Abstract
Plasmocytoid variant urothelial carcinoma (PVUC) of the urinary bladder is a rare histological variant of transitional cell carcinoma. Data regarding PVUC shows that this neoplasia presents a distinctive clinical outcome represented by aggressive behavior and poor survival rate. The authors report a case of a 57-year-old male patient with a 3-month history of hematuria and pelvic pain. Radical cystectomy with lymphadenectomy was performed and pathological examination showed a pT3pN0 PVUC of the bladder. The patient remained free of recurrence for 8 months, but the disease recurred involving the abdominal wall and subcutaneous tissue. Chemotherapy provided a positive clinical response and relief of symptoms. The authors call attention to the aggressiveness of this rare variant of bladder cancer and recommend radical surgery and multidisciplinary management of this neoplasm.
Keywords: Carcinoma, Urothelium, Urinary Bladder Neoplasms, Cystectomy
CASE REPORT
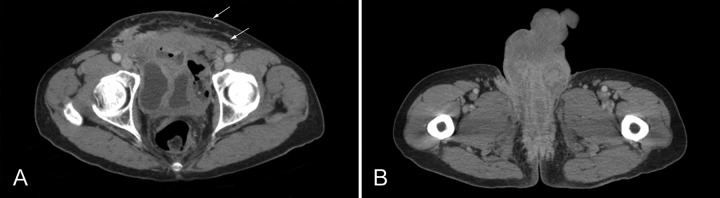
A 57-year-old man sought the Urology Service complaining of pelvic pain and hematuria for three months. His past medical history included heavy smoking. No familial history of cancer was present. The first diagnostic approach involved a cystoscopy, which revealed thickened urinary bladder mucosa. Therefore he was submitted to transurethral resection, which showed a muscle-invasive urothelial carcinoma on histological examination. Initial pelvic, abdominal and thoracic computed tomography (CT) showed bladder wall thickening (Figure 1) without regional or distant lymphadenopathy neither distant metastasis.
Figure 1. Axial pelvic CT showing bladder wall thickening (arrow).

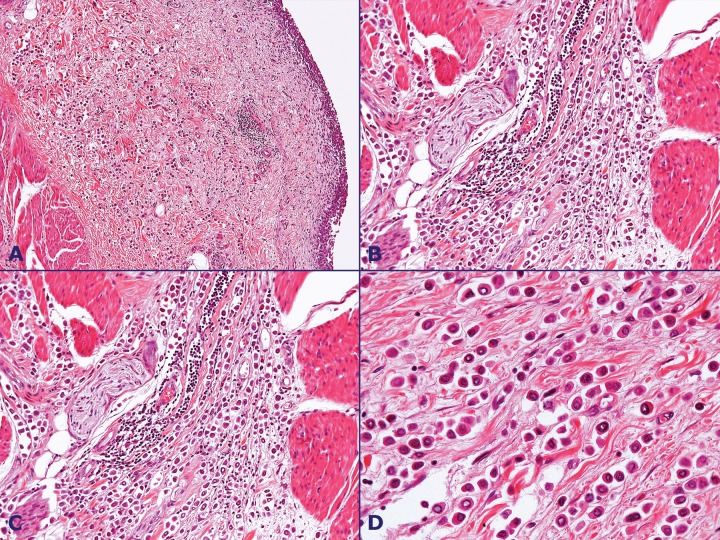
A radical cystectomy with lymphadenectomy was performed. Pathological examination showed plasmocytoid urothelial carcinoma invading perivesical adipose tissue and anterior bladder wall. (Figure 2)
Figure 2. Photomicrography of the bladder tumor - A - Invasive carcinoma with plasmocytoid features (HE, 100X); B - Detail of tumor cells spread in single cell formation (HE, 200X); C and D - Detail of tumor cells spread in “Indian file” (HE, 400X).
