Abstract
A new meningococcal serogroup B vaccine (4CMenB) has recently been licensed. This study assessed the acceptability of 4CMenB vaccine among parents and healthcare workers (HCWs). From May to July 2013 in Milan, Italy, self-administered questionnaires were distributed to 2050 parents of infants presenting at immunization clinics for the mandatory hexavalent vaccination and submitted to 350 HCWs involved in immunization practices.
1842 parents (89.1%) responded to the survey; 64.4% of parents wanted their child to receive the 4CMenB vaccine and 5.1% would not vaccinate their children. Multivariate analysis showed that recognition of the severity of meningitis [a life threatening vs a mild or unthreatening disease (Odds ratio (OR): 2.3; confidence interval (CI): 1.4–3.6], awareness of vaccination as a beneficial preventive measure (very beneficial vs not beneficial OR = 6.4; CI 3.0–13.7) and knowledge of the Meningococcal C vaccine (OR = 1.4; CI 1.1–1.8) were strongly associated to willingness to receive 4CMenB vaccine. On the contrary, level of education was associated with refusal of immunization (university vs education level lower than middle school OR = 0.68; CI 0.47–0.97). Among the parents who were willing to immunize their children, 66.9% would agree with three injections to be administered during the same visit. A total of 291 HCWs (83.1%) agreed to participate in the survey; 73% considered 4CMenB vaccine a priority in infants’ immunization schedule; 26.8% of HCWs suggested the concomitant administration with routine infant immunization.
Parental and HCWs acceptability of 4CMenB vaccine was high. Increasing knowledge about meningitis and vaccine prevention might further increase the acceptability of this vaccine.
Keywords: healthcare providers, meningococcal B, parents, survey, vaccine
Abbreviations
- CI
confidence interval
- HCWs
health care workers
- MenB
meningococcal serogroup B
- MenC
Meningococcal serogroup C
- OR
odds ratio
Introduction
Neisseria meningitidis remains a serious public health problem worldwide with an annual number of invasive disease cases estimated to be at least 1.2 million, even if the incidence of meningococcal disease has decreased in many developed countries in the past decade.1,2 The decline is in part related to the introduction of new polysaccharide-protein conjugate vaccines (serogroup C meningococcal vaccine; serogroups A, C, Y and W-135 multivalent meningococcal vaccine). In particular, the introduction for routine use of the conjugate serogroup C meningococcal vaccine has dramatically changed the epidemiology of the disease, leaving serogroup B as the predominant cause of invasive meningococcal disease in Europe, Latin America and Northern America.3,4 The incidence of meningococcal B infection is estimated to be between 20,000 and 80,000 cases per year worldwide, with a 10% fatality rate even with appropriate treatment.5 The highest incidence is seen in infants less than one year of age, in adolescents and young adults.
In Italy, meningococcal serogroup B is the most frequent cause of bacterial meningitis at paediatric age, with the highest incidence reported in children younger than 24 months of age (peaking at 4–8 months of age).6
In 2013, a new-generation MenB vaccine (4CMenB) was licensed in the European Union, USA, Canada and Australia.7,8 Nevertheless, substantial debates surround the introduction of 4CMenB into immunization programmes.9 Concerns have been raised regarding the vaccine's effectiveness, its safety when administered with routine infant vaccines and the cost-effectiveness of a large-scale vaccine introduction.10,11 Regarding vaccine effectiveness it is not clear if the predicted vaccine coverage (ranges between 73% and 87% in Europe) will be confirmed in post-licensure studies, if 4CMenB will prevent carriage, and therefore provide herd immunity, and how long the protection will persist.12,13 These data are crucial to estimate the cost-effectiveness of infant immunization programme. Regarding vaccine safety, the overall fever rates were reported to be higher when 4CMenB vaccine is given concomitantly with routine vaccines.11
In Italy, 4CMenB was licensed by Italian Pharmaceutical Agency in May 2013 with a 3+1 schedule in infants aged from 3 to 5 months, 2+1 schedule from 6 to 23 months and 2 dose schedule in children >2 years. However considering the epidemiological picture of MenB meningitis in Italy, 3+1 immunization schedule seems the most logical strategy. The inclusion of the new 4CMenB in the current Italian infant immunization schedule, which consists of hexavalent and pneumococcal 13-valent vaccines given at 3, 5 and 11 months, may require an increase in the number of injections per session or in the number of visits, raising the possibility of higher discomfort levels for both child and parents. Moreover, adding a new vaccine to the routine infant immunization schedule could potentially adversely affect parental acceptance of the routine infant immunization program.
