Abstract
Cartilage injury of the knee that is associated with significant subchondral bone loss can result in great morbidity, and treatment options that provide durable repair are limited. Osteochondral autograft and allograft reconstruction of these lesions has been used extensively; however, these techniques often require a more invasive surgical exposure, and restoring the natural articular surface radius of curvature can be challenging, particularly in larger lesions. Cell-based repair of these lesions, using autologous chondrocytes in conjunction with bone grafting, has been used with success, although this procedure requires the patient to undergo 2 operations, and access is often restricted due to the high associated costs. Comparable medium-term clinical outcomes have been shown with scaffold-associated mesenchymal stem cell grafting, and this cell-based procedure may also be performed arthroscopically to minimize patient morbidity. In cases of cartilage injury associated with bone loss, this procedure has great potential to repair osteochondral injury when used in conjunction with bone grafting. We present the one-step arthroscopic technique of biologic inlay osteochondral reconstruction in the knee, using an autologous bone graft and a hyaluronic acid-based scaffold embedded with bone marrow aspirate concentrate, to treat full-thickness cartilage lesions associated with significant subchondral bone loss.
Full-thickness cartilage injury may be associated with significant subchondral bone pathology and deficiency, leading to further challenges when undertaking cartilage restoration procedures of the knee. Numerous techniques of cartilage restoration are currently used, including marrow stimulation, osteochondral grafting, and cell-based techniques such as autologous chondrocyte implantation (ACI) and mesenchymal stem cell repair procedures. Unfortunately, in cases of combined cartilage injury and subchondral bone loss, lesions may not be amenable to treatment by conventional repair techniques.
ACI has been shown to provide durable cartilage repair, and may also be used in conjunction with bone grafting to reconstitute subchondral bone deficiency. In cases of subchondral bone loss greater than approximately 8 mm, a “sandwich” type ACI procedure may be used to reconstruct osteochondral lesions. Originally described by Peterson,1 this technique uses bone grafting in association with autologous chondrocytes contained between the layered periosteal graft. This technique has since been modified by Bartlett et al.,2 using a matrix-assisted chondrocyte implantation technique in conjunction with bone grafting. Unfortunately, the use of cell-based cartilage repair techniques using autologous chondrocytes may be limited by cost, as this is a 2-stage procedure that requires expansion of chondrocyte cell lines off-site.
Single-stage, cell-based cartilage repair techniques using mesenchymal stem cells sourced from bone marrow aspirate concentrate (BMAC) have been developed that provide comparable durability of repair to ACI techniques, at significantly reduced cost and operative time.3, 4 Cartilage repair using implantation of a hyaluronic acid-based scaffold embedded with activated bone marrow aspirate concentrate (HA-BMAC) has shown durable cartilage restoration at medium-term follow-up, with preferential formation of hyaline-like repair tissue.5 This technique has provided good to excellent clinical outcomes in a wide range of lesion sizes within the knee, including multicompartment lesions more than 20 cm2 in size.6
Minimally invasive techniques of cartilage repair are favored due to the lessened morbidity of surgery and the reduced postoperative recovery period. Arthroscopic cartilage restoration using an HA-BAMC has been described previously, and is used regularly by our institutions.7 In cases of significant subchondral bone loss, this technique of cartilage repair may be used arthroscopically in conjunction with bone grafting to reconstruct a wide variety of osteochondral lesion types. We present the one-step arthroscopic technique of biologic inlay osteochondral reconstruction (BIOR) in the knee, using an HA-BMAC and autologous bone graft inlay, to treat full-thickness cartilage lesions associated with significant subchondral bone loss (Video 1).
Surgical Technique
Patient Positioning and Arthroscopic Preparation of Cartilage Defect
The patient is positioned supine in a typical manner for knee arthroscopy, and the operative knee is appropriately exposed. The ipsilateral iliac crest is prepared in anticipation of bone marrow aspiration, and the planned site of autologous bone graft harvest is also exposed. We prefer the ipsilateral proximal tibia as the site for bone graft harvest, with the exception of cases that require a larger volume of graft, where the ipsilateral iliac crest may be used. Preoperative magnetic resonance imaging is routinely performed to measure the size of the osteochondral lesion and to estimate the required volume of the bone graft inlay (Fig 1 B and C). The patient is typically given a general anesthetic. An examination of the knee under anesthesia is performed, and concurrent treatment of associated pathology may proceed as indicated. Treatment of bony malalignment and restoration of knee stability will provide the optimal environment for cartilage repair tissue to mature and remodel.
