Abstract.
Blue intratissue refractive index shaping (blue-IRIS) is a method with potential to correct ocular refraction noninvasively in humans. To date, blue-IRIS has only ever been applied to cat corneas and hydrogels. To test the comparability of refractive index change achievable in cat and human tissues, we used blue-IRIS to write identical phase gratings in ex vivo feline and human corneas. Femtosecond pulses (400 nm) were focused below the epithelial surface of excised cat and human corneas and scanned to write phase gratings with lines wide, spaced apart, using a scan speed of . Additional cat corneas were used to test writing at 3 and in order to document speed dependence of the refractive index change magnitude. The first-order diffraction efficiency was immediately measured and used to calculate the refractive index change attained. Our data show that blue-IRIS induces comparable refractive index changes in feline and human corneas, an essential requirement for further developing its use as a clinical vision correction technique.
Keywords: femtosecond, refractive, stroma, cornea
1. Introduction
Laser refractive surgeries, including laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK), correct visual refractive errors by the ablation of corneal tissue, usually in the corneal stroma. Photoablation of the stromal bed is typically accomplished via a single-photon absorption mechanism at 193 nm.1–3 This process modifies the cornea’s refractive and biomechanical properties and induces additional optical power in the cornea by changing the shape of its anterior surface. However, complications, such as dry eye,4 stromal haze,5 diffuse lamellar keratitis,6 or inflammation7 can occur from stromal photoablation, epithelial debridement, and/or the creation of the epithelial flap.
We have shown that the power of a refractive optical element, such as the cornea, can also be modified by inducing refractive index (RI) changes within the element, while the surface shape remains unaltered. In 2010, building on previous work with infrared pulses,8–10 we first reported writing diffractive phase patterns in ex vivo feline corneas using 400-nm femtosecond (fs)-pulsed laser light.11 In 2014, we demonstrated the ability to write phase structures in cat corneas in vivo and verified that the intended wavefront aberration changes were achieved in a living eye using RI modifications.12 Importantly, the attained wavefront aberration changes remained stable for up to 12 months.12
Blue intratissue refractive index shaping (blue-IRIS) works by tightly focusing 400 nm, fs laser pulses into the corneal stroma; it takes advantage of the intrinsic two-photon absorption of the cornea to alter its RI in the focal volume of the laser. Importantly, blue-IRIS works below the ablation threshold of corneal tissue.8,12 As a result, unlike PRK or LASIK, it does not appear to damage the epithelium, endothelium, or even the stroma outside the focal zone. A preliminary study of blue-IRIS with terminal deoxynucleotidyl transferase-mediated dUTP-digoxigenin nick end labeling staining has shown that apoptosis is largely restricted to the stromal laser focal region,13 suggesting that blue-IRIS may produce a smaller or no wound healing response compared to LASIK or PRK.
Many feline corneal properties, such as thickness of the stroma and epithelium, cellular and structural organization, and molecular composition, are approximate that of humans, making it a suitable model for refractive vision correction studies despite not being identical to human corneal tissue.14–16 However, before we can begin testing blue-IRIS as a method for correcting refractive error in humans, we must first verify that it can alter the RI of human corneal stroma. In this proof-of-concept study, blue-IRIS was used to write identical phase gratings in excised, living feline, and human corneal tissues using a scanning speed of . This allowed us to determine if the blue-IRIS process could be successfully performed in human corneal tissue, and to compare the amount of phase change achieved in feline and human corneas directly. The present study is a critical step toward establishing the potential of blue-IRIS as a new method of laser refractive vision correction.