Currently, few studies have focused on attitudes towards and acceptance of the 4CMenB vaccine among parents and health care workers (HCWs).14-16 Therefore, we performed a survey with the aim of generating information about knowledge and attitudes towards meningococcal serogroup B infection and the acceptability of 4CMenB vaccine among a sample of parents and HCWs in Italy.
Results
A total of 2050 questionnaires were distributed to parents during the study period; 1842 questionnaires (89.8%) were filled in and returned, 97% of which answered more than 70% of the questions provided.
A total of 350 HCWs received questionnaires: 291 (83.1%) agreed to participate in the survey and returned the questionnaire with more than 70% of questions answered.
Table 1 summarizes the socio-demographic characteristics of the study population.
Table 1.
Characteristics of the study population
| Characteristics of parents | N | % |
|---|---|---|
| Parent | ||
| Mother | 1428 | 78.68 |
| Father | 283 | 15.59 |
| Both | 104 | 5.73 |
| Age (years) | ||
| ≤ 25 | 127 | 6.97 |
| 26–40 | 1438 | 78.97 |
| >40 | 256 | 14.06 |
| Nationality | ||
| Italian | 1387 | 76.13 |
| Non-Italian | 424 | 23.27 |
| Two nationalities including Italian | 11 | 0.6 |
| Number of children (a) | ||
| 1 | 943 | 55.7 |
| 2 | 601 | 35.5 |
| >3 | 149 | 8.8 |
| Mother education attainment | ||
| Primary school/none | 17 | 0.96 |
| Middle school | 250 | 14.16 |
| High school | 659 | 37.34 |
| Degree | 838 | 47.54 |
| Father education attainment (b) | ||
| Primary school/none | 26 | 1.83 |
| Middle school | 243 | 17.14 |
| High school | 538 | 37.94 |
| Degree | 611 | 43.09 |
| Employment of mother | ||
| Yes | 1302 | 74,19 |
| No | 453 | 25.81 |
| Employment of father (c) | ||
| Yes | 1552 | 91.89 |
| No | 137 | 8.11 |
| Information about child | ||
| Age (months, SD) | 8,3 | 14 |
| Being firstborn (N; %) (d) | 996 | 57.71 |
| Health care workers | N | % |
| Gender | ||
| Male | 39 | 13.73 |
| Female | 245 | 86.27 |
| Age (years) | ||
| ≤ 35 | 17 | 6.09 |
| 36-50 | 72 | 25.81 |
| >50 | 190 | 68.10 |
| Qualification | ||
| Specialist in Hygiene and Preventive Medicine | 15 | 5.41 |
| Paediatrician | 163 | 58,62 |
| Nurse | 100 | 35,97 |
| Occupational field | ||
| Immunization Clinic | 110 | 39,43 |
| Outpatient Clinic | 128 | 45.88 |
| Hospital | 16 | 5,73 |
| Other (Infectious Disease Clinic) | 25 | 8,96 |
N: number of subjects; SD: standard deviation. Percentages of missing data: (a) 8.09, (b) 23.02, (c) 8.31, (d) 6.30, . Missing data of the remaining items were <6.00.
Parent survey
The majority of parents were Italian-born (76.1%), mothers (78.7%), aged between 26 and 40 years (79%). High educational attainment (degree) was reported for 47.5% of mothers and 43% of fathers. Employment percentages for mothers and fathers were 74.2% and 91.9% respectively; however, the quality of data on fathers’ employment was quite poor, as a large amount (23%) was missing.
Table 2 shows the distribution of the parents’ answers concerning their personal knowledge of vaccination in general and of meningitis.
Table 2.
