Abstract
Maternal immunization is an important strategy recommended to protect both mothers and infants from serious infectious diseases; however uptake of maternal immunization is poor in Australia. This study aimed to gain an in-depth understanding of the decision making process and factors influencing a pregnant woman's decisions about recommended immunizations. This qualitative study used semi-structured interviews with open-ended questions to interview pregnant women. Data were analyzed using thematic analysis techniques and drew on the Health Belief Model. Pregnant women (n = 17) were asked about their attitudes toward immunization during pregnancy and their perceptions about risk during pregnancy. Women were also asked to detail their decision making process and factors influencing their decisions about immunizations in relation to pregnancy. Most of the participants were not aware of the immunizations recommended during pregnancy, in pregnancy planning or after delivery. In addition to endorsement by their health care provider (HCP), perception of risk and benefit, including risk of infection, previous vaccination experiences and assessing cost benefit play a vital role in women's decisions whether to be immunized while pregnant. Although the role of the healthcare provider in advising pregnant women about immunizations was identified as vitally important, the majority of women had not been advised of recommended vaccines by their healthcare provider. Healthcare providers are key to ensuring pregnant mothers are informed about recommended vaccines and these need to be more proactively supported and encouraged by healthcare providers. This is likely to have a positive effect on acceptance and uptake of immunization by pregnant women.
Keywords: decision making, Influenza vaccine, maternal immunization, pregnancy, qualitative interviews
Abbreviations
- HCP
healthcare provider
Introduction
Maternal immunization is an important strategy for reducing the burden of infectious disease in pregnant women and their newborn infants. Many countries including the U.K, Australia and USA recommend influenza vaccination during pregnancy and more recently a pertussis booster for mothers in preconception or post-partum period or alternatively in the third trimester of pregnancy (see Box 1).1-3 Perinatal or postpartum maternal immunization confers benefits both to the pregnant mother and the baby. Immunizing the mother prevents infection in the mother and transmission of infection to infants. It is potentially effective for protecting newborn infants, as parents are often the primary reservoir and source of neonatal and infant infections.4-6 Immunizing parents and siblings, carriers and grandparents as part of a cocooning strategy provides additional protection for the newborn.7-10
Box 1.
Immunization recommendations during pregnancy planning and pregnancy in the Australian Immunisation Handbook 10th Edition (Department of Health and Aging, 2013)
| Measles, Mumps and Rubella (MMR) Vaccination- can be given at least 28 days before becoming pregnant and is routinely given after delivery if no serological evidence of immunity |
| Varicella (chickenpox) vaccination- Given at least 30 days before becoming pregnant |
| Influenza Vaccination- Can be given at any time during pregnancy |
| Pertussis (whooping cough) Vaccination- Can be given before becoming pregnant or post-delivery. Or given in the third trimester (recent recommendation in Australia)* |
*this recommendation was made after the study had commenced.
Influenza and pertussis create a significant burden of disease affecting both mothers and newborns. Influenza has been found to increase a pregnant woman's risk of respiratory hospitalization and preterm delivery.11,12 Maternal influenza illness during pregnancy has also been linked to congenital abnormalities in infants and other adverse pregnancy outcomes.11-13 Pertussis is a serious infection in young infants with the highest hospitalization rates and deaths from pertussis in infants less than 3 months of age. As infants are too young to have received adequate pertussis immunization, reducing transmission from parents is likely to reduce the risk to young infants.14
However, despite the known risks of infectious illnesses during pregnancy, the potential benefits of vaccination, and the existence of clear recommendations in the Australian immunization guidelines, maternal immunization rates remain suboptimal. Uptake of influenza vaccine during pregnancy in Australia is currently around 30%.15,16 As pertussis vaccination during pregnancy is not funded in Australia, uptake of this strategy is expected to be low compared to both the UK, where 60% of pregnant women were vaccinated during a recent pertussis epidemic,3 and with the 91% uptake of the recommended childhood immunizations in Australia.17
Thus, understanding reasons for suboptimal uptake of maternal immunizations is important for devising strategies to increase vaccination in this at risk group. Surveys of pregnant women have identified a number of factors associated with increased likelihood of immunization including prior vaccination status,16,18 knowledge of vaccines and the diseases they prevent,16,19-21 perceived susceptibility to vaccine preventable illnesses15,16,19 and healthcare provider (HCP) recommendation.21-23 Lack of trust in vaccine information19,24 and in the safety and effectiveness of vaccines are factors associated with reduced likelihood of maternal immunization during pregnancy.23,24 These factors align with what is known about parental decision-making for childhood immunization25 and the decision-making process adults undertake on their own behalf about vaccination.26
However, much less is known about how pregnant women make decisions about maternal immunization including how they weigh benefits and risks and whether particular factors are important under particular conditions. Two recent qualitative studies27-29 have found similar themes to those identified from surveys: importance of HCP recommendation and trusting relationships, perceptions of risk and susceptibility regarding vaccines and vaccine-preventable diseases, and lack of awareness and knowledge about the availability of maternal immunizations. However, both also highlight something not identified from the surveys or from the wider immunization decision literature; the challenge of balancing the risks and benefits to both the mother and the unborn baby in making the decision to vaccinate. The decision-making process mirrors that found about food safety recommendations during pregnancy.30,31 Typically, in these types of weighing up processes for pregnant women the risks and benefits for the unborn child dominate over those of the mother.32
This study aimed to understand pregnant women's decision-making process about vaccination before, and during pregnancy.
