Abstract
A 12-year-old adolescent girl with intractable pneumonia and desaturation was sent to our hospital. An immunocompromised state was highly suspected because of an oral thrush persisting for a year and pneumonia of unusual severity. Laboratory tests confirmed she had human immunodeficiency virus (HIV) infection and full-blown AIDS. She lived with her adopted parents and reported no history of sexual abuse, drug abuse, or blood transfusion. We contacted the Center of Disease Control and discovered that her mother had HIV and had passed away a few years ago, thus confirming that she was a case of vertically transmitted HIV patient who had only developed AIDS recently. Even though her mother had HIV, our public health department failed to follow her as a potential HIV victim, probably because routine HIV examinations for pregnant women only started in 2005, 4 years after she was born.
Keywords: Adolescent, AIDS, HIV, Vertical transmission
1. Introduction
Nowadays, pediatric AIDS patients are rare, thanks to the thorough prenatal health examination and meticulous perinatal care of infants of HIV (human immunodeficiency virus) mothers in developed countries. Although AIDS remains a challenging disease, it can be well controlled early with modern therapy. Fresh cases of AIDS children are seldom encountered now in our country because of the routine HIV examinations for pregnant women, established in 2005. Here, we report a rare case of adolescent onset of untreated AIDS in a teenager who was born prior to 2005, when there were no routine HIV examinations for pregnant women.
2. Case Report
A 12-year-old girl was admitted to our emergency room because of high fever up to 40° C with productive cough and shortness of breath for 4 days. In the emergency room, O2 saturation was 68% under room air. She had been treated at another hospital for 3 days and was treated with ampicillin–sulbactam and azithromycin and later shifted to vancomycin and cefotaxime. Urine pneumococcal antigen and mycoplasma IgM test results were negative there. A purified protein derivative test and sputum acid fast stain also yielded negative results, and a chest X-ray (Fig. 1) was also taken there. Because of her poor response to this treatment, she was transferred to our hospital.
Fig. 1.

Patient's chest X-ray showing reticulonodular changes.
Tracing her history, she was found to be an elementary school student with vaccinations up to date except for the pneumococcal polysaccharide conjugate vaccine and influenza vaccines. She had a history of allergic rhinitis, asthma, and atopic dermatitis, and she had been admitted to a hospital because of pneumonia twice over the past year. She was adopted, according to her adoptive mother's statement during hospitalization. Her adoptive family history was insignificant and her biological mother's history was not available at that time.
At the emergency room, her temperature/pulse rate/respiratory rate was 37.2/134/48, and her blood pressure was 118/64 mmHg. Her body weight was 53 kg (75–90th percentile), and her height was 160 cm (75–90th percentile). O2 saturation was maintained at 96–98% with a nasal cannula with a flow of 4–5 L/min. Chronic relapsing oral thrush was noted over her right buccal mucosa. Breathing sounds showed rhonchi and rales bilaterally, and subcostal retraction was noted. Both hands showed lesions of molluscum contagiosum. Laboratory tests showed white blood cell count of 6200 μL (segment, 75%; lymphocytes, 17%) and C-reactive protein level of 7.19 mg/dL. Venous blood gas showed the following details: pH 7.33; Pco2 53 mmHg; Po2 20 mmHg; HCO3− 27 mmol/L. Three sets of sputum acid fast stain were all negative, and a sputum culture showed nontuberculosis mycobacterium. A throat culture revealed HSV1+, but the influenza and adenovirus rapid tests were negative. An antinuclear antibody test also yielded negative results.
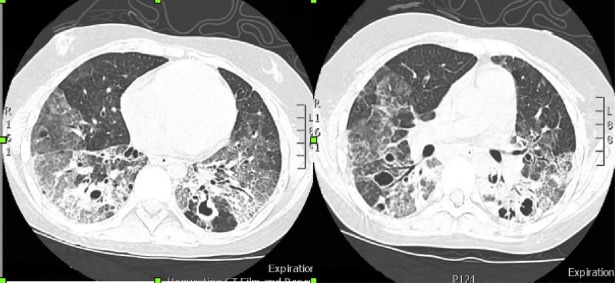
Under the impression of pneumonia with impending respiratory failure and suspected immunodeficiency, we administered vancomycin, levofloxacin, oseltamivir, trimethoprim-sulfamethoxazole, and valganciclovir for empiric treatment. However, because her condition continued to deteriorate, bilevel positive airway pressure support was given and a high-resolution computed tomography was performed that showed cystic changes along with multifocal interstitial infiltrates (Fig. 2).
