Abstract
MicroRNAs (miRs) play critical roles in the development and malignant progression of human cancers. miR-148a has previously been found to inhibit the migration and invasion of breast cancer cells. However, the underlying mechanism of miR-148a in regulating the viability and migration of estrogen receptor (ER) α-positive breast cancer cells is still unknown. In this study, ERα-positive breast cancer MCF7 cells were treated with estradiol (E2). Data from MTT and wound healing assays showed that E2 treatment promoted the viability and migration of MCF7 cells. A bioinformatics analysis and luciferase reporter assay identified ERα as a direct target of miR-148a. Ectopic expression of miR-148a significantly decreased the protein expression of ERα (P<0.01), while knockdown of miR-148a significantly increased the ERα protein level in MCF7 cells (P<0.01). Furthermore, miR-148a overexpression significantly inhibited the E2-induced viability and migration of MCF7 cells (P<0.01), similar to the effect of silencing ERα. However, overexpression of ERα rescued the suppressed viability and migration caused by miR-148a upregulation. Finally, it was found that E2 treatment led to a significant decrease in the miR-148a level in MCF7 cells (P<0.01). These results suggest that miR-148a can suppress the E2-induced viability and migration of MCF7 breast cancer cells via inhibition of ERα protein expression, expanding the understanding of miR function in ERα-positive breast cancer.
Keywords: breast cancer, microRNA-148a, estrogen, estrogen receptor α
Introduction
Breast cancer is the most common malignant tumor type in females, and the second most common cancer type worldwide (1). It is the leading cause of cancer mortality in women, responsible for 14% of all cancer-related fatalities (2,3). Notable improvements in the diagnosis and treatment of breast cancer have been made in recent decades, and the mortality rate of this disease has decreased by more than 30% (2,3). A better understanding of the molecular mechanisms underlying the malignant progression of breast cancer will be beneficial for improving the efficacy of breast cancer treatment strategies (4).
Hormone 17-β-estradiol (E2), one of the most prevalent endogenous estrogens, has been found to be involved in physiological and pathological processes, including the development and malignant progression of breast cancer (5). E2 functions through activation of estrogen receptor (ER) α-mediated signaling pathways, which are involved in the mediation of cell proliferation, differentiation and migration, as well as homeostasis (6–8). Almost 70% of breast cancers are ERα positive (9), thus ERα has been developed into a therapeutic target for breast cancer (10,11). For instance, tamoxifen is a selective ER modulator and represents the standard treatment for the majority of breast cancer patients (9). However, the regulatory mechanism of ERα expression in breast cancer is still largely unknown.
MicroRNAs (miRs) are endogenous non-coding RNAs that can suppress gene expression by directly binding to the 3′untranslated region (3′UTR), causing translation inhibition or mRNA degradation (12). They have been demonstrated to play crucial roles in various biological processes, such as cell proliferation, differentiation, apoptosis and migration, as well as tumorigenesis (13,14). Moreover, the development and malignant progression of breast cancer is tightly associated with gene mutation and deregulation, as well as epigenetic mechanisms including miRs (15,16). Previously, downregulation of miR-148a has been implicated in breast cancer (17,18) and found to inhibit the migration and invasion of breast cancer cells (19,20). For instance, Jiang et al recently found that miR-148a suppressed the migration and invasion of breast cancer cells by directly targeting WNT-1 (19). Xue et al reported that miR-148a inhibited the migration of breast cancer cells by targeting MMP-13 (20). However, to the best of our knowledge, the exact role of miR-148a in ERα-positive breast cancer remains unclear. In the present study, we aimed to reveal the underlying mechanism of miR-148a in mediating E2-induced viability and migration of ERα-positive breast cancer cells.
Materials and methods
Cell culture and E2 treatment
A human embryonic kidney cell line, HEK293 and a human breast cancer cell line, MCF7, were obtained from the Cell Bank of Central South University (Changsha, China). MCF7 cells were cultured in Dulbecco's modified Eagle's medium (DMEM; Thermo Fisher Scientific, Inc., Waltham, MA, USA) with 10% fetal bovine serum (Thermo Fisher Scientific, Inc.) at 37°C with 5% CO2. MCF7 cells were treated with E2 for 3 h, then cell viability and migration rates were analyzed.
MTT assay
An MTT assay was used to examine cell viability. MCF7 cells (5,000 per well) were cultured in a 96-well plate. Each well contained 100 µl fresh serum-free DMEM with 0.5 g/l MTT. Following an incubation at 37°C for 0, 12, 24, 48 or 72 h, the medium was removed by aspiration and 50 µl dimethyl sulfoxide (5 mg/ml; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) was added to each well. After incubation at room temperature for 10 min, formazan production was detected by measuring the optical density at 570 nm using an AIA 600II Automated Enzyme Immunoassay Analyzer (Tosoh Corporation, Tokyo, Japan).
Wound healing assay
A wound healing assay was used to examine cell migration. MCF7 cells were cultured at 37°C with 5% CO2 to full confluence in 6-well plates. Wounds of ~1 mm width were created with a plastic scriber. After that, cells were washed with phosphate-buffered saline (PBS) and incubated at 37°C with 5% CO2 for 48 h. Then, the wounds were observed and photographed under an Eclipse Ti-E inverted microscope (Nikon Corporation, Tokyo, Japan).
