Abstract
Tonometry is a fundamental procedure in routine ophthalmologic examination. Although regarded as the reference standard, the Goldmann applanation tonometer (GAT) has its limitations. A new portable alternative to the GAT is the iCare rebound tonometer (RT). The aim of the present study was to compare the intraocular pressure (IOP) results obtained using the RT and GAT and then correlate the results with the central corneal thickness (CCT). Moreover, the tolerability and safety of the RT were evaluated. The IOP of 336 patients (672 eyes) was determined by the RT and GAT. The patients were divided into three groups (group A, 7–15 mmHg, n=74; group B, 16–22 mmHg, n=218; and group C, 23–50 mmHg, n=44), based on the GAT IOP readings. Pachymetry and slit lamp inspection were also performed. To establish an agreement between the devices, a Bland-Altman analysis and paired t-test were performed. The correlation between CCT and IOP readings obtained by the two devices were assessed using linear regression correlation analysis. The mean IOP values of the RT and the GAT were 18.30±5.10 and 18.52±4.46 mmHg, respectively. There were no significant differences between them (t=−1.31, P=0.19). The 95% confidence interval of the differences between the two devices was −5.80–6.24 mmHg. The RT readings are correlated well with those of GAT (r=0.806, P=0.001). However, the RT measurements were significantly (t=−2.84, P=0.007) lower (−1.66±3.87 mmHg) than those obtained with GAT when GAT ≥23 mmHg. Both the RT (r=0.390, P=0.001) and the GAT (r=0.191, P=0.001) showed positive correlations with CCT. The IOP measurement with RT was well tolerated. None of the corneal epithelial defects was detected and all subjects denied discomfort. The RT is well tolerated and safe, and can be considered a reliable alternative to GAT for patients in a low to moderate IOP range. However, in patients with high IOP values, the measurements obtained with RT did not correlate well with those obtained by GAT. The RT readings are influenced more by CCT compared to GAT.
Keywords: iCare rebound tonometer, Goldmann applanation tonometry, intraocular pressure, central corneal thickness
Introduction
Tonometry is a fundamental procedure in routine ophthalmologic examination. Accurate measurements of intraocular pressure (IOP) are key to diagnosing and monitoring glaucoma (1–4). The Goldmann applanation tonometer (GAT) is regarded as the reference standard in tonometry in current clinical practice (5). The GAT uses a small probe to gently flatten a part of the cornea to measure eye pressure and a microscope known as a slit lamp to examine the eye. The pressure in the eye is measured by the amount of force required to flatten the cornea. This type of tonometry is extremely accurate and is often used to measure IOP after a simple screening test. The iCare rebound tonometer (RT) is a new type of portable tonometer. It calculates IOP by measuring the motion parametric variation after the probe strikes the cornea. Compared with the GAT, the RT is handy, convenient and independent from other equipment.
In the present study, the two tonometers were compared to assess the reliability of applying RT in clinical procedures.
Patients and methods
General information
In total, 336 patients (672 eyes) from the Department of Ophthalmology, the First People's Hospital of Xiangyang (Hubei, China) from January 2013 to October 2013 were recruited to participate in this study. There were 151 males and 185 females whose ages ranged from 23 to 81, with an average age of 53 years. The patients were diagnosed with glaucoma and suspected glaucoma (150 patients), ametropia (91 patients) and other eye diseases (95 patients). Patients with corneal cicatrix, corneal edema and corneal refractive surgeries as well as those with corneal astigmatism ≥3D were excluded from the study. Ratified by the Ethics Committee of the hospital, all the subjects were informed of the purpose and process of this study, and signed informed consents before the examination.
Major measuring equipment
The Goldmann AT 900 applanation tonometer (Hagg-Streit AG, Koeniz, Switzerland); iCare TA01i rebound tonometer (Tiolat Oy, Helsinki, Finland); and the DGH Pachette 3 cornea thickness meter (DGH Technology Inc., Exton, PA, USA) were used to conduct this study.