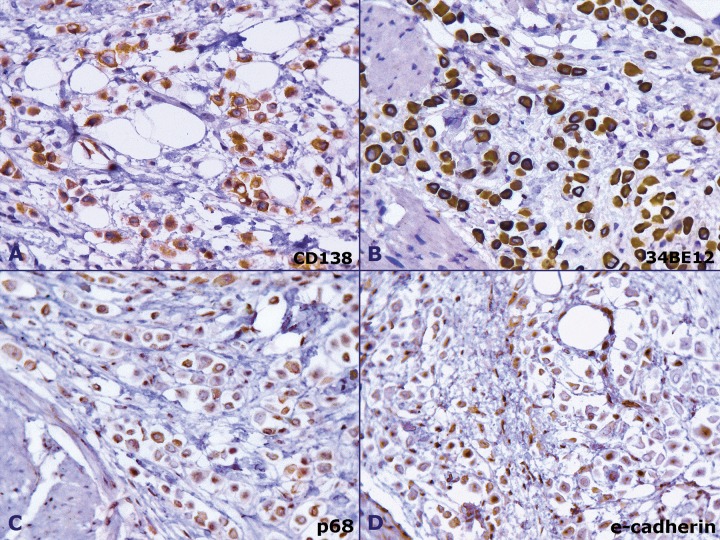
The urethral margins were tumor free but perineural invasion was present. No tumoral involvement was observed in 9 dissected lymph nodes. The immunohistochemistry study revealed positivity to cytokeratin CK7, CK20, 34bE12 and CD138. Napsin A, CDX-2, p63 and E-cadherin were negative. Pathological staging was pT3pN0. (Figure 3)
Figure 3. Photomicrography of the bladder tumor - Immunohistochemistry. A - CD138 positive staining (400x); B - CK34BE12 positive staining (400x); C - E-cadherin negative staining (400x); D - p63 negative staining (400x).
After 8 months, the patient presented progressive swelling and pain in the suprapubic region and scrotum. CT scan showed a densification of adipose and muscle layers of the anterior abdominal wall extending to the scrotum. (Figure 4).
Figure 4. Axial CT of the pelvis. A - showing densification of adipose tissue and muscle layers of the anterior abdominal (arrows); B - extension of the infiltration to the scrotum.
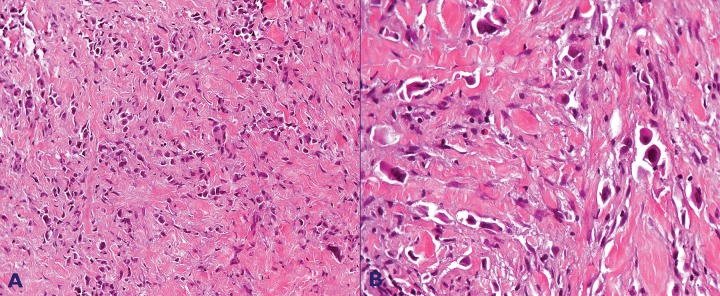
A biopsy of the subcutaneous adipose tissue confirmed poorly cohesive and plasmocytoid features of the carcinoma compatible with high-grade urothelial carcinoma. (Figure 5)
Figure 5. A - Carcinoma infiltration of the subcutaneous adipose tissue (HE x 100); B - poorly cohesive and plasmocytoid features consistent with metastatic plasmacytoid carcinoma (HE x400).
Chemotherapy (MVAC regimen) was prescribed as follow: methotrexate 30 mg/m2 on days 1, 15 and 22; vinblastine 3 mg/m2 on days 2, 15 and 22, doxorubicin 30 mg/m2 on day 2 and cisplatin 70 mg/m2 on day 2, every 28 days each cycle. After 3 cycles, the patients showed marked relief of pain and notably decrease of the suprapubic and scrotal swelling.
DISCUSSION
In 1991, Sahin et al.1 described the first case of plasmocytoid variant urothelial carcinoma (PVUC) of the bladder in a 63-year-old-man presenting a bladder tumor and multiple lytic bone lesions with histologic appearance that mimicked multiple myeloma. This neoplasm is a rare variant of transitional cell carcinoma.
Recently, case series and case reports concerning this carcinoma variant have been published.2,3 Data regarding PVUC show that this neoplasm presents a distinctive clinical outcome represented by high aggressiveness and poor survival rate.2-4 The number of case reports increased during the last decade, what raised the suspicion of an unrecognized ongoing causative factor or a better recognition of this variant could explain this increment.