Parents’ knowledge of meningococcal infection and vaccination
| Items and questions | N | % |
|---|---|---|
| Perceived benefits of vaccination | ||
| Do you think that vaccinations in general are | ||
| Very beneficial in preventing infectious diseases | 1074 | 59.14 |
| Beneficial | 689 | 37.94 |
| Not beneficial | 6 | 0.33 |
| I do not have any opinion about that | 47 | 2.59 |
| Did you receive appropriate and useful information about vaccination in general? | ||
| Yes | 1556 | 85.40 |
| No | 266 | 14.60 |
| If yes, did you receive information froma | ||
| Paediatrician | 907 | 60.07 |
| Immunization Clinic | 853 | 56.49 |
| Prenatal classes | 85 | 5.63 |
| Friends | 127 | 8.41 |
| Internet | 189 | 12.52 |
| Books and magazines | 70 | 4.64 |
| Knowledge about meningitis | ||
| Have you heard of meningitis? | ||
| I have never heard of meningitis | 303 | 16.98 |
| My knowledge of meningitis is poor | 954 | 53.48 |
| My knowledge of meningitis is fair | 434 | 24.33 |
| My knowledge of meningitis is good | 93 | 5.21 |
| Knowledge about etiology of meningitis | ||
| Do you know that meningococcal meningitis is caused by serogroup B and C? | ||
| Yes | 599 | 34.15 |
| No | 1155 | 65.85 |
| Recognition of severity of meningitis | ||
| How severe do you think meningitis could be? | ||
| Unthreatening disease | 56 | 3.23 |
| A mild disease | 76 | 4.38 |
| A severe disease | 293 | 16.89 |
| A life-threatening disease | 1310 | 75.50 |
| Do you know that a Meningococcal C vaccine is approved for immunization? | ||
| Yes | 967 | 54.82 |
| No | 797 | 45.18 |
aMore than one response was permitted.
More than 95% of parents thought that vaccination is a beneficial or very beneficial preventive measure. The majority of parents (85.4%) declared they had received appropriate and useful information about vaccination, mostly from their pediatrician or from HCWs working in immunization clinics (Table 2).
Almost 71% of parents reported no or poor knowledge about meningitis (respectively 17% and 53.5%); 24.3% of parents had a fair knowledge of meningitis, while only 5.2% reported a good knowledge. In all, 75.5% of parents consider meningitis a life threatening-disease, whereas only 34.1% of parents stated they were aware of the aetiology of meningitis. Almost half of the parents (54.8%) knew that vaccination against meningococcal serogroup C (MenC) is included in the immunization program in Italy.
Poor knowledge about meningitis was associated with non-Italian nationality (p < 0.0001), mother's lower educational attainment, primipary and being unemployed at the time of the study (p < 0.0001, p = 0.0021 and p = 0.0009 respectively). Lack of knowledge about aetiology of meningitis was associated with younger age of parents (p = 0.0107), mother's lower educational attainment (p = 0.0050) and primipary (p < 0.0001). Lower perception of meningitis severity was associated with younger (p < 0.0001) and non-Italian (p < 0.0001) parents, mother's lower educational attainment (p < 0.0001) and unemployed mother and father (p < 0.0001 both).
A total of 1143 parents (64.39%) were favorable towards vaccinating their children against MenB, 30.5% didn't express any opinion and only 5.1% stated that they would not vaccinate their children.
When father's employment status was not reported, responses about the acceptability of 4CMenB vaccine showed a distribution very similar to those of unemployed fathers. We therefore considered “no response” as informative and a new level of the variable regarding parental employment in the logistic regression.
The results of univariable analysis are reported in Table 3. At multivariable analysis the acceptability of 4CMenB was positively affected by perception of vaccination benefit and knowledge of a previously licensed MenC vaccine (Table 3).
Table 3.
Univariate and multivariate correlates of 4CMenB vaccine acceptability among parents
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | |
| Parent | 0.0656 | 0.1556 | ||