Cell transfection
MCF7 cells were transfected with a scrambled miR mimic (Yearthbio, Changsha, China) as a negative control (miR-NC), an miR-148a mimic (Yearthbio), a negative control inhibitor (Yearthbio), an miR-148a inhibitor (Yearthbio), ERα siRNA (Yearthbio) or pcDNA3.1-ERα ORF plasmid (Yearthbio) using Lipofectamine® 2000 (Thermo Fisher Scientific, Inc.), in accordance with the manufacturer's protocols. Transfection efficiency was measured using reverse transcription-quantitative polymerase chain reaction (RT-qPCR) and western blotting as follows.
RT-qPCR assay
Total RNA from MCF7 cells was isolated using Trizol reagent (Thermo Fisher Scientific, Inc.), according to the manufacturer's instructions. Total RNA was reverse transcribed using the RevertAid Reverse Transcription kit (Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. Then, qPCR was conducted using the SYBR-Green miScript PCR kit (Qiagen, Inc., Valencia, CA, USA) and a Roche LightCycler 480 PCR machine (Roche Diagnostics, Basel, Switzerland). All primers were purchased from Sangon Biotech Co., Ltd. (Shanghai, China). The primers for ERα were: Forward, 5′-CCCACTCAACAGCGTGTCTC-3′ and reverse, 5′-CGTCGATTATCTGAATTTGGCCT-3′. The primers for GAPDH were: Forward, 5′-ACAACTTTGGTATCGTGGAAGG-3′ and reverse, 5′-GCCATCACGCCACAGTTTC-3′. The reaction conditions were: 95°C for 10 min, followed by 45 cycles of 95°C for 15 sec and 60°C for 30 sec. The relative mRNA expression of ERα was normalized against that of GAPDH. The relative expression of miR-148a was normalized against that of U6. The relative expression was analyzed by the 2−ΔΔCq method (21).
Western blot analysis
Cells were lysed using RIPA buffer (Beyotime Institute of Biotechnology, Shanghai, China). The concentration of protein was quantified using the Pierce BCA Protein Assay kit (Thermo Fisher Scientific, Inc.). After that, proteins (50 µg) were separated using 10% SDS-PAGE gels (Beyotime Institute of Biotechnology) and blotted onto a polyvinylidene difluoride (PVDF) membrane (Life Technologies, Grand Island, NY, USA), which was then blocked with 5% non-fat dried milk (Mengniu, Beijing, China) in PBS with Tween (PBST; Beyotime Institute of Biotechnology) overnight at 4°C. The PVDF membrane was then incubated with rabbit monoclonal anti-human ERα antibody (1:100; ab32063; Abcam, Cambridge, MA, USA), or rabbit monoclonal anti-human GAPDH antibody (1:100; ab9485; Abcam) antibody at room temperature for 3 h. After being washed with PBST three times, the PVDF membrane was incubated with goat anti-rabbit horseradish peroxidase-conjugated secondary antibody (1:5,000; ab7090; Abcam) for 40 min at room temperature. Chemiluminescent detection was performed with an ECL kit (Thermo Fisher Scientific, Inc.). The relative protein expression was determined using Image-Pro plus software version 6.0 (Media Cybernetics, Inc., Rockville, MD, USA), represented as the density ratio vs. GAPDH.
Bioinformatics analysis and luciferase reporter assay
TargetScan 3.1 online software (Whitehead Institute for Biomedical Research, Cambridge, MA, USA) was used to analyze the putative target genes of miR-148a (22).
A wild type (WT)-or mutant type (MT)-ERα 3′UTR was inserted downstream of the luciferase reporter gene in a pMIR-REPORT vector (Yearthbio), generating a WT-ERα-3′UTR reporter vector or MT-ERα-3′UTR reporter vector, respectively. HEK293 cells were co-transfected with miR-148a mimic (Yearthbio) or miR-NC (Yearthbio), a WT-ERα-3′UTR or MT-ERα-3′UTR reporter vector, and pRL-SV40 (Promega Corporation, Madison, WI, USA) expressing Renilla luciferase using Lipofectamine® 2000 according to the manufacturer's protocol. Following incubation at 37°C with 5% CO2 for 48 h, the luciferase activities were measured using the Dual-Luciferase Reporter Assay System (Promega Corporation), according to the manufacturer's instructions.
Statistical analysis
Data are expressed as the mean ± standard deviation of three independent experiments. The Student's t-test was used to compare differences between two groups. One-way analysis of variance was used to analyze differences among more than two groups. Statistical analysis was conducted using SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA) and P<0.05 was considered to indicate a statistically significant difference.
Results
E2 treatment promotes MCF7 cell viability and migration
It has been well established that MCF7 is an ERα-positive breast cancer cell line (23). In the current study, MCF7 were treated with E2 (1 mM) for 3 h, followed by analyses of cell viability and migration. MTT assay data indicated that MCF7 cell viability was significantly increased following treatment with E2 for 48 h (P<0.05) or 72 h (P<0.01), as compared with the control group (Fig. 1A). Furthermore, wound healing assay data showed that E2 treatment also upregulated the migration of MCF7 cells at 48 h, when compared to the control group (P<0.01; Fig. 1B). These results suggest that E2 activates ERα-mediated viability- and migration-related signaling pathways in MCF7 cells.
Figure 1.