Fig. 2.
Patient's computed tomography showing cystic changes with multifocal interstitial infiltrates.
Further immunology workup showed no antibody or complement abnormalities. However, an HIV-antibody-enzyme immuno-assay test was positive, and Western blotting for HIV confirmed HIV infection. The CD4 T cell count was 2.4 cells/mm3, and AIDS was confirmed. The HIV viral load was 60,598. We then changed the treatment to vancomycin, levofloxacin, oseltamivir, trimethoprim-sulfamethoxazole, ganciclovir, amphotericin B, and methylprednisolone for Pneumocystis jiroveci pneumonia (PJP) treatment. The sputum PJP polymerase chain reaction was strongly positive, and highly active antiretroviral therapy with efavirenz and kivexa was initiated.
We consulted a gynecologist and a social worker, and no drug or sexual abuse was found. Her family also denied a history of blood transfusion. We contacted the Center of Disease Control and were informed that her biological mother had died of AIDS.
Although her condition seemed to stabilize for a while, on the 7th day of hospitalization a sudden onset of desaturation occurred. A chest X-ray showed left-sided pneumothorax (Fig. 3), so a chest tube was inserted. Her condition continued to deteriorate, and right-sided pneumothorax was found and again treated with a chest tube. On the 10th day of hospitalization, unstable blood pressure and oliguria were noted, and despite fluid challenge and the administration of inotropic agents she died on the 12th day of hospitalization.
Fig. 3.

Patient had left-sided pneumothorax on 7th day of admission.
3. Discussion
In Taiwan, routine HIV examinations for pregnant women were established in 2005. In this case, the patient was born in 2001 and so our public health department failed to register her as a potential HIV patient even though her biological mother had full-blown AIDS.
The natural history of untreated vertically transmitted HIV is characterized by progressive immunosuppression. Most children infected with HIV show progression of HIV infection to AIDS and die before 5 years of age [1,2]. Our patient only showed clinical deterioration to AIDS at 12 years of age.
Among children who acquire HIV vertically, there is considerable variability in the manifestations of HIV infection, disease progression, and mortality. There appears to be two basic patterns of disease progression: rapid disease progression in which children reach a severe clinical stage within the 1st year of life, or a more typical, slower progression, with clinical deterioration by the age of 5 to 6 years. The clinical presentations of AIDS children are different from those of adults. In the early onset group, patients usually present with PJP infection with high mortality as well as encephalopathy and wasting syndrome [3]. In the late onset group, the clinical presentation could be recurrent bacterial infection, generalized lymphadenopathy, hepatomegaly, lymphocytic interstitial pneumonitis, and parotitis. Kaposi's sarcoma, lymphoma, and opportunistic central nervous system infection are relatively rare in children. Other manifestations, including PJP pneumonia, neurologic abnormalities, recurrent eczema, cardiomyopathy, exanthema, fever and diarrhea, are common in both adult and pediatric AIDS patients [3,4].
The timing of HIV vertical transmission seems to be an important determinant of disease progression. Children infected within the first 2 months of life have a higher mortality rate at 12 months than those infected later [2,5]. Rapid progression has been reported to be inversely related to maternal CD4 count and more common in infants with intrauterine infections [6].
The number of adolescents with vertically transmitted HIV is increasing in developed countries. A study from New York City reported that the percentage of children with vertically transmitted HIV who were 9 years or older increased from 5% to 25% between 1989–1991 and 1995–1998 [7]. The survival of children to adolescence represents the success of antiretroviral therapy and aggressive prophylaxis and treatment of opportunistic infections. However, the number of cases of vertical transmission should decrease with the success of perinatal highly active antiretroviral therapy.