Methods
Tonometry
To obtain the IOP reading using the RT, the one-off probe was changed for each reading and the patient was required to be seated, staring straight ahead at the 0.05 sighting mark within a distance of 5 meters. The frontal support bar was adjusted to position the probe at the same height as the corneal vertex at about 4–8 mm. The probe was vertical to the central corneal plane. After obtaining six successful measurements by continuous measurements, the iCare analyzes the data automatically and displays the IOP. Based on the standard deviation of the measurements, the tonometer showed 4 types of error bars - null, low, medium and high. This study only recorded IOP results with null error bar; otherwise, another measurement would be implemented.
To obtain the IOP reading using the GAT, the patient was seated and was required to stare at the 0.05 sighting mark within a distance of 5 meters. According to conventional methods, the eyelid margins and eyelashes could not be touched when the head was pressed, and the eyeball should not receive any external pressure when lightly lifting the upper eyelid during the measurement. The reading was carried out three times and if the difference value was within ±1 mmHg, the medium value was recorded as the result of this IOP measurement.
When measuring the IOP, the RT and GAT were operated by Q. Zhao and F. Gao, respectively. Considering that the eyeball massage effect occurring during the examination would lower the IOP, every patient was tested with the RT first. The doctor who operated the GAT had no knowledge of the RT measurements before each examination. The measurements of two tonometers were completed within 10 min. During the examination, the right eye was tested first and then the left. Only the measured values of the right eyes were used to conduct the statistical analysis.
The RT tolerance and security measurement using the visual analog scale (VAS) was used to evaluate the degree of comfort during the examination
Patients were required to mark the comfort level of the RT measurement in a calibrated line segment with one end (0) referring to pain while the other end (10) referring to comfort in order to quantitate the record results. After the RT measurement, the corneal fluorescein dye was inspected under the slit lamp and used to record the integrity of the patients' corneal epithelium.
Central corneal thickness (CCT) measurement
The central part of the pupil was selected to locate the central cornea. After measuring for five times, the minimum value was recorded as the result.
Statistical method
The SPSS 17.0 statistical software (Chicago, IL, USA) was used to conduct the statistical analysis. The measured data in this study are shown as mean ± SD. According to the K-S verification, the IOP values measured by the RT and GAT conformed to the normal distribution. The consistency of the RT and GAT measurements were analyzed by Bland-Altman with a paired t-test to indicate the differences between the two. The correlation among the RT, GAT and CCT were assessed with the Pearson linear regression correlation analysis. P<0.05 indicates a statistical significance.
Results
Consistency of the RT and GAT measurements
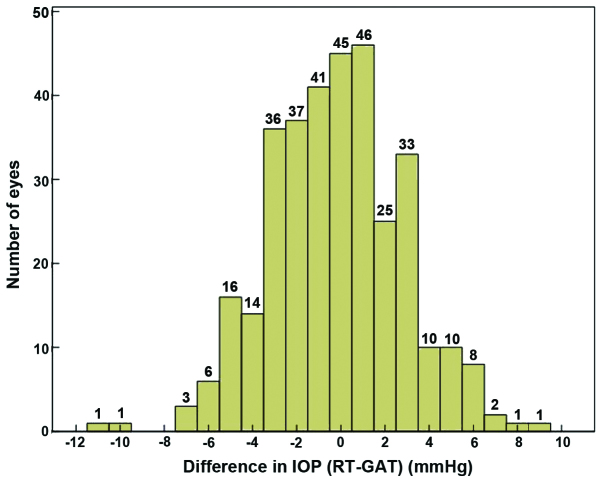
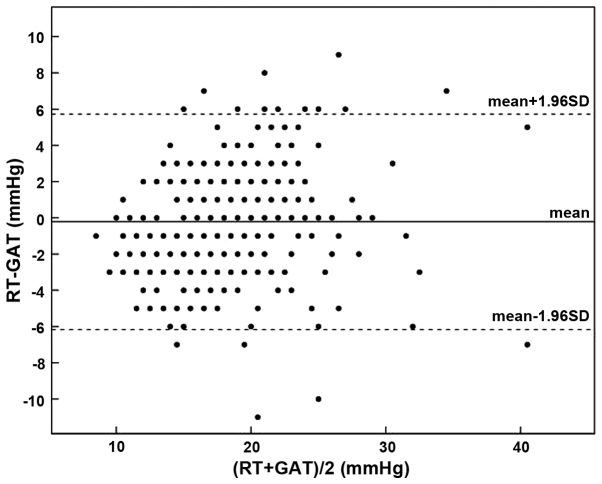
The average IOP value of the 336 right eyes measured by the RT and GAT were 18.30±5.10 and 18.52±4.46 mmHg, respectively. The RT readings were relatively lower than those obtained by GAT. However, their difference had no statistical significance (t=−1.31, P=0.19) (Table I). As shown by the linear regression analysis, the measurements of the two tonometers had a significant correlation (r=0.806, P=0.001). The measurement difference of the tested 263 eyes (78.3%) was ≤ ±3 mmHg, with its distribution shown in Fig. 1. The Bland-Altman diagram showed that the difference value between the RT and GAT measurements was −0.22±3.07 mmHg, with a 95% confidence interval (CI) of −5.80–6.24 mmHg (Fig. 2).