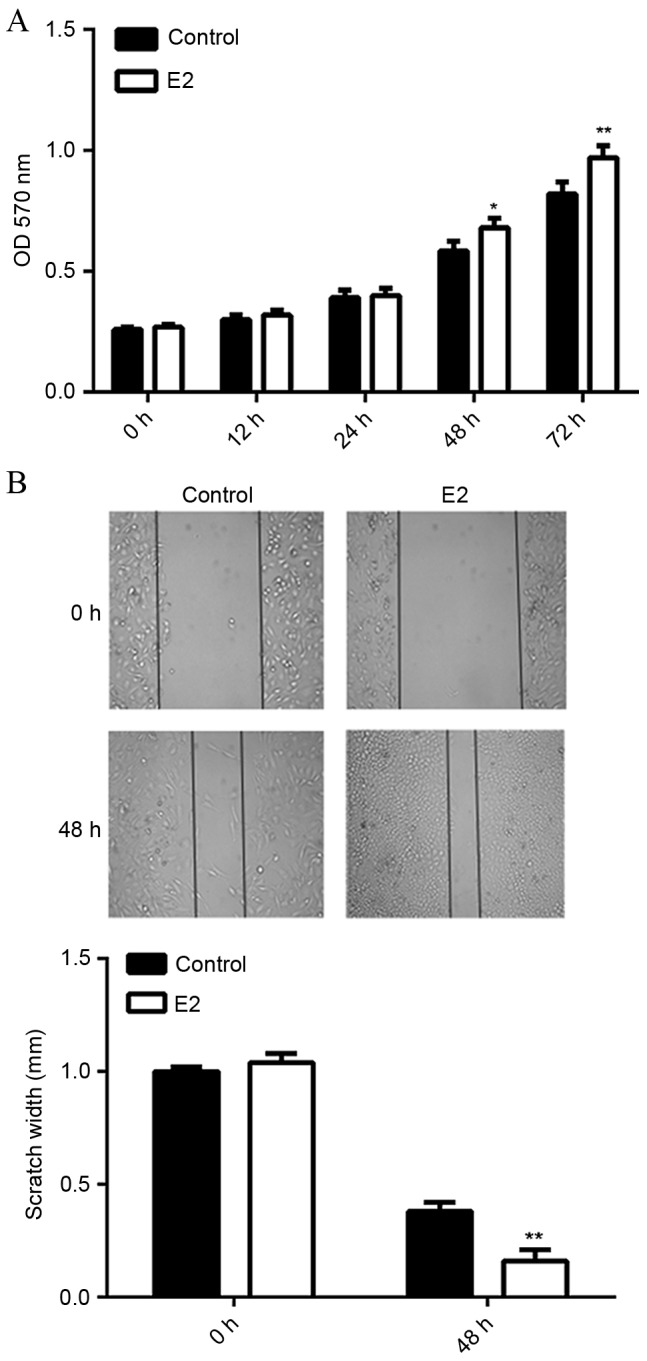
Effect of E2 treatment on MCF7 cell viability and migration. MCF7 cells were treated with 1 mM of E2 for 3 h. (A) MTT assay and (B) wound healing assay were used to evaluate cell viability and migration, respectively. Non-treated MCF7 cells were used as the control. *P<0.05 vs. control, **P<0.01 vs. control. OD, optical density; E2, estradiol.
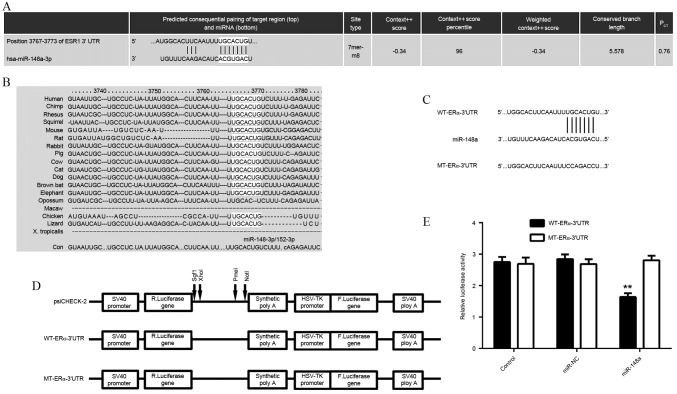
ERα is a direct target of miR-148a
As the function of E2 is through activation of ERα-mediated downstream signaling, a bioinformatics search was conducted for putative miRs that directly target ERα. As indicated in Fig. 2A and B, ERα was predicted to be a direct target of miR-148a, and the targeting relationship was evolutionarily conserved. In order to examine this targeting relationship, the WT- or MT-ERα-3′UTR was inserted downstream of the luciferase reporter gene in a pMIR-REPORT vector (Fig. 2C and D). A luciferase reporter assay demonstrated that transfection with the miR-148a mimic significantly reduced the luciferase activity in HEK293 cells transfected with WT-ERα-3′UTR reporter vector, but not in cells transfected with MT-ERα-3′UTR reporter vector, when compared to the control group (P<0.01; Fig. 2E). These findings indicated that ERα was a direct target of miR-148a.
Figure 2.
