Abstract
Expectations about future health and longevity are important determinants of individuals’ decisions to invest in physical and human capital. Few population-level studies have measured subjective expectations and examined how they are affected by scale-up of antiretroviral therapy (ART). We assessed these expectations in communities receiving annual HIV testing and universal ART. Longitudinal data on expectations were collected at baseline and one year later in 16 intervention communities participating in the Sustainable East Africa Research in Community Health (SEARCH) trial of the test and treat strategy in Kenya and Uganda (NCT01864603). A random sample of households with and without an HIV-positive adult was selected after baseline HIV testing. Individuals’ expectations about survival to 50, 60, 70, and 80 years of age, as well as future health status and economic well-being, were measured using a Likert scale. Primary outcomes were binary variables indicating participants who reported being very likely or almost certain to survive to advanced ages. Logistic regression analyses were used to examine trends in expectations as well as associations with HIV status and viral load for HIV-positive individuals. Data were obtained from 3126 adults at baseline and 3977 adults in year 1, with 2926 adults participating in both waves. HIV-negative adults were more likely to have favorable expectations about survival to 60 years than HIV-positive adults with detectable viral load (adjusted odds ratio [AOR] 1.87, 95% CI 1.53–2.30), as were HIV-positive adults with undetectable viral load (AOR 1.41, 95% CI 1.13–1.77). Favorable expectations about survival to 60 years were more likely for all groups in year 1 compared to baseline (AOR 1.53, 95% CI 1.31–1.77). These findings are consistent with the hypothesis that universal ART leads to improved population-level expectations about future health and well-being. Future research from the SEARCH trial will help determine whether these changes are causally driven by the provision of universal ART.
Keywords: Antiretroviral therapy, test and treat, health expectations, subjective life expectancy
Background
Life expectancy has long been hypothesized as an important determinant of individuals’ decisions to invest in physical and human capital (Becker, 1964; Ben-Porath, 1967) and this premise of economic theory has played a central role in the study of economic development. Several recent studies have empirically documented a link between changes in life expectancy and human capital investment, with one study showing that during the early years of the HIV/AIDS epidemic when life expectancy declined considerably, households reduced their investments in schooling (Fortson, 2011; Jayachandran & Lleras-Muney, 2009; Oster, Shoulson, & Dorsey, 2013). Moreover, because it strengthens the incentives to invest in human capital, life expectancy has also been recognized as having a causal effect on economic growth at the macroeconomic level (Kalemli-Ozcan, 2002; Soares, 2005).
Given the potential importance of life expectancy in decision-making, there is growing recognition of the value of measuring individuals’ subjective expectations about future health and studying factors that influence these expectations. In the US and other developed countries, elicitation of individuals’ expectations about survival to advanced ages and about major life events has become fairly common. For example, the Health and Retirement Survey has included such measures (Hurd & McGarry, 1995, 2002) and several studies have shown that eliciting individuals’ expectations is not only feasible but also useful for understanding important aspects of individuals’ decisions (Delavande & Rohwedder, 2011). In developing countries, however, very few population-level studies have elicited individuals’ expectations about longevity (Delavande, Gine, & McKenzie, 2011).
Particularly in sub-Saharan Africa (SSA), which saw dramatic declines in life expectancy after the onset of HIV/AIDS epidemic followed by large reductions in adult mortality as HIV treatment with antiretroviral therapy (ART) was scaled-up in the past decade (UNAIDS, 2015), there have been strikingly few studies examining associations between HIV/AIDS and individuals’ subjective expectations about life expectancy. One study in Malawi has measured individuals’ survival expectations and examined its association with key socio-economic characteristics as well HIV-related risk behaviors (Delavande & Kohler, 2009), but no studies have examined how individuals may be updating their expectations as ART scale-up occurs and bolder “treatment as prevention” strategies are implemented.
We assessed cross-sectional patterns and trends in individuals’ subjective expectations about survival, health, and economic conditions in rural Kenyan and Ugandan communities that began receiving annual HIV testing and universal ART.
Methods
Data were collected in two waves, at baseline and year 1, in 16 intervention communities participating in the ongoing Sustainable East Africa Research in Community Health (SEARCH) HIV test and treat cluster randomized controlled trial (NCT01864603). The SEARCH trial consists of 32 communities (20 in eastern and southwestern Uganda and 12 in western Kenya), which were selected from 54 candidate communities that met initial eligibility criteria of a rural community, had a population of about 10,000 individuals, and contained an HIV clinic. Sixteen matched pairs of communities were selected on the basis of region, population density, occupational mix, access to transport routes, and number of trading centers (Balzer, Petersen, van der Laan, & SEARCH Consortium, 2015).
Procedures used to enumerate study communities and implement a hybrid mobile HIV testing approach in each community at baseline have recently been described elsewhere (Chamie et al., 2016). In brief, at baseline a door-to-door census was first conducted in each community. This was followed by 2 week multiple-disease community health campaigns (CHCs) that included HIV testing, counseling, and referral to care if HIV infected. Non-HIV services designed to improve community health were also provided, and these included hypertension and diabetes screening, malaria rapid diagnostic testing for participants with fever, male condom distribution, referral for medical male circumcision, family planning and cervical cancer screening, and vitamin A and albendazole treatment for young children. The CHCs were held at central locations in communities. Individuals aged ≥15 years who did not participate in the CHCs were approached for home-based testing (HBT) within 1–6 months after the CHC. For HIV-positive individuals, HIV-1 viral load measurements were performed by reference testing laboratories in Uganda, Kenya and the United States using commercial real-time PCR assays following the manufacturer’s instructions. This hybrid testing approach achieved a high level of HIV testing coverage in the population at baseline (Chamie et al., 2016) and was repeated one year later in the sixteen SEARCH intervention communities.