2. Methods
2.1. Sample Preparation
Eighteen-enucleated feline eye globes (Liberty Research, Inc., Waverly, New York) were placed in Optisol-GS (Bausch & Lomb, Inc., Rochester, New York) immediately postmortem and shipped overnight on ice to keep the corneas alive until the experiment was performed. Optisol-GS is a commercially available storage medium widely used to keep human corneal tissue destined for transplantation alive for up to 14 days.17 Once received on site for the experiment, feline corneas were surgically removed from each globe by cutting around the limbal edge, creating a 1-cm-diameter corneal button. All animal procedures were conducted in accordance with the guidelines from the University of Rochester Committee on Animal Research, the ARVO statement for the Use of Animals in Ophthalmic and Vision Research, and the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Four excised human corneas were received postmortem from the Lions Eye Bank at Rochester (Rochester, New York), a satellite of Lions Eye Bank Albany (Albany, New York). Just like cat corneas, human corneas were preserved in Optisol-GS and delivered on ice after being deemed unsuitable for transplantation. The postmortem time varied from 2 to 6 days before delivery. Upon arrival, all human corneal samples were visibly yellowed and cloudy. The three human donors were ages 46, 59, and 69, and the causes of death were melanoma, metastatic brain cancer, and pancreatic cancer, respectively. The donor with melanoma also had reduced stromal and endothelial cell counts due to guttate.
Both human and feline corneas were handled, prepared, and treated identically. Excised central, full-thickness corneal buttons of diameter were placed endothelial side down on a glass slide, such that the laser pulses were focused into the stroma from the anterior surface, as they would be when blue-IRIS would be performed in vivo. A small amount of Optisol-GS was added to the slide to prevent dehydration, which would decrease transparency and may affect the RI change. A #1 glass coverslip was placed over the corneal tissue to keep it flat and prevent solution evaporation. Mylar spacers were used to ensure minimal tilt on the coverslip surface and even applanation across the entire cornea.
2.2. Blue-IRIS Procedure
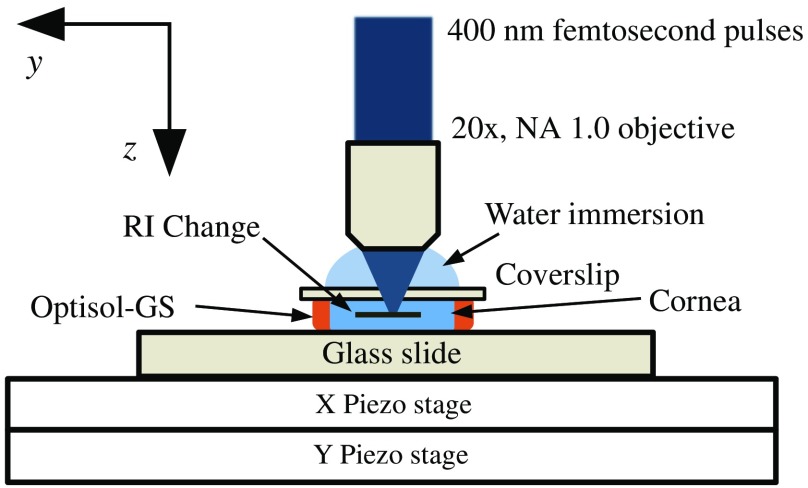
The present experiments were performed with a system that included a mode-locked femtosecond Ti:Sapphire oscillator (Vitesse; Coherent Corporation, Santa Clara, California), which emitted 800 nm, 100 fs pulses at 80 MHz. The average output power at 800 nm was . Second harmonic generation was used to frequency double the 800-nm beam, producing up to 250 mW of 400-nm light. An adjustable, metallic neutral density filter was used to attenuate the average power in the focal region to , which corresponded to pulse energies of . As shown in Fig. 1, the 400-nm pulses were tightly focused through a high numerical aperture (), water immersion objective (, W Plan-Apochromat; Carl Zeiss, Jena, Germany) into the midstromal region of the cornea, below the surface of the epithelium (normal feline and human corneal thicknesses are similar, averaging between 500 and ).14,15
Fig. 1.
Schematic of the blue-IRIS experimental setup. Pulses of 800 nm, 100 fs from a Ti:Sapphire laser were frequency doubled to produce 400 nm, 100 fs pulses using second harmonic generation. These pulses were then tightly focused through a , water immersion objective into the stromal region of an excised corneal sample mounted on a glass slide, bathed in a storage medium (Optisol-GS, Bausch & Lomb), and applanated with a #1 coverslip. The whole assembly was placed on a three-dimensional scanning platform. The piezostages were used to inscribe the IRIS phase grating pattern by raster scanning the sample under the microscope objective. The scan speed (3, 5, for feline tissue and for human tissue) describes the speed of the -axis piezo stage.