Bioinformatics and luciferase reporter assays to investigate miRNAs involved in ERα signaling pathways. (A and B) TargetScan software predicted that ERα (ESR1) was a target gene of miR-148a, and their targeting relationship was evolutionarily conserved. (C and D) WT or MT ERα-3′UTR was inserted downstream of the luciferase reporter gene in a pMIR-REPORT vector. (E) A luciferase reporter assay following co-transfection of the WT-ERα-3′UTR or MT-ERα-3′UTR reporter vector with an miR-148a mimic or a control miRNA in HEK293 cells. **P<0.01 vs. control. ERα, estrogen receptor α; miR, microRNA; WT, wild type; MT, mutant type; 3′UTR, 3′untranslated region; miR-NC, scrambled miR mimic.
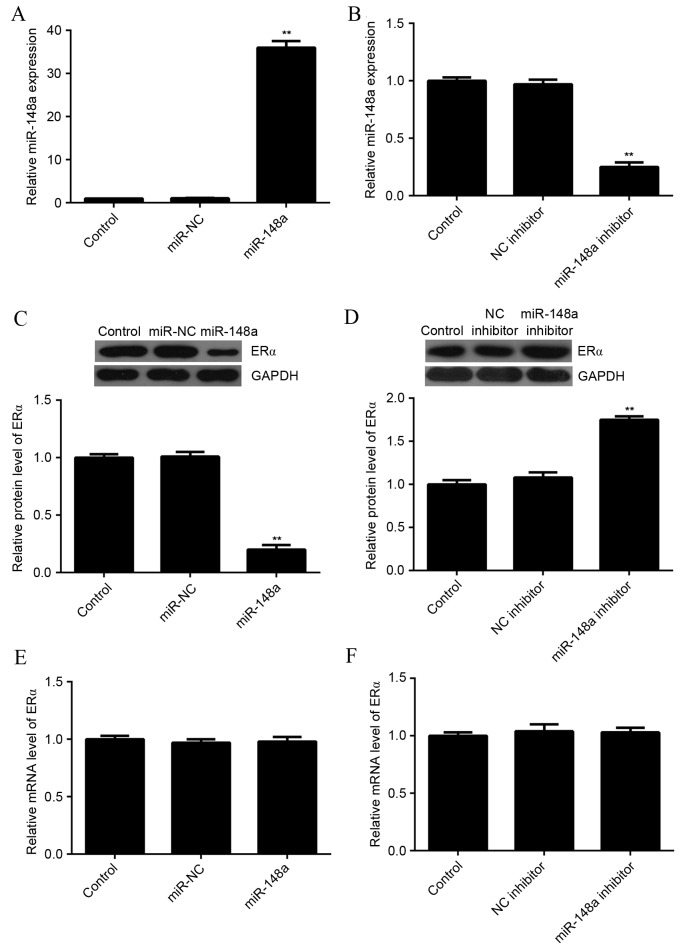
miR-148a negatively regulated the protein expression of ERα in MCF7 cells
As miRs most often inhibit the expression of their target genes at the post-transcriptional level, the effects of miR-148a upregulation and downregulation on the protein level of ERα in MCF7 cells were evaluated. MCF7 cells were transfected with miR-NC, miR-148a mimic, NC inhibitor, or miR-148a inhibitor. After transfection, qPCR was used to evaluate the level of miR-148a expression in each group. As indicated in Fig. 3A and B, transfection with an miR-148a mimic significantly increased the level of miR-148a expression, while transfection with an miR-148a inhibitor significantly decreased the level of miR-148a expression in MCF7 cells as compared with the control group (P<0.01 for both).
Figure 3.
Effect of miR-148a on ERα protein expression in MCF7 cells. (A and B) Using qPCR, the miR-148a level was evaluated in MCF7 cells transfected with miR-NC, miR-148a mimic, NC inhibitor or miR-148a inhibitor. (C and D) Western blot analysis and (E and F) qPCR were used to evaluate the protein and mRNA expression of ERα. Non-transfected MCF7 cells were used as the control. **P<0.01 vs. control. ERα, estrogen receptor α; NC, negative control; miR, microRNA; miR-NC, scrambled miR mimic; qPCR, quantitative polymerase chain reaction.
Next, a western blot analysis was conducted to determine the protein level of ERα. Overexpression of miR-148a significantly reduced the level of ERα protein (Fig. 3C), while knockdown of miR-148a significantly increased the level of ERα protein in MCF7 cells, as compared with the control (P<0.01 for both; Fig. 3D). In addition, neither miR-148a upregulation nor downregulation affected the mRNA expression of ERα in MCF7 cells (Fig. 3E and F). These results suggested that miR-148a negatively regulated the expression of ERα at the post-transcriptional level in MCF7 cells.