| father vs mother | 1.368 (0.857–2.182) | 1.294 (0.742–2.257) | ||
| both vs mother | 0.784 (0.600–1.023) | 0.768 (0.558–1.057) | ||
| Age | 0.6013 | |||
| 26-40 years vs<= 25 years | 0.836 (0.561–1.247) | |||
| > 40 years vs<= 25 years | 0.789 (0.496–1.255) | |||
| Nationality | 0.1210 | |||
| non-Italian vs Italian/both | 1.209 (0.951–1.536) | |||
| Mother education | 0.0017 | 0.0005 | ||
| High school vs middle school or lower | 1.192 (0.875–1.623) | 1.087 (0.756–1.563) | ||
| Degree vs middle school or lower | 0.802 (0.597–1.076) | 0.678 (0.474–0.971) | ||
| Mother employment | 0.4964 | |||
| employed vs unemployed | 0.887 (0.705–1.116) | |||
| doesn't respond vs unemployed | 1.057 (0.635–1.757) | |||
| Father employment | 0.0043 | 0.0824 | ||
| employed vs unemployed | 0.597 (0.398–0.896) | 0.701 (0.427–1.150) | ||
| doesn't respond vs unemployed | 0.939 (0.550–1.601) | 1.069 (0.567–2.013) | ||
| Perceived benefits of vaccination | <.0001 | <.0001 | ||
| very beneficial vs not beneficial/not having any opinion | 9.463 (4.871–18.384) | 6.401 (2.984–13.731) | ||
| Beneficial vs not beneficial/not having any opinion | 3.331 (1.711–6.486) | 2.682 (1.250–5.755) | ||
| Appropriate information – yes vs no | 0.0086 | 1.434 (1.096–1.877) | 0.4740 | 0.889 (0.645–1.226) |
| Knowledge about meningitis | <0.0001 | 0.0474 | ||
| good vs poor or none | 2.498 (1.489–4.191) | 1.684 (0.943–3.006) | ||
| fair vs poor or none | 1.641 (1.293–2.084) | 1.349 (1.014–1.794) | ||
| Knowledge about aetiology of meningitis - yes vs no | <0.0001 | 1.594 (1.288–1.973) | 0.1868 | 1.203 (0.914–1.583) |
| Recognition of severity of meningitis | <0.0001 | <0.0001 | ||
| Life threatening vs mild/unthreatening disease | 1.885 (1.299–2.735) | 2.288 (1.443–3.626) | ||
| Severe vs mild/unthreatening disease | 0.911 (0.598–1.388) | 1.322 (0.795–2.198) | ||
| Knowledge of a previously licensed MenC vaccine | ||||
| yes vs no | <0.0001 | 1.593 (1.308–1.941) | 0.0063 | 1.397 (1.099–1.775) |
OR: odds ratio; IC: confidence interval; Men C vaccine: vaccine against meningococcal serogroup C.
Considering meningitis a life-threatening disease is also associated with higher acceptability of 4CMenB vaccine, compared to considering meningitis unthreatening or a mild disease. On the contrary, in mothers a high level of education (university) was associated with less acceptability of 4CMenB vaccination, vs middle school or a lower level of education. Comparison of mothers with degrees and those with high school education showed that higher education level was associated with less willingness toward vaccination against MenB (p = 0.0002 OR = 0.624 95% IC = 0.488–0.798; contrast not reported in table).
Acceptability of 4CMenB vaccine was associated with knowledge about meningitis, although with a p-value near 0.05; fair self-reported knowledge is more associated with willingness to receive this vaccine than poor or no knowledge. The odds ratio (OR) confidence interval of very good versus poor or no knowledge varies from 0.943 to 3.006 and is non-significant even if it is shifted beyond 1. The very low number of parents that declared a thorough understanding of meningitis could have influenced this result.
Among the parents willing to vaccinate their child with 4CMenB, 66.9% would like to accept concomitant vaccination with routine infant immunization, whereas 11.3% would not and 21.8% expressed no opinion.
HCWs survey
Overall, the interviewed HCWs were mainly women (86.3%), aged over 35 years old (25.8% aged between 36 and 50 years old, 68.1% more than 50 years old). Paediatricians made up 58.6% of HCWs, followed by nurses (27.3%). A total of 128 (45.9%) HCWs worked in outpatient clinics, whereas 110 worked in immunization clinics (39.4%) (Table 1).
Attitudes towards meningitis and vaccine prevention among HCWs are represented in Figure 1.
Figure 1.
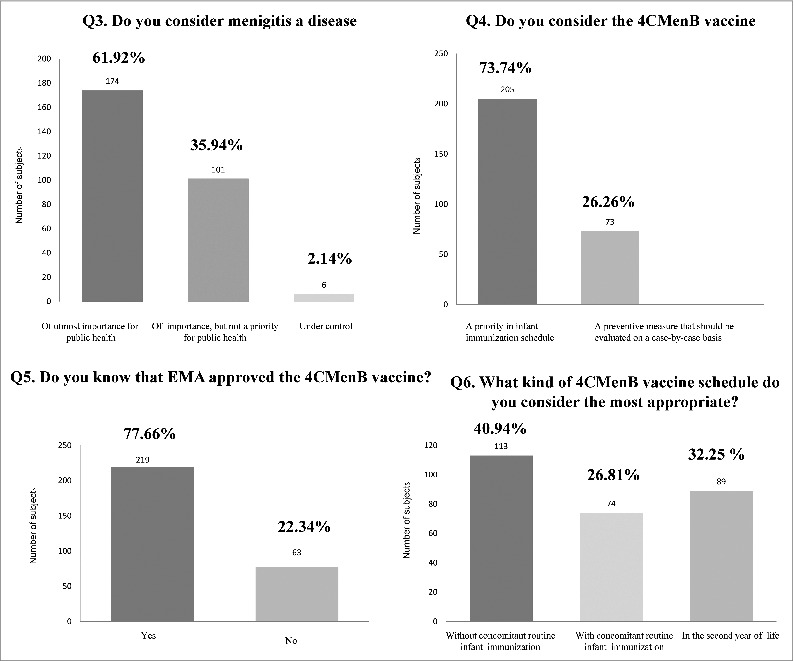
Attitudes towards meningitis and vaccine prevention among HCWs.
