Abstract
Case study description and analysis of a complex craniovertebral dysplasia in an 8-year-old male patient, in which conventional cervical spine radiographs demonstrated a regularly differentiated occipital base, as well as the presence of two lateral masses of the proatlas vertebra and two lateral masses of the atlas vertebra. Further assessment included computed tomography of the occipital base and the upper cervical spine as well as three-dimensional reconstruction. Malsegmentation of the fourth occipital vertebra can result in various anomalies that are known as ‘manifestation of the proatlas’. The occurrence of a persistent proatlas with additional segmentation of the craniovertebral junction represents an extremely rare dysplasia. To our knowledge, it is the second report concerning the persistence of a complete human proatlas vertebra. We consider the biomechanical and embryological particularities of this complex dysplasia to represent sufficient basis for future differentiation from other malformations of the fourth occipital vertebra. Comprehensive literature review and discussion about the entity will be provided.
Keywords: persistent proatlas, additional segmentation, manifestation of proatlas, manifestation of occipital vertebra, malformation, craniovertebral junction, cervical spine, occipital vertebra, atlas vertebra, computed tomography, CT scan, plain radiographs, X-ray, Sandberg-Gutmann
CASE REPORT
The complex craniovertebral dysplasia of an 8-year-old boy was analysed retrospectively. The child’s parents sought advice from a specialist in pediatric orthopedics because of movement restriction of the cervical spine, occasional headaches, attention deficits, and suspect posture. Diagnostics included conventional radiography the upper cervical spine and computed tomography (CT) of the occipital base and the upper cervical spine with three-dimensional (3D) reconstruction. Clinical neuro-orthopedic evaluation revealed moderate dysdiadochokinesia in both hands. No neurological deficits were observed. Inclination was decreased for the upper cervical range of motion.
Radiological evaluation showed serious malformation of the upper cervical spine with formation of 8 upper cervical spine segments (Fig. 2–4). A persistent proatlas (persisting bone material of the sixth somite in formation of the craniovertebral junction) with two lateral masses of the proatlas vertebra and its posterior arch was present above the actual atlas vertebra (Fig. 1–6, 8–11). Anterior arches of proatlas and atlas vertebra had been replaced by connective tissue (Fig. 2–4, 8, 11). The lateral masses of the atlas vertebra were normally formed, while its posterior arch was hypoplastic without compression of the medulla spinalis (Fig. 2–4, 5, 10–11). An os odontoideum was located above the dens axis (Fig. 2,5,7,8).
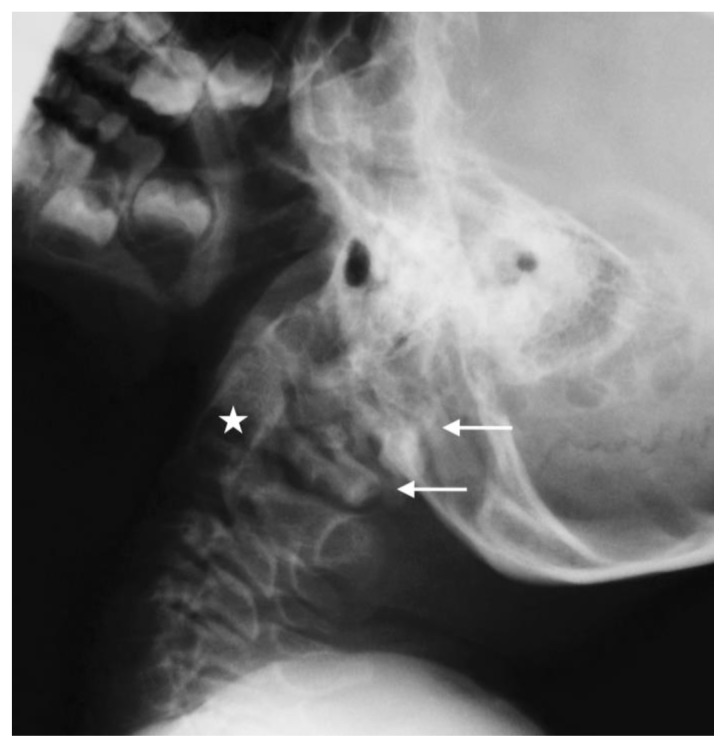
Figure 2.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction. Eight upper cervical spine segments.