Table I.
Measured IOP values of RT and GAT.
| RT (mmHg) | GAT (mmHg) | ΔIOP (mmHg) | |
|---|---|---|---|
| Mean ± SD | 18.30±5.10 | 18.52±4.46 | −0.22±3.07 |
| Range | 8–43 | 9–44 | −11–9 |
| 95% CI | 8.30–28.30 | 9.78–27.78 | −5.80–6.80 |
ΔIOP=RT-GAT. IOP, intraocular pressure; RT, rebound tonometer; GAT, Goldmann applanation tonometer; CI, confidence interval.
Figure 1.
Distribution histogram of the difference in IOP (RT - GAT). IOP, intraocular pressure; RT, rebound tonometer; GAT, Goldmann applanation tonometer.
Figure 2.
Difference of the RT and GAT measurements analyzed by Bland-Altman. RT, rebound tonometer; GAT, Goldmann applanation tonometer.
According to the IOP value measured by GAT and ISO 8612 (6), tested patients were classified into three groups: group A, 7–15 mmHg, n=74; group B, 16–22 mmHg, n=218; and group C, 23–50 mmHg, n=44. As shown by the group comparison (Table II), when GAT measurement fell into the range of 7–15 and 16–22 mmHg, the difference of the IOP value measured by the RT and the GAT was quite small and of no statistical significance, which were −0.12±2.77 and 0.04±2.86 mmHg, respectively. However, when the GAT reading was ≥23 mmHg, the RT measurement −1.66±3.87 mmHg was significantly lower than those obtained with the GAT. The difference was statistically significant (t=−2.84, P=0.007). Moreover, 95% CI (−9.25–5.93) of the difference increased significantly. The measurement difference of 206 eyes (61.4%) was ≤ ±3 mmHg while that of 76 eyes (22.7%) was > ±5 mmHg.
Table II.
RT and GAT measured values of three different IOP groups.
| Group A (IOP 7–15 mmHg, n=74) | Group B (IOP 16–22 mmHg, n=218) | Group C (IOP 23–50 mmHg, n=44) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RT | GAT | RT | GAT | RT | GAT | ||||
| Mean ± SD | 13.28±3.09 | 13.41±1.60 | 18.64±3.58 | 18.60±1.85 | 25.07±5.54 | 26.73±4.44 | |||
| Range | 8–20 | 9–15 | 11–31 | 16–12 | 15–43 | 23–44 | |||
| ΔIOP (mmHg) | −0.12±2.77 | 0.04±2.86 | −1.66±3.87 | ||||||
| (mean ± SD) | (t=−0.38, P=0.71) | (t=0.21, P=0.83) | (t=−2.84, P=0.007) | ||||||
| 95% CI | −5.66–5.66 | −5.57–5.57 | −9.25–5.25 | ||||||
| ΔIOP ≤ ±3 mmHga | 83.7% | 79.8% | 61.4% | ||||||
| ΔIOP > ±5 mmHgb | 2.7% | 5.5% | 22.7% | ||||||
ΔIOP = RT - GAT.
The percentage of the difference between RT and GAT measured IOP values is with ±3 mmHg.
The percentage of the difference between RT and GAT measured IOP values is more than ±5 mmHg. RT, rebound tonometer; GAT, Goldmann applanation tonometer; IOP, intraocular pressure; CI, confidence interval.