Samples were mounted on glass slides as described above and placed on a three-axis motion stage consisting of two piezo stages (M-663, Physik Instrumente, Auburn, Massachusetts) for fine motion control, and three linear servo stages (VP-25XA, Newport, Mountain View, California) for large-scale motion to position the sample under the objective. Phase gratings were inscribed by raster scanning the sample underneath the focusing microscope objective to create lines of phase change. Grating lines were written along the -axis; thus, the scan speed describes the velocity of the -axis piezo stage. All phase gratings covered a area and had a center-to-center line spacing of . Scan speed was set to for human tissue while feline corneas were inscribed with phase gratings written at 3, 5, and to study the effect of scan speed on RI change.
2.3. Refractive Index Measurement
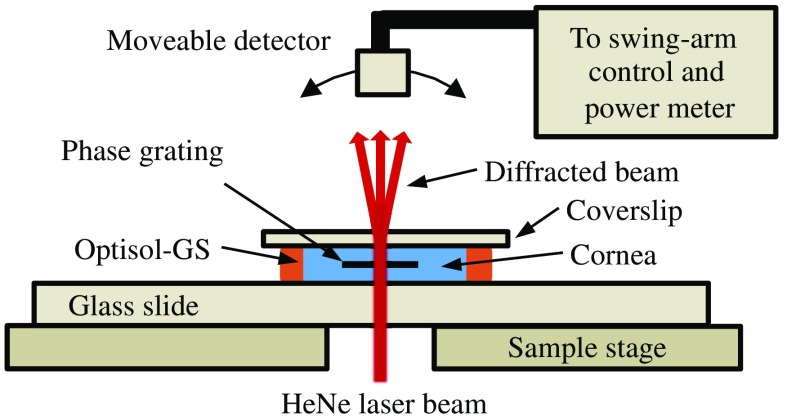
Immediately after the blue-IRIS procedure, the samples were transferred to a custom-built diffractometer with a He–Ne laser source (Fig. 2). A power meter measured the intensity distribution of the diffraction patterns obtained by sending the beam through the sample’s grating.
Fig. 2.
Schematic of custom diffractometer used to measure RI change attained with blue-IRIS. A He-Ne laser beam was incident upon the blue-IRIS phase gratings, causing the beam to diffract. A power detector was mounted to a swing-arm, and measured the diffraction pattern over a hemisphere ranging from to , taking measurements at 0.125 deg intervals. Higher diffraction orders were seen, but RI change was calculated by assessing the first-order diffraction efficiency. The diffraction pattern was measured at three separate locations in each phase grating to account for small variations in intrinsic corneal background scatter.
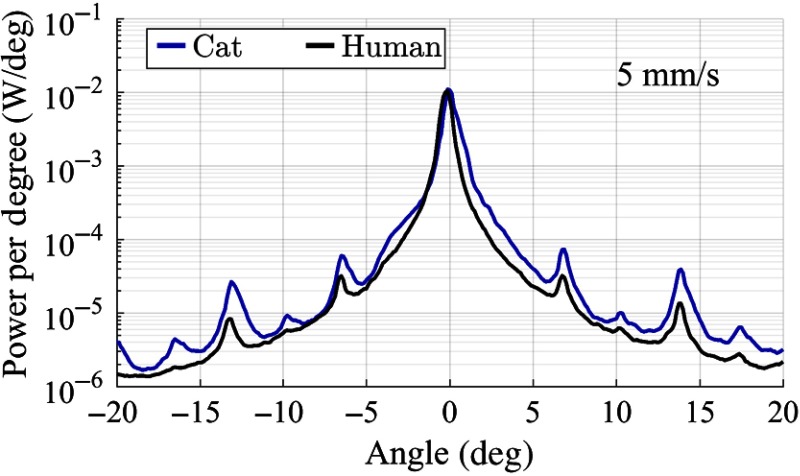
Diffraction patterns (Fig. 3) were measured in three separate places in each blue-IRIS phase grating, as well as in untreated tissues, to account for small variations across and between samples. Due to the size of the phase gratings () and the size of the He–Ne beam used to measure the diffraction efficiency ( to 1.5 mm) only three nonoverlapping measurements could be taken within a sample while avoiding edge effects from the borders of the phase grating. From measurements inside the gratings, the first-order diffraction efficiency was obtained and was then used to calculate the RI change, as previously described.18
Fig. 3.