Technique: Lateral plain radiograph according to Sandberg-Gutmann (75 kvp, 10 mAs).
Findings: Two posterior arches of C1 (white arrows) as well as normal C2 vertebra (white asterisk). The anterior arches of “regular” C1 and of the persisting proatlas vertebra are missing.
Figure 3.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction. Eight upper cervical spine segments.
Technique: Lateral plain radiograph in inclination according to Sandberg-Gutmann (75 kvp, 10 mAs).
Findings: Two posterior arches of C1 (white arrows). No obvious functional instability.
Figure 4.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Lateral plain radiograph in reclination according to Sandberg-Gutmann (75 kvp, 10 mAs).
Findings: Two posterior arches of C1 (white arrows) as well as normal C2 vertebra (white asterisk). No functional instability in reclination.
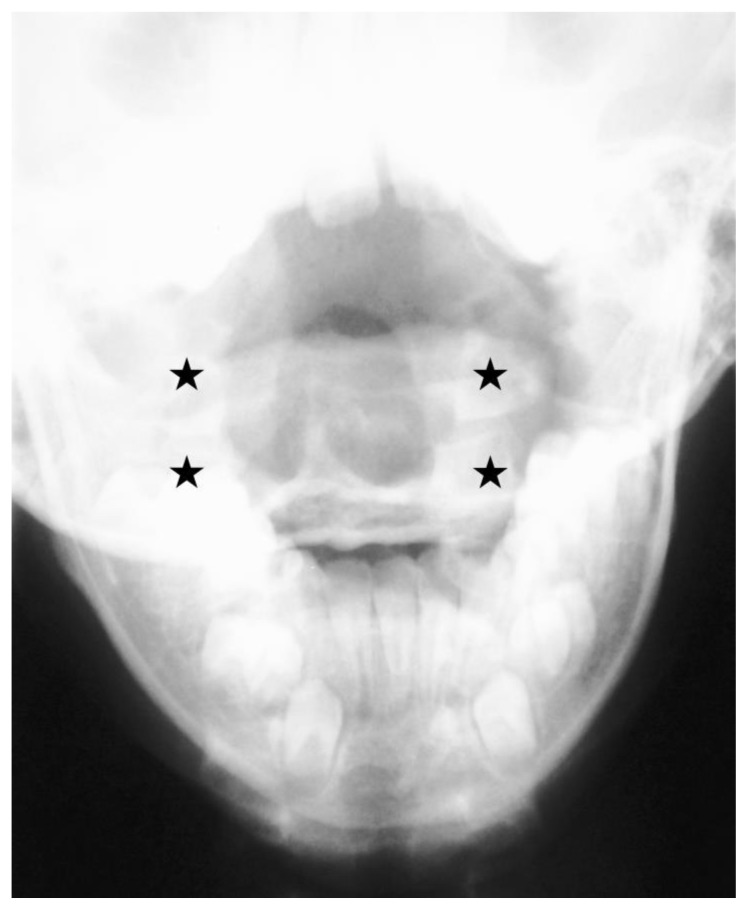
Figure 1.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Plain a.p. radiograph according to Sandberg-Gutmann (75 kvp, 10 mAs).
Findings: Additional lateral masses of C1 (black asterisks upper row) representing a complete persistence of proatlas vertebra and the “regular” lateral masses of C1 (black asterisks lower row).