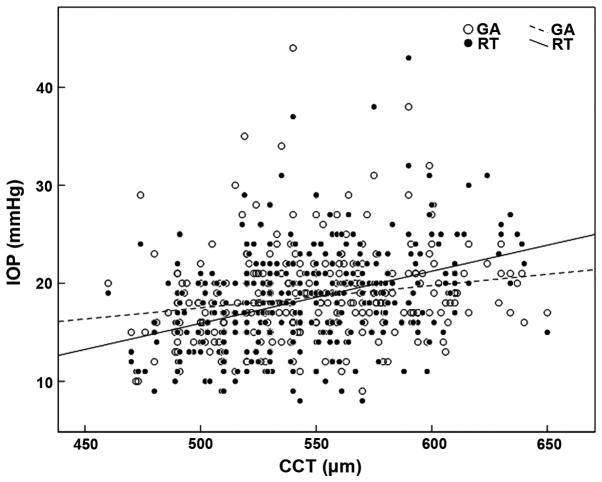
Correlation between the RT and GAT measured values and CCT
The linear regression analysis showed that the RT (r=0.390, P=0.001) and the GAT (r=0.191, P=0.001) showed a positive correlation with CCT. The impact of CCT on the RT was stronger than that following GAT. The equation of linear regression was RT=−10.67+0.053 × CCT and GAT=6.10+0.023 × CCT, respectively. The scatter diagram is shown in Fig. 3.
Figure 3.
Scatter diagram of the correlation between the CCT and IOP values measured with the RT and the GAT. CCT, central corneal thickness; IOP, intraocular pressure; RT, rebound tonometer; GAT, Goldmann applanation tonometer.
Security and endurance of the RT
After the RT measurement, no corneal epithelial defect was detected among the 336 tested patients. All the subjects denied discomfort with the average VAS of 9.82±1.05.
Discussion
Tonometry is a fundamental procedure in routine ophthalmologic examination. IOP is especially important for treating glaucoma. Although intraocular hypertension is not a requirement, it is still a significant risk factor in the development of glaucoma treatment (7,8). Lowering the IOP level is also the only effective treatment means to control the development of glaucoma in clinical practices. Therefore, accurately measuring IOP is crucial when diagnosing and monitoring glaucoma.
The anterior chamber cannula technique is the most accurate method to measure IOP directly (9). However, it is an invasive operation, as this method can only be applied in experimental research (10). In clinical applications, GAT is recognized as the global reference standard of tonometry (11–14). With relatively high accuracy, the GAT has become a standard to test the reliability of other tonometers in clinical applications. The iCare RT invented by Kontiola is a new type of portable tonometer, which calculates the tonometer through magnetic induction and records velocity change after the probe strikes the cornea (15–17). The RT measurement shows relatively high accuracy in rats and other animals. However, few studies with large sample size have been conducted concerning its clinical application.
This study, in which patients who had cornea-related diseases are removed, investigates 336 patients by using the GAT and the RT to measure IOP. The comparison shows that the results of two tonometers have a significant correlation (r=0.806, P=0.001), and the RT measurements are a little lower than those obtained with GAT (−0.22±3.07 mmHg) and have no statistical significance (t=−1.31, P=0.19). The Bland-Altman diagram shows that a 95% CI of the difference value is −5.80–6.24 mmHg and the difference value of 263 eyes (78.3%) ≤ ±3 mmHg, which is similar to Iliev et al (18) study of 95% CI −3.2–5.2 mmHg and difference value ≤ ±3 mmHg. All of these results indicate high consistency between the RT and the GAT.
When the tested eyes are further grouped with the IOP results obtained with the GAT, the results show that in the normal IOP range of 7–22 mmHg, the RT measurements are consistent with the overall results. However, in the high IOP values (23–50 mmHg), there is a significant difference between the RT and the GAT readings with the average of −1.66 mmHg (t=−2.84, P=0.007). However, this difference may not be of great significance in clinical practice (19). Considering that the discrete parameter SD (3.87) and 95% CI (−9.25–5.93) are on the increase, we still think that we should be cautious in the clinical application since the measurement with the RT does not correlate well with the GAT in high IOP values.