Diffraction patterns used to calculate RI change in cornea. The power meter used in the custom diffractometer (Fig. 2) scans across a hemisphere ranging from to , collecting the power at 0.125 deg intervals. As well as the diffraction pattern from the blue-IRIS phase gratings, the scans also collect the intrinsic corneal scatter. This background scatter can clearly be seen in the figure as the wide central peak. The first-order diffraction efficiency is used to calculate RI change. A higher diffraction efficiency indicates a higher magnitude of RI change.
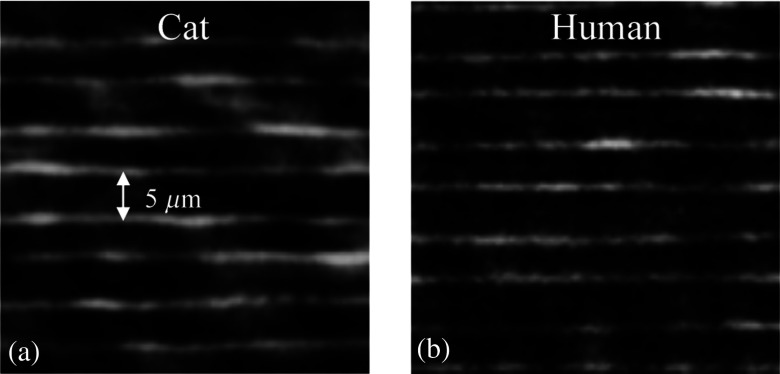
It should be noted that this method was developed using hydrogel polymers and did not originally account for the normal, intrinsic background scatter of corneal tissue. The quality of the lines was also visually assessed by examining the samples with a differential interference contrast (DIC) microscope; the lines of RI change were clearly visible relative to the background of the cornea, but they did appear wavy (Fig. 4). Based on the previously published results, this waviness is from the inaccuracies in the scanning stages rather than from intrinsic irregularities of the material or tissue.19
Fig. 4.
DIC images of blue-IRIS phase grating lines in feline and human corneas. Phase grating (bright) lines inscribed with blue-IRIS at in (a) cat and (b) human corneal tissue. Note the comparable appearance of phase lines in both species. There was no visible damage (bubbles or burns) in tissue from either species. Line waviness is most likely due to jitter in the piezo stages used for scanning.
The blue-IRIS procedure is used to inscribe a phase grating whose transmittance function can be written as
| (1) |
where is the grating line width (), is the grating period, and and are the phase delays of the grating lines and the ambient region, respectively. In terms of the index of refraction, the phase delays may be written as: and , where is the grating line thickness (), is the average index of refraction of cornea, is the RI of the grating lines, and is the wavelength of light incident on the gratings (632.8 nm). These parameter values are based on our previous work in hydrogels and were obtained from DIC images of a cross section of a grating line.18
To calculate the RI change from the first-order diffraction efficiency, a physical optics model was used. Blue-IRIS is a multiphoton process, and RI change will only occur in the focal region. Across that area, the intensity profile of the laser beam should be nearly uniform, thus a uniform (“top hat” shape) index change in the grating lines is assumed. From there, using Eq. (1) and the convolution theorem, the spectrum of the grating is found. Then, the intensity distribution of the diffraction pattern is given by
| (2) |
From Eq. (3), the zeroth- and first-order diffraction intensities are given by
| (3) |
| (4) |
The first-order diffraction efficiency is given by . From this, the RI change in the grating lines may be calculated.