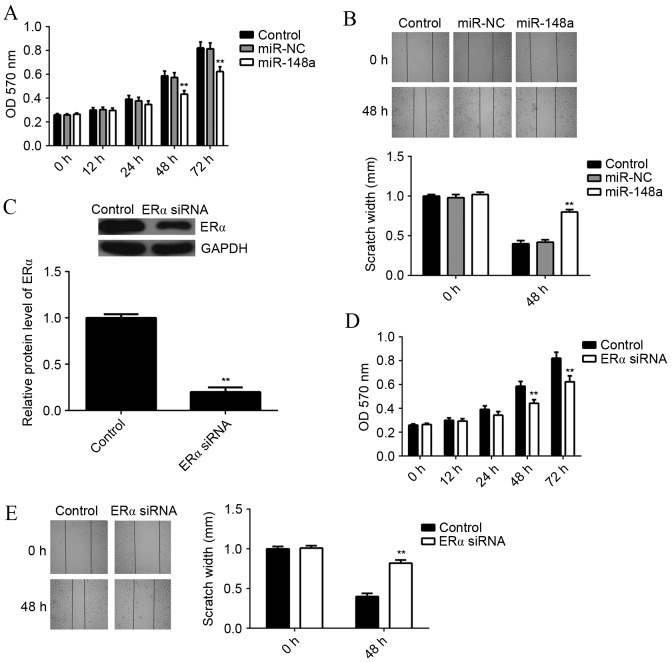
miR-148a overexpression or ERα knockdown inhibits E2-induced MCF7 cell viability and migration
As E2 functions through activation of ERα-mediated signaling, it was examined whether miR-148a could affect E2-induced MCF7 cell viability and migration. MCF7 cells with or without miR-148a overexpression were treated with E2 for 3 h. An MTT assay was then used to examine the cell viability in each group. It was found that the viability rate of miR-148a-overexpressing cells was significantly reduced at 48 and 72 h, as compared with the control group (P<0.01; Fig. 4A). A wound healing assay showed that the scratch width for miR-148a-overexpressing cells was significantly larger at 48 h compared with the control group, indicating that the migration rate of miR-148a-overexpressing cells was significantly reduced (P<0.01; Fig. 4B).
Figure 4.
Effect of miR-148a overexpression or ERα knockdown on E2-induced MCF7 cell viability and migration. MCF7 cells transfected with miR-NC or miR-148a mimic were treated with E2 for 3 h. (A) MTT assay and (B) wound healing assay were used to determine the cell viability and migration, respectively. (C) MCF7 cells were transfected with ERα-specific siRNA, and western blot analysis was used to evaluate the protein expression of ERα. Then, MCF7 cells with or without ERα knockdown were treated with E2 for 3 h. (D) MTT assay and (E) wound healing assay were used to determine the cell viability and migration, respectively. Non-transfected MCF7 cells were used as the control. **P<0.01 vs. control. ERα, estrogen receptor α; E2, estradiol; miR, microRNA; siRNA; small interfering RNA; miR-NC, scrambled miR mimic.
In order to investigate the underlying mechanism of miR-148a further, MCF7 cells were transfected with ERα-specific small interfering RNA (siRNA), which significantly decreased the protein level of ERα as compared with the control (P<0.01; Fig. 4C). MCF7 cells with or without ERα knockdown were treated with E2 for 3 h. An MTT assay showed that the viability of MCF7 cells was significantly decreased after knockdown of ERα for 48 or 72 h, when compared to the control group (P<0.01; Fig. 4D). A wound healing assay showed that the scratch width for MCF7 ERα-knockdown cells was significantly larger at 48 h compared with the control group, indicating that the migration rate of MCF7 cells was significantly decreased after knockdown of ERα (P<0.01; Fig. 4E). These results suggest that both miR-148a overexpression and ERα knockdown result in suppressed E2-induced viability and migration of MCF7 cells.
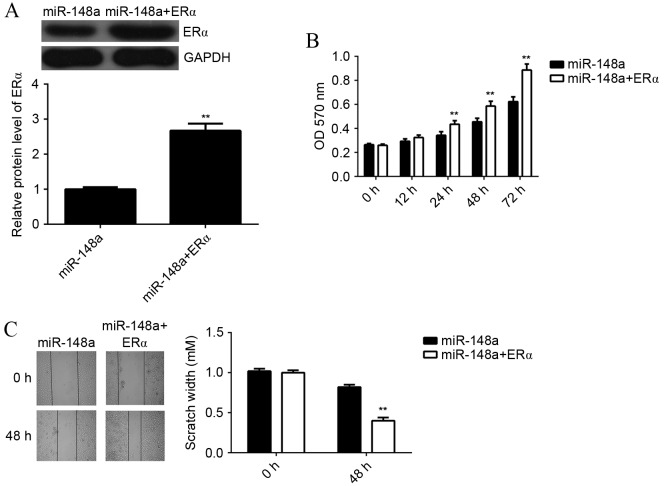
miR-148a inhibits E2-induced MCF7 cell viability and migration via inhibition of ERα expression
In order to investigate whether the effects of miR-148a on E2-induced MCF7 cell viability and migration were through directly targeting ERα, MCF7 cells were co-transfected with miR-148a mimic and ERα ORF plasmid. A western blot analysis showed that the protein level of ERα was significantly higher in cells co-transfected with miR-148a mimic and ERα ORF plasmid, when compared with cells transfected with miR-148a mimic alone (P<0.01; Fig. 5A). This indicated that transfection with ERα ORF plasmid rescued the suppressive effect of miR-148 on the protein expression of ERα in MCF7 cells. Next, MCF7 cells in each group were treated with E2 for 3 h, and MTT and wound healing assays were performed. The viability of MCF7 cells was significantly increased in cells at 24, 48 and 72 h after co-transfection with miR-148a mimic and ERα ORF plasmid, as compared with miR-148a-overexpressing cells without plasmid (P<0.01; Fig. 5B). In a wound healing assay, the scratch width of MCF7 cells at 48 h after co-transfection with miR-148a and ERα ORF plasmid was significantly smaller compared with miR-148a-overexpressing cells without plasmid, indicating that the migration rate of was significantly increased (P<0.01; Fig. 5C). These results suggest that miR-148a inhibits E2-induced MCF7 cell viability and migration via inhibition of ERα expression.
Figure 5.