In SEARCH intervention communities, HIV-positive individuals are rapidly initiated on ART independent of CD4 cell count. ART is delivered in a streamlined, patient-centered, approach that includes appointment reminders, quarterly visits, reduced waiting times at clinics, and viral load results counseling wherein patients receive their viral load results and counseling to understand the anticipated benefits of viral suppression and consequences of detectable viral loads. The control communities follow country guidelines for ART initiation and delivery.
Immediately following the CHCs and in parallel with HBT, a random sample of households with and without an HIV-positive adult were selected for structured household surveys. One HIV-positive adult (i.e. index person) was selected in the households that contained one or more HIV-positive adults, and one HIV-negative adult (i.e. index person) was selected randomly in the households with no HIV-positive adults. In each community, we aimed to conduct surveys with 100 households that included an HIV-positive adult and 100 households that did not include an HIV-positive adult. The surveys assessed socio-economic conditions of households and consisted of several modules that obtained information on demographic characteristics, employment and income of household members aged ≥12 years, ownership of assets, health care utilization, and education of household members aged 6–25 years. These surveys were adapted from Living Standards Measurement Surveys (Grosh & Glewwe, 2000) administered in numerous developing countries. Surveys were administered by trained interviewers who visited the randomly sampled households. Information collected in the surveys was linked at the individual level to information on HIV status (and for HIV-positive adults, to HIV-1 viral load) that was obtained during CHCs and HBT. Household surveys were repeated one year later with the same households that participated in the baseline surveys.
Expectations measures
In the household surveys, individuals’ expectations about their likelihood of survival to 50, 60, 70, and 80 years of age were measured using a 5-point Likert scale. Expectations about survival to each of the four ages were only elicited if the individual was younger than the corresponding target age. Individuals’ expectations about their own health in 1 year and 3 years were also elicited using a 5-point Likert scale, as were their expectations about the standard of living of their community in 1 year and the financial well-being of their own household in 3 years. At baseline, questions about expectations were administered to only one randomly-selected adult in each household whereas at follow-up year 1, these questions were administered to all adult household members who were present at the time of the survey.
Statistical analyses
Analyses of baseline and follow-up data were limited to SEARCH intervention communities and did not include comparisons to control communities because the SEARCH trial is ongoing. For each of the advanced ages for which we elicited expectations, participants’ responses were classified as binary variables that indicated whether they felt it was “very likely” or “almost certain” they would survive the corresponding age, or if instead they responded with “almost impossible”, “not very likely”, or “maybe”. Similarly, for expectations about future health status and economic well-being, participants’ responses were classified as binary variables that indicated whether they felt it was “very likely” or “almost certain”. Logistic regression models were used to examine the association between each of the binary expectation measures and key exposure variables and to estimate time trends. The main exposure variable of interest was a categorical variable indicating whether an individual was HIV-negative, HIV-positive with HIV-1 viral load <500 copies/μL (undetectable viral load), or HIV-positive with HIV-1 viral load ≥500 copies/μL (detectable viral load). Viral load was included in the exposure measure to reflect successful ART use. HIV-positive individuals with detectable viral load served as the reference group.
In analyses that pooled the baseline and follow-up year 1 data, time trends were estimated using a binary variable that indicated whether the outcome was being measured in follow-up year 1. The analyses also controlled for several individual characteristics including gender, age (defined in four categories), highest level of education completed (defined in three categories: no education, primary level, secondary level, or greater), marital status, and included community and interviewer fixed effects. Models with individual fixed effects were also estimated to examine the association between the main outcomes and viral load using variation over time in HIV-positive individuals’ viral load.
The Makerere University School of Medicine Research and Ethics Committee, the Ugandan National Council for Science and Technology, the Kenya Medical Research Institute Ethical Review Committee, and the University of California San Francisco Committee on Human Research approved the study. All participants provided verbal informed consent in their preferred language with fingerprint confirmation of consent.
Results
Household surveys that obtained information on individuals’ subjective expectations were conducted at study baseline, between July 2013 and August 2014, with 3118 households in the 16 intervention communities. A total of 3126 adults responded to questions on subjective expectations at baseline. In follow-up year 1, 2973 households were revisited between October 2014 and September 2015 and information on subjective expectations was obtained from 3977 adults. Our analytic sample was restricted to subjects whose HIV status and HIV-1 viral load were known and who were between the ages of 18–80 years at time of survey (2676 individuals in 2670 households at baseline and 3410 individuals in 2695 households at follow-up year 1). For analyses of expectations to survive to 50, 60, 70, and 80 years, respectively, individuals who were younger than the corresponding target age were excluded.