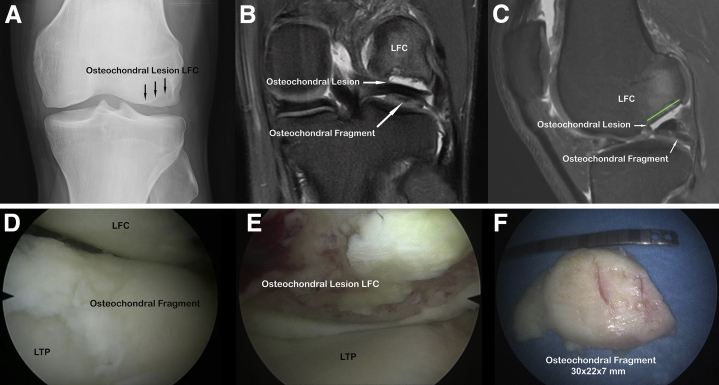
Fig 1.
Plain anteroposterior radiograph (A), and coronal (B) and sagittal (C) magnetic resonance imaging slices (Proton Density Fat Saturation, 3.0 tesla scanner) of a left knee depicting an osteochondral lesion of the lateral femoral condyle and adjacent loose osteochondral fragment. (D-F) Patient supine, arthroscopic view of a left knee lateral compartment visualized via the anteromedial portal. (D) Loose osteochondral fragment overlying the lateral tibial plateau (LTP), (E) osteochondral defect of the lateral femoral condyle (LFC), and (F) loose osteochondral fragment removed from the lateral compartment.
A diagnostic arthroscopy of all knee compartments is performed to locate sites of osteochondral injury, and to completely delineate the cartilage defect dimensions (Fig 1 D and E). A thorough assessment is necessary to ensure visualization of the entire defect to confirm the appropriateness of arthroscopic treatment. Loose osteochondral fragments should be identified and removed (Fig 1F). Comfortable access to the relevant knee compartment may be improved by strategic placement of retraction instruments to manipulate adjacent joint capsule and synovium (Arthroscopic Retracting System, ATMED-Z, Rafalski, Katowice, Poland).8 Preparation of the cartilage defect begins with excision of all unstable chondral flaps. The defect periphery should be debrided back to a stable, vertical wall of cartilage that is perpendicular to the natural contour of the subchondral plate. A prepared defect that is well contained circumferentially is preferred, as this provides a more favorable environment for cartilage repair tissue to mature. Specialized arthroscopic instruments are often used at our institution to achieve consistent perpendicularity of the cartilage wall surrounding the defect (Chondrectomes Set, ATMED-Z; Fig 2A). The condition of subchondral bone at the base of the defect should be examined in detail to identify bony deficiency that will be amenable to application of a bone graft inlay to restore the natural radius of curvature of the subchondral articular surface. Any calcified cartilage located within the base of the defect should be removed, and areas of planned bone grafting should be debrided back to healthy bone (Fig 2B). The surface area of the defect should be assessed using an arthroscopic measuring device or a template to accurately size-match the HA-BMAC graft.