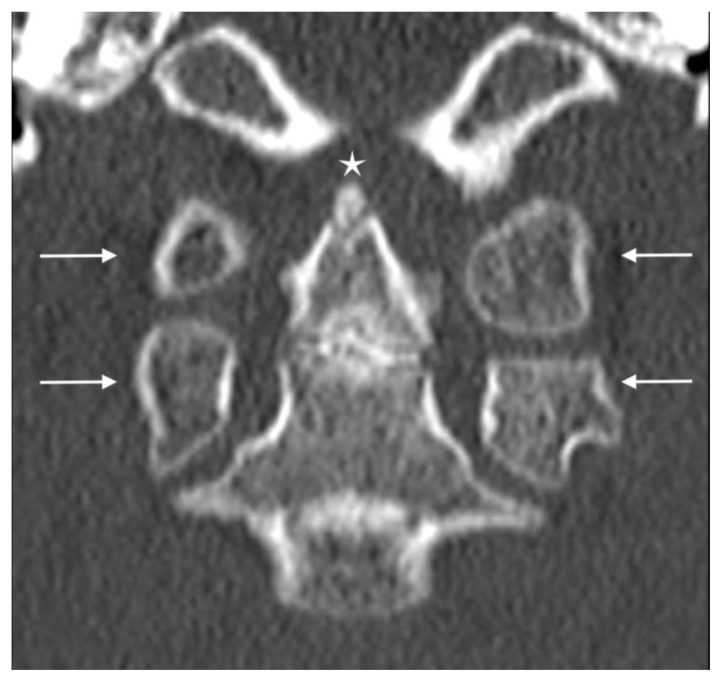
Figure 5.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm), coronal plane.
Findings: Lateral masses of ‘two atlas-like vertebrae’ (white arrows) - the proatlas vertebra (above) and the atlas vertebra (below) - as well as os odontoideum (white asterisk).
Figure 6.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm), sagittal plane.
Findings: Occipital base and the lateral masses of ‘two atlas-like vertebrae’ (white arrows). Proatlas vertebra (above) and “regular” atlas vertebra (below).
Figure 8.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm). 3-D-reconstruction.
Findings: Anterior aspect with dens axis and the lateral masses of ‘two atlas-like vertebrae’ (white asterisks). Anterior arches of proatlas (above) and atlas vertebra (below) are missing. Os odontoideum at the top of dens axis with characteristic location. Dens axis without any sign of malformation.
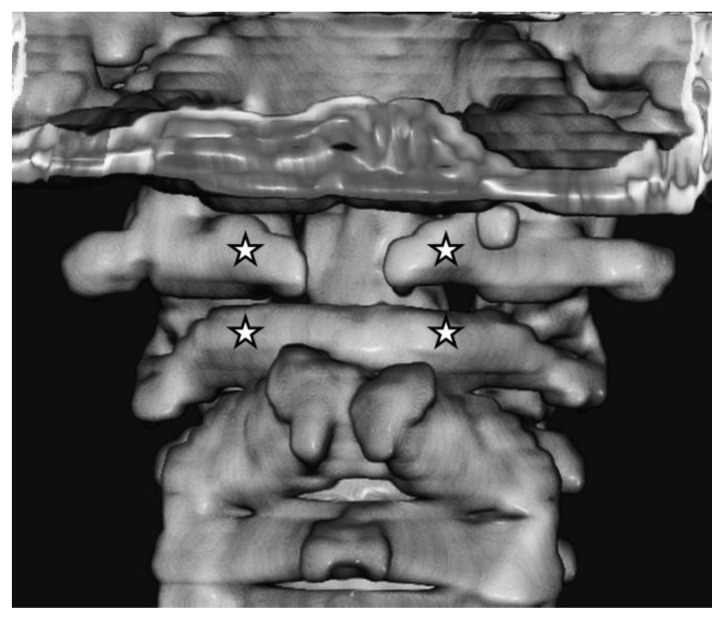
Figure 9.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm). 3-D-reconstruction.
Findings: Posterior aspect with posterior arch of C2, proatlas (white asterisks upper row) and atlas vertebra (white asterisks lower row). Malfusion of posterior arch of the persisting proatlas whereas the posterior arch of the “regular” C1 is closed.