More than 80% of HCWs thought that meningitis is a disease with high (56.9%) or very high (23.3%) mortality rate and with high (65.4%) or very high risk of causing permanent damage (20.7%). The majority of HCWs (61.9%) thought that meningitis is a disease of utmost importance for public health, while 35.94% thought that although important, meningitis is not a public health priority. The majority of HCWs (77.6%) had received information about the European Medical Agency approval of 4CMenB and 73% considered the new 4CMenB vaccine a priority in infants’ immunization schedule, while 26.3% agreed that immunization with this vaccine should be evaluated on a case-by-case basis. None of HCWs considered 4CMenB vaccine an unnecessary preventive measure.
When asked which schedule is considered the most appropriate, only 26.8% of HCWs suggested the concomitant administration of 4CMenB with routine infant immunization, whereas 32.2% suggested immunization at two years of age (Fig. 1).
Paediatricians considered meningitis a disease with a higher mortality rate risk than non-paediatricians (p = 0.0006); they also considered 4CMenB vaccination a priority for all newborns unlike non-paediatricians (p = 0.0248). 4CMenB vaccine was known by paediatricians more than by other HCWs (p = 0.0163).
Discussion
This survey provides a snapshot of HCWs’ and parents’ knowledge regarding meningococcal serogroup B infection and acceptability of the 4CMenB vaccine soon after its recent European Medical Agency licensure.
In our large sample of Italian parents, acceptability of 4CMenB vaccine was relatively high: 64.3% of parents were favorable towards vaccinating their children against MenB, whereas only 5.1% stated that they would not vaccinate their children. Similar data was reported by a multinational survey conducted in seven countries around the globe, confirming initial positive acceptance of this new vaccine worldwide.15 Higher acceptability was reported in a recent Australian survey, where more than 80% of parents stated they wanted their children to receive the 4CMenB vaccine.14 This between-country difference in parental vaccine acceptability is not unexpected. Different factors, such as ethnicity, socio-demographic and psychosocial factors, perceptions about disease severity and susceptibility and mistrust of the medical profession are known to influence parental vaccine uptake in different settings.17-21 Moreover, the so called “national culture perspective on vaccination”, which includes varied and deep-seated beliefs as result of the tension between divergent cultural viewpoints and value systems, is considered to play an important role in this field.22 Therefore understanding community acceptance of a new vaccine and barriers to immunization at the national level is an essential tool for Health Authorities and immunization policy providers.
A considerable amount of parents (30.5%) did not express any opinion about having their child vaccinated with 4CMenB. Considering that acceptability of 4CMenB vaccine was higher in parents who believed that meningitis is a life threatening disease and that vaccinations are a beneficial or very beneficial preventative measure, adequate educational programs aiming to underline benefits of vaccination and to increase the awareness of outcomes of meningitis might increase the acceptability of this vaccination. Interestingly, being a graduate was associated with refusal of immunization. This association was reported in other studies demonstrating that children whose parents refused all vaccines were significantly more likely to have a college-graduate mother and to live in a household with a higher annual family income.23-25 The lower compliance with vaccine recommendations in parents of higher educational level probably reflects their easier access to various information sources, increasing their concern about vaccine safety. Considering the increased educational levels in Italy in the past decades, effort should be made to understand the deeper reasons for this association.26
The majority of parents willing to vaccinate their children would like to accept three injections during the same visit. However, our questionnaire did not provide a detailed description of the main vaccine-related adverse events; therefore the acceptability of this schedule could have been overestimated.
From the HCWs’ perspective, the majority of HCWs would include the 4CMenB vaccine in the national infant and children immunization schedule and prefer to give 4CMenB vaccine separately from other vaccines. These results probably reflects two main concerns, even if no specific questions were addressed to examine the reason for their choice. The first is about safety: clinical trials suggest that the frequency of fever following routine infant immunizations would be expected to substantially increase if 4CMenB is given with other routine infant immunizations, and this could reduce the uptake of this vaccine.11 The second is the potential reduction in parental acceptance of the routine infant immunization program if an additional injection in the same visit is introduced.