Table 1 summarizes key demographic and socioeconomic characteristics of study participants in the analytic sample. Approximately 64% of all respondents were female. Approximately 70% of respondents were married, and at baseline, about 20% of respondents were between 18 and 25 years of age and about 70% were ≤45 years of age. At baseline and follow-up year 1, 63.8% and 64.8% of respondents were HIV-negative, respectively.
Table 1.
Descriptive characteristics of study participants in SEARCH intervention communities.
| Baseline No. (%) | Follow-up year 1 No. (%) | p-Value | |
|---|---|---|---|
| No. individuals | 2676 | 3410 | |
| No. households | 2670 | 2695 | |
| HIV status | |||
| HIV+, detectable viral load | 526 (19.7) | 164 (4.8) | <0.001 |
| HIV+, undetectable viral load | 535 (20.0) | 1,084 (31.8) | <0.001 |
| HIV-status | 1615 (60.4) | 2162 (63.4) | 0.009 |
| Female | 1706 (63.8) | 2209 (64.8) | 0.723 |
| Age categories | |||
| 18–25 years old | 530 (19.8) | 561 (16.5) | 0.151 |
| 26–35 years old | 730 (27.3) | 859 (25.2) | 0.043 |
| 36–45 years old | 602 (22.5) | 808 (23.7) | 0.765 |
| 46–80 years old | 814 (30.4) | 1182 (34.7) | 0.004 |
| Education level | |||
| No education | 439 (16.4) | 503 (14.8) | 0.068 |
| Primary education | 1669 (62.4) | 2201 (64.6) | 0.121 |
| Secondary or more education | 567 (21.2) | 703 (20.6) | 0.839 |
| Married/cohabiting | 1828 (68.3) | 2430 (71.3) | 0.117 |
| Wealth index | |||
| Least wealth | 576 (21.6) | 655 (19.2) | 0.012 |
| Less wealth | 549 (20.6) | 667 (19.6) | 0.260 |
| Middle wealth | 512 (19.2) | 658 (19.3) | 0.876 |
| More wealth | 520 (19.5) | 693 (20.3) | 0.317 |
| Most wealth | 512 (19.2) | 737 (21.6) | 0.006 |
| Region | |||
| Southwest Uganda | 837 (31.3) | 1064 (31.2) | 0.744 |
| Eastern Uganda | 818 (30.6) | 1100 (32.3) | 0.744 |
| Kenya | 1021 (38.2) | 1246 (36.5) | 0.532 |
Notes: p-Values based on chi-squared tests comparing characteristics of participants at baseline and follow-up. Wealth quintiles are based on a wealth index created using principal components analysis of ownership of 47 items. Characteristics reported are for participants aged 18–80 years, with HIV status and HIV-1 viral load information.
Participants’ expectations at baseline and follow-up year 1 about survival to advanced ages, as well as future health and financial well-being, are summarized in Table 2 and Figure 1. As the target age increased, the proportion of participants who reported being very likely or almost certain to survive until that age declined monotonically. For example, among all participants who responded at baseline, 53% of participants reported being very likely or almost certain to survive until 50 years whereas only 40.9%, 28.1%, and 20.7% of participants reported being very likely or almost certain to survive until 60, 70, and 80 years, respectively. A similar pattern in survival expectations was observed in follow-up year 1 data.
Table 2.
Survival, health, and economic expectations of participants, by HIV status and over time in SEARCH intervention communities.
| Baseline
|
Follow-up year 1
|
|||||||
|---|---|---|---|---|---|---|---|---|
| HIV+, detectable viral load No. (%) | HIV+, undetectable viral load No. (%) | HIV-uninfected No. (%) | Full Sample No. (%) | HIV+, detectable viral load No. (%) | HIV+, undetectable viral load No. (%) | HIV-uninfected No. (%) | Full sample No. (%) | |
| Very likely or almost certain to survive to: | ||||||||
| 50 years | 204 (44.3) | 237 (56.6) | 619 (55.3) | 1060 (53.0) | 73 (50.7) | 468 (56.0) | 955 (65.7) | 1496 (61.5) |
| 60 years | 153 (30.2) | 203 (40.8) | 607 (45.0) | 963 (40.9) | 60 (38.2) | 478 (47.6) | 981 (55.3) | 1519 (51.7) |
| 70 years | 93 (19.5) | 133 (26.3) | 453 (31.6) | 679 (28.1) | 38 (26.0) | 315 (31.8) | 751 (39.8) | 1104 (36.5) |
| 80 years | 72 (15.3) | 93 (18.7) | 347 (23.0) | 512 (20.7) | 31 (22.0) | 214 (22.5) | 569 (29.2) | 814 (26.8) |
| Expects much better or somewhat better: | ||||||||
| Health in 1 year | 288 (56.8) | 279 (54.6) | 902 (57.7) | 1469 (56.9) | 104 (65.0) | 703 (67.0) | 1363 (64.9) | 2170 (65.6) |
| Health in 3 years | 313 (59.5) | 312 (58.3) | 1,004 (62.2) | 1629 (60.9) | 110 (67.1) | 744 (68.6) | 1478 (68.4) | 2332 (68.4) |
| Standard of living in | 239 (45.4) | 228 (42.6) | 739 (45.8) | 1206 (45.1) | 74 (45.1) | 534 (49.3) | 1194 (55.2) | 1802 (52.8) |
| community in 1 year | ||||||||
| Household financial well-being in 3 years | 258 (49.0) | 225 (42.1) | 808 (50.0) | 1291 (48.2) | 80 (48.8) | 577 (53.2) | 1216 (56.2) | 1873 (54.9) |
Notes: Analyses were limited to participants aged 18–80 years, with HIV status and HIV-1 viral load information. Expectations about survival to each of the target ages of 50, 60, 70, and 80 years were elicited from participants who were younger than the corresponding target age.
