Abstract
Pseudoaneurysms are potentially fatal complications of vascular trauma; however, they are rarely seen as the sole complication of penetrating injury. We present a case of a pseudoaneurysm with an associated arteriovenous fistula of the left lateral thoracic artery as a result of direct trauma from a knife stab. The patient presented only with a painful, swollen left pectoralis muscle. Upon diagnosis, he was taken to the interventional radiology suite and treated successfully with fluoroscopic guided coil embolization. Cases such as these are infrequent and should encourage more aggressive use of contrast enhanced computed tomography imaging for soft tissue injury, as a missed traumatic pseudoaneurysm may result in life-threatening hemorrhage.
Keywords: Pseudoaneurysm, Trauma, Interventional radiology, Hemorrhage, Computed tomography, Thoracic Trauma
CASE REPORT
We present the case of a 52 year old male with no significant past medical history who presented to an outside hospital after being stabbed with a knife in the left upper chest. Workup at the outside facility included standard laboratory panels, which were negative for any significant derangement, and a chest x-ray showing no acute fractures, hemothorax or pneumothorax. The patient was transferred to our institution for further management. On arrival, primary survey was intact, hemoglobin was within normal limits and the patient endorsed a history of a single stab wound to the left chest and no other trauma. He was complaining of loco-regional pain and physical examination revealed a 1.5 centimeter entrance wound, circumferential soft tissue swelling without a palpable thrill or pulsation and no visible exit wound. Chest x-ray was negative for any acute abnormalities and the decision was made to proceed with computed tomography scanning of the chest to assure no occult injuries to vital structures. The chest scan conducted with intravenous contrast revealed a 6.7 (transverse) by 9.4 (craniocaudal) centimeter hematoma on the left anterior chest wall with an associated 1.4 (transverse) by 1.0 (antero-posterior) by 2.4 (craniocaudal) centimeter pseudoaneurysm and arteriovenous fistula in the left axilla (Figure 1).
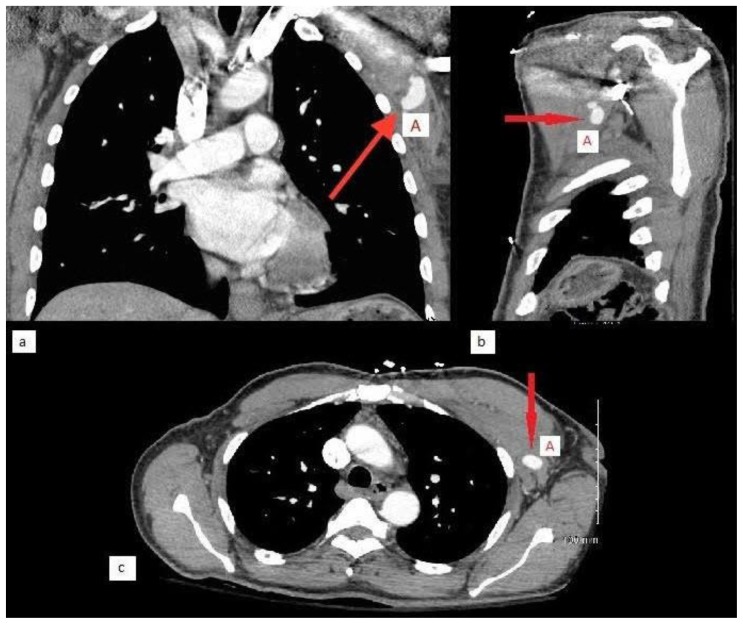
Figure 1.
A 52 year old male status post stabbing with a traumatic left lateral thoracic artery pseudoaneurysm.
Findings: A saccular, contrast-enhanced 1.4 (transverse) by 1.0 (antero-posterior) by 2.4 (craniocaudal) cm pseudoaneurysm (A) within the musculature of the left chest wall. In the surrounding soft tissue there is a heterogeneous fluid collection measuring 6.7 (transverse) by 9.4 (craniocaudal) cm, suggested of hematoma formation. Demonstrated are coronal (a), sagittal (b) and axial (c) views.
Technique: GE Healthcare Discovery CT 750HD™ chest computed tomography scan enhanced with 300 cc of intravenous iohexol solution (1.25 mm slice thickness, 5060 mAs, 120 kVp).
The patient was subsequently admitted to the trauma service and transferred directly to the interventional radiology suite. Left subclavian arteriography identified a pseudoaneurysm with an adjacent arteriovenous fistula originating from a branch of the left lateral thoracic artery (