Findings
Of the 75 women approached, 20 consented to participate in the study (one later withdrew from the study for time reasons and 2 were not contactable after several attempts). Participants were at various stages of their pregnancy ranging from their first antenatal appointment to the last trimester and 4 of the 17 women had their husband or another person present with them during the interview. Information about immunization status for the recommended vaccines was also collected from the women at the time of the interview (see Table 1), and is summarized in brackets after each illustrative quotation below.
Table 1.
Awareness of pregnancy immunization recommendations, willingness to receive them in pregnancy and vaccination status of interview participants
| Participant | Aware of influenza vaccination in pregnancy | Awareness of pertussis vac recommended in pregnancy planning or post-natally1 | Willingness to have vaccines during pregnancy | Vaccination status during pre-pregnancy planning/ pregnancy |
|---|---|---|---|---|
| 1. Australian | Yes | No | No | Nil2 |
| 2. Australian | No | No | No | Nil |
| 3. Australian | No | No | Yes as long as no risk to the baby | Nil |
| 4. Australian | No | No | No | Nil |
| 5. Australian | No | No | Yes as long as no risk to the baby | Nil |
| 6. Australian | Yes | Yes | Yes as long as no risk to the baby | Pertussis vaccine after birth of last child Nil during current pregnancy |
| 7. Australian | No | No | No | Nil |
| 8. Australian | No | No | Yes as long as no risk to the baby | Influenza vaccine |
| 9. Australian | Yes | Yes | Yes | Nil |
| 10. Indonesian (+husband) | No | Yes | Yes | Nil |
| 11. Australian | No | Yes | Yes depends on risk to the baby | Nil |
| 12. Sri Lankan | No | Yes | Yes depends on risk to the baby | Rubella vaccine Influenza vaccine |
| 13. Australian (+Partner) | No | No | No | Nil |
| 14. Australian (+husband) | No | Yes | Yes depends on risk to the baby | Influenza vaccine |
| 15. Indonesian | No | No | Not sure | Nil |
| 16. Australian | No | No | No | Nil |
| 17. Australian (+husband) | No | Yes | Not sure | Nil |
Notes: 1. This was the recommendation at the time of interview. This has subsequently had the addition of pertussis vaccination in the third trimester of pregnancy added to the recommendation for pertussis vaccine in pregnancy planning or postnatally 2. Had not received any maternal immunization in this pregnancy at the time of interview.
Using the Health Belief Model as a framework for this analysis the study identified themes underlying the decision making process of pregnant women. The Health Belief Model refers to individual perceptions, modifying factors and the likelihood of action when considering health behaviors. This model has been used to assess other pregnancy related behaviors such as acceptance of food safety recommendations31 and vaccination.30 Our analysis was consistent with the key elements of this framework. Individual perceptions included perceived susceptibility and perception of risk to both the mother and the unborn child, and women's beliefs and attitudes about pregnancy decision-making in general and about immunization decision-making in particular. Modifying factors included knowledge and awareness, and previous experiences of immunizations and vaccine-preventable diseases. Likelihood of action or cues to action was most strongly influenced by HCP (Fig. 1). These themes are discussed with illustrative quotes from the interviews.
Figure 1.
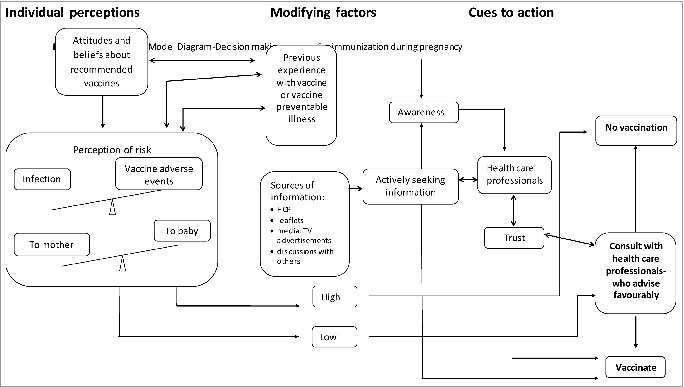
Decision making process for immunization during pregnancy.
