Abstract
Most surgeons create a T-shaped or interportal capsulotomy to ensure good visibility when performing hip arthroscopy. This entails transecting the iliofemoral ligament, which may or may not be repaired at the end of the procedure. Cases of iatrogenic hip instability and pain after hip arthroscopy suggest that the iliofemoral ligament plays a crucial role in the stability of the hip joint, and thus preservation should be a goal in hip arthroscopy. We describe a minimally invasive iliofemoral ligament–sparing capsulotomy, guided by the reflected head of the rectus tendon, that can be easily repaired after arthroscopic rim trimming, labral refixation, and offset correction.
A number of hip arthroscopists perform a T-shaped capsulotomy to ensure good visibility during hip arthroscopy and may not close this at the end of the procedure. Others perform a so-called interportal capsulotomy that results in transection of the iliofemoral ligament (IFL), again with or without repair at the end of the procedure.1
Reports of iatrogenic hip instability have shed light on the importance of the soft-tissue structures around the hip. Most patients in these studies had anterior dislocations.2 The major anatomic structure limiting extension and external rotation and thus anterior translation and subluxation of the femoral head is the IFL.2, 3
In a series of revision cases excluding those with residual femoroacetabular impingement, 7 of 9 cases were found to have capsular defects on magnetic resonance imaging and 2 had gross deficiency of the capsule intraoperatively.4 A likely explanation for symptoms is the resulting microinstability, consistent with cadaveric studies.5 Recent studies have suggested that capsular repair improves patient outcomes.6, 7 We propose a capsulotomy technique that protects the continuity of the IFL.
Surgical Technique
Our Preferred Method
The presented technique is a modification of a previously described extra-articular approach described by the senior author (R.F.H.).8
Positioning
The patient is placed in the supine position on a trauma table with leg extensions and a perineal post. Traction is applied to the operative leg only, whereas the contralateral leg is secured to a mobile leg holder as might be done for intramedullary nailing.
Extracapsular Approach
Anterior pericapsular infiltration is performed under an image intensifier with 20 mL of saline solution with epinephrine diluted to 1:100. The distal anterolateral (DALA) portal and anterior portal are established as previously described8 (Fig 1). The first portal is the DALA portal. Blunt dissection of the ventral capsule is carried out with a sweeping motion with the trocar before insertion of the arthroscope (70° HD arthroscope; Arthrex, Naples, FL). By use of the anterior portal, the capsular surface is then exposed (Dissector [Arthrex] and Super Multivac 50 ICW with 8.0-mm × 72-mm threaded cannula [Smith & Nephew, London, England]). We clear the fatty tissue between the gluteus minimus, iliocapsularis, and vastus lateralis muscles.
Fig 1.
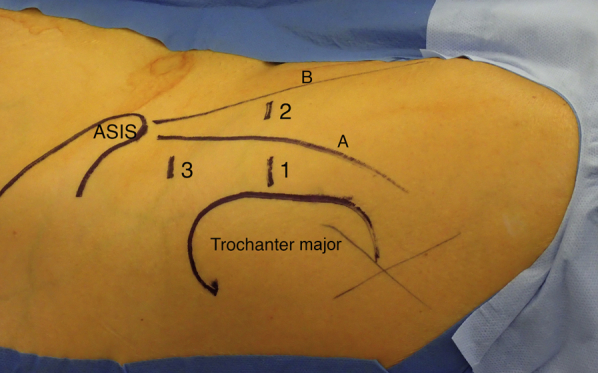
The arthroscopic portals used are shown in a right hip, with the patient in the supine position: 1, distal anterolateral portal; 2, anterior portal; and 3, proximal anterolateral portal. (A, medial border of musculus tensor fasciae latae; ASIS, anterior superior iliac spine; B, lateral border of musculus sartorius.)
Capsulotomy
We identify the tendinous portion of the reflected head of the rectus muscle; this serves as an internal reference for the capsulotomy, which is performed parallel to the fibers of the IFL at its lateral border (Fig 2, Fig 3, Fig 4). This blends with the capsule at the 12-o'clock position. Aiming just anterior to this area corresponds to the superior margin of the IFL (Fig 4).
Fig 2.