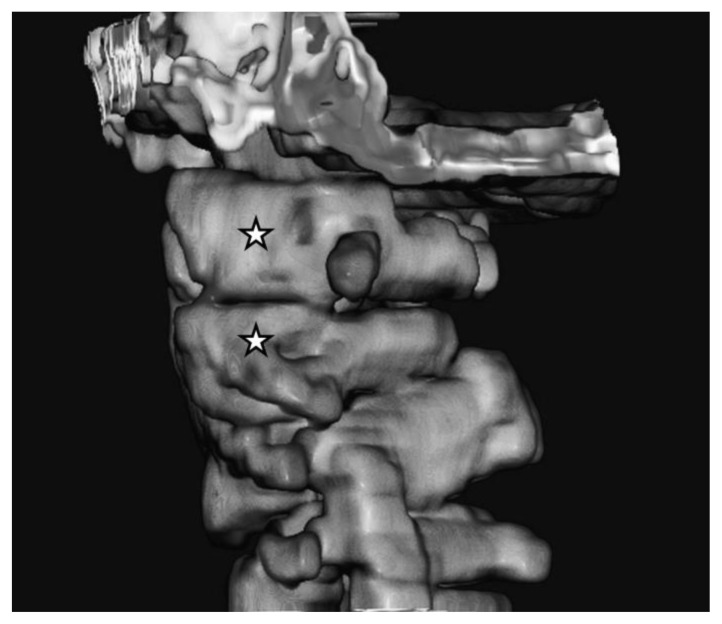
Figure 10.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm). 3-D-reconstruction.
Findings: Left lateral aspect showing the lateral masses of the proatlas (white asterisk above) and atlas vertebra (white asterisk below) representing an additional segment of the upper cervical spine.
Figure 11.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm). 3-D-reconstruction.
Findings: Right lateral/anterior aspect showing the lateral masses of proatlas (above) and atlas vertebra (below) - (white asterisks). Malfusion of the anterior arches of proatlas (above) and atlas vertebra (below).
Figure 7.
Eight-year-old boy with persistent proatlas and additional segmentation of the craniovertebral junction.
Technique: Non contrast CT (Siemens, 110kV, 25mAs, 0,6 mm, 16,06 mGycm), sagittal plane.
Findings: Os odontoideum at the top of dens axis (white arrow) with characteristic location. Clivus without malformation.
Therapy primarily focused on posture training and prevention of cervical anteflexion (e.g. at school), as well as social-medical counselling. Regular follow-ups of the developmental changes in the cervical region and of the posture were planned.
DISCUSSION
Etiology & Demographics
Manifestation of an additional suboccipital segment in humans, as normal in certain reptiles and dinosaur fossils, has been reported only once so far [1]. Tsuang et al. reported a case of proatlas manifestation [2].
Clinical & Imaging findings
The radiological findings revealed ‘two atlas-like vertebrae’ between the occipital bone and the axis without obvious instability. To our knowledge, no previous report has described proatlas manifestation with an accessory suboccipital cervical spine segment. This unique malformation has not been previously described or analysed. Hence, the present documented case represents the second description of this type of malformation.
We consider the manifestation of a proatlas with additional suboccipital cervical spine segmentation should be differentiated from other manifestations of the proatlas, due to the biofunctional importance of an additional segment in the upper cervical spine and the anatomical aspects of its development [3, 4, 5]. Following the customary terminology of similar dysplasia and an appreciation of the first observers, we propose the term ‘Tsuang-Goehmann malformation’ to describe this condition. Specifically, the Tsuang-Goehmann malformation is characterised by the formation of an additional cervical segment of the spine above the atlas with the development of two lateral masses of the proatlas vertebra. Primary biomechanical function of the atlantooccipital joint is movement in the sagittal plane, especially inclination [6]. Accordingly this particular plane of motion was functionally impaired in the 8-year-old boy. However reclination movement compensated for this impaired movement.
Tsuang-Goehmann malformation appears to result from homeotic transformation. The craniocervical junction is displaced cranially by one single segment. From a phylogenetic perspective, the homeobox is a highly conservative deoxyribonucleic acid (DNA) segment responsible for the expression of regional margins [7]. Similar dysplasia has been observed in mice with experimentally altered homeobox genes [1]. A third occipital vertebra accompanies the repositioning of the craniocervical junction. The structures of the anteproatlas would directly influence the development of the craniocervical region in this case. The existence of two lateral masses of the proatlas vertebra with cranial and caudal articular surfaces is manifested by the formation of an additional cervical segment and displacement of the craniocervical junction. By contrast, manifestations commonly termed ‘proatlas’ are merely disorders of the differential process of the proatlas.
The Tsuang-Goehmann malformation represents its own developmental entity, and its pathogenetic background remains to be fully understood. The discovery of this dysplasia is another milestone in the on-going exploration of the development of the craniocervical region.