Individual perceptions
Perceived susceptibility: Perception of risk
Pregnant mothers in this study described having to ‘weigh up’ the risk both for themselves and for their infant of having the vaccine versus the risk of acquiring the infection. Some mothers compared the risk associated with vaccines to those associated with other potential risks in pregnancy. While for others the potential risks associated with vaccination outweighed the risk posed by the infection.
What is the risk to the baby? Is there less risk to the baby me having the vaccination or having the vaccination's gonna mess up the baby. If it's gonna cause, you know, massive birth defect, miscarriage, or….then I wouldn't get it. P5 (not vaccinated or willing to be vaccinated)
I: You said you haven't had the whooping cough vaccine as well, do you intend to have it once your baby is born?
R: Probably I’d still say no. I still think my risk is quite low. If I was traveling a bit more maybe and with the baby. It would be something I’d consider. P3 (not vaccinated but willing to consider if no risk to baby)
I: And so in the future if there were more vaccines offered during pregnancy such as the whooping cough [vaccine], would you consider having it and why or why not?
R: Ahhh, um I’d probably still wait until after to be honest……. Just um well I think if you can have it straight after it's probably just as effective and then you are eliminating any risk. P8 (received influenza vaccine, willing to consider pertussis if no risk to baby)
Beliefs and Attitudes
Women's beliefs about immunization, previous experiences of immunization and also of vaccine-preventable diseases, and perceptions of risk about immunization and vaccine-preventable diseases (both for themselves and for their unborn child), influenced how they felt about immunization during their pregnancy. Most women were favorably disposed toward immunizations and had previously received immunizations against influenza and/or pertussis, and those who were mothers already, had ensured their children received their childhood immunizations. However, several women had a previous negative experience with the influenza vaccine (usually the perception that they had become infected with influenza infection from the vaccine) which influenced their decision not to have it during pregnancy.
…[the flu vaccination] I have had a bad experience myself and then it's been my decision that I don't actually get anymore I used to get it every year and then I was bed ridden for 3 weeks at one stage so it just put me off I just would probably still choose not to get it to be honest….purely because of what it's done for me in the past but now I do think that that's definitely important to recommend and at least give people the choice to see if they want to go that way… P9 (not vaccinated but willing to consider)
Participants who were hesitant to accept the influenza vaccine, or any others including the pertussis vaccine if it was recommended in pregnancy, often judged they were in the category of ‘low risk’ and felt such recommendations were not directed at them but at women who had a known susceptibility to infection or who were classified as having a high risk pregnancy by their HCP due to a pre-existing condition (e.g. obesity) or because of a pregnancy-related condition (e.g., preeclampsia). Many women in this study believed that during their pregnancy they were at no greater risk of infections than when they weren't pregnant and one participant believed she was less susceptible during pregnancy than when she was not pregnant, reasoning that as she was adopting a healthier lifestyle because she was pregnant this would also reduce her susceptibility to vaccine-preventable infections. Some women believed that if they normally recovered easily and quickly from infections that the influenza vaccination (in particular) was not essential for them.
I wouldn't just have it (the flu vaccination) on the off chance something would go wrong. If I was considered to be high risk or something, or if I did always get sick, then I wouldn't have a problem with it. P6 (not vaccinated in this pregnancy, pertussis vaccine last pregnancy, willing to consider this pregnancy)
Modifying Factors
Knowledge, awareness and information provision
Awareness of recommended vaccines pre-conception and during pregnancy was quite low (14 of the 17 participants were not aware that the influenza vaccine is offered in pregnancy and 10 were unaware that the pertussis vaccine is also recommended during pregnancy planning or postnatally). All believed that more information should be available from their HCP about the recommended immunizations. Even those who weren't sure whether they would accept influenza vaccination felt that the information should be made more readily available so that pregnant women are aware of the recommendations and could make an informed choice about whether to receive the immunization.
But if is not commonly known [recommended vaccines] like I certainly don't know of any or haven't been told of any vaccinations that are safe for me to have during my pregnancy. So I don't know much information about it. P9 (not vaccinated but willing to consider)
Other sources (or suggested sources) of information for some of the participants in this study were: discussions with others (other parents, friends, family members); leaflets; the media; and from actively seeking information on the internet.