Figure 1.
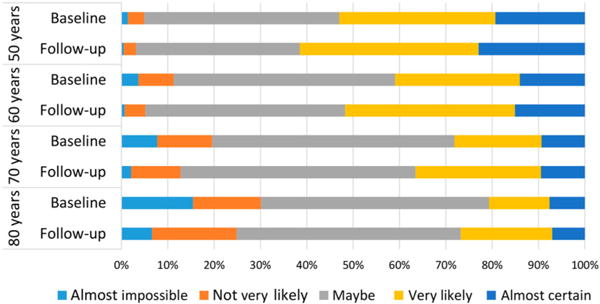
Trends in survival at baseline and follow-up year 1. Notes: Each bar represents participants’ subjective expectations to survive to age 50, 60, 70, and 80 using a 5-point Likert scale. Responses are presented separately for baseline and follow-up year 1. Expectations about survival to each of the target ages of 50, 60, 70, and 80 years were elicited from participants aged below the corresponding target age.
Survival expectations of participants changed considerably between baseline and follow-up (Figure 1). For each of the advanced ages that were discussed in the expectations surveys, a higher proportion of participants reported being very likely or almost certain to survive until that age at follow-up year 1 than at baseline. Similar shifts were observed in the expectations of one’s health status in 1 and 3 years from the time of the survey (not reported).
Measures of current health such as HIV status and viral load as well as expectations of future health were strongly associated with participants’ reported survival expectations at baseline (Table 3). Compared to HIV-positive adults with a detectable viral load, adults who were HIV-positive and had an undetectable viral load were significantly more likely to report being very likely or almost certain to survive to 50 years (unadjusted odds ratio [OR] 1.64, 95% CI 1.26–2.14). HIV-negative adults also had significantly higher expectations than HIV-positive adults with detectable viral load (OR 1.56, 95% CI 1.25–1.94). A similar pattern was observed for expectations of survival to ages of 60 and 70 years, although for these ages HIV-negative adults had slightly higher expectations than HIV-positive adults with undetectable viral load. For survival to age 80 years, there was no significant difference in expectations between HIV-positive adults with detectable and undetectable viral load (OR 1.28, 95% CI 0.91–1.79), but HIV-negative adults were significantly more likely to report being very likely or almost certain of survival than HIV-negative adults with detectable viral load (OR 1.66, 95% CI 1.26–2.19). In all of these analyses, post-estimation hypotheses testing that compared regression coefficients indicated there were no significant differences in expectations between HIV-negative persons and HIV-positive persons with undetectable viral load.
Table 3.
Bivariate logistic regression results at baseline
| Very likely or almost certain to survive to
|
||||
|---|---|---|---|---|
| 50 years OR [95% CI] |
60 years OR [95% CI] |
70 years OR [95% CI] |
80years OR [95% CI] |
|
| HIV status and viral load | ||||
| Ref: HIV+, detectable viral load | Ref. | Ref. | Ref. | Ref. |
| HIV+, undetectable viral load | 1.64*** [1.26–2.14] |
1.59*** [1.22–2.06] |
1.48* [1.10–2.00] |
1.28 [0.91–1.79] |
| HIV-status | 1.56*** [1.25–1.94] |
1.89*** [1.52–2.35] |
1.92*** [1.49–2.47] |
1.66*** [1.26–2.19] |
| Observations | 2000 | 2352 | 2415 | 2477 |
| Expected future health | ||||
| Better or much better health in 1 year | 1.90*** [1.58–2.29] |
1.80*** [1.51–2.13] |
1.63*** [1.35–1.96] |
1.63*** [1.32–2.00] |
| Observations | 1931 | 2270 | 2339 | 2403 |
| Much better health in 1 year | 2.92*** [2.19–3.88] |
2.34*** [1.84–2.98] |
1.84*** [1.44–2.35] |
1.79*** [1.38–2.33] |
| Observations | 1931 | 2270 | 2339 | 2403 |
| Better or much better health in 3 years | 1.91*** [1.58–2.29] |
1.81*** [1.52–2.15] |
1.50*** [1.24–1.82] |
1.54*** [1.25–1.89] |
| Observations | 2000 | 2352 | 2415 | 2477 |
| Much better health in 3 years | 2.77*** [2.20–3.48] |
2.06*** [1.69–2.51] |
1.56*** [1.27–1.92] |
1.50*** [1.20–1.88] |
| Observations | 2000 | 2352 | 2415 | 2477 |
Notes: OR, odds ratio; 95% CI, 95% confidence interval. Logistic regression model was used to separately examine the association between the binary dependent variables and each of the five independent variables: (1) HIV status and HIV-1 viral load; (2) better or much better health in 1 year; (3) much better health in 1 year; (4) better or much better health in 3 years; (5) much better health in 3 years in separate logistic regression models. For each of the target ages of 50, 60, 70, and 80 years, the sample was limited to participants who were younger than the target age. 95% confidence intervals calculated using robust standard errors clustered at the individual level are reported in brackets.
p < .05.
p < .001.