Histopathological characteristics of PVUC show eccentrically placed nucleus and abundant eosinophilic cytoplasm. Nuclear grade are usually low to intermediate, with occasional pleomorphism. The tumor cells spread in single cell formation, known as “Indian file”, along nerve bundles.2,5,6 Immunohistochemical profile of PVUC is characterized by positivity for CD138, a marker shared with myeloma cells. The cell adhesion marker E-cadherin is down-regulated, suggesting a possible role of epithelial-mesenchymal transition event in PVUC carcinogenesis. Loss of E-cadherin may also allow the discohesive nature of PVUC cells to invade into surrounding tissue, along fascial planes and draining lymph nodes.7 MUM-1 positivity, which occurs in myeloma cells, has not been observed in PVUC.5
Immunohistochemical markers considered specific for urothelial lineage was observed in PVUC in an analysis involving variants of urothelial carcinoma, such as GATA3 (100%), S-100P (100%), Thrombomodulin (45%), CK7 (70%), CK20 (60%), p63(54%), HMCK (90%) and uroplakin (8%).8
Although retrospective cohorts studies of tertiary referral centers have been published, there is still paucity of published data on the clinical behavior and treatment of this malignancy.
In a recent retrospective analysis, Kaimakliotis et al.9 analyzed 624 patients submitted to radical cystectomy from 2008 to 2013. Among them, 25 patients were diagnosed with PVUC. Positive paravesical margins, urethral surgical margins and lymph node involvement were higher in PVUC than in nonvariant subtype. These results indicated more aggressiveness of local spread and called attention for surgeons and pathologists on surgical margins in PVUCs.9
Local treatment for non muscle-invasive bladder urothelial carcinoma is based on transurethral resection with or without intravesical BCG therapy according to high risk factors. Some authors, however, tend to recommend early cystectomy in patients with other urothelial carcinoma variants, such as PVUC, due to the high risk of relapse and aggressive local dissemination.10
Similarly, there is no standard recommendation for initial management of locally-advanced or muscle-invasive PVUC. Dayyani et al.3 reported the MD Anderson Cancer Center experience with 31 patients with PVUC. Sixteen patients had potentially surgically resectable tumor, 5 of them received neoadjuvant chemotherapy, 10 underwent initial surgery and 1 was treated with transurethral resection. Among the patients who received neoadjuvant chemotherapy, pathological down staging was present in 80%. However, there was no difference in the survival rate between patients that received initial surgery or neoadjuvant chemotherapy. The median survival rate of this cohort was 17.7 months; 45.8 months for stages I-III and 13.3 months for stage IV. Patients with metastatic disease at presentation were treated with chemotherapy and showed the median survival rate of 12.6 months. In this cohort the peritoneum was a common site of recurrence (19 of 23 patients).
In other cohort of patients with muscle-invasive bladder tumor after cystectomy, median overall survival rate of patients with PVUC was 22 months, which was significantly lower comparing with patients with non-variant carcinoma. Therefore, among patients selected for cystectomy, those with PVUC had increased risk of mortality at cystectomy.11
Polychemotherapy regimen MVAC has improved survival and overall response rate in comparison with single-agent cisplastin in randomized phase III trial for metastatic or unresectable urothelial bladder carcinoma.12 There is no consensus nor strong evidence regarding the use of specific chemotherapeutic agents in PVUC. However, in the present case, MVAC regimen provided rapid symptoms relief associated with reasonable tolerance.
The aggressive behavior of the present case is in accordance with the literature showing the poor outcome associated with PVUC. Chemotherapy may play a role in disease control and relief of symptoms in unresectable or recurrent disease, as showed in the present case. However, neoadjuvant chemotherapy did not seem to impact in long-term survival in the retrospective cohort aforementioned.11
We believe that early diagnosis and radical surgical approach are pivotal for modifying the clinical course of this subtype of bladder carcinoma. A multidisciplinary team in referral centers is the ideal scenario for managing PVUC treatment.
CONCLUSION
We presented a case of PVUC, a rare histological variant of urothelial bladder carcinoma. The patient’s clinical course is in accordance with the literature data in terms of locally aggressiveness of this tumor. Morphologic distinction of the plasmocytoid phenotype is critical for clinician awareness with regard to the risk for early regional and metastatic progression of the disease.