Normally, when you are in the hospital you have a lot of leaflets and stuff from [the waiting room] Sometimes I’m browsing on the internet to see which ones are good and what to do. Because I know that Rubella is not good to have when you’re planning for a baby a…within 3 months or something. So.. yeah.. I’m going through and which ones to have… P3 (not vaccinated but willing to consider if no risk to baby)
You see the ads, I mean the biggest one is probably whooping cough with the new born baby. You know it's heart breaking. So yeah.. P5 (not vaccinated but willing to consider if no risk to baby)
Previous Experiences
Pregnant mothers who had a negative experience with vaccine-preventable illness either personally or while caring for a child or family member appeared to be more aware of vaccine- preventable illnesses and more accepting of recommended vaccines.
…and with the influenza, like the swine flu, my sister having it. You know, sitting in ICU with her and that it's seen..what… first hand sort of thing, what actually does happen. So, you wanna do whatever you can to prevent that happening to yourself. P5 (not vaccinated but willing to consider if no risk to baby)
Likelihood of action/Cues to action
Role of healthcare providers in the decision-making process
HCPs were an important source of information about immunizations during pregnancy, and were often the first person that women would turn to for help in making decisions about their pregnancy care. Participants’ awareness of the recommendations to receive immunizations during pregnancy were often dependent on being told about this by their HCP. Even if the women learned about the recommended vaccines through another source, they usually sought the endorsement of their HCP before making a decision to accept vaccination. Trust in the information provided by the HCP and in the care provided during their pregnancy was central to the women's decision to accept their HCP's recommendation.
Interviewee : (thinking) Actually, I approached the doctor and asked whether it's good to have the flu vaccine…
Investigator: And after that you ha[d] it?
Interviewee : yeah… P3 (not vaccinated but willing to consider if no to baby)
Well I weigh up you know whether but generally I mean I feel pretty comfortable that if the obstetrician says you know it's okay you should have it then it should be fine. P6 (not vaccinated in this pregnancy, pertussis vaccine last pregnancy, willing to consider this pregnancy)
If they [my HCP] recommend it and say “look, I really should have it” I wouldn't hesitate. P8 (influenza vaccine, willing to consider pertussis if no risk to baby)
I like my doctor. If she recommends something or she believes that something is the right way to go. I’m fine with that. P6 (not vaccinated in this pregnancy, pertussis vaccine last pregnancy, willing to consider this pregnancy)
I have considered things myself and weigh things up. And then I go by what they [HCP] say, but I mean basically I’m trying to stick with what they know, cause they know a lot more than we know (laughs). They study a lot longer P7 (not vaccinated, not willing to consider vaccination)
Discussion
Making decisions about vaccination during pregnancy is complex. As with any decision about medical care during pregnancy women must simultaneously weigh up the perceived risks and benefits to themselves and their baby. They must balance the risk of not being treated (in this case the risk of infection with the vaccine-preventable illness) against the risk of being treated, including considering the possibility of adverse events or side-effects of the intended treatment. Often these factors pull in opposite directions, with the benefit accruing to one while the risk is borne by the other.
In the case of immunization during pregnancy we found that this balancing process was mediated by the mother's attitudes, beliefs and values about vaccinations in general, and her experiences of both vaccination and vaccine-preventable diseases (both for herself and for family and close friends). Previous negative experiences with vaccines (in particular the perception of having developed influenza after having received the influenza vaccine) tended to predispose women toward refusing the vaccine if offered, while negative experiences of vaccine-preventable diseases (whether for themselves or for a close relative or friend) heightened the perception of risk posed by these diseases generally and tended to predispose women to be more accepting of the vaccine recommendation. These findings are consistent with studies of other risk associated decision-making processes during pregnancy, including vaccination decisions.22,29-31
Whether a woman decided to receive the recommended vaccine during pregnancy was strongly linked to whether her health care provider raised the possibility and in particular, made a positive recommendation. The most significant cue to action as described in the health belief model for the mothers in this study was endorsement from their HCP. At a minimum, pregnant women viewed issues brought to their attention by their health care providers as the most important issues they are likely to consider. Given the large volume of pregnancy related information that a woman needs to consider during the course of her pregnancy, immunization may be considered a topic of lower priority. As with parental decision-making in childhood vaccination decisions,25 HCP endorsement appears to be a key factor in the decision making process for pregnant mothers about vaccines during pregnancy.22,23,30,33 Midwives, obstetricians and GPs play a vital role not only in raising awareness about recommended vaccines, but also in raising awareness about the importance of being protected against influenza as a pregnant mother and similarly the importance of protecting their baby against pertussis and influenza at a time related to high mortality. We found that the women in our study were not generally aware that pregnancy increases their risk of acquiring vaccine-preventable infections and that some of those who were hesitant to accept vaccination cited their low risk of infection as the reason.