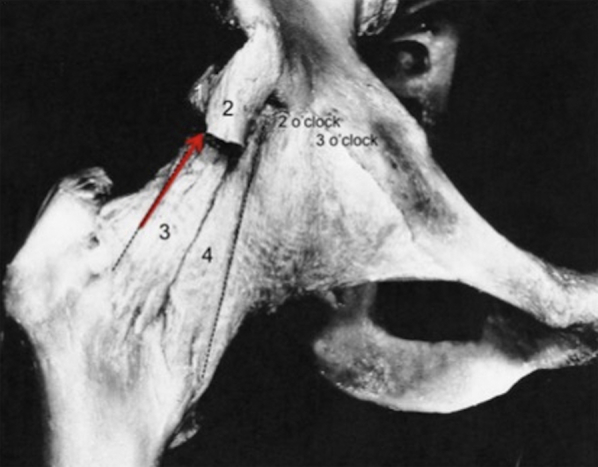
Cadaveric specimen of a right hip, anterior view. The arrow indicates the longitudinal capsulotomy parallel to the fibers along the lateral border of the lateral bundle of the iliofemoral ligament. (1, reflected head of rectus tendon [landmark]; 2, direct head of rectus tendon; 3, lateral bundle of iliofemoral ligament; 4, medial bundle of iliofemoral ligament.)
(Reproduced with permission from Springer Science+Business Media from Guyot J. Atlas of human limb joints. Berlin: Springer-Verlag, 1990.)
Fig 3.
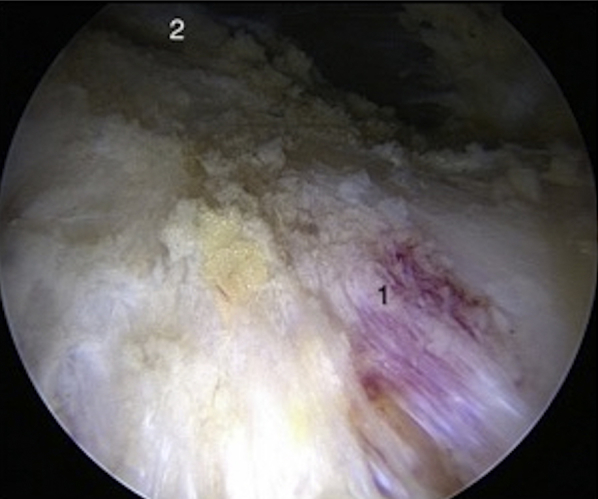
Left hip after resection of pericapsular fat tissue (camera in distal anterolateral portal, with 12-o'clock position at top of image). (1, capsulotomy along longitudinal fibers indicating direction of iliofemoral ligament; 2, reflected head of rectus femoris muscle.)
Fig 4.
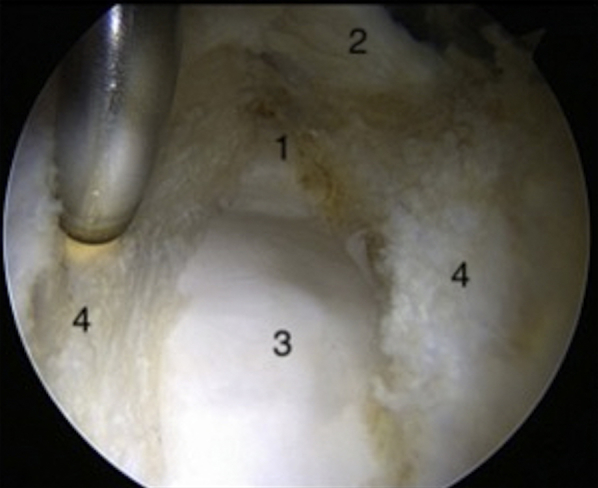
Longitudinal capsulotomy in a left hip guided by the reflected head of the rectus muscle (camera in distal anterolateral portal, instrument in anterior portal, with 12-o'clock position at top of image). (1, acetabular labrum; 2, reflected head of tendon of rectus muscle; 3, cam deformity and femoral head; 4, divided joint capsule.)
The reflected head of the rectus tendon can be found behind the caput recurvatum of the rectus tendon, a thin, white fibrous structure just covering the reflected head while moving superomedially on the surface of the anterosuperior aspect of the capsule.9 Once the labrum is visible, traction is applied and intra-articular inspection can proceed.
Central Compartment
Thorough intra-articular inspection and probing of the acetabular labrum are performed including the anterior and posterior horn, ligamentum teres, and cartilage surfaces of the acetabulum and femoral head. The proximal anterolateral (PALA) portal is made, and labral treatment is performed as necessary (Video 1).
The arthroscope is switched into the PALA portal, and drill holes are made through the DALA portal or an additional portal with a cannula. Sutures (No. 2 FiberWire; Arthrex) are passed through the chondrolabral junction (SpeedStitch suturing device; Smith & Nephew) or through both the chondrolabral junction and the base of the labrum, and these are then fixed in the acetabular rim by knotless anchors (2.9-mm BioComposite PushLock; Arthrex) as shown in Video 1.