The strengths of this study is that this survey explores the attitudes towards a vaccine not yet introduced into routine immunization program in a large parent population and in a sample of HCWs. In our knowledge no data are currently available on this topic in Italy. The very high participation rate probably reflect the considerable interest in this survey. The limitations of this study include: a) our sample was not representative of the general Italian population, because recruitment was limited to one Italian region; b) we missed about the 5% of parents who do not usually attend the immunization clinics (these parents probably do not have positive attitudes towards vaccinations); c) the information was gathered by a self-reported questionnaire; thus, some responses were missed. Moreover we did not investigate the parents’ perception of the risk of long-term sequelae as an additional measure of their knowledge about meningitis and we did not explore how the increased reactogenity of 4CMenBgiven concomitantly with other vaccines might have affected vaccine uptake.
In conclusion parental and HCWs acceptability of 4CMenB vaccine was high. A tailored parental educational program focused on increasing knowledge about outcomes of meningitis and vaccine prevention might increase the acceptability of this vaccine.
Materials and Methods
This study was conducted between May and July 2013 in the metropolitan area of Milan, Northern Italy.
We designed a cross-sectional survey, divided into two sections. One section involved parents of infants aged 3 to 12 months, and the second consisted of HCWs regularly involved in immunization practice or infant care. The questionnaires were developed by a multidisciplinary team including pediatricians and specialists in Hygiene and Preventive Medicine and were pilot-tested on a convenience sample of parents and HCWs attending the outpatient clinic of the Luigi Sacco Hospital in order to ensure clarity and ease of administration.
The study was approved by the Ethics Committee of Luigi Sacco Hospital, Milan, Italy.
Parent survey
In Italy some childhood vaccinations are mandatory, in particular vaccines against hepatitis B, poliomelitis, diphteria and tetanus, are included into the hexavalent vaccination. The current national immunization program is carried out through immunization clinics within the Italian National Health Service, which bears the cost of mandatory vaccines. Less than 5% of parents opt for immunization in outpatient setting. In Milan area, 17 immunization clinics guarantee childhood vaccinations, and the mean coverage of hexavalent vaccination is similar to the regional and national coverage (95%, data unpublished).
In order to interview the great majority of parents living in Milan area, a self-administered anonymous questionnaire (see online supplement) was offered by a study investigator to all parents or legal guardians who accompanied their infant to one of the 17 immunization clinics of the Milan area for hexavalent vaccination. Parents were approached by a research assistant in the waiting rooms of the immunization clinic asking if they would be willing to complete a survey about meningitis and vaccine prevention in children. If they agreed, they were moved to a private room or quiet area of the waiting room where the study was explained in detail. Each questionnaire was also accompanied by a formal letter describing the aims of the study, and explaining how to complete the questionnaire. A brief introduction on 4CMenB vaccine (composition, licensure in Italy and doses required in the first year of age) was presented at the beginning of each questionnaire. Parents had to return the questionnaire to the member of the research team before leaving the immunization clinic. The questionnaire was multi-sectional, consisting of 16 items with closed-ended questions (each item can be answered as follows: 'yes', 'no', 'don't know' or using an intensity or comparison scale according to the different questions). The first section of the questionnaire evaluated parents’ demographic and socioeconomic characteristics, including sex, age, nationality, education, employment and number and age of siblings. The second section investigated the parents’ attitudes towards vaccinations in general, the perceived benefits of vaccinations and self-reported knowledge on meningitis and meningitis prevention, with a particular focus on meningococcal meningitis. Lastly, the third section evaluated parental willingness to have their children vaccinated with the new 4CMenB vaccine and the acceptability of different vaccine schedules (with or without concomitant routine infant vaccinations).
Health care workers survey
A self-administered anonymous multi-sectional questionnaire was distribute to 2/3 of HCWs (350) randomly selected from a list of about 500 pediatricians, nurses and specialists in Hygiene and Preventive Medicine operating in Milan area and affiliated to the Italian National Health System via an email invitation that included a link to a Web-based survey. The first web page described the aims of the study, and explained how to complete the questionnaire. In Italy HCWs included in our survey are directly involved in immunization practices: pediatricians usually discuss with parents the role of vaccination in childhood, specialists in Hygiene and Preventive Medicine and nurses work in immunization clinics. The questionnaire was composed of two sections with a total of 10 closed-ended questions (each item can be answered as follows: 'yes', 'no', 'don't know' or using an intensity scale or selecting 3 different options according to the different questions).
The first section described age, job title and employment. The second section evaluated the self-reported knowledge of meningococcal disease (epidemiology, lethality, morbidity), personal perception of the public importance of meningococcal B diseases and perceived priority of preventing infection. Finally, opinions about the most appropriate 4CMenB vaccination schedule were investigated.