Further validation of expectations measures was obtained by comparing participants’ expectations about their future health with their survival expectations (Table 3). Relative to those who expected to be in worse or similar health in 3 years, those who expected to be in somewhat better or much better health were significantly more likely to report being very likely or almost certain to survive to each of the four target ages (for survival to 60 years, OR 1.81, 95% CI 1.52–2.15). In addition, those who expected to be in much better health generally had better survival expectations than those who expected to be in somewhat better health.
In models that combined data from baseline and follow-up year 1 and included controls for important individual- and household-level characteristics as well as community fixed effects and interviewer fixed effects (Table 4), the associations with HIV status and viral load largely remained evident. Survival expectations were also associated with gender and education. Women had a lower likelihood of reporting being very likely or almost certain to survive to the advanced ages, and individuals with secondary or more education had more favorable survival expectations. In general, older individuals who were closer to the ages specified in elicitations of survival expectations had higher odds of reporting being likely to survive to those ages, although these individuals were also significantly more likely to expect their health to deteriorate in the next year 1 year and 3 years.
Table 4.
Adjusted logistic regression results using pooled data from baseline and follow-up.
| Very likely or almost certain to survive to
|
Very likely or almost certain to have better
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 50 years AOR [95% CI] |
60 years AOR [95% CI] |
70 years AOR [95% CI] |
80 years AOR [95% CI] |
Health in 1 year AOR [95% CI] |
Health in 3 years AOR [95% CI] |
Standard of living in this community in 1 year AOR [95% CI] |
Household financial well-being in 3 years AOR [95% CI] |
|
| Follow-up year 1 indicator variable | 1.29** [1.10–1.53] |
1.53*** [1.31–1.77] |
1.72*** [1.48–2.01] |
1.72*** [1.45–2.03] |
2.12*** [1.82–2.47] |
1.63*** [1.40–1.89] |
1.49*** [1.29–1.71] |
1.41*** [1.23–1.61] |
| HIV status and viral load | ||||||||
| HIV+, detectable viral load | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| HIV+, undetectable viral load | 1.24 [0.98–1.57] |
1.41** [1.13–1.77] |
1.36* [1.05–1.75] |
1.08 [0.81–1.43] |
1.15 [0.91–1.44] |
1.21 [0.96–1.52] |
1.01 [0.81–1.25] |
1.05 [0.85–1.29] |
| HIV-status | 1.72*** [1.39–2.13] |
1.87*** [1.53–2.30] |
1.82*** [1.43–2.30] |
1.51** [1.16–1.96] |
0.87 [0.71–1.07] |
0.97 [0.78–1.19] |
0.94 [0.77–1.14] |
1.02 [0.84–1.23] |
| Female | 0.76*** [0.65–0.88] |
0.73*** [0.64–0.83] |
0.63*** [0.55–0.73] |
0.66*** [0.56–0.77] |
0.83** [0.73–0.95] |
0.86* [0.74–0.99] |
0.87* [0.76–0.99] |
0.75*** [0.66–0.85] |
| Age categories (Ref: 18–25) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 26–35 years old | 1.16 [0.97–1.39] |
1.03 [0.86–1.23] |
1.04 [0.85–1.28] |
1.04 [0.83–1.32] |
0.84 [0.69–1.03] |
0.80* [0.65–0.98] |
0.87 [0.72–1.06] |
0.84 [0.70–1.02] |
| 36–45 years old | 1.66*** [1.37–2.02] |
1.37** [1.13–1.65] |
1.14 [0.92–1.40] |
1.08 [0.85–1.37] |
0.62*** [0.50–0.76] |
0.51*** [0.41–0.62] |
0.88 [0.72–1.06] |
0.60*** [0.50–0.73] |
| 46–80 years old | 3.02*** [2.24–4.08] |
2.84*** [2.32–3.46] |
2.63*** [2.16–3.21] |
2.08*** [1.67–2.59] |
0.45*** [0.37–0.54] |
0.39*** [0.32–0.47] |
0.76** [0.64–0.92] |
0.43*** [0.36–0.52] |
| Education (Ref: None) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Primary education | 1.06 [0.81–1.39] |
1.18 [0.96–1.47] |
1.36** [1.11–1.67] |
1.15 [0.92–1.44] |
1.59*** [1.32–1.91] |
1.52*** [1.27–1.82] |
1.27** [1.07–1.52] |
1.83*** [1.52–2.20] |
| Secondary or more education | 1.72*** [1.28–2.32] |
1.87*** [1.47–2.39] |
1.89*** [1.49–2.40] |
1.68*** [1.30–2.19] |
2.49*** [1.99–3.13] |
2.39*** [1.90–3.00] |
1.97*** [1.59–2.45] |
3.38*** [2.71–4.21] |
| Married/cohabiting | 1 [0.85–1.17] |
1.15 [0.99–1.33] |
1.03 [0.89–1.20] |
0.97 [0.82–1.15] |
1.30*** [1.12–1.49] |
1.34*** [1.16–1.55] |
1.14 [1.00–1.31] |
1.46*** [1.27–1.67] |
| Observations | 4423 | 5277 | 5432 | 5406 | 5880 | 6073 | 6079 | 6073 |
| Number of clusters | 3103 | 3664 | 3851 | 3894 | 4100 | 4170 | 4173 | 4170 |
| Community fixed effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Interviewer fixed effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Notes: AOR, adjusted odds ratio; 95% CI, 95% confidence interval. Logistic regression models included HIV status and HIV-1 viral load, gender, age categories, education categories, marital status, community fixed effects, and interviewer fixed effects. For each of the target ages of 50, 60, 70, and 80 years, the sample was limited to participants who were younger than the target age. 95% confidence intervals calculated using robust standard errors clustered at the individual level are reported in brackets.