In general, the women in this study were much more aware of the potential risks to their unborn child of any medical treatment (including vaccinations) and were much more hesitant to accept treatments if there could be any risk of harm to their babies. In terms of vaccination, this concern could be ameliorated by a direct recommendation from their HCP to receive the vaccine, and many of the participants in this study said they would be willing to consider having vaccinations postpartum (having passed the point in their pregnancy when the immunization can be safely provided before becoming aware of the recommendation). While discussion with partners, friends and family were also important we identified that HCPs play a gatekeeper role, both in terms of ensuring pregnant women are aware of recommended vaccines and also in terms of endorsing a women's decision to receive them. Thus a trusting relationship between the woman and her HCP is vital.
The majority of women in this study had not received any information from their HCP about recommended immunizations before, during and after pregnancy and many were completely unaware that such recommendations existed. While lack of knowledge of recommended vaccines and the failure of HCPs involved in obstetric care to provide this information appears to contribute to the current low rate of uptake of these important recommended vaccines, 2 recent studies have found that these maternal immunizations would be offered routinely if they were incorporated into the antenatal care plan or pathway.18,34 Thus rather than being a problem requiring change in HCP or maternal attitudes and knowledge, efforts to improve uptake could usefully focus on including these vaccines in routine care. Our study and others15,22,23 suggest that many women would accept these immunizations if offered.
The results of this study might not be generalizable to all pregnant women. There may be differences in views across women with different parity and stage of pregnancy that could not be explored given the small qualitative sample and aims of this study. Despite our efforts to sample women who had and had not been vaccinated during their current pregnancy, only 3 of our 17 participants had been vaccinated, although more than half expressed a willingness to be vaccinated once they were aware of the possibility. It is possible that if awareness of pregnancy immunizations increases a different pattern of responses might be observed. While the study included participants from both a public and a private clinic within a public tertiary hospital, it is not known what, if any, information is given to pregnant women in other maternity centers and/or may be limited to the Australian context. The fact that some mothers had their partners present at the interviews may have influenced how the mothers answered the questions; however, partners are important contributors in the decision making process and for positive outcomes on a number of decisions for pregnant mothers.20,35
Conclusion
Weighing up risk with regard to immunization is a complex decision making process for pregnant mothers and HCP endorsement appears to be a key. Midwives, obstetricians and GPs play a vital role in raising awareness about recommended vaccines and about the importance of both the pregnant woman and her unborn child being protected against influenza and pertussis.
Methods
Setting and participants
Pregnant women aged 18 and over in various stages of pregnancy (12 to 36 weeks) were recruited from the public antenatal clinic (13 participants) and a private obstetric clinic (4 participants) both located in a large tertiary obstetric hospital in Adelaide, South Australia with approximately 5000 obstetric deliveries annually. Three models of care are offered to pregnant women within the hospital; obstetrics (through the public and private systems), midwifery group practice and shared care. This setting allowed for inclusion of participants from a range of socio-economic backgrounds and from all models of care.
Data collection
Data collection occurred from April 2011 to January 2012. At this time influenza vaccination for pregnant women was recommended but this was before a recommendation was made in Australia for pertussis immunization during the third trimester of pregnancy. Potential participants were approached in the public and private antenatal clinics before their scheduled appointment. They were eligible to participate at any stage of their pregnancy if they had proficiency in English. Following consent, this study used a qualitative approach to data collection and analysis. Semi-structured interviews were undertaken with 17 pregnant women, either in person at the hospital or by telephone by 3 researchers (IA, NT, JC) Open-ended questions were used to explore the decision-making process about recommended immunizations during pregnancy planning and during pregnancy. Participants were asked to discuss their decision making process toward recommended vaccinations during pregnancy planning and in pregnancy including:
knowledge and perception of infections that may affect pregnant women and their baby
how pregnant women find information about recommended vaccinations while planning for, or during, pregnancy
knowledge and perceptions of vaccinations in general
factors influencing the decision to either accept or refuse vaccinations both during pregnancy and in general
Interviews were digitally recorded and transcribed verbatim and managed with qualitative data analysis software (Nvivo 9).