Statistical analysis
Descriptive analysis of variables collected through parents’ and HCWs’ questionnaires were given by absolute number and percentages. Association of knowledge about meningitis, aetiology of meningitis and awareness of outcomes with parents’ demographic characteristics was evaluated. Variables considered were: sex and age of respondent, nationality of parents, number of children, father's and mother's education and employment and being firstborn. Association was evaluated via chi-square or Fisher's exact test with a significance level of 0.05. Parents willing to have their children vaccinated against MenB were analysed using a logistic regression. Parents’ characteristics and their knowledge and perceptions of meningitis were considered as independent variables. Variables showing a proportion of missing data higher than 6% on the entire sample (see Table 1) were excluded from uni- and multivariable analyses. Through multivariable analysis we were interested to evaluate which variables affected parents' propensity to vaccinate their children. Therefore we performed a logistic regression on acceptability of 4CMenB vaccine recoding parents' responses into two groups: “Yes” and “No \ don't know”. Variables with a p-value higher than 0.10 in univariate analysis were included in the multivariate model.
Responses about risk associated with meningitis, importance of vaccine, knowledge about MenB vaccine and interest in widening knowledge were compared between paediatricians and other healthcare figures.
Analyses were performed using SAS 9.2 statistical software.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgment
We would particularly like to thank the many parents and health care workers without whose collaboration this study would not have been possible.
Funding
The statistical analysis was supported by a grant from Romeo and Enrica Invernizzi Foundation.
Supplemental Material
Supplemental data for this article can be accessed on the publisher's website.
References
- 1.McIntyre PB, O'Brien KL, Greenwood B, van de Beek D. Effect of vaccines on bacterial meningitis worldwide. Lancet 2012; 380:1703-11; PMID:23141619; http://dx.doi.org/ 10.1016/S0140-6736(12)61187-8 [DOI] [PubMed] [Google Scholar]
- 2.Jafri RZ, Ali A, Messonnier NE, Tevi-Benissan C, Durrheim D, Eskola J, Fermon F, Klugman KP, Ramsay M, Sow S, et al. . Global epidemiology of invasive meningococcal disease. Popul Health Metr 2013; 11:17; PMID:24016339; http://dx.doi.org/ 10.1186/1478-7954-11-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Racloz VN, Luiz SJ. The elusive meningococcal meningitis serogroup: a systematic review of serogroup B epidemiology. BMC Infect Dis 2010; 10:175; PMID:20565757; http://dx.doi.org/ 10.1186/1471-2334-10-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bettinger JA, Scheifele DW, Le Saux N, Halperin SA, Vaudry W, Tsang R; Members of Canadian Immunization Monitoring Program, Active (IMPACT) The disease burden of invasive meningococcal serogroup B disease in Canada. Pediatr Infect Dis J 2013; 32:e20-5; PMID:22926207; http://dx.doi.org/ 10.1097/INF.0b013e3182706b89 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Initiative for vaccine research, bacterial infections. Neisseria meningitidis. Available at: http://www.who.int/vaccine_research/diseases/soa_bacterial/en/index2.html. Accessed on March 15, 2010. [Google Scholar]
- 6.Azzari C, Canessa C, Lippi F, Moriondo M, Indolfi G, Nieddu F, Martini M, de Martino M, Castiglia P, Baldo V, et al. Distribution of invasive meningococcal B disease in Italian pediatric population: Implications for vaccination timing. Vaccine 2014; 32:1187-91; PMID:24120548; http://dx.doi.org/ 10.1016/j.vaccine.2013.09.055 [DOI] [PubMed] [Google Scholar]
- 7.EMA Authorization Details for Bexsero. Available at: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002333/human_med_001614.jsp&mid=WC0b01ac058001d124. Accessed 29th January 2014. [Google Scholar]
- 8.Australian Register of Therapeutic Goods Bexsero Public Summary. Available at: https://www.ebs.tga.gov.au/. Accessed 29th January 2014. [Google Scholar]
- 9.Granoff DM. Commentary: European Medicines Agency recommends approval of a broadly protective vaccine against serogroup B meningococcal disease. Pediatr Infect Dis J 2013; 32:372-3; PMID:23263177; http://dx.doi.org/ 10.1097/INF.0b013e318282942f [DOI] [PubMed] [Google Scholar]