p < .05.
p <.01.
p < .001.
Expectations about survival to advanced ages, health status, and financial well-being of one’s household and community became significantly more favorable over time. For example, participants were more likely to report being very likely or almost certain to survive until 60 years in year 1 than at baseline (adjusted odds ratio (AOR) 1.53, 95% CI 1.31–1.77). Similar time trends were found in expectations about health in 1 year (AOR 2.12, 95% CI 1.82–2.47) and 3 years (AOR 1.63, 95% CI 1.40–1.89). Between baseline and follow-up year 1, participants in SEARCH intervention communities also developed more favorable expectations about the future standard of living of their own community (for reporting that the standard of living would be somewhat or much better, AOR 1.49, 95% CI 1.29–1.71). A similar time trend was observed in expectations the economic well-being of their own household would be somewhat or much better (AOR 1.41, 95% CI 1.23–1.61). These time trends in expectations were also found in models that excluded all covariates and only included measures of HIV status and viral load (Appendix Table 1A), as well as models with individual fixed effects that used data from only those individuals appearing in both waves of data collection and controlled for time-invariant individual characteristics (Appendix Table 2).
Discussion
This study assesses patterns in individuals’ health, survival, and economic expectations in a large sample of adults in Kenya and Uganda that includes sizable numbers of HIV-positive and HIV-negative adults. Individuals’ subjective assessments of their likelihood of surviving to advanced ages were largely correlated with objective measures of health status, including HIV status and an indicator of whether those who were HIV-positive were virally suppressed. The measures of subjective life expectancy were validated by comparisons to individuals’ expectations about their future health. In addition, individuals’ expectations about their future health, life expectancy, and economic circumstances became more favorable over time. This positive trend was observed among both HIV-positive and HIV-negative adults in the SEARCH intervention communities.
A key finding in this study was that HIV-positive individuals with an undetectable viral load had relatively similar expectations about survival to advanced ages as HIV-negative adults. Moreover, compared to HIV-positive individuals with a detectable viral load, expectations to survive to advanced ages were significantly higher among both HIV-negative individuals and HIV-positive individuals with an undetectable viral load. These findings are consistent with the possibility that HIV-positive individuals who realize the well-documented individual health benefits of ART initiation (Cohen et al., 2011) and information received in viral load counseling tend to update their expectations about future health, a finding that has not been reported previously.
Other findings in this study provide support for the validity of the expectations measures and their value in evaluations of health interventions, including universal test and treat interventions. Survival expectations elicited from individuals had an education gradient that is consistent with life expectancies among individuals of different education levels, and expectations of survival declined as the target age increased. These and other patterns in individuals’ subjective expectations were comparable to those reported in a few other population-based studies conducted in SSA. As observed in Malawi (Delavande & Kohler, 2009) and in high-income countries, despite having greater life expectancies than men, women reported a lower subjective expectation of survival to advanced ages than men (Delavande & Rohwedder, 2011; Hurd & McGarry, 1995).
A striking finding is that in the SEARCH trial communities, individuals’ subjective expectations about their likelihood of survival to advanced ages increased significantly over a one year period. Explanations for the sizable, positive trend in expectations include the multi-disease screening and services provided at CHCs, which enabled many individuals to learn whether they had HIV (Chamie et al., 2016) and also receive prompt referral to care, particularly ART irrespective of CD4 count for those who were HIV-positive. Actual improvements in the health of individuals and others in their networks could have also bolstered optimism about future health and survival to advanced ages. Explanations related to ART expansion would be consistent with several studies showing that ART expansion has led to substantial reductions in mortality and gains in life expectancy (Bendavid, Holmes, Bhattacharya, & Miller, 2012; Bor, Herbst, Newell, & Barnighausen, 2013) as well as improvements in economic conditions (Bor, Tanser, Newell, & Barnighausen, 2012; Thirumurthy, Zivin, & Goldstein, 2008; Wagner, Barofsky, & Sood, 2015). However, to our knowledge this is the first study to examine trends in individuals’ subjective expectations about health, survival, and economic conditions following expanded ART provision. Despite these potential explanations, it is also possible that other unrelated factors may have influenced these measures. Future research that utilizes additional longitudinal data and compares SEARCH intervention and control communities can be useful for better understanding these trends.
