Introduction
Since throat swab specimens obtained from three adult Chinese patients were confirmed as an avian-origin influenza A (H7N9) virus by local Centers for Disease Control and Prevention (CDC) in 2013,[1] many confirmed cases have been reported in Mainland of China. Although family and hospital clusters with confirmed or suspected avian H7N9 virus infection were previously reported and person-to-person transmission was put forward, human infection of H7N9 appears to be associated with exposure to infected live poultry or contaminated environments[2] and no clear evidence has proved that it could transmit from person to person. Here, we report a case confirmed with H7N9 after intimately contact with his H7N9 ward mate, it may be the first case infected between ward mates in a ward, so we report it here.
Case Report
The index case, a 66-year-old male with hypertension and type II diabetes for more than 10 years, was admitted to the respiratory department for cough and expectoration with 3 days, aggravation with bloody sputum with 1 day on December 17, 2016. He was transferred to the nephrology department for elevated serum creatinine and hypourocrinia the next day (December 18). The symptom of cough and expectoration was exacerbated, developed with dyspnea, dizzy, pink foam sputum, and descend transcutaneous oxygen saturation in the 3rd day (December 19), and was transferred to intensive care unit soon. Laboratory investigation of the throat swabs showed that he was positive for H7N9 by real-time polymerase chain reaction (RT-PCR). X-rays showed bilateral pneumonia and high-density patchiness in the left lung [December 19, Figure 1a]. He was died of persistent hyperpyrexia, respiratory failure, and acute respiratory distress syndrome at last although treated with mechanical ventilation, broad-spectrum antibiotics, oseltamivir, and immunological therapy. The index patient had visited a live-poultry market (LPM) to buy food every day within 10 days before his illness onset and had no direct contact with live poultry in the market.
Figure 1.
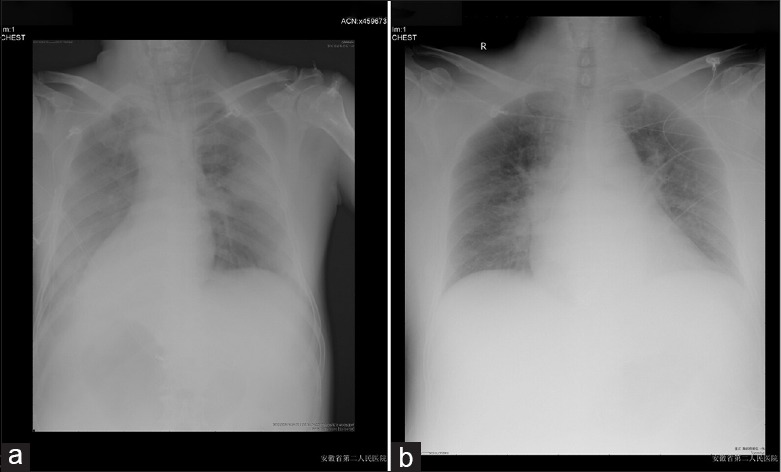
(a) X-rays of the index case showed bilateral pneumonia and high-density patchiness in the left lung. (b) X-rays of Case 2 (index case's ward mate) showed bilateral pneumonia.
Case 2 (index case's ward mate), a 62-year-old male with no underlying disease, was admitted to the nephrology department and diagnosed as nephrotic syndrome due to edema of lower extremity for 1 months and palpebral edema for 3 days on December 16, treated with hormone drug. Case 2 had an intimate contact with the index case on December 18; he and the index case stayed in the same room in the nephrology ward for approximately 20 h, developed a throat sore and cough on December 21. RT-PCR analysis of throat swabs from the patient tested positive for novel avian H7N9 nucleic acid (the same method and reagent as the index case). X-rays showed bilateral pneumonia [December 25, Figure 1b]. His condition remained stable and symptoms were improved. He was discharged after sputum samples tested negative for H7N9 by RT-PCR 10 days later. He had no history of exposure to live poultry or LPM before the illness onset.
Discussion
Since the three of avian influenza A (H7N9) cases were first reported in China on 31 March 2013, there have been five major epidemic waves until January 2017. A study showed that 68% of infected cases visited LPMs or were exposed to market poultry, even without direct (touching) or indirect (within 1 m) contact; it indicates that exposure to poultry in markets was associated with A (H7N9) virus infection, even without poultry contact.[3] LPMs have been reported as a main source of H7N9 transmission by the way of human-poultry contact and avian-related environmental exposures; after LPM closure was enforced in several Chinese cities, the incidence of H7N9 human cases rapidly reduced.[4] Even though human-to-human transmission has never been confirmed, there were some case reports of cluster in many cities of China.
Most affected H7N9 cases had a history of visiting LPMs or contacting with poultry 7–10 days before the onset of illnesses, indicating that the sources of infection were likely to be either contaminated environment or infected poultry.[5] Though family and hospital clusters with confirmed or suspected avian H7N9 virus infection were previously reported, no clear evidence indicated that the novel virus could transmit from person to person. The second case in this report had physical contact with the index case when assisting the index case to the bathroom (it lasted for 10 min) and had no history of exposure to live poultry or LPMs before the illness onset. There were a lot of family members in the ward, but he was the only one who was in close contact with the index case, and he was the only one confirmed H7N9 besides the index case. To the best of our knowledge, the case indicates that it is human-to-human transmission happened in a ward with detailed epidemiological, clinical, virological data, and genome analyses of two collected H7N9 virus for providing genetic homology are submitting to CDC.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
References
- 1.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888–97. doi: 10.1056/NEJMoa1304459. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: Clinical analysis and characterisation of viral genome. Lancet. 2013;381:1916–25. doi: 10.1016/S0140-6736(13)60903-4. doi: 10.1016/S0140-6736(13) 60903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu B, Havers F, Chen E, Yuan Z, Yuan H, Ou J, et al. Risk factors for influenza A (H7N9) disease – China, 2013. Clin Infect Dis. 2014;59:787–94. doi: 10.1093/cid/ciu423. doi: 10.1093/cid/ciu423. [DOI] [PubMed] [Google Scholar]
- 4.Murhekar M, Arima Y, Horby P, Vandemaele KA, Vong S, Zijian F, et al. Avian influenza A (H7N9) and the closure of live bird markets. Western Pac Surveill Response J. 2013;4:4–7. doi: 10.5365/WPSAR.2013.4.2.008. doi: 10.5365/WPSAR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He Y, Liu P, Tang S, Chen Y, Pei E, Zhao B, et al. Live poultry market closure and control of avian influenza A (H7N9), Shanghai, China. Emerg Infect Dis. 2014;20:1565–6. doi: 10.3201/eid2009.131243. doi: 10.3201/eid2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