2.4. Statistical Analyses
Values provided are and 95% confidence intervals (CI) with two-tailed -tests, ANOVAs or Pearson’s correlations used to assess significance as .20
3. Results
The average RI change obtained in human corneal tissue in this experiment was (), compared with () achieved in feline corneal tissue at the same scan speed of . Two-tailed, unpaired Student’s -tests revealed no significant differences between the RI change attained in cat versus human corneas (, ).
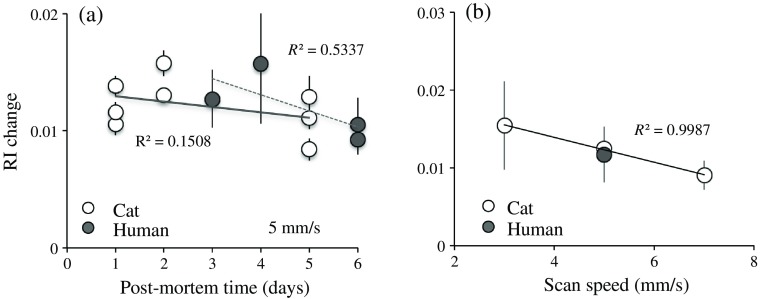
Because the postmortem time prior to delivery varied rather significantly between 2 and 6 days for human corneal tissue, and because dissected corneal tissue is known to degrade over time, we also investigated whether postmortem time impacted the magnitude of RI change attainable with blue-IRIS, and whether this is different between cats and humans. Linear regression analysis performed on the data revealed no significant correlation between RI change and the range of postmortem times used in the present study for either species [Fig. 5(a), feline cornea: , , , lower for , upper for ; human cornea: , , , lower for , upper for ]. Finally, we also assessed the relationship between RI change and scan speed. This was done in cat tissue only, as it was more readily obtainable than human tissue. The RI changes attained for scan speeds of 3 and were and , respectively [Fig. 5(b)]. When combined with our cat data, this appears to support our previous findings13,21 of a significant inverse relationship between RI change and scan speed (, , , lower for , upper for ).
Fig. 5.
(a) Magnitude of RI change versus postmortem age of the tissue. (b) Magnitude of RI change versus scan speed. Linear regression analysis revealed a significant inverse correlation between RI change and scan speed (), whereas for postmortem time, the correlation with RI change was not significant ( for cat, and for human). values for each regression line are indicated in the graphs.
As mentioned earlier, this method for measuring RI change was developed in inert hydrogel materials and did not account for the intrinsic background scatter from the cornea (Fig. 3). Using the custom diffractometer, scatter was measured in both unaltered and blue-IRIS-treated corneas. Scatter was measured in areas adjacent to the blue-IRIS phase gratings, and no difference was seen between the intrinsic scatter in treated and untreated eyes.
3.1. Comparison with Previous Results
We first reported writing blue-IRIS structures in ex vivo feline corneal tissue11 with an RI change of at a scan speed of . In the present study, the RI change achieved at the same scan speed was only . We posit that the main reason for this difference is that in the present study, we used lower power in the focal volume (61 mW compared with 80 mW) and wrote deeper in the stroma ( below the surface compared with ). Blue-IRIS relies on the intrinsic two-photon absorption of the tissue, a nonlinear process we now know to be affected by both laser power and focal spot degradation, due to uncorrected spherical aberration.18,21,22 The greater writing depth and uncorrected spherical aberration in our objective likely contributed to focal spot degradation and to a lower RI change.
4. Discussion
The present proof-of-concept study showed—for the first time—that RI change was achievable in human corneal tissue using blue-IRIS. However, because we used relatively slow scan speeds and low laser power (consistent with our previously published reports),8,10,13 the magnitudes of RI changes achieved in the present study were relatively low and unlikely to be usable as such for the purpose of clinical refractive correction. In order to create clinically relevant refractive structures, multiple blue-IRIS layers, written at high density (rather than in the form of widely spaced grating lines as done here), either continuously or using phase wrapping techniques to create Fresnel lenses will need to be employed. For Fresnel-based refractive devices, at least one wave of phase change in the visible spectrum (535 nm) is necessary. Using the formula for phase change presented in Sec. 2.3, an RI change of 0.0284 can be used to achieve one wave of phase change per layer. Alternatively, if three layers are written, the RI change per layer needs to only be 0.0095, the change achieved in this study, in order to induce one wave of phase change.