- 10.Pouwels KB, Hak E, van der Ende A, Christensen H, van den Dobbelsteen GP, Postma MJ. Cost-effectiveness of vaccination against meningococcal B among Dutch infants: Crucial impact of changes in incidence Hum Vaccin Immunother 2013; 9:1129-38; PMID:23406816; http://dx.doi.org/ 10.4161/hv.23888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vesikari T, Esposito S, Prymula R, Ypma E, Kohl I, Toneatto D, Dull P, Kimura A; EU Meningococcal B Infant Vaccine Study group Immunogenicity and safety of an investigational multicomponent, recombinant, meningococcal serogroup B vaccine (4CMenB) administered concomitantly with routine infant and child vaccinations: results of two randomised trials. Lancet 2013; 381:825-35; PMID:23324563 [DOI] [PubMed] [Google Scholar]
- 12.English P. Vaccination against meningitis B: is it worth it? Drugs Context 2013; 2013:212246; PMID:24432035; http://dx.doi.org/ 10.7573/dic.212246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogel U, Taha MK, Vazquez JA, Findlow J, Claus H, Stefanelli P, Caugant DA, Kriz P, Abad R, Bambini S, et al. . Predicted strain coverage of a meningococcal multicomponent vaccine (4CMenB) in Europe: a qualitative and quantitative assessment. Lancet Infect Dis. 2013; 13:416-25; PMID:23414709: http://dx.doi.org/ 10.1016/S1473-3099 [DOI] [PubMed] [Google Scholar]
- 14.Marshall H, Clarke M, Sullivan T. Parental and community acceptance of the benefits and risks associated with meningococcal B vaccines. Vaccine 2014; 32:338-44; PMID:24269618; http://dx.doi.org/ 10.1016/j.vaccine.2013.11.042 [DOI] [PubMed] [Google Scholar]
- 15.Bakhache P, Rodrigo C, Davie S, Ahuja A, Sudovar B, Crudup T, Rose M. Health care providers' and parents' attitudes toward administration of new infant vaccines–a multinational survey. Eur J Pediatr. 2013; 172:485-92; PMID:23271490; http://dx.doi.org/ 10.1007/s00431-012-1904-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen R, Levy C, Bechet S, Elbez A, Corrard F. What do pediatricians and general practitioners think about the implementation of meningococal B vaccination in France. Arch Pediatr 2012; 19:1379-85; PMID:23159343; http://dx.doi.org/ 10.1016/j.arcped.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 17.Theeten H, Lefevere E, Vandermeulen C, Van Damme P, Hens N. Factors influencing infant and adolescent vaccine uptake in flanders, Belgium. Modeling the Interplay Between Human Behavior and the Spread of Infectious Diseases 2013; 3:43-55. [Google Scholar]
- 18.Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: a cross–sectional study. BMC Public Health 2013; 13:908.PMID:24083352; http://dx.doi.org/ 10.1186/1471-2458-13-908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Cur Med Res Opin 2008; 13:1719-412; PMID:18474148; http://dx.doi.org/ 10.1185/03007990802085692 [DOI] [PubMed] [Google Scholar]
- 20.Muhsen K, Abed El-Haia R, Amit-Aharonb A, Nehamab H, Gondiaa M, Davidovitchc N, Goren S, Cohen D. Risk factors of underutilization of childhood immunizations in ultraorthodox Jewish communities in Israel despite high access to health care services. Vaccine 2012; 13:2109-15; PMID:22285273; http://dx.doi.org/ 10.1016/j.vaccine.2012.01.044 [DOI] [PubMed] [Google Scholar]
- 21.Abbotts B, Osborn LM. Immunization status and reasons for immunization delay among children using public health immunization clinics. Am J Dis Child 1993; 13:965-8; PMID:8362813 [DOI] [PubMed] [Google Scholar]
- 22.Bonanni P, Bergamini M. Factors influencing vaccine uptake in Italy. Vaccine 2001; 20(Suppl 1):S8-12; discussion S1; PMID:11587801 [DOI] [PubMed] [Google Scholar]
- 23.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental Delay or Refusal of Vaccine Doses, Childhood Vaccination Coverage at 24 Months of Age, and the Health Belief Model. Public Health Rep 2011; 126(Suppl 2):135-46; PMID:21812176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics 2004; 114:187-95; PMID:15231927 [DOI] [PubMed] [Google Scholar]
- 25.Hak E, Schonbeck Y, De Melker H, Van Essen GA, Sanders EAM. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine 2005; 13:3103-7; PMID:15837208 [DOI] [PubMed] [Google Scholar]
- 26. http://www.istat.it Accessed on 30th January 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