Sampling frame and analysis
A purposive sampling frame36 was used for recruiting pregnant women in the antenatal clinic. We purposively sought to interview pregnant women who had been vaccinated during pregnancy (or indicated their willingness to accept vaccination) as well as those who had not (or who indicated intention to refuse vaccination). All women who agreed to participate in the study were recruited and our sampling strategy was not stratified by any predetermined demographic or other criteria, however we continued to recruit until we had sampled women of varying vaccination status. Participants were recruited until no more new information was being elicited, or when the data reached saturation.37
Data were analyzed using iterative thematic analysis techniques38,39 to enable an understanding of the participant's experiences, processes occurring and reasons for participant responses.39 This iterative process allowed movement between data collection and analysis as codes were interpreted and themes generated. The transcripts were read and reread and initial codes assigned based on the language used by the participants themselves. These codes were organized into meaningful groups as the analysis continued and codes were combined or new codes added as each interview was coded. Discussion between researchers, coding notes and memos were used to ensure consistency in the coding framework. Initial themes were identified by discussion between the researchers and matrixes, grids and tables were used to visualize the relationships between the themes and the experiences of each of the women interviewed to try to understand the decision-making process.39 Common elements of the decision-making processes were identified and a diagrammatic representation created (see Fig. 1). As we discussed and refined this we recognized that key elements of the Health Belief Model were evident and from this point onward we used that model to help structure the analysis. While there are other models which could be used to examine decision-making we found that the Health Belief Model fitted well with the themes we identified since we were interested in what the participants had done and would do, in particular what might explain their health behavior in relation to pregnancy vaccination as well as how they came to make decisions about health-care during pregnancy. The HBM has been used previously to examine vaccine decision-making.24,28,40,41
The study was approved by the Women's and Children's Health Network (WCHN) Human Research Ethics Committee.
Disclosure of Potential Conflicts of Interest
HM would like to declare she has support from a National Health and Medical Research Council Career Development Fellowship No. 1016272. HM is also principal investigator on a number of studies sponsored by vaccine manufacturers such as GlaxoSmithKline, Pfizer and Sanofi and is a member of vaccine advisory boards.
Acknowledgments
We would like to thank the pregnant mothers who gave up their time to participate in this study. Preliminary findings were presented by JC at the Public Health Association of Australia's National Immunisation Conference, Darwin, June 2012.
Funding
We acknowledge project funding support from SA Health.
References
- 1.Department of Health and Ageing The Australian Immunisation Handbook 10th Edition 2013 Canberra, Australia, 2013. [Google Scholar]
- 2.Centers for Disease Control and Prevention Summary of Recommendations for Adult Immunizations. http://www.immunize.org/catg.d/p2011.pdf, 2012. Available from: http://www.immunize.org/catg.d/p2011 [Google Scholar]
- 3.National Health Service Whooping cough vaccination in pregnancy. In: NHS, ed Pregnancy and baby: National Health Service, 2012. Available at: http://www.nhs.uk/conditions./pregnancy-and-baby/pages/whooping-cough-vaccination-pregnant.aspx. [Google Scholar]
- 4.Wendelboe AM, Njamkepo E, Bourillon A, Floret DD, Gaudelus J, Gerber M, Grimprel E, Greenberg D, Halperin S, Liese J, et al. . Transmission of Bordetella pertussis to young infants. Pediatr Infec Dis J 2007; 26:293-9; PMID:17414390; http://dx.doi.org/ 10.1097/01.inf.0000258699.64164.6d [DOI] [PubMed] [Google Scholar]
- 5.Grizas AP, Camenga D, Vazquez M. Cocooning: a concept to protect young children from infectious disease. Curr Opin Pediatr 2012; 24:92-7; PMID:22157361; http://dx.doi.org/ 10.1097/MOP.0b013e32834e8fe9 [DOI] [PubMed] [Google Scholar]