Peripheral Compartment
The cam deformity is addressed by beginning the osteoplasty adjacent to the retinacular vessels proceeding to a point at which further exposure would be required (ClearCut Burr; Arthrex) (Fig 5). The hip is then flexed up to 50° with slight external rotation to reach the medial synovial fold. Finally, the capsule is repaired in a side-to-side fashion (SpeedStitch suturing device and No. 2 FiberWire) (Fig 6). Table 1 lists pearls and pitfalls of the described technique, and Table 2 lists advantages and disadvantages.
Fig 5.
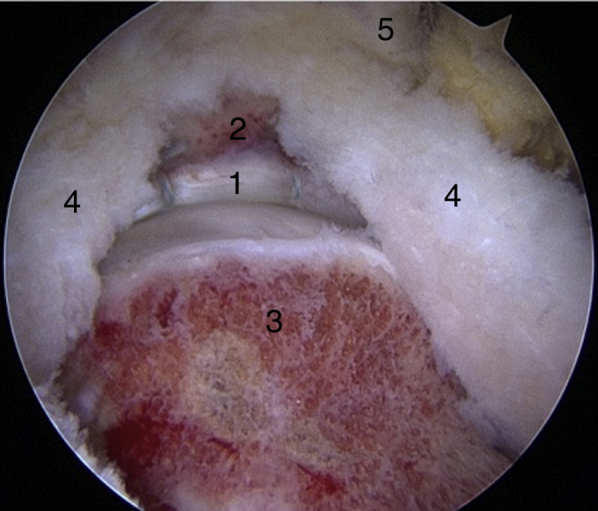
Left hip after correction of the head-neck offset showing the substance of the iliofemoral ligament and the position of the reflected head of the rectus muscle (camera in distal anterolateral portal, with 12-o'clock position at top of image). (1, acetabular labrum; 2, acetabular rim; 3, restored offset at head-neck junction; 4, joint capsule; 5, reflected head of rectus tendon.)
Fig 6.
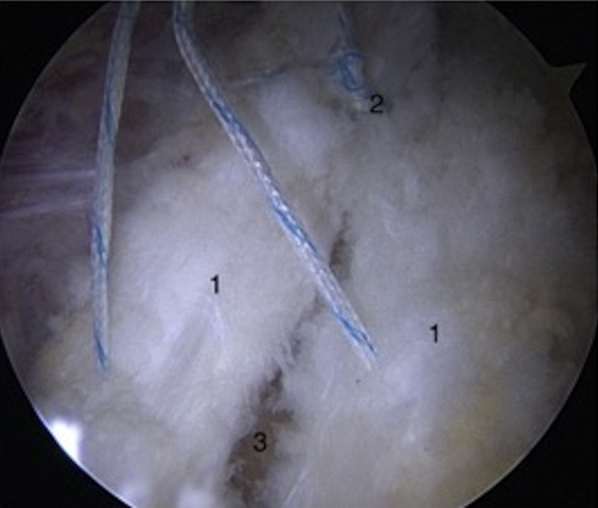
Closure by passing sutures through both lips of the capsule in a left hip (camera in distal anterolateral portal, instrument in anterior or proximal anterolateral portal, with 12-o'clock position at top of image). (1 and 2, tying of knots; 3, resected surface of femoral neck.)
Table 1.
Pearls and Pitfalls
| Pearls |
| In obese or muscular patients or patients with coxa antetorta, slightly more anterior placement of the DALA portal will facilitate maneuvering the camera. |
| When the deep layer of the capsule is being approached, the labrum will be in proximity and the synovial tissue will be visible next to the cartilage layer. |
| Rim trimming distal to the capsulotomy (2- to 3-o'clock position) is performed with the burr in the PALA portal. Rim trimming proximal to the capsulotomy (12- to 1-o'clock position and beyond) is performed with the burr in the anterior portal. |
| In the case of pincer impingement, a more extensive perilabral release of the deep portion of the IFL may be helpful. |
| In the case of coxa profunda, an L-shaped release of the capsular flaps can be performed. In this instance, refixation with separate anchors is recommended. |
| A pistol-grip deformity may require slight extension and internal rotation of the hip. Care must be taken to spare the retinacular vessels. |
| Pitfalls |
| The surgeon should check the trajectory of the drill before drilling and, if necessary, prepare an additional portal more lateral than the DALA portal to avoid penetration of the acetabulum. |
DALA, distal anterolateral; IFL, iliofemoral ligament; PALA, proximal anterolateral.