There are several limitations of this study that should be noted. Because trends in the SEARCH intervention communities were not compared to those in control communities, where CHCs did not occur by design in year 1, it is not possible to assess whether the observed changes in expectations were due to the implementation of universal test and treat interventions. Instead, these data are useful for studying factors associated with individuals’ expectations and for generating hypotheses about the likely role of ART scale-up in influencing these expectations. Because our study measured expectations using a Likert scale instead of a probabilistic scale, as some other studies have done (Delavande et al., 2011; Delavande & Kohler, 2009), our data cannot be used to compute specific life expectancies held by individuals. The methodology we used can make interpersonal comparisons more challenging, but this can be overcome by reliance on longitudinal data instead. Moreover, probabilistic expectations measures have other drawbacks, as individuals have been shown to substantially overestimate their mortality risk (Delavande & Kohler, 2009). Finally, the results presented here do not address whether individuals’ expectations influence their forward-looking behaviors, which is a question that will be examined in our future work.
As major investments in improving population health are undertaken, measuring subjective expectations of individuals can be useful for assessing whether objective improvements in health status are accompanied by changes in individuals’ expectations. The findings reported here are largely supportive of the hypothesis that bold efforts to eliminate new HIV infections through a “test and treat” strategy can contribute to positive changes at the population level in individuals’ expectations about their future health and well-being. However, definitive conclusions can only be drawn after making comparisons to SEARCH trial communities that have received the standard of care, including ART according to country guidelines.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, PEPFAR, or Gilead. The SEARCH project gratefully acknowledges the Ministries of Health of Uganda and Kenya, our research team, collaborators and advisory boards, and especially all communities and participants involved.
Funding
This work was supported by the Division of AIDS of National Institute of Allergy and Infectious Diseases [U01AI099959], and in part by the President’s Emergency Plan for AIDS Relief and Gilead Sciences. Thirumurthy acknowledges support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development [K01HD061605].
Appendix Table 1A.
Unadjusted logistic regression results using pooled data from baseline and follow-up.
| 50 years OR [95% CI] |
60 years OR [95% CI] |
70 years OR [95% CI] |
80 years OR [95% CI] |
Health in 1 year OR [95% CI] |
Health in 3 years OR [95% CI] |
Standard of living in this community in 1 year OR [95% CI] |
Household financial well-being in 3 years OR [95% CI] |
|
|---|---|---|---|---|---|---|---|---|
| Follow-up year 1 indicator variable | 1.34*** [1.18–1.51] |
1.45*** [1.30–1.62] |
1.40*** [1.25–1.57] |
1.37*** [1.21–1.55] |
1.44*** [1.29–1.60] |
1.38*** [1.24–1.54] |
1.37*** [1.24–1.52] |
1.32*** [1.20–1.46] |
| HIV status and viral load | ||||||||
| Ref: HIV+, detectable viral load | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| HIV+, undetectable viral load | 1.34** [1.10–1.65] |
1.50*** [1.22–1.83] |
1.40** [1.11–1.76] |
1.17 [0.91–1.50] |
1.02 [0.84–1.24] |
1.03 [0.85–1.25] |
0.93 [0.78–1.12] |
0.91 [0.75–1.09] |
| HIV status | 1.70*** [1.41–2.05] |
1.94*** [1.62–2.33] |
1.92*** [1.55–2.37] |
1.61*** [1.28–2.03] |
1.01 [0.85–1.20] |
1.09 [0.91–1.30] |
1.14 [0.96–1.35] |
1.10 [0.92–1.30] |
| Observations | 4433 | 5289 | 5438 | 5516 | 5889 | 6086 | 6086 | 6086 |
| Number of clusters | 3108 | 3670 | 3854 | 3944 | 4105 | 4177 | 4177 | 4177 |
Notes: OR, odds ratio; 95% CI, 95% confidence interval. Logistic regression models included an indicator variable for follow-up year 1 and controls for HIV status and HIV-1 viral load. For each of the target ages of 50, 60, 70, and 80 years, the sample was limited to participants who were younger than the target age. Ninety-five percentage confidence intervals calculated using robust standard errors clustered at the individual level are reported in brackets.
p < .01.
p < .001.
Appendix Table 2.
Linear probability models with individual fixed effects.