- 6.Healy CM, Rench MA, Baker CJ. Implementation of cocooning against pertussis in a high-risk population. Clin Infect Dis 2011; 52:157-62; PMID:21288837; http://dx.doi.org/ 10.1093/cid/ciq001 [DOI] [PubMed] [Google Scholar]
- 7.Cooper Robbins SC, Leask J, Hayles EH, Sinn JKH. Midwife attitudes: An important determinant of maternal postpartum pertussis booster vaccination. Vaccine 2011; 29:5591-4; PMID:21624420; http://dx.doi.org/ 10.1016/j.vaccine.2011.05.049 [DOI] [PubMed] [Google Scholar]
- 8.Coudeville L, Van Rie A, Andre P. Adult pertussis vaccination strategies and their impact on pertussis in the United States: Evaluation of routine and targeted (cocoon) strategies. Epidemiol Infect 2008; 136:604-20; PMID:17612417; http://dx.doi.org/ 10.1017/S0950268807009041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Rie A, Hethcote HW. Adolescent and adult pertussis vaccination:Computer simulations of five new strategies. Vaccine 2004; 22:3154-65; PMID:15297068; http://dx.doi.org/ 10.1016/j.vaccine.2004.01.067 [DOI] [PubMed] [Google Scholar]
- 10.Munoz F, Englund J. Infant Pertussis: Is Cocooning the answer? Clin Infect Dis 2011; 53:893-6; PMID:21946188; http://dx.doi.org/ 10.1093/cid/cir542 [DOI] [PubMed] [Google Scholar]
- 11.Håberg SE, Trogstad L, Gunnes N, Wilcox AJ, Gjessing HK, Samuelsen SO, Skrondal A, Cappelen I, Engeland A, Aavitsland P, et al. . Risk of Fetal Death after Pandemic Influenza Virus Infection or Vaccination. New England J Med 2013; 368:333-40; http://dx.doi.org/ 10.1056/NEJMoa1207210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierce M, Kurinczuk JJ, Spark P, Brocklehurst P, Knight M. Perinatal outcomes after maternal 2009/H1N1 infection: national cohort study. British Med J 2011; 342:d3214; PMID:21672992; http://dx.doi.org/ 10.1136/bmj.d3214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acs N, Banhidy F, Puho E, Czeizel AE. Maternal influenza during pregnancy and risk of congenital abnormalities in offspring. Birth Defects Res Part A 2005; 73:989-96; http://dx.doi.org/ 10.1002/bdra.20195 [DOI] [PubMed] [Google Scholar]
- 14.de Greeff SC, Mooi FR, Weterhof A, Verbakel JMM, Peeters MF, Heuvelman CJ, Notermans DW, Elvers LH, Schellekens JF, de Melker HE. Pertussis disease burden in the household: How to protect young infants. Clin Infect Dis 2010; 50:1339-45; PMID:20370464; http://dx.doi.org/ 10.1086/652281 [DOI] [PubMed] [Google Scholar]
- 15.Wiley KE, Massey PD, Cooper SC, Wood N, Leask J. Pregnant women's intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: A cross sectional survey. Vaccine 2013; 31:3972-8; PMID:23777954; http://dx.doi.org/ 10.1016/j.vaccine.2013.06.015 [DOI] [PubMed] [Google Scholar]
- 16.Lu AB, Halim AA, Dendle C, Kotsanas D, Giles ML, Wallace EM, Buttery JP, Stuart RL. Influenza vaccination uptake amongst pregnant women and maternal care providers is suboptimal. Vaccine 2012; 30:4055-9; PMID:22521842; http://dx.doi.org/ 10.1016/j.vaccine.2012.04.012 [DOI] [PubMed] [Google Scholar]
- 17.Australian Government Department of Health and Ageing. Immunization Coverage Data. Available at: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/acir-curr-data.htm. [Google Scholar]
- 18.Yeh S, Mink C, Kim M, Naylor S, Zangwill KM, Allred NJ. Effectiveness of hospital-based postpartum procedures on pertussis vaccination among postpartum women. Am J Obstetr Gynecol 2014; 210:e1-6; PMID:24096180 [DOI] [PubMed] [Google Scholar]
- 19.Cheng P-J, Huang S-Y, Shaw S-W, Kao C-C, Chueh H-Y, Chang S-D, Hsu TY, Kung FT, Hsieh TT. Factors influencing women's decisions regarding pertussis vaccine: A decision-making study in the Postpartum Pertussis Immunization Program of a teaching hospital in Taiwan. Vaccine 2010; 28:5641-7; PMID:20600516; http://dx.doi.org/ 10.1016/j.vaccine.2010.05.078 [DOI] [PubMed] [Google Scholar]
- 20.Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Educ Res 2006; 22:166-76; PMID:16855015 [DOI] [PubMed] [Google Scholar]
- 21.Rossman Beel E, Rench MA, Montesinos DP, Mayes B, Healy CM. Knowledge and attitudes of postpartum women toward immunization during pregnancy. Human Vacines and Immunother 2013; 9:1-6; http://dx.doi.org/ 10.4161/hv.23606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taksdal SE, Mak DB, Joyce S, Tomlin S, Carcione D, Armstrong PK, Effler PV. Predictors of uptake of influenza vaccination: A survey of pregnant women in Western Australia. Aust Fam Physician 2013; 42:582-6; PMID:23971070 [PubMed] [Google Scholar]