Both our present and prior work show that the amount of RI change is dependent on scan speed.13,21 Recent improvements to our blue-IRIS system now allow scan speeds upward of and powers of to be used to perform blue-IRIS.23,24 As such, we have been able to attain phase changes greater than one wave (at 535 nm) in tissue substitutes (hydrogels) and as well as in ex vivo and in vivo corneal tissues.23 Moreover, we have used blue-IRIS to write arbitrary refractive structures,21 including Fresnel lenses,24 and in 2014, we wrote cylinder lenses in four eyes of living cats, which remained stable for up to 12 months.12 In these four inscribed eyes, no statistically significant changes to corneal curvature or thickness were observed 1 month postoperatively, suggesting that blue-IRIS did not induce major structural changes to the cornea.12
5. Conclusion
Blue-IRIS creates comparable RI changes in both human and feline corneal tissues at low power and low scanning speeds. The fact that a measurable phase change can be reliably achieved in human corneal tissue at comparable speeds and laser power as in the cat cornea provides confidence that blue-IRIS systems can be successfully scaled up (higher power, faster scan speeds, and suitable writing patterns) to create the arbitrary refractive structures needed for refractive correction in humans. This present proof-of-concept study was thus a crucial step in the development of blue-IRIS for refractive vision correction.
Acknowledgments
The authors thank Margaret DeMagistris for excellent technical support, particularly in corneal tissue preparation. This project was supported by an unrestricted grant to the University of Rochester’s Department of Ophthalmology from the Research to Prevent Blindness (RPB) Foundation, by the National Institutes of Health (R01 grant EY015836 to KRH; Core grant P30 EY01319F to the Center for Visual Science; a Center for Visual Science training grant fellowship T32 EY007125 to DES), by a grant from Clerio Vision, Inc. with partial matching funds by the University of Rochester’s Center for Emerging & Innovative Sciences, a NYSTAR-designated Center for Advanced Technology, and by an Incubator Grant from the University of Rochester’s CTSI Scientific Advisory Committee (SAC).
Biography
Biographies for the authors are not available.
Disclosures
The authors declare the following interests: K.R. Huxlin, W. H. Knox, and J. D. Ellis have founder’s equity in Clerio Vision, Inc., which partially supported this research. K. R. Huxlin, W. H. Knox, and J. D. Ellis have no fiduciary responsibility in Clerio Vision, Inc.
References
- 1.Krueger R., Trokel S., Schubert H., “Interaction of ultraviolet laser light with the cornea,” Invest. Ophthalmol. Visual Sci. 26(11), 1455–1464 (1985). [PubMed] [Google Scholar]
- 2.Gartry D. S., “Treating myopia with the excimer laser: the present position,” Br. Med. J. 310(6985), 979–985 (1995). 10.1136/bmj.310.6985.979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dai G.-m., Wavefront Optics for Vision Correction, Vol. 179, SPIE Press, Bellingham, Washington: (2008). [Google Scholar]
- 4.Ambrósio R., Tervo T., Wilson S. E., “LASIK-associated dry eye and neurotrophic epitheliopathy: pathophysiology and strategies for prevention and treatment,” J. Refractive Surg. 24(4), 396–407 (2008). [DOI] [PubMed] [Google Scholar]
- 5.Nakamura K., et al. , “Intact corneal epithelium is essential for the prevention of stromal haze after laser assisted in situ keratomileusis,” Br. J. Ophthalmol. 85(2), 209–213 (2001). 10.1136/bjo.85.2.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Paula F. H., et al. , “Diffuse lamellar keratitis after laser in situ keratomileusis with femtosecond laser flap creation,” J. Cataract Refractive Surg. 38(6), 1014–1019 (2012). 10.1016/j.jcrs.2011.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Netto M. V., et al. , “Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy,” Cornea 24(5), 509–522 (2005). 10.1097/01.ico.0000151544.23360.17 [DOI] [PubMed] [Google Scholar]