The standard test for HIV infection in infants and children younger than 18 months is polymerase chain reaction for two reasons. First, maternal HIV antibodies may persist for months after delivery. In a study of 271 children born to HIV-infected mothers, 234 uninfected, immunologically normal, well children were followed for over a year [8]. The mean age at losing maternal antibodies was found to be 10.3 months, and one child did not lose maternal antibodies until the toddler was older than 18 months. Second, when antiretroviral therapy has been administered to the mother, either as treatment or to prevent vertical transmission, and also administered as prophylaxis to the baby, an HIV viral load may be undetectable even in an infected infant. Cord blood should not be used for testing because of the possibility of contamination with maternal blood. Repeated testing is necessary because HIV infection can occur perinatally, and a very recent infection will not be detectable.
Vertical transmission of HIV can occur at any time during gestation and delivery, and through breast milk in the postpartum period. More than 95% of HIV-infected children worldwide acquire the virus via vertical transmission, and the rate of vertical transmission ranges from 20% to 30% in the absence of antiretroviral therapy. Although it is known that HIV can be transmitted early in gestation in utero, most transmissions (50% to 80%) are believed to occur during the period near or during delivery [9]. The use of antiretroviral therapy in HIV-infected pregnant women and their infants has reduced the mother-to-child transmission rate to less than 2% in some parts of the world. Prevention of new vertical HIV infections is one of the most powerful methods available to reduce the global impact of HIV.
In conclusion, vertical transmission of HIV plays a significant role in pediatric HIV. Public health registration of HIV patients and close follow-up of their sex partners and offspring is very important in the early diagnosis of HIV carriers, which, for vertical transmission, can be done with the help of polymerase chain reaction. Chronic pediatric relapsing oral thrush should raise the clinical suspicion of an immunocompromised state. The diagnosis of pediatric HIV depends on clinical alertness and careful history taking.
Footnotes
Conflicts of interest: none.
References
- [1].Spira R, Lepage P, Msellati P, Van De Perre P, Leroy Y, Simonon A, et al. Natural history of human immunodeficiency virus type 1 infection in children: a five-year prospective study in Rwanda. Mother-to-Child HIV-1 Transmission Study Group. Pediatrics. 1999;104:e56. doi: 10.1542/peds.104.5.e56. [DOI] [PubMed] [Google Scholar]
- [2].Newell ML, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F, et al. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet. 2004;364:1236–43. doi: 10.1016/S0140-6736(04)17140-7. [DOI] [PubMed] [Google Scholar]
- [3].Kovacs A, Scott GB. Advances in the management and care of HIV-positive newborns and infants. In: Pizzo PA, Wilfert CM, editors. Pediatric AIDS. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. pp. 567–92. [Google Scholar]
- [4].Bamhart HX, Caldwell MB, Thomas P, Nascola L, Ortiz I, Hsu H, et al. Natural history of human immunodeficiency virus disease in perinatally infected children: an analysis from the Pediatric Spectrum of Disease Project. Pediatrics. 1996;97:710–6. [PubMed] [Google Scholar]
- [5].Mbori-Ngacha D, Nduati R, John G, Reilly M, Richardson B, Mwatha A, et al. Morbidity and mortality in breastfed and formula-fed infants of HIV-1-infected women: a randomized clinical trial. JAMA. 2001;286:2413–20. doi: 10.1001/jama.286.19.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mphatswe W, Blanckenberg N, Tudor-Williams G, Prensergast A, Thobakqale C, Mkhwanazi N, et al. High frequency of rapid immunological progression in African infants infected in the era of perinatal HIV prophylaxis. AIDS. 2007;21:1253–61. doi: 10.1097/QAD.0b013e3281a3bec2. [DOI] [PubMed] [Google Scholar]
- [7].Abrams EJ, Weedon J, Bertolli J, Bornschlegel K, Cervia J, Mendez H, et al. Aging cohort of perinatally human immunodeficiency virus-infected children in New York City. New York City Pediatric Surveillance of Disease Consortium. Pediatr Infect DisJ. 2001;20:511–7. doi: 10.1097/00006454-200105000-00008. [DOI] [PubMed] [Google Scholar]
- [8].Mother-to-child transmission of HIV infection. The European Collaborative Study. Lancet. 1988;2:1039–43. [PubMed] [Google Scholar]
- [9].Pizzo PA, Wilfert CM. Pediatric AIDS: the challenge of HIV infection in infants, children, and adolescents. Baltimore, MD: Williams and Wilkins; 1998. [Google Scholar]