REFERENCES
Footnotes
Fonseca LG, Souza CE, Mattedi RL, Girardi DM, Sarkis AS, Hoff PMG. Plasmacytoid urothelial carcinoma: a case of histological variant of urinary bladder cancer with aggressive behavior. Autopsy Case Rep [Internet]. 2014;4(4):57-61. http://dx.doi.org/10.4322/acr.2014.040
References
- 1.Sahin AA, Myhre M, Ro JY, Sneige N, Dekmezian RH, Ayala AG. Plasmacytoid transitional cell carcinoma. Report of a case with initial presentation mimicking multiple myeloma. Acta Cytol. 1991;35(3):277-80. PMid:. [PubMed] [Google Scholar]
- 2.Keck B, Stoehr R, Wach S, et al. The plasmacytoid carcinoma of the bladder—rare variant of aggressive urothelial carcinoma. Int J Cancer. 2011;129(2):346-54. http://dx.doi.org/10.1002/ijc.25700. PMid: [DOI] [PubMed] [Google Scholar]
- 3.Dayyani F, Czerniak BA, Sircar K, et al. Plasmacytoid urothelial carcinoma, a chemosensitive cancer with poor prognosis, and peritoneal carcinomatosis. J Urol. 2013;189(5):1656-61. http://dx.doi.org/10.1016/j.juro.2012.11.084. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mai KT, Park PC, Yazdi HM, et al. Plasmacytoid urothelial carcinoma of the urinary bladder report of seven new cases. Eur Urol. 2006;50(5):1111-4. http://dx.doi.org/10.1016/j.eururo.2005.12.047. PMid: [DOI] [PubMed] [Google Scholar]
- 5.Lopez-Beltran A, Requena MJ, Montironi R, Blanca A, Cheng L. Plasmacytoid urothelial carcinoma of the bladder. Hum Pathol. 2009;40(7):1023-8. http://dx.doi.org/10.1016/j.humpath.2009.01.001. PMid: [DOI] [PubMed] [Google Scholar]
- 6.Raspollini MR, Sardi I, Giunti L, et al. Plasmacytoid urothelial carcinoma of the urinary bladder: clinicopathologic, immunohistochemical, ultrastructural, and molecular analysis of a case series. Hum Pathol. 2011;42(8):1149-58. http://dx.doi.org/10.1016/j.humpath.2010.11.011. PMid: [DOI] [PubMed] [Google Scholar]
- 7.Erdemir F, Ozcan F, Kilicaslan I, Parlaktas BS, Uluocak N, Gokce O. The relationship between the expression of E-cadherin and tumor recurrence and progression in high-grade stage T1 bladder urothelial carcinoma. Int Urol Nephrol. 2007;39(4):1031-7. http://dx.doi.org/10.1007/s11255-006-9159-5. PMid: [DOI] [PubMed] [Google Scholar]
- 8.Paner GP, Annaiah C, Gulmann C, et al. Immunohistochemical evaluation of novel and traditional markers associated with urothelial differentiation in a spectrum of variants of urothelial carcinoma of the urinary bladder. Hum Pathol. 2014;45(7):1473-82. http://dx.doi.org/10.1016/j.humpath.2014.02.024. PMid: [DOI] [PubMed] [Google Scholar]
- 9.Kaimakliotis HZ, Monn MF, Cheng L, et al. Plasmacytoid bladder cancer: variant histology with aggressive behavior and a new mode of invasion along fascial planes. Urology. 2014;83(5):1112-6. http://dx.doi.org/10.1016/j.urology.2013.12.035. PMid: [DOI] [PubMed] [Google Scholar]
- 10.Porten SP, Willis D, Kamat AM. Variant histology: role in management and prognosis of nonmuscle invasive bladder cancer. Curr Opin Urol. 2014;24(5):517-23. http://dx.doi.org/10.1097/MOU.0000000000000089. PMid: [DOI] [PubMed] [Google Scholar]
- 11.Kaimakliotis HZ, Monn MF, Cary KC, et al. Plasmacytoid variant urothelial bladder cancer: is it time to update the treatment paradigm? Urol Oncol. 2014;32(6):833-8. http://dx.doi.org/10.1016/j.urolonc.2014.03.008. PMid: [DOI] [PubMed] [Google Scholar]
- 12.Loehrer PJ Sr, Einhorn LH, Elson PJ, et al. A randomized comparison of cisplatin alone or in combination with methotrexate, vinblastine, and doxorubicin in patients with metastatic urothelial carcinoma: a cooperative group study. J Clin Oncol. 1992;10(7):1066-73. PMid:. [DOI] [PubMed] [Google Scholar]