revisits to the emergency department. Am J Emerg Med. 1992;10:366–70. doi: 10.1016/0735-6757(92)90022-p. [DOI] [PubMed] [Google Scholar]
- [4].Wilkins PS, Beckett MW. Audit of unexpected return visits to an accident and emergency department. Arch Emerg Med. 1992;9:352–6. doi: 10.1136/emj.9.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wu CL, Wang FT, Chiang YC, Chiu YF, Lin TG, Fu LF, et al. Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med. 2010;38:512–7. doi: 10.1016/j.jemermed.2008.03.039. [DOI] [PubMed] [Google Scholar]
- [6].Hu KW, Lu YH, Lin HJ, Guo HR, Foo NP. Unscheduled return visits with and without admission post emergency department discharge. J Emerg Med. 2012;43:1110–8. doi: 10.1016/j.jemermed.2012.01.062. [DOI] [PubMed] [Google Scholar]
- [7].Cheng SY, Wang HT, Lee CW, Tsai TC, Hung CW, Wu KH. The characteristics and prognostic predictors of unplanned hospital admission within 72 hours after ED discharge. Am J Emerg Med. 2013;31:1490–4. doi: 10.1016/j.ajem.2013.08.004. [DOI] [PubMed] [Google Scholar]
- [8].Nunez S, Hexdall A, Aguirre-Jaime A. Unscheduled returns to the emergency department: an outcome of medical errors? Qual Saf Health Care. 2006;15:102–8. doi: 10.1136/qshc.2005.016618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lindsay P, Schull M, Bronskill S, Anderson G. The development ofindicators to measure the quality of clinical care in emergency departments following a modified-delphi approach. Acad Emerg Med. 2002;9:1131–9. doi: 10.1111/j.1553-2712.2002.tb01567.x. [DOI] [PubMed] [Google Scholar]
- [10].Liaw SJ, Bullard MJ, Hu PM. Rates and causes of emergency department revisits within 72 hours. J Formos Med Assoc. 1999;98:422–5. [PubMed] [Google Scholar]
- [11].Pham JC, Kirsch TD, Hill PM, De Ruggerio K, Hoffmann B. Seventy-two-hour returns may not be a good indicator of safety in the emergency department: a national study. Acad Emerg Med. 2011;18:390–7. doi: 10.1111/j.1553-2712.2011.01042.x. [DOI] [PubMed] [Google Scholar]
- [12].Kelly AM, Chirnside AM, Curry CH. An analysis of unscheduled return visits to an urban emergency department. N Z Med J. 1993;106:334–6. [PubMed] [Google Scholar]
- [13].Chung CH, Ng CP. An analysis of unscheduled return visits to the accident and emergency department of a general public hospital. J Emerg Med. 2003;10:153–61. [Google Scholar]
- [14].White DKL, Eddy L. Characteristics of patients who return to the emergency department within 72 hours in one community hospital. Adv Emerg Nurs J. 2011;33:344–53. doi: 10.1097/TME.0b013e31823438d6. [DOI] [PubMed] [Google Scholar]
- [15].Gordon JA, An LC, Hayward RA, Williams BC. Initial emergency department diagnosis and return visits: risk versus perception. Ann Emerg Med. 1998;32:569–73. doi: 10.1016/s0196-0644(98)70034-4. [DOI] [PubMed] [Google Scholar]
- [16].Wang HY, Chew G, Kung CT, Chung KJ, Lee WE. The use of Charlson comor-bidity index for patients revisiting the emergency department within 72 hours. Chang Gung Med J. 2007;30:437–44. [PubMed] [Google Scholar]
- [17].Tresch DD. Atypical presentations of cardiovascular disorders in the elderly. Geriatrics. 1987;42:41–6. [PubMed] [Google Scholar]
- [18].Fox RA. Atypical presentation of geriatric infection. Geriatrics. 1988;43:58–68. [PubMed] [Google Scholar]
- [19].O’Dell C. Atypical presentations of neurological illness in the elderly. Geriatrics. 1988;43:35–7. [PubMed] [Google Scholar]