Table 2.
Advantages and Disadvantages
| Advantages |
| Iliofemoral ligament is left nearly intact (except for release of deep fibers at acetabular rim if needed) |
| Low traction force |
| Low traction times (approximately 35-40 min in case of rim trimming and labral repair) |
| Easy to obtain full closure |
| No risk of over-tightening capsule |
| Short duration of image intensifier use |
| Disadvantages |
| Challenging technique |
Discussion
Several biomechanical studies underline the importance of the IFL for hip stability including distraction, extension combined with external rotation, and restraint against anterior translation.3, 5, 10 In case reports the mechanism of dislocation involved extension and external rotation and the direction of dislocation was anterior. This corresponds to typical arthroscopic interportal capsulotomy techniques, transecting the IFL.
Cadaveric studies have also described restoration of the stability of the hip joint after closure of either interportal or T-capsulotomies. The cadaveric setting does not necessarily account for secondary attenuation and distraction of the healing IFL, which may result in potential recurrent instability.
A capsulotomy that spares the longitudinal integrity of the IFL is less likely to lead to iatrogenic instability compared with an unrepaired capsulotomy that involves transection of the IFL. Indeed, it is possible that it may have advantages compared with a repaired interportal capsulotomy. However, this has yet to be confirmed.
A crucial step in our technique is the definition of the reflected head of the rectus muscle, which consistently guides the capsulotomy. The IFL is thickest between the 1- and 2-o'clock positions measuring approximately 7.2 to 8.3 mm.11 The reflected head of the rectus tendon blends with the capsule at the 12-o'clock position. Aiming just anterior to this area corresponds to the superior margin of the IFL. Therefore, most of the IFL can be spared because its superior margin corresponds to the 12:45 clock-face to 1-o'clock position.11
In rare instances, extension of the exposure may be necessary. An extensive capsulotomy was required in 17 of the first 100 cases. In 10 cases the medial bundle of the IFL was released at the acetabular origin in an L shape; in another case a T-capsulotomy was made. In 4 cases a parallel incision (not applied beyond the first 100 cases) was used, and in 2 other cases a conventional approach8 was performed. The mean age and body mass index of these patients was 30.5 years (standard deviation, 12.7 years) and 23.8 (standard deviation, 3.5), respectively.
To minimize the risk of iatrogenic instability, we developed an IFL-sparing capsulotomy, parallel and lateral to the longitudinal fibers of the ligament. The key to this approach is the definition of the reflected head of the rectus muscle, which serves as a consistent guiding landmark and enables surgery without the need for an image intensifier. We emphasize that a complete anatomic closure is possible in most cases. We speculate that this technique may result in a shorter rehabilitation period especially in case of athletes by improving proprioception. Further studies are needed to evaluate the objective benefits.
Footnotes
The authors report the following potential conflict of interest or source of funding: C.F-H. is employed by the Lucerne County Hospital Wolhusen as current and sole employer. B.G.D. receives support from American Hip Institute, AANA Learning Center Committee, Arthrex, Pacira, Stryker MAKO Surgical, Amplitude, Orthomerica, DJO Global, Breg, and ATI. R.F.H. receives support from Orthopaedic Department, Lucerne County Hospital Wolhusen.
Supplementary Data
The patient is positioned on a conventional extension table as for the treatment of proximal femoral fractures that is well padded at the perineum. The right hip is operated on in this case. Pericapsular tissue is infiltrated with diluted epinephrine. Resection of the pericapsular fat is performed between the iliocapsularis and gluteus medius muscle toward the acetabular rim with a shaver and Hip Vac 50 (ArthroCare) (70° camera [Arthrex] in distal anterolateral [DALA] portal, instrument in anterior portal). The reflected head of the rectus tendon is identified. The tendon blends with the capsule at the 12-o'clock position. Capsulotomy is performed aiming just anterior to the aforementioned position. The cranial margin of the femoral neck can be seen in the case of correct placement of the capsulotomy. The synovial tissue appears just lateral to the labrum; the labrum is then carefully exposed. Traction is applied and intra-articular assessment performed. We decided to repair the labrum in this case. The proximal anterolateral (PALA) portal is made for instrumentation of the perilabral sulcus at the 1- to 3-o'clock position (camera in DALA portal, instrument in PALA or anterior portal). Perilabral preparation follows, and subsequently, rim trimming is performed (camera in DALA portal, instrument in PALA or anterior portal). Drill holes are made for anchors (camera in PALA portal, drill in DALA portal). Sutures are passed through the chondrolabral junction. Knotless anchors (2.9 mm) are used, and debris is removed from the central compartment. Traction is released. The retinacular vessels are identified: One should note the pulsating artery (camera in DALA portal, instrument in PALA portal) enabling a safe femoral preparation (camera in DALA portal, instrument in PALA or anterior portal). The medial synovial fold is identified marking the 6-o'clock position; the hip may be flexed to 50° (camera in DALA portal, instrument in anterior portal). After correction of the offset, the impingement test is performed in 90° of flexion to maximal internal rotation. The capsule is closed by passing 2 sutures (FiberWire) through both sides of the split capsule, one medially and one at the zona orbicularis. A sliding knot is used (camera in DALA portal, instrument in PALA or anterior portal). The capsule is anatomically closed.