Effect of miR-148a on E2-induced MCF7 cell viability and migration via inhibition of ERα expression. (A) MCF7 cells were co-transfected with miR-148a mimic and ERα ORF plasmid, and western blot analysis was used to evaluate the protein expression of ERα. Next, MCF7 cells were treated with E2 for 3 h. (B) MTT and (C) wound healing assays were used to determine cell viability and migration, respectively. miR-148a-overexpressing MCF7 cells were used as the control. **P<0.01 vs. miR-148a. ERα, estrogen receptor α; E2, estradiol; miR, microRNA.
E2 treatment decreases the expression of miR-148a in MCF7 cells
The effect of E2 treatment on the expression of miR-148a in MCF7 cells was examined using qPCR. It was found that E2 treatment decreased the miR-148a levels in MCF7 cells in a dose-dependent manner (Fig. 6). A dosage of 1 mM significantly reduced miR-148a expression as compared with the control (P<0.01). Furthermore, a dosage of 10 mM significantly reduced miR-158a expression as compared with a dosage of 1 mM. These results suggest that E2 treatment decreases miR-148a expression, which increases the ERα protein level in MCF7 cells. Through activation of ERα-mediated downstream signaling, E2 treatment induces the viability and migration of breast cancer cells.
Figure 6.
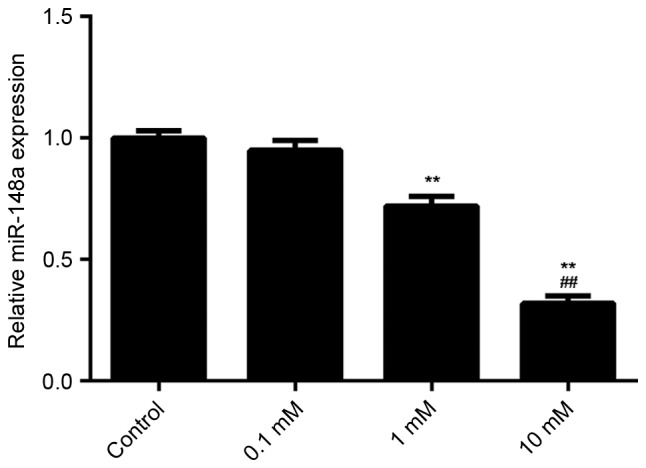
Effect of E2 treatment on the expression of miR-148a in MCF7 cells. (A) Using, qPCR, the expression levels of miR-148a were evaluated in MCF7 cells treated with E2 of different concentrations (0.1, 1 or 10 mM) for 3 h. Non-treated MCF7 cells were used as the control. **P<0.01 vs. control. ##P<0.01 vs. 1 mM. E2, estradiol; miR, microRNA.
Discussion
The present study investigated the function and underlying mechanism of miR-148a in mediating the E2-induced viability and migration of ERα-positive breast cancer MCF7 cells. The results showed that treatment with E2 significantly enhanced the viability and migration of MCF7 cells. miR-148a was found to negatively regulate the protein expression of ERα in MCF7 cells through directly binding to the 3′UTR of ERα mRNA and thus causing translation inhibition. Ectopic expression of miR-148a significantly suppressed the E2-induced viability and migration of MCF7 cells, similar to the effect of ERα knockdown. Furthermore, overexpression of ERα rescued the suppressive effect of miR-148a on E2-induced viability and migration of MCF7 cells. Finally, treatment with E2 was found to suppress miR-148a expression in MCF7 cells in a dose-dependent manner.
ERα, coded by gene ESR1, is a ligand-activated transcription factor composed of several domains important for hormone binding, DNA binding and activation of transcription (24). ERα localizes to the nucleus where it may form a homodimer or a heterodimer with ERβ (25). It has previously been demonstrated that E2 and ERα are essential for sexual development and reproductive function, and are involved in some human cancers such as breast cancer and endometrial cancer (26–28). In the present study, treatment with E2 promoted the viability and migration of ERα-positive breast cancer MCF7 cells. Therefore, the E2/ERα-mediated signaling pathway is a promising target in the treatment of ERα-positive breast cancer. Shang et al demonstrated that baicalein could inhibit E2-induced migration, adhesion and invasion of breast cancer cells via the G-protein-coupled receptor 30 signaling pathway (29).
Furthermore, treatment with E2 has previously been found to cause deregulation of many miRs during the mammary carcinogenesis process (30), suggesting that miRs may play a role in breast cancer. For instance, miR-125b was found to be significantly upregulated in breast cancer, and its upregulation was associated with poor prognosis and aromatase inhibitor resistance (31). miR-200b was reported to be downregulated in breast cancer, and its low expression was correlated with late Tumor, Node, Metastasis stages, negative ER and positive HER-2 statuses, and poor prognosis (32).