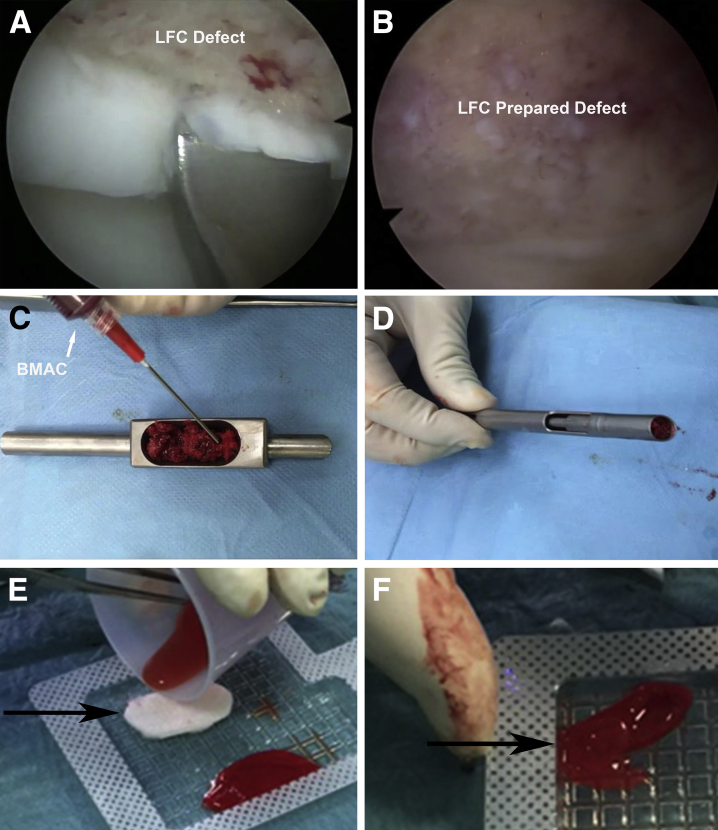
Fig 2.
(A, B) Patient supine, arthroscopic view of a left knee lateral compartment visualized via the anteromedial portal. (A) Curettage of the lateral femoral condyle (LFC) osteochondral lesion to create a contained defect surrounded by the vertical walls of the cartilage, (B) prepared osteochondral lesion within the LFC, (C) cancellous autologous bone graft harvested from the ipsilateral proximal tibia inserted into the box compartment of the applicator and combined with several drops of bone marrow aspirate concentrate (BMAC) and fibrin glue, (D) prepared bone graft compressed into the 10-mm barrel of the applicator tool, (E) hyaluronic acid-based scaffold (arrow) processed to size-match cartilage defect, and (F) creation of a hyaluronic acid-based scaffold embedded with activated bone marrow aspirate concentrate (HA-BMAC) graft by the application of BMAC to the hyaluronic acid-based scaffold (arrow).
HA-BMAC and Bone Graft Inlay Preparation
After estimating the volume of the required bone graft, autologous cancellous bone harvest should proceed from either the ipsilateral proximal tibia or iliac crest. Bone marrow is aspirated from the ipsilateral iliac crest and a commercially available system is used to prepare the BMAC (Angel, Cytomedix., Gaithersberg, MD). The morselized bone chips are inserted into the box chamber of the graft applicator tool. Several drops of BMAC and fibrin glue are added to the bone chips (Fig 2C) and the graft is compressed into the 10-mm-diameter barrel of the applicator (Fig 2D). In the absence of such a bone inlay applicator, the bone chips may simply be mixed in a dish and later applied to the defect using an arthroscopic paddle or spoon via a valveless cannula.
The 3-dimensional hyaluronic acid-based scaffold (Hyalofast, Anika Therapeutics, Srl, Abano Terme, Italy) is appropriately size-matched to the defect dimensions (Fig 2E). To more easily contain the BMAC and apply it to the scaffold, the BMAC may be clot-activated using batroxobin (Plateltex Act, Plateltex SRO, Bratislava, Slovakia) or autologous thrombin. The surgeon may choose to use the BMAC without activation in cases of arthroscopic treatment. The malleable HA-BMAC graft is created by combining the BMAC with the hyaluronic acid-based scaffold (Fig 2F).