References
- 1.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 2.Duplantier N.L., McCulloch P.C., Nho S.J., Mather R.C., III, Lewis B.D., Harris J.D. Hip dislocation or subluxation after hip arthroscopy: A systematic review. Arthroscopy. 2016;32:1428–1434. doi: 10.1016/j.arthro.2016.01.056. [DOI] [PubMed] [Google Scholar]
- 3.Abrams G.D., Hart M.A., Takami K. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 4.McCormick F., Slikker W., III, Harris J.D. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
- 5.Myers C.A., Register B.C., Lertwanich P. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S–91S. doi: 10.1177/0363546511412161. [DOI] [PubMed] [Google Scholar]
- 6.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 7.Domb B.G., Stake C.E., Finley Z.J., Chen T., Giordano B.D. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31:643–650. doi: 10.1016/j.arthro.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Horisberger M., Brunner A., Herzog R.F. Arthroscopic treatment of femoroacetabular impingement of the hip: A new technique to access the joint. Clin Orthop Relat Res. 2010;468:182–190. doi: 10.1007/s11999-009-1005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tubbs R.S., Stetler W., Jr., Savage A.J. Does a third head of the rectus femoris muscle exist? Folia Morphol (Warsz) 2006;65:377–380. [PubMed] [Google Scholar]
- 10.Nepple J.J., Philippon M.J., Campbell K.J. The hip fluid seal—Part II: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22:730–736. doi: 10.1007/s00167-014-2875-y. [DOI] [PubMed] [Google Scholar]
- 11.Philippon M.J., Michalski M.P., Campbell K.J. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc. 2015;23:2548–2553. doi: 10.1007/s00167-014-3030-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned on a conventional extension table as for the treatment of proximal femoral fractures that is well padded at the perineum. The right hip is operated on in this case. Pericapsular tissue is infiltrated with diluted epinephrine. Resection of the pericapsular fat is performed between the iliocapsularis and gluteus medius muscle toward the acetabular rim with a shaver and Hip Vac 50 (ArthroCare) (70° camera [Arthrex] in distal anterolateral [DALA] portal, instrument in anterior portal). The reflected head of the rectus tendon is identified. The tendon blends with the capsule at the 12-o'clock position. Capsulotomy is performed aiming just anterior to the aforementioned position. The cranial margin of the femoral neck can be seen in the case of correct placement of the capsulotomy. The synovial tissue appears just lateral to the labrum; the labrum is then carefully exposed. Traction is applied and intra-articular assessment performed. We decided to repair the labrum in this case. The proximal anterolateral (PALA) portal is made for instrumentation of the perilabral sulcus at the 1- to 3-o'clock position (camera in DALA portal, instrument in PALA or anterior portal). Perilabral preparation follows, and subsequently, rim trimming is performed (camera in DALA portal, instrument in PALA or anterior portal). Drill holes are made for anchors (camera in PALA portal, drill in DALA portal). Sutures are passed through the chondrolabral junction. Knotless anchors (2.9 mm) are used, and debris is removed from the central compartment. Traction is released. The retinacular vessels are identified: One should note the pulsating artery (camera in DALA portal, instrument in PALA portal) enabling a safe femoral preparation (camera in DALA portal, instrument in PALA or anterior portal). The medial synovial fold is identified marking the 6-o'clock position; the hip may be flexed to 50° (camera in DALA portal, instrument in anterior portal). After correction of the offset, the impingement test is performed in 90° of flexion to maximal internal rotation. The capsule is closed by passing 2 sutures (FiberWire) through both sides of the split capsule, one medially and one at the zona orbicularis. A sliding knot is used (camera in DALA portal, instrument in PALA or anterior portal). The capsule is anatomically closed.