miR-148a has been demonstrated to serve a suppressive function in multiple cancer types (33,34). For instance, miR-148a was downregulated in gastric cancer due to hypermethylation in its promoter region (35). Furthermore, miR-148a was found to regulate numerous target genes and pathways involving tumor proliferation, invasion and metastasis (35). It is also significantly downregulated in non-small cell lung cancer (NSCLC) compared to adjacent non-cancerous lung tissues, and its low level is significantly associated with lymph-node metastasis (36). In addition, it can suppress epithelial-to-mesenchymal transition by targeting ROCK1 in NSCLC cells (36). In the present study, ERα was found to be a direct target gene of miR-148a, and its expression was negatively regulated by miR-148a at the post-transcriptional level in MCF7 cells. To further reveal the role of miR-148a in ERα-positive breast cancer, MCF7 cells were transfected with miR-148a mimic to increase its expression level. Overexpression of miR-148a suppressed the E2-induced viability and migration of MCF7 cells. Moreover, siRNA-induced ERα downregulation also inhibited the E2-induced MCF7 cell viability and migration, similar to the effect of miR-148a upregulation. These results suggested that miR-148a affected the E2-induced MCF7 cell viability and migration through inhibiting the protein expression of ERα. To verify this, ERα ORF plasmid was transfected into miR-148a-overexpressing MCF7 cells. The resulting overexpression of ERα reversed the suppressive effect of miR-148a effect on E2-induced MCF7 cell viability and migration. Therefore, ERα has been demonstrated to be involved in the miR-148a-mediated viability and migration of MCF7 cells treated with E2.
In addition, it was found that treatment with E2 decreased the miR-148a levels in MCF7 cells in a dose-dependent manner. This indicated that E2 treatment not only activates the ERα-mediated viability and migration-related signaling in MCF7 cells, but also increases the ERα protein level via inhibition of miR-148a expression.
In conclusion, the present study demonstrates that miR-148a inhibits the E2-induced viability and migration of ERα-positive breast cancer cells, at least partly via inhibition of ERα protein expression. These findings expand the understanding of miR function in breast cancer, and suggest that miR-148a is a promising candidate for the treatment of ERα-positive breast cancer.
Acknowledgements
This study was supported by the National Basic Research Program of China (grant no. +2013CB835100 to Dr Lingjiang Li), the Projects of the Science and Technology Department of Hunan Province (grant no. 2011FJ6043) and the Health Department of Hunan Province (grant no. B2011-017).
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 4.Segovia-Mendoza M, González-Gonzalez ME, Barrera D, Díaz L, García-Becerra R. Efficacy and mechanism of action of the tyrosine kinase inhibitors gefitinib, lapatinib and neratinib in the treatment of HER2-positive breast cancer: Preclinical and clinical evidence. Am J Cancer Res. 2015;5:2531–2561. [PMC free article] [PubMed] [Google Scholar]
- 5.Das Gupta S, Sae-Tan S, Wahler J, So JY, Bak MJ, Cheng LC, Lee MJ, Lin Y, Shih WJ, Shull JD, Safe S, et al. Dietary γ-Tocopherol rich mixture inhibits estrogen-induced mammary tumorigenesis by modulating estrogen metabolism, antioxidant response and PPARγ. Cancer Prev Res (Phila) 2015;8:807–816. doi: 10.1158/1940-6207.CAPR-15-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas C, Gustafsson JA. Estrogen receptor mutations and functional consequences for breast cancer. Trends Endocrinol Metab. 2015;26:467–476. doi: 10.1016/j.tem.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Xu B, Lovre D, Mauvais-Jarvis F. Effect of selective estrogen receptor modulators on metabolic homeostasis. Biochimie. 2016;124:92–97. doi: 10.1016/j.biochi.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Misawa A, Inoue S. Estrogen-related receptors in breast cancer and prostate cancer. Front Endocrinol (Lausanne) 2015;6:83. doi: 10.3389/fendo.2015.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiong R, Patel HK, Gutgesell LM, Zhao J, Delgado-Rivera L, Pham TN, Zhao H, Carlson K, Martin T, Katzenellenbogen JA, et al. Selective human estrogen receptor partial agonists (ShERPAs) for tamoxifen-resistant breast cancer. J Med Chem. 2016;59:219–237. doi: 10.1021/acs.jmedchem.5b01276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: A synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11:1531–1543. [PubMed] [Google Scholar]
- 11.Fan P, Maximov PY, Curpan RF, Abderrahman B, Jordan VC. The molecular, cellular and clinical consequences of targeting the estrogen receptor following estrogen deprivation therapy. Mol Cell Endocrinol. 2015;418:245–263. doi: 10.1016/j.mce.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ambros V. The functions of animal microRNAs. Nature. 2004;431:350–355. doi: 10.1038/nature02871. [DOI] [PubMed] [Google Scholar]