Many studies (20,10) show that the GAT readings are influenced by CCT. When the corneal thickness increases by 10 µm, the GAT readings will increase by about 0.2 mmHg accordingly. This study verifies the results that we obtained while conducting this research. The linear regression equation of the GAT and the CCT are GAT=6.10+0.023 × CCT (r=0.191, P=0.001). Moreover, the RT shows a positive correlation with the CCT (RT=−10.67+0.053 × CCT; r=0.390, P=0.001). When the CCT increases by 10 µm, the RT readings will increase by about 0.5 mmHg. Besides, as the RT has a higher correlation coefficient than that of the GAT, the RT readings are influenced more by the CCT compared to the GAT. However, some studies (21,22) consider that the corneal biomechanical property including the corneal hysteresis (CH) and the corneal resistance factor (CRF) impose more influence on the IOP. Thus, the multivariate regression analysis is much more suitable to uncover and interpret the correlation among the IOP and CCT, and CH and CRF. The weaker correlation coefficient between the GAT, RT and CCT is shown in this study.
The RT probe weighs about 24 mg, and the radius of the plastic head end that contacts the cornea is about 0.9 mm. The speed of the probe striking the cornea is about 0.25–0.35 m/sec which is faster than a blink reflex. All these characteristics enable the RT measurement to be quick and comfortable. When compared with the GAT, the advantages of the RT measurement can be best reflected in patients who are disabled, have poor coordination, and those with corneal cicatrix (23).
In conclusion, the RT is well tolerated and safe, and is a reliable alternative to the GAT in patients with a low to moderate IOP range. However, in patients with high IOP values, the measurements obtained with RT do not correlate well with the GAT. The RT readings are influenced more by the CCT compared to the GAT. Beside, further investigations should be conducted to discuss the influence of corneal biomechanical properties with the GAT and RT measurements.
References
- 1.Tamburrelli FC, Genitiempo M, Bochicchio M, Donisi L, Ratto C. Cauda equina syndrome: evaluation of the clinical outcome. Eur Rev Med Pharmacol Sci. 2014;18:1098–1105. [PubMed] [Google Scholar]
- 2.Zicari AM, Rugiano A, Ragusa G, Savastano V, Bertin S, Vittori T, Duse M. The evaluation of adenoid hypertrophy and obstruction grading based on rhinomanometry after nasal decongestant test in children. Eur Rev Med Pharmacol Sci. 2013;17:2962–2967. [PubMed] [Google Scholar]
- 3.Portincasa P, Moschetta A, Giampaolo M, Palasciano G. Diffuse gastrointestinal dysmotility by ultrasonography, manometry and breath tests in colonic inertia. Eur Rev Med Pharmacol Sci. 2000;4:81–87. [PubMed] [Google Scholar]
- 4.Jiang SP, Huang LW. Role of gastroesophageal reflux disease in asthmatic patients. Eur Rev Med Pharmacol Sci. 2005;9:151–160. [PubMed] [Google Scholar]
- 5.Kass MA. Standardizing the measurement of intraocular pressure for clinical research. Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103:183–185. doi: 10.1016/S0161-6420(96)30741-0. [DOI] [PubMed] [Google Scholar]
- 6.Internationaler Standard für Augentonometer ISO 8612. Beuth-Verlag GmbH; Berlin: 2001. (In German) [Google Scholar]
- 7.Hu J, Bui KM, Patel KH, Kim H, Arruda JA, Wilensky JT, Vajaranant TS. Effect of hemodialysis on intraocular pressure and ocular perfusion pressure. JAMA Ophthalmol. 2013;131:1525–1531. doi: 10.1001/jamaophthalmol.2013.5599. [DOI] [PubMed] [Google Scholar]