Treatment & Prognosis
Therapy in this case primarily focused on posture training and prevention of cervical anteflexion (e.g. at school). Regular follow-ups of the developmental changes in the cervical region and of the posture were scheduled. The prognosis for the patient is unknown.
Differential Diagnoses
Differential diagnoses of this exceptional and rare entity, despite incorrect determination of the number of cervical segments, do not exist to the author’s knowledge.
Due to the complexity of the transition region, however, some special situations have to be considered and explained by their embryological formation [3].
Accessory bony malformations and/or dysplasia of proatlas formation origin
The entity described, as well as the accessory occipital condyle, the persisting ossiculum terminale, the os odontoideum, the hypoplastic occipital condyles and the consequent basilar impression can be summarized as accessory bony malformations and/or dysplasia of proatlas formation origin. Particular feature of the accessory occipital condyle is its location at the midpoint on the anterior margin of the foramen magnum (basion) [7]. It can easily be detected on plain anterior-posterior (a.p.) and lateral X-ray films, under the condition that the base of the skull is well focused. Distinguishing feature of the ossiculum terminale persistens is its location above the tip of the dens axis; in comparison the os odontoideum is located above the base of the dens axis at the apical portion. Computed tomography is optional for verification in most cases. Hypoplasia of the occipital condyles is characterised by ascending of the tip of the axis over the digastric line (drawn between right and left digastric groove on plain a.p. films). This may be a possible indicator of the presence of a basilar impression. On lateral films the same situation is characterised by the tip ascending McRae’s line (drawn between basion and opisthion). Analogously ascending over digastric line can be measured on coronal reconstructed CT images and over McRae’s line on midsagittal reconstructed CT images. Basilar impression (BI) has to be differentiated into anterior BI due to platybasia or shortening of the clivus and medial BI due to hypoplasia of the condyles or Paget disease. In the majority of the cases computed tomography is used for verification of the suspected BI.
Dysplasia of atlas formation origin
Assimilation of the atlas vertebra with the skull base and the malformations of the arches of C1 can be summarized as dysplasia of atlas formation origin [3]. In Atlas-Assimilation ossification of the skull base and the atlas vertebra can occur unilateral or bilateral. In case of suspect findings dynamic studies according to Sandberg-Gutmann (inclination/reclination) should be considered to draw conclusions about the stability of the particular situation [6]. Anomalies of the arches of C1 result from malfusion and relate to the anterior, the posterior, or less common, both arches. Hypoplasia as well as aplasia is possible. Dynamic studies (see above) may be helpful to clarify.
Dysplasia of atlas and axis formation origin
Assimilation of C1 and C2 is classified as malformation of atlas and axis formation origin and is usually seen as characteristic unilateral or bilateral ossification of atlas and axis vertebra. It can easily be detected on plain a.p. and lateral X-ray films and rarely makes difficulties in differentiation.
Dysplasia of axis formation origin
Defects of atlanto-axial segmentation, on the other hand, are classified as dysplasia of axis formation and represent as hemiaplasia or aplasia of the axis shoulder (unilateral/bilateral) or block vertebra with partial or complete fusion of the adjacent vertebral bodies [3]. Dynamic studies are recommended to make statements about the functional significance in most cases [6].
Even if anomalies of the odontoid process (seen as ossiculum terminale Bergmann, os odontoideum and os odontoideum verum) might occur due to proatlas formation disturbance (see above), an assignment to the group of axis formation origin is possible as well [3]. From embryological point of view, as well as from radiological point of view, precise clarification is difficult. Radiological imaging might be challenging in some cases. Anomalies of the arch of C2 result from malfusion. This dysplasia of axis formation origin is seen as partial hypoplasia, hyperplasia or aplasia. The first two mentioned rarely have clinical significance, making further diagnostic imaging unnecessary, when they occur isolated [6]. Fusion of C2 and C3, dysplasia of axis formation origin again, represent as block vertebra with partial or complete fusion of the adjacent vertebral bodies. In the mindset of Gutmann dynamic studies are obligatory to make statements about the functional impact and are recommended by the authors [6].