- 13.John B, Enright AJ, Aravin A, Tuschl T, Sander C, Marks DS. Human MicroRNA targets. PLoS Biol. 2004;2:e363. doi: 10.1371/journal.pbio.0020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 15.Boukerroucha M, Josse C, ElGuendi S, Boujemla B, Frères P, Marée R, Wenric S, Segers K, Collignon J, Jerusalem G, Bours V. Evaluation of BRCA1-related molecular features and microRNAs as prognostic factors for triple negative breast cancers. BMC Cancer. 2015;15:755. doi: 10.1186/s12885-015-1740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kehl KL, Shen C, Litton JK, Arun B, Giordano SH. Rates of BRCA1/2 mutation testing among young survivors of breast cancer. Breast Cancer Res Treat. 2016;155:165–173. doi: 10.1007/s10549-015-3658-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu J, Li Q, Xu Q, Liu L, Jiang B. MiR-148a inhibits angiogenesis by targeting ERBB3. J Biomed Res. 2011;25:170–177. doi: 10.1016/S1674-8301(11)60022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aydogdu E, Katchy A, Tsouko E, Lin CY, Haldosén LA, Helguero L, Williams C. MicroRNA-regulated gene networks during mammary cell differentiation are associated with breast cancer. Carcinogenesis. 2012;33:1502–1511. doi: 10.1093/carcin/bgs161. [DOI] [PubMed] [Google Scholar]
- 19.Jiang Q, He M, Ma MT, Wu HZ, Yu ZJ, Guan S, Jiang LY, Wang Y, Zheng DD, Jin F, Wei MJ. MicroRNA-148a inhibits breast cancer migration and invasion by directly targeting WNT-1. Oncol Rep. 2016;35:1425–1432. doi: 10.3892/or.2015.4502. [DOI] [PubMed] [Google Scholar]
- 20.Xue J, Chen Z, Gu X, Zhang Y, Zhang W. MicroRNA-148a inhibits migration of breast cancer cells by targeting MMP-13. Tumour Biol. 2016;37:1581–1590. doi: 10.1007/s13277-015-3926-9. [DOI] [PubMed] [Google Scholar]
- 21.Soltani S, Mokarian F, Panjehpour M. The expression of CK-19 gene in circulating tumor cells of blood samples of metastatic breast cancer women. Res Pharm Sci. 2015;10:485–496. [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwal V, Bell GW, Nam JW, Bartel DP. Predicting effective microRNA target sites in mammalian mRNAs. Elife. 2015;4:e05005. doi: 10.7554/eLife.05005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schröder L, Koch J, Mahner S, Kost BP, Hofmann S, Jeschke U, Haumann J, Schmedt J, Richter DU. The effects of petroselinum crispum on estrogen receptor-positive benign and malignant mammary cells (MCF12A/MCF7) Anticancer Res. 2017;37:95–102. doi: 10.21873/anticanres.11294. [DOI] [PubMed] [Google Scholar]
- 24.Murphy E. Estrogen signaling and cardiovascular disease. Circ Res. 2011;109:687–696. doi: 10.1161/CIRCRESAHA.110.236687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthews J, Gustafsson JA. Estrogen signaling: A subtle balance between ER alpha and ER beta. Mol Interv. 2003;3:281–292. doi: 10.1124/mi.3.5.281. [DOI] [PubMed] [Google Scholar]
- 26.Anbalagan M, Rowan BG. Estrogen receptor alpha phosphorylation and its functional impact in human breast cancer. Mol Cell Endocrinol. 2015;418:264–272. doi: 10.1016/j.mce.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 27.Bondesson M, Hao R, Lin CY, Williams C, Gustafsson JÅ. Estrogen receptor signaling during vertebrate development. Biochim Biophys Acta. 2015;1849:142–151. doi: 10.1016/j.bbagrm.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan S. A review of selective estrogen receptor modulators in the treatment of breast and endometrial cancer. Semin Oncol. 2002;29(3 Suppl 11):S129–S133. doi: 10.1016/S0093-7754(02)70136-X. [DOI] [PubMed] [Google Scholar]
- 29.Shang D, Li Z, Zhu Z, Chen H, Zhao L, Wang X, Chen Y. Baicalein suppresses 17-β-estradiol-induced migration, adhesion and invasion of breast cancer cells via the G protein-coupled receptor 30 signaling pathway. Oncol Rep. 2015;33:2077–2085. doi: 10.3892/or.2015.3786. [DOI] [PubMed] [Google Scholar]
- 30.Munagala R, Aqil F, Vadhanam MV, Gupta RC. MicroRNA ‘signature’ during estrogen-mediated mammary carcinogenesis and its reversal by ellagic acid intervention. Cancer Lett. 2013;339:175–184. doi: 10.1016/j.canlet.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vilquin P, Donini CF, Villedieu M, Grisard E, Corbo L, Bachelot T, Vendrell JA, Cohen PA. MicroRNA-125b upregulation confers aromatase inhibitor resistance and is a novel marker of poor prognosis in breast cancer. Breast Cancer Res. 2015;17:13. doi: 10.1186/s13058-015-0515-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yao Y, Hu J, Shen Z, Yao R, Liu S, Li Y, Cong H, Wang X, Qiu W, Yue L. MiR-200b expression in breast cancer: A prognostic marker and act on cell proliferation and apoptosis by targeting Sp1. J Cell Mol Med. 2015;19:760–769. doi: 10.1111/jcmm.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, Song YX, Wang ZN. The microRNA-148/152 family: Multi-faceted players. Mol Cancer. 2013;12:43. doi: 10.1186/1476-4598-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takahashi M, Cuatrecasas M, Balaguer F, Hur K, Toiyama Y, Castells A, Boland CR, Goel A. The clinical significance of MiR-148a as a predictive biomarker in patients with advanced colorectal cancer. PLoS One. 2012;7:e46684. doi: 10.1371/journal.pone.0046684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xia J, Guo X, Yan J, Deng K. The role of miR-148a in gastric cancer. J Cancer Res Clin Oncol. 2014;140:1451–1456. doi: 10.1007/s00432-014-1649-8. [DOI] [PubMed] [Google Scholar]
- 36.Li J, Song Y, Wang Y, Luo J, Yu W. MicroRNA-148a suppresses epithelial-to-mesenchymal transition by targeting ROCK1 in non-small cell lung cancer cells. Mol Cell Biochem. 2013;380:277–282. doi: 10.1007/s11010-013-1682-y. [DOI] [PubMed] [Google Scholar]