| Very likely or almost certain to survive to
|
Very likely or almost certain to have better
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 50 years
|
60 years
|
70 years
|
80 years
|
Health in 1 year
|
Health in 3 years
|
Standard of living in this community in 1 year
|
Household financial well-being in 3 years
|
|
| Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
Coef. [95% CI] |
|
| Follow-up year 1 indicator variable | 0.19** [0.06–0.31] |
0.34*** [0.22–0.46] |
0.24*** [0.11–0.37] |
0.21** [0.07–0.36] |
0.30*** [0.17–0.43] |
0.29*** [0.15–0.43] |
0.27*** [0.13–0.41] |
0.20** [0.07–0.34] |
| HIV status and viral load | ||||||||
| (Ref: HIV+, detectable viral load) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| HIV+, undetectable viral load* Year 1 | −0.16 [−0.34–0.01] |
−0.19* [−0.35–−0.03] |
−0.13 [−0.30–0.05] |
−0.07 [−0.27–0.12] |
−0.11 [−0.29–0.07] |
−0.12 [−0.30–0.07] |
−0.27** [−0.46–−0.08] |
−0.06 [−0.24–0.12] |
| HIV-status* Year 1 | −0.03 [−0.18–0.12] |
−0.13 [−0.27–0.00] |
−0.02 [−0.17–0.13] |
−0.06 [−0.22–0.11] |
−0.12 [−0.27–0.03] |
−0.10 [−0.26–0.06] |
−0.01 [−0.17–0.15] |
−0.06 [−0.21–0.09] |
| Number of observations | 2,928 | 3,550 | 3,436 | 3,406 | 3,902 | 4,180 | 4,180 | 4,180 |
| Number of individuals | 1,464 | 1,775 | 1,718 | 1,703 | 1,951 | 2,090 | 2,090 | 2,090 |
Abbreviations: Coef., coefficient; 95% CI, 95% confidence interval. Linear regression models included indicator variable for follow-up year 1, indicator variables for baseline HIV/viral load status, and an interaction between these variables and year 1. Sample was restricted to participants who answered questions in each wave. P-values notation:
p < 0.001,
p <0.01.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Balzer LB, Petersen ML, van der Laan MJ, SEARCH Consortium Adaptive pair-matching in randomized trials with unbiased and efficient effect estimation. Statistics in Medicine. 2015;34(6):999–1011. doi: 10.1002/sim.6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker G. Human capital. Chicago, IL: University of Chicago Press; 1964. [Google Scholar]
- Ben-Porath Y. The production of human capital and the life cycle of earnings. Journal of Political Economy. 1967;75:352–365. [Google Scholar]
- Bendavid E, Holmes CB, Bhattacharya J, Miller G. HIV development assistance and adult mortality in Africa. The Journal of the American Medical Association. 2012;307(19):2060–2067. doi: 10.1001/jama.2012.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Herbst AJ, Newell ML, Barnighausen T. Increases in adult life expectancy in rural South Africa: Valuing the scale-up of HIV treatment. Science. 2013;339(6122):961–965. doi: 10.1126/science.1230413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Tanser F, Newell ML, Barnighausen T. In a study of a population cohort in South Africa, HIV patients on antiretrovirals had nearly full recovery of employment. Health Affairs. 2012;31(7):1459–1469. doi: 10.1377/hlthaff.2012.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamie G, Clark TD, Kabami J, Kadede K, Ssemmondo E, Steinfeld R, Charlebois ED. A hybrid mobile approach for population-wide HIV testing in rural east Africa: An observational study. The Lancet HIV. 2016 doi: 10.1016/S2352-3018(15)00251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Fleming TR. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delavande A, Gine X, McKenzie D. Measuring subjective expectations in developing countries: A critical review and new evidence. Journal of development economics. 2011;94:151–163. [Google Scholar]
- Delavande A, Kohler HP. Subjective expectations in the context of HIV/AIDS in Malawi. Demographic Research. 2009;20:817–875. doi: 10.4054/DemRes.2009.20.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delavande A, Rohwedder S. Differential survival in Europe and the United States: Estimates based on subjective probabilities of survival. Demography. 2011;48:1377–1400. doi: 10.1007/s13524-011-0066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortson J. Mortality risk and human capital investment: The impact of HIV/AIDS in sub-Saharan Africa. Review of Economics and Statistics. 2011;93(1):1–15. [Google Scholar]
- Grosh M, Glewwe P. Designing household survey questionnaires for developing countries: Lessons from 15 years of the living standards measurement study. Washington, DC: The World Bank; 2000. Vols 1, 2, and 3. [Google Scholar]
- Hurd M, McGarry K. Evaluation of the subjective probabilities of survival in the health and retirement study. Journal of Human Resources. 1995;30:s268–s292. [Google Scholar]
- Hurd M, McGarry K. The predictive validity of subjective probabilities of survival. The Economic Journal. 2002;112:966–985. [Google Scholar]
- Jayachandran S, Lleras-Muney A. Life expectancy and human capital investments: Evidence from maternal mortality declines. Quarterly Journal of Economics. 2009;124(1):349–397. [Google Scholar]
- Kalemli-Ozcan S. Does the mortality decline promote economic growth? Journal of Economic Growth. 2002;7:411–439. [Google Scholar]
- Manski CF. Measuring expectations. Econometrica. 2004;72:1329–1376. [Google Scholar]
- Oster E, Shoulson I, Dorsey ER. Limited life expectancy, human capital and health investments. American Economic Review. 2013;103(5):1977–2002. doi: 10.1257/aer.103.5.1977. [DOI] [PubMed] [Google Scholar]
- Soares R. Mortality reductions, educational attainment and fertility choice. American Economic Review. 2005;95:580–601. doi: 10.1257/0002828054201486. [DOI] [PubMed] [Google Scholar]
- Thirumurthy H, Zivin JG, Goldstein M. The economic impact of AIDS treatment: Labor supply in western Kenya. The Journal of Human Resources. 2008;43(3):511–552. [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. HIV treatment in Africa: A looming crisis. Geneva: UNAIDS; 2015. [Google Scholar]
- Wagner Z, Barofsky J, Sood N. PEPFAR funding associated with an increase in employment among males in ten sub-Saharan African countries. Health Affairs. 2015;34(6):946–953. doi: 10.1377/hlthaff.2014.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]