- 8.Vyas P, Naik U, Gangaiah JB. Efficacy of bimatoprost 0.03% in reducing intraocular pressure in patients with 360° synechial angle-closure glaucoma: a preliminary study. Indian J Ophthalmol. 2011;59:13–16. doi: 10.4103/0301-4738.73708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsuura K, Suto C, Akura J, Inoue Y. Bag and chamber flushing: a new method of using intracameral moxifloxacin to irrigate the anterior chamber and the area behind the intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2013;251:81–87. doi: 10.1007/s00417-012-2098-1. [DOI] [PubMed] [Google Scholar]
- 10.Kohlhaas M, Boehm AG, Spoerl E, Pürsten A, Grein HJ, Pillunat LE. Effect of central corneal thickness, corneal curvature, and axial length on applanation tonometry. Arch Ophthalmol. 2006;124:471–476. doi: 10.1001/archopht.124.4.471. [DOI] [PubMed] [Google Scholar]
- 11.Eldaly MA. Goldmann versus disposable applanation tonometer tips in glaucoma patients and normal subjects. Curr Eye Res. 2015 Aug 19; doi: 10.3109/02713683.2015.1015144. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 12.Tamçelik N, Atalay E, Cicik E, Özkök A. Comparability of Icare pro rebound tonometer with Goldmann applanation and noncontact tonometer in a wide range of intraocular pressure and central corneal thickness. Ophthalmic Res. 2015;54:18–25. doi: 10.1159/000381781. [DOI] [PubMed] [Google Scholar]
- 13.Sinha G, Gupta S, Temkar S, Pandey V, Sihota R, Dada T. IOP agreement between I-Care TA01 rebound tonometer and the Goldmann applanation tonometer in eyes with and without glaucoma. Int Ophthalmol. 2014 Dec 16; doi: 10.1007/s10792-014-0026-6. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 14.Farhood QK. Comparative evaluation of intraocular pressure with an air-puff tonometer versus a Goldmann applanation tonometer. Clin Ophthalmol. 2013;7:23–27. doi: 10.2147/OPTH.S38418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee TE, Yoo C, Hwang JY, Lin S, Kim YY. Comparison of intraocular pressure measurements between Icare pro rebound tonometer and Tono-Pen XL tonometer in supine and lateral decubitus body positions. Curr Eye Res. 2014;40:1–7. doi: 10.3109/02713683.2014.964416. [DOI] [PubMed] [Google Scholar]
- 16.Lee YK, Lee JY, Moon JI, Park MH. Effectiveness of the ICare rebound tonometer in patients with overestimated intraocular pressure due to tight orbit syndrome. Jpn J Ophthalmol. 2014;58:496–502. doi: 10.1007/s10384-014-0350-4. [DOI] [PubMed] [Google Scholar]
- 17.Sanz Borrego L, Morales-Fernandez L, de-la-Casa Martínez JM, Sáenz-Francés F, Fuentes M, García-Feijóo J. The Icare-pro rebound tonometer versus the hand-held applanation tonometer in congenital glaucoma. J Glaucoma. 2016;25:149–154. doi: 10.1097/IJG.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 18.Iliev ME, Goldblum D, Katsoulis K, Amstutz C, Frueh B. Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. Br J Ophthalmol. 2006;90:833–835. doi: 10.1136/bjo.2005.089870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pakrou N, Gray T, Mills R, Landers J, Craig J. Clinical comparison of the Icare tonometer and Goldmann applanation tonometry. J Glaucoma. 2008;17:43–47. doi: 10.1097/IJG.0b013e318133fb32. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-de-la-Casa JM, Garcia-Feijoo J, Vico E, Fernandez-Vidal A, del Benitez Castillo JM, Wasfi M, Garcia-Sanchez J. Effect of corneal thickness on dynamic contour, rebound, and goldmann tonometry. Ophthalmology. 2006;113:2156–2162. doi: 10.1016/j.ophtha.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31:146–155. doi: 10.1016/j.jcrs.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 22.Chui WS, Lam A, Chen D, Chiu R. The influence of corneal properties on rebound tonometry. Ophthalmology. 2008;115:80–84. doi: 10.1016/j.ophtha.2007.03.061. [DOI] [PubMed] [Google Scholar]
- 23.Moreno-Montañés J, García N, Fernández-Hortelano A, García-Layana A. Rebound tonometer compared with goldmann tonometer in normal and pathologic corneas. Cornea. 2007;26:427–430. doi: 10.1097/ICO.0b013e318030df6e. [DOI] [PubMed] [Google Scholar]