- 8.Ding L., et al. , “Enhancement of intra-tissue refractive index shaping (IRIS) of the cornea by two-photon absorption,” in Conf. on Lasers and Electro-Optics, Optical Society of America; (2009). [Google Scholar]
- 9.Ding L., et al. , “Intra-tissue refractive index shaping (IRIS) of the cornea and lens using a low-pulse-energy femtosecond laser oscillator,” Invest. Ophthalmol. Visual Sci. 49(12), 5332 (2008). 10.1167/iovs.08-1921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagy L. J., et al. , “Potentiation of femtosecond laser intratissue refractive index shaping (IRIS) in the living cornea with sodium fluorescein,” Invest. Ophthalmol. Visual Sci. 51(2), 850 (2010). 10.1167/iovs.09-3901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu L., et al. , “Non-invasive blue intra-tissue refractive index shaping (IRIS) in living, excised cornea,” in Frontiers in Optics, Optical Society of America; (2010). [Google Scholar]
- 12.Savage D. E., et al. , “First demonstration of ocular refractive change using blue-iris in live cats,” Invest. Ophthalmol. Visual Sci. 55(7), 4603 (2014). 10.1167/iovs.14-14373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu L., et al. , “Noninvasive intratissue refractive index shaping (IRIS) of the cornea with blue femtosecond laser light,” Invest. Ophthalmol. Visual Sci. 52(11), 8148 (2011). 10.1167/iovs.11-7323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doughty M. J., Zaman M. L., “Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach,” Surv. Ophthalmol. 44(5), 367–408 (2000). 10.1016/S0039-6257(00)00110-7 [DOI] [PubMed] [Google Scholar]
- 15.Gilger B., et al. , “Corneal thickness measured by ultrasonic pachymetry in cats,” Am. J. Veterinary Res. 54(2), 228–230 (1993). [PubMed] [Google Scholar]
- 16.Nagy L. J., et al. , “Photorefractive keratectomy in the cat eye: biological and optical outcomes,” J. Cataract Refractive Surg. 33(6), 1051–1064 (2007). 10.1016/j.jcrs.2007.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindstrom R. L., et al. , “Optisol corneal storage medium,” Am. J. Ophthalmol. 114(3), 345–356 (1992). 10.1016/S0002-9394(14)71803-3 [DOI] [PubMed] [Google Scholar]
- 18.Ding L., et al. , “Large refractive index change in silicone-based and non-silicone-based hydrogel polymers induced by femtosecond laser micro-machining,” Opt. Express 14(24), 11901–11909 (2006). 10.1364/OE.14.011901 [DOI] [PubMed] [Google Scholar]
- 19.Brooks D. R., et al. , “Precision large field scanning system for high numerical aperture lenses and application to femtosecond micromachining of ophthalmic materials,” Rev. Sci. Instrum. 85(6), 065107 (2014). 10.1063/1.4880727 [DOI] [PubMed] [Google Scholar]
- 20.Lowry R., “VassarStats: website for statistical computation,” www.vassarstats.net (17 May 2017).
- 21.Gandara-Montano G. A., et al. , “Femtosecond laser writing of freeform gradient index microlenses in hydrogel-based contact lenses,” Opt. Mater. Express 5(10), 2257–2271 (2015). 10.1364/OME.5.002257 [DOI] [Google Scholar]
- 22.Xu L., Knox W. H., Huxlin K. R., “Exogenous and endogenous two-photon absorption for intra-tissue refractive index shaping (IRIS) in live corneal tissue [Invited],” Opt. Mater. Express 1(7), 1159–1164 (2011). 10.1364/OME.1.001159 [DOI] [Google Scholar]
- 23.Ellis J., et al. , “Scalability in contact lens manufacturing to improve the refractive performance and user comfort,” in ASPE Sprint Tropical Meeting: Precision Engineering and Optics, Tucson, Arizona: (2017). [Google Scholar]
- 24.Zheleznyak L., et al. , “First demonstration of human visual performance through refractive-index-modified ophthalmic devices written in hydrogels,” in Association for Research in Vision and Ophthalmology Annual Meeting, Baltimore, Mary Land: (2017). [Google Scholar]