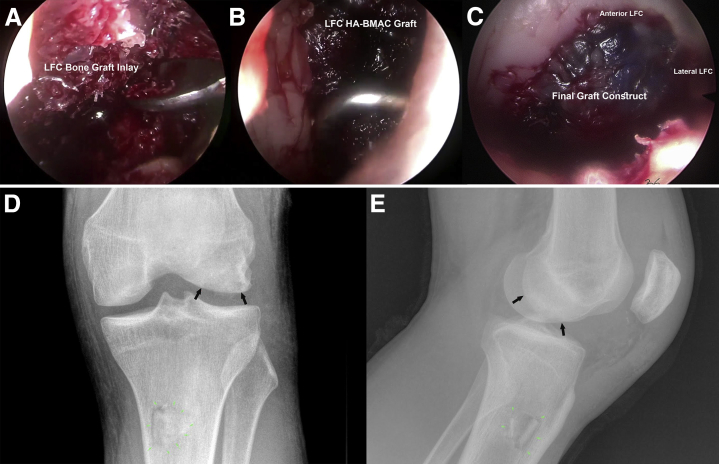
Dry Arthroscopic BIOR Procedure
Drain the arthroscopic fluid from the knee and re-evaluate the prepared osteochondral defect to confirm complete visualization. Apply the prepared bone graft to the base of the defect using the specialized applicator, or a preferred chosen arthroscopic instrument. Reconstitute bony deficiency at the base of the defect with the bone graft inlay, using an arthroscopic paddle to contour and compress the graft (Fig 3A). Recreation of the natural radius of curvature of the articular surface is a priority. Using a grasper or nontoothed forceps, insert the HA-BMAC into the appropriate knee compartment via a valveless cannula or skid, and place the graft into the repair site. Press-fit the graft securely within the defect, and re-examine the contour of the dual-layer repair structure circumferentially to ensure that the expected radius of curvature has been achieved. Under arthroscopic visualization, gently cycle the knee repeatedly to confirm secure seating of the BIOR construct. Fibrin glue may be added to the graft to provide greater security.9 Close all surgical wounds and apply sterile dressings. The operative knee is immobilized in a brace set to correspond to the articular tibiofemoral contact angle (typically 40° of flexion) after the repair of osteochondral lesions within the medial or lateral compartments. The advantages/limitations and the pearls/pitfalls of this surgical procedure are summarized in Tables 1 and 2, respectively.
Fig 3.
(A-C) Patient supine, arthroscopic view of a left knee lateral compartment visualized via the anteromedial portal. (A) Bone graft inlay placed within the osteochondral defect of a lateral femoral condyle (LFC) and contoured with the arthroscopic paddle, (B) hyaluronic acid-based scaffold embedded with activated bone marrow aspirate concentrate (HA-BMAC) graft positioned and press-fit within the osteochondral defect of the LFC, and (C) final position of biologic inlay osteochondral reconstruction (BIOR) construct after the application of fibrin glue about the periphery. Anteroposterior (D) and lateral (E) radiographs of the left knee performed 7 weeks postoperatively showing medial/lateral and anterior/posterior boundaries of repair tissue (black arrows) within the LFC.
Table 1.
Advantages and Limitations of Biologic Inlay Osteochondral Reconstruction
| Advantages | One-stage cartilage repair that is capable of addressing subchondral bone deficiency |
| Arthroscopic technique provides magnification that enables detailed visualization of the defect and implantation procedure | |
| Osteochondral defect is repaired without removing adjacent healthy tissue, as opposed to osteochondral transfer procedures that remove healthy cartilage and subchondral bone | |
| HA-BMAC has been shown to provide durable cartilage restoration that is superior to standard techniques such as marrow stimulation | |
| Minimally invasive approach that is low morbidity and encourages early recovery and rehabilitation | |
| Favorable cost profile compared with other cell-based procedures of osteochondral repair such as autologous chondrocyte implantation with bone grafting | |
| Limitations | Surgical time in cases of multiple compartment cartilage lesions may be reduced with an open technique |
| Arthroscopic technique may not provide optimal visualization for larger osteochondral lesions | |
| Long-term clinical outcome data for HA-BMAC used in conjunction with bone grafting are not yet available |
HA-BMAC, hyaluronic acid-based scaffold embedded with activated bone marrow aspirate concentrate.
Table 2.
Pearls and Pitfalls of Biologic Inlay Osteochondral Reconstruction
| Pearls | Use preoperative imaging and arthroscopic visualization to carefully assess dimensions of subchondral bone deficiency, and match bony inlay accordingly. |
| Ensure comfortable visualization of the entire osteochondral defect and use preferred traction techniques as needed to maximize the working space. | |
| The hyaluronic acid-based scaffold composition is symmetrical; the HA-BMAC graft may be placed into the cartilage defect with either side adjacent to the bony inlay. | |
| Pitfalls | Arthroscopic cartilage restoration techniques should be used only in appropriate cases where the complete osteochondral defect can be appreciated; otherwise an open technique is preferable. |
| Confirm secure seating of the HA-BMAC inlay construct within the osteochondral defect by cycling the knee under arthroscopic visualization to minimize the risk of postoperative implant displacement. |
HA-BMAC, hyaluronic acid-based scaffold embedded with activated bone marrow aspirate concentrate.