- [20].Gambert SR, Escher JE. Atypical presentation of endocrine disorders in the elderly. Geriatrics. 1988;43:69–78. [PubMed] [Google Scholar]
- [21].Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients – Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- [22].Nguyen TV, Hillman KM, Buist MD. Adverse events in British hospitals. Preventive strategies, not epidemiological studies, are needed. BMJ. 2001;322:1425. [PMC free article] [PubMed] [Google Scholar]
- [23].Angus DC, Linde-Zwirble WT, Sirio CA, Rotondi AJ, Chelluri L, Newbold RC, 3rd, et al. The effect of managed care on ICU length of stay: implications for medicare. JAMA. 1996;276:1075–82. [PubMed] [Google Scholar]
- [24].Wu AW, Pronovost P, Morlock L. ICU incident reporting systems. J Crit Care. 2002;17:86–94. doi: 10.1053/jcrc.2002.35100. [DOI] [PubMed] [Google Scholar]
- [25].Young MP, Birkmeyer JD. Potential reduction in mortality rates using an intensivist model to manage intensive care units. EffClin Pract. 2000;3:284–9. [PubMed] [Google Scholar]
- [26].Cheng KU, Lu CL, Chung YC, Huang MC, Shen HN, Chen HM, et al. ICU service in Taiwan. J Intensive Care. 2014;2:8. doi: 10.1186/2052-0492-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Fan JS, Kao WF, Yen HT, Wang LM, Huang CI, Lee CH. Risk factors and prognostic predictors of unexpected intensive care unit admission within 3 days after D discharge. Am J Emerg Med. 2007;25:1009–14. doi: 10.1016/j.ajem.2007.03.005. [DOI] [PubMed] [Google Scholar]
- [28].Mintegui Raso S, Benito Fernandez J, Vazquez Ronco MA, Ortiz Andres A, Capape Zache S, Fernandez Landaluce A. Children's unscheduled return visit to an emergency department. An Esp Pediatr. 2000;52:542–7. [PubMed] [Google Scholar]
- [29].Goldman RD, Ong M, Macpherson A. Unscheduled return visits to the pedi-atric emergency department-one-year experience. Pediatr Emerg Care. 2006;22:545–9. doi: 10.1097/01.pec.0000230553.01917.05. [DOI] [PubMed] [Google Scholar]
- [30].McCusker J, Healey E, Bellavance F, Connolly B. Predictors of repeat department visits by elders. Acad Emerg Med. 1997;4:581–8. doi: 10.1111/j.1553-2712.1997.tb03582.x. [DOI] [PubMed] [Google Scholar]
- [31].McCusker J, Ionescu-Ittu R, Ciampi A, Vadeboncoeur A, Roberge D, Larouche D, et al. Hospital characteristics and emergency department care of older patients are associated with return visits. Acad Emerg Med. 2007;14:426–33. doi: 10.1197/j.aem.2006.11.020. [DOI] [PubMed] [Google Scholar]
- [32].Vukmir RB, Kremen R, Dehart DA, Meneqazzi J. Compliance with emergency department patient referral. Am J Emerg Med. 1992;10:413–7. doi: 10.1016/0735-6757(92)90065-6. [DOI] [PubMed] [Google Scholar]
- [33].Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010;28:304–9. doi: 10.1016/j.ajem.2008.12.014. [DOI] [PubMed] [Google Scholar]
- [34].Trezeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–5. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wang JN, Wu JM, Chen YJ. Validity of the updated pediatric risk of mortality score (PRISM III) in predicting the probability of mortality in a pediatric intensive care unit. Acta Paediatr Taiwan. 2001;42:333–7. [PubMed] [Google Scholar]
- [36].Lameris W, van Randen A, van Es HW, van Heesewijk JP, van Ramshorst B, Bouma WH, et al. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ. 2009;338:b2431. doi: 10.1136/bmj.b2431. [DOI] [PMC free article] [PubMed] [Google Scholar]