- 23.Wiley KE, Massey PD, Cooper SC, Wood N, Ho J, Quinn HE, Leask J. Uptake of influenza vaccine by pregnant women: a cross-sectional survey. Med J Aust 2013; 198:373-5; PMID:23581957; http://dx.doi.org/ 10.5694/mja12.11849 [DOI] [PubMed] [Google Scholar]
- 24.Henninger M, Naleway A, Crane B, Donohue J, Irving S. Predictors of seasonal influenza vaccination during pregnancy. Obstet Gynecol 2013; 121:741-9; PMID:23635673; http://dx.doi.org/ 10.1097/AOG.0b013e3182878a5a [DOI] [PubMed] [Google Scholar]
- 25.Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, Vincent CA, Fraser G, Sevdalis N. Factors underlying parental decisions about combination childhood vaccinations including MMR: A systematic review. Vaccine 2010; 28:4235-48; PMID:20438879; http://dx.doi.org/ 10.1016/j.vaccine.2010.04.052 [DOI] [PubMed] [Google Scholar]
- 26.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014; 32:2150-9; PMID:24598724; http://dx.doi.org/ 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- 27.Crabb S, LeCouteur A. 'Fiona Farewells her breasts': A popular magazine account of breat cancer prevention. Critical Public Health 2006; 16:5-18; http://dx.doi.org/ 10.1080/09581590600601957 [DOI] [Google Scholar]
- 28.Meharry P, Colson E, Grizas A, Stiller R, Vázquez M. Reasons Why Women Accept or Reject the Trivalent Inactivated Influenza Vaccine (TIV) During Pregnancy. Matern Child Health J 2013; 17:156-64; PMID:22367067; http://dx.doi.org/ 10.1007/s10995-012-0957-3 [DOI] [PubMed] [Google Scholar]
- 29.Sim JA, Ulanika AA, Katikireddi SV, Gorman D. ‘Out of two bad choices, I took the slightly better one’: Vaccination dilemmas for Scottish and Polish migrant women during the H1N1influenza pandemic. Public Health 2011; 125:505-11; PMID:21802701; http://dx.doi.org/ 10.1016/j.puhe.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 30.Fabry P, Gagneur A, Pasquir J-C. Determinants of A (H1N1) vaccination: Cross-sectional study in a population of pregnant women in Quebec. Vaccine 2011; 29:1824-9; PMID:21219988; http://dx.doi.org/ 10.1016/j.vaccine.2010.12.109 [DOI] [PubMed] [Google Scholar]
- 31.Athearn PN, Kendall PA, Hillers V, Schroeder M, Bergmann V, Chen G, Medeiros LC. Awareness and acceptance of current food safety recommendations during pregnancy. Matern Child Health J 2004; 8:149-62; PMID:15499871; http://dx.doi.org/ 10.1023/B:MACI.0000037648.86387.1d [DOI] [PubMed] [Google Scholar]
- 32.Tooher R, Middleton P, Crowther C. A thematic analysis of factors influencing recruitment to maternal and perinatal trials. BMC Pregnancy and Childbirth 2008; 8:36; PMID:18687110; http://dx.doi.org/ 10.1186/1471-2393-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fridman D, Steinberg E, Azhar E, Weedon J, Wilson TE, Minkoff H. Predictors of H1N1 vaccination in pregnancy. Am J Obstet Gynecol 2011; Supplement to June:S124-S7; PMID:21640229; http://dx.doi.org/ 10.1016/j.ajog.2011.04.011 [DOI] [PubMed] [Google Scholar]
- 34.Webb H, Street J, Marshall HS. Incorporating immunizations into routine obstetric care to facilitate Health Care Practitioners in implementing maternal immunization recommendations. Human Vacin Immunother 2014; 10:0-1; PMID:24509790; http://dx.doi.org/ 10.4161/hv.27893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroelinger CD, Oths KS. Partner Support and Pregnancy Wantedness. Birth 2000; 27:112-9; PMID:11251489; http://dx.doi.org/ 10.1046/j.1523-536x.2000.00112.x [DOI] [PubMed] [Google Scholar]
- 36.Patton MQ. Qualitative evaluation and research methods. Thousand Oaks, CA: Sage Publications, Inc, 1990 [Google Scholar]
- 37.Kvale S, Brinkmann S. InterViews: Learning the Craft of Qualitative Research Interviewing. Thousand Oaks: Sage Publication, Inc, 2008. [Google Scholar]
- 38.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research In Psychology 2006; 3:77-101; http://dx.doi.org/ 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 39.Hansen EC. Successful Qualitative Health Research: A practical introduction. Bershire, England: Open University Press, 2006. [Google Scholar]
- 40.Chen M-F, Wang R-H, Schneider JK, Tsai C-T, Jiang DD-S, Hung M-N, et al. . Using the Health Belief Model to Understand Caregiver Factors Influencing Childhood Influenza Vaccinations. J Commun Health Nursing 2011; 28:29-40; PMID:21279888; http://dx.doi.org/ 10.1080/07370016.2011.539087 [DOI] [PubMed] [Google Scholar]
- 41.Smith P, Humiston S, Marcuse E, Zhao Z, Dorell C, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Reports 2011; 126:135-46; PMID:21812176 [DOI] [PMC free article] [PubMed] [Google Scholar]