Step-by-Step Technique Summary
-
1.
Place the patient in the supine position, and expose the ipsilateral iliac crest and site of bone graft harvest (e.g., proximal tibia) in addition to the operative knee.
-
2.
Examine the operative knee under anesthesia, and prepare for treatment of associated pathology as indicated.
-
3.
Perform diagnostic arthroscopy, ensure complete visualization of cartilage lesion and affected subchondral bone, and confirm that arthroscopic treatment is appropriate.
-
4.
Treat associated pathology or perform corrective osteotomy as indicated.
-
5.
Debride cartilage lesion, remove loose cartilaginous tissue, and prepare defect periphery to obtain a well-shouldered, contained defect.
-
6.
Prepare the base of the defect, remove any layers of calcified cartilage, assess subchondral bone involvement, and debride the base to expose healthy bone at the sites of the planned inlay.
-
7.
Measure the prepared cartilage defect and record dimensions for size-matching of the hyaluronic acid-based scaffold.
-
8.
Aspirate bone marrow from the iliac crest and harvest autologous cancellous bone from the planned site.
-
9.
Prepare BMAC using the chosen commercially available system.
-
10.
On a back table, prepare an autologous bone graft by placing chips into the box compartment of the applicator and add several drops of BMAC and fibrin glue.
-
11.
Load the prepared bone graft into the 10-mm barrel of the applicator, or place into a dish if the specialized applicator is not used.
-
12.
Create a size-matched hyaluronic acid-based scaffold appropriate for cartilage defect.
-
13.
Use batroxobin to activate BMAC and combine with the scaffold to create an HA-BMAC implant. The surgeon may elect to use BMAC that has not been clot-activated.
-
14.
Remove the remaining fluid from the joint space and confirm complete visualization of the prepared osteochondral defect under dry arthroscopy.
-
15.
Apply the bone graft to the base of the cartilage defect and create a bony inlay that reconstitutes the bone deficit, matching the natural radius of curvature of the subchondral surface.
-
16.
Insert the HA-BMAC implant into the joint space, use a grasper or nontoothed forceps to place the graft into the cartilage defect and press fit securely.
-
17.
Fibrin glue may be applied to the periphery of the graft to further secure the implant.
-
18.
Gently cycle the knee while visualizing the graft to ensure stability of the construct.
-
19.
Close the surgical wounds, apply sterile dressing, and immobilize the operative knee in a brace set to 40° of flexion to maintain the shape of the graft until fibrous consolidation.
Postoperative Rehabilitation
Postoperatively, the patient is placed into a cast or knee brace, locked into a position corresponding to the articular tibiofemoral contact angle of the repaired osteochondral lesion for a period of 5 to 7 days. Initially, the patient is non-weight bearing and ambulates with crutches. For the second postoperative week, the patient is immobilized in full extension and passively mobilized through a range of motion 4 times daily for 15-minute periods, preferably with external manual traction. Beginning postoperative week 3, partial weight bearing with crutches is allowed, and passive mobilization progresses, without external traction. Continuous passive motion may be used as much as tolerated by the patient. Between weeks 3 and 6, active motion is encouraged 5 times per day, without weight bearing. The patient may wean off crutches to full weight bearing 7 to 8 weeks postoperatively. At 9 to 10 weeks, the focus of rehabilitation is to restore normal gait. Progression to straight line running is encouraged after 3 months, with an emphasis on strength, endurance, and aerobic training. Sport-specific training will typically commence at 8 months postoperatively, with anticipated return to competition by 10 months.
Discussion
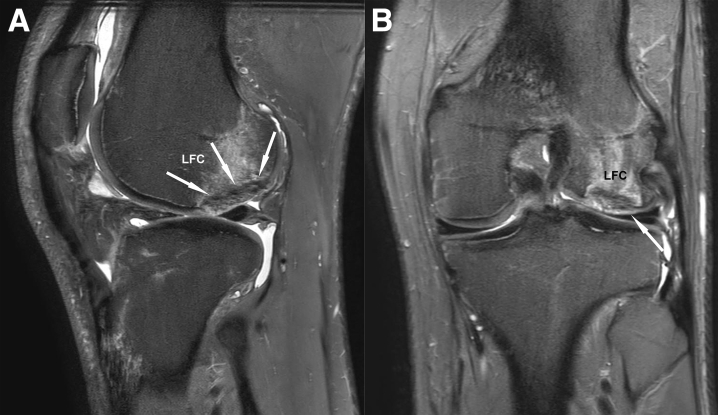
The treatment of cartilage injury associated with significant subchondral bone loss with the arthroscopic BIOR technique enables reconstruction of damaged osteochondral tissue, while providing a method to restore the natural anatomic contour of the articular surface, in a minimally invasive fashion (Fig 4). The one-step cell-based cartilage technique of HA-BMAC has been used at our institutions with success using both open and arthroscopic methods to treat cartilage defects of varying dimensions, and in cases of multicompartmental knee cartilage injury. The arthroscopic BIOR technique combines HA-BMAC cartilage repair with a malleable bony inlay to provide a bilayer autologous reconstruction of the osteochondral unit, with minimal morbidity.
Fig 4.
Magnetic resonance imaging (MRI) of a left knee (Proton Density Fat Saturation, 3.0 tesla scanner) 3 months after the biologic inlay osteochondral reconstruction procedure to treat cartilage injury of a lateral femoral condyle (LFC) associated with significant subchondral bone loss. (A) Sagittal MRI slice depicting integration of the bony inlay into the surrounding bone (arrows). (B) Coronal MRI slice depicting restoration of the articular cartilage, contoured to accurately re-establish the anatomic radius of curvature (arrow).
With respect to osteochondral injuries within the knee joint, autologous osteochondral transfers or osteochondral allograft transplantation is a well-accepted method of repair for a wide range of cartilage lesion size and depth of bony deficiency. Although osteochondral transfers within the knee may be performed arthroscopically, this repair technique is limited to lesions of 3 to 4 cm2, and there may be donor site morbidity, particularly in cases of autologous mosaicplasty. In cases of larger osteochondral lesions, osteochondral allograft transplantation is capable of repairing the damaged osteochondral unit; however, this is typically performed in an open fashion due to technique limitations. A further limitation of these techniques is the required use of one or more circular grafts of any given diameter, necessitating the removal of healthy cartilage and subchondral bone in the case of noncircular or irregular osteochondral lesions. In addition, there may not be full integration of the osteochondral block within the adjacent native bone and cartilage, potentially leading to procedure failure.10 Reconstitution of the anatomic contour of the articular surface may also be problematic with osteochondral transfer or transplantation procedures, particularly if a mosaicplasty technique is employed.
Considering the available methods to treat cartilage injury, ACI has shown durable clinical results, and the use of autologous chondrocytes in conjunction with bone grafting can be used to repair osteochondral lesions of varying depths and sizes. Unfortunately, the widespread use of techniques involving 2-stage ACI is doubtful, due to the cost-prohibitive nature of the procedure and the necessity to expose the patient to an additional surgery. Cell-based cartilage repair using biologic scaffolds in conjunction with BMAC has shown comparable medium-term clinical outcomes to ACI, and has the benefit of being a single-stage procedure that is less resource intensive.3, 6
It should be noted that although good to excellent medium-term outcomes have been shown with the use of HA-BMAC to treat cartilage injury within the knee, a similar outcome analysis is not yet available for the use of this technique in conjunction with a bony inlay to reconstitute subchondral bone loss. With regard to the choice of scaffold, a type I/III collagen graft, or similar material, may be used in place of the hyaluronic acid-based scaffold. In our experience, the hyaluronic acid-based scaffold is preferred for arthroscopic use, due to the malleable and adherent nature of the HA-BMAC graft, allowing precise manipulation and placement of the graft within the cartilage defect.
The BIOR technique of osteochondral repair has the capability to treat a wide range of lesion sizes, with varying depths of subchondral bone loss. In addition, lesions of irregular shape may be repaired without sacrificing healthy adjacent tissue, as opposed to reconstruction procedures that involve circular-shaped osteochondral grafting. Furthermore, although osteochondral autograft or allograft procedures require graft implantation from a near-90° approach, the BIOR technique may be used to restore the natural anatomic radius of curvature of articular surfaces from a wide variety of angles. This single-stage, dual-layer, cell-based cartilage repair procedure with a bony inlay is a versatile technique that has an attractive cost profile, and may be used in a minimally invasive fashion for a variety of joint cartilage injuries that involve subchondral bone deficiency.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Preparation of a bone graft inlay and a hyaluronic acid-based scaffold with bone marrow aspirate concentrate, and demonstration of the arthroscopic biologic inlay osteochondral reconstruction procedure to repair a large cartilage lesion with associated subchondral bone deficiency of the lateral femoral condyle in a left knee. Patient supine, arthroscopic view of the lateral compartment via the anteromedial portal, and instrumentation via the anterolateral portal.
References
- 1.Peterson L. Chondrocyte transplantation. In: Jackson D.W., editor. Master techniques in orthopaedic surgery: Reconstructive knee surgery. Lippincott, Williams & Wilkins; Philadelphia: 2003. pp. 353–373. [Google Scholar]
- 2.Bartlett W., Gooding C.R., Carrington R.W.J., Skinner J.A., Briggs T.W.R., Bentley G. Autologous chondrocyte implantation at the knee using a bilayer collagen membrane with bone graft. A preliminary report. J Bone Joint Surg Br. 2005;87:330–332. doi: 10.1302/0301-620x.87b3.15552. [DOI] [PubMed] [Google Scholar]
- 3.Gobbi A., Chaurasia S., Karnatzikos G., Nakamura N. Matrix-induced autologous chondrocyte implantation versus multipotent stem cells for the treatment of large patellofemoral chondral lesions: A nonrandomized prospective trial. Cartilage. 2015;6:82–97. doi: 10.1177/1947603514563597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gobbi A., Karnatzikos G., Sankineani S.R. One-step surgery with multipotent stem cells for the treatment of large full-thickness chondral defects of the knee. Am J Sports Med. 2014;42:648–657. doi: 10.1177/0363546513518007. [DOI] [PubMed] [Google Scholar]
- 5.Gobbi A, Scotti C, Karnatzikos G, Mudhigere A, Castro M, Peretti GM. One-step surgery with multipotent stem cells and hyaluronan-based scaffold for the treatment of full-thickness chondral defects of the knee in patients older than 45 years [published online January 14, 2016]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-3984-6. [DOI] [PMC free article] [PubMed]
- 6.Gobbi A., Whyte G.P. One-stage cartilage repair using a hyaluronic acid-based scaffold with activated bone marrow-derived mesenchymal stem cells compared with microfracture: Five-year follow-up. Am J Sports Med. 2016;44:2846–2854. doi: 10.1177/0363546516656179. [DOI] [PubMed] [Google Scholar]
- 7.Whyte G.P., Gobbi A., Sadlik B. Dry arthroscopic single-stage cartilage repair of the knee using a hyaluronic acid-based scaffold with activated bone marrow-derived mesenchymal stem cells (HA-BMAC) Arthrosc Tech. 2016;5:e913–e918. doi: 10.1016/j.eats.2016.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadlik B., Wiewiorski M. Dry arthroscopy with a retraction system for matrix-aided cartilage repair of patellar lesions. Arthrosc Tech. 2014;3:e141–e144. doi: 10.1016/j.eats.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whyte G.P., McGee A., Jazrawi L., Meislin R. Comparison of collagen graft fixation methods in the porcine knee: Implications for matrix-assisted chondrocyte implantation and second-generation autologous chondrocyte implantation. Arthroscopy. 2016;32:820–827. doi: 10.1016/j.arthro.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Williams R.J., Ranawat A.S., Potter H.G., Carter T., Warren R.F. Fresh stored allografts for the treatment of osteochondral defects of the knee. J Bone Joint Surg Am. 2007;89:718–726. doi: 10.2106/JBJS.F.00625. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preparation of a bone graft inlay and a hyaluronic acid-based scaffold with bone marrow aspirate concentrate, and demonstration of the arthroscopic biologic inlay osteochondral reconstruction procedure to repair a large cartilage lesion with associated subchondral bone deficiency of the lateral femoral condyle in a left knee. Patient supine, arthroscopic view of the lateral compartment via the anteromedial portal, and instrumentation via the anterolateral portal.