Conclusion
In conclusion, we were able to retrospectively verify the existence of a persistent proatlas with additional segmentation of the cervical spine. This dysplasia is a unique entity and should therefore be differentiated from other disorders of the fourth occipital vertebra. Hence, we propose the term Tsuang-Goehmann malformation because of unique biomechanical and developmental particularities.
TEACHING POINT
The importance of radiological differential diagnostics of cervical dysfunction in children is still or more than ever controversial especially in manual medicine, which raises the question whether the requirement of x-ray-diagnostics prior to any manual manipulation treatment is necessary or not. With regard to the diagnosis of the spinal column valuable diagnostic information can be obtained by plain radiographs of the upper cervical spine. The indication for radiological diagnostics using computed tomography should be made carefully after consultation with the radiologist. The chosen case example from routine practice shows that a functional disorder of the upper cervical spine can be expression of extremely rare pathomorphological situation and that imaging diagnostic is essential in the clinical diagnostic setup.
Table 1.
Summary table for Tsuang-Goehman-malformation.
| Etiology | homeotic transformation with cranial “shift” of the craniovertebral junction by one single segment |
| Incidence | extremely rare, two cases (this included) |
| Gender ratio | unknown |
| Age predilection | unknown |
| Risk factors | unknown |
| Treatment | depending of stability/functional stability |
| Prognosis | unknown |
| Imaging findings | X-ray and CT: presence of two lateral masses of the proatlas vertebra and two lateral masses of the atlas vertebra |
Table 2.
Differential diagnosis table for craniocervical malformations and embryologic origin.
| Pathology | X-ray a.p. | X-ray lat. | CT |
|---|---|---|---|
| Tsuang-Goehman-malformation |
|
|
|
| Accessory occipital condyle |
|
|
|
| Ossiculum terminale persistens |
|
|
|
| Os odontoideum |
|
|
|
| Hypoplasia of occipital condyles |
|
|
|
| Basilar impression (BI) |
|
|
|
| Assimilation of Atlas vertebra |
|
|
|
| Anomalies of arches (C1) |
|
|
|
| Assimilation of C1/C2 |
|
|
|
| Defects of atlanto-axial segmentation |
|
|
|
| Anomalies of odontoid process |
|
|
|
| Anomalies of arch (C2) |
|
|
|
| Fusion of C2/C3 |
|
|
|
ABBREVIATIONS
- 3D
three-dimensional
- a.p.
anterior-posterior
- BI
basilar impression
- C1
Atlas vertebra
- C2
Axis vertebra
- C3
third cervical vertebra
- CT
computed tomography
- DNA
deoxyribonucleic acid
- lat.
lateral
REFERENCES
- 1.Kessel M, Balling R, Gruss P. Variations of the cervical vertebrae after expression of a Hox-1.1 transgene in mice. Cell. 1990;61:301–8. doi: 10.1016/0092-8674(90)90810-2. [DOI] [PubMed] [Google Scholar]
- 2.Tsuang FY, Chen JY, Wang YH, et al. Neurological Picture. Occipitocervical malformation with atlas duplication. J Neurol Neurosurg Psychiatry. 2011;82:1101–2. doi: 10.1136/jnnp-2011-300200. [DOI] [PubMed] [Google Scholar]
- 3.Prescher A, Brors D, Adam G. Anatomic and radiologic appearance of several variants of the craniocervical junction. Skull Base Surg. 1996;6:83–94. doi: 10.1055/s-2008-1058649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Went H. Zur Manifestation eines Proatlas. Fortschr Röntgenstr. 1961;95:370–4. [PubMed] [Google Scholar]
- 5.Goldfeld M, Loberant N, Herskovits M. Manifestations of persistent proatlas: radiographic and computed tomographic appearance. Eur Radiol. 1994;4:71–4. [Google Scholar]
- 6.Gutmann G. Funktionelle Pathologie und Klinik der Wirbelsäule. Band 1: Die Halswirbelsäule. Stuttgart: Fischer; 1981. pp. 117–24. [Google Scholar]
- 7.Pang D, Thompson D. Embryology and bony malformations of the craniovertebral junction. Childs Nerv Syst. 2011;27:523–64. doi: 10.1007/s00381-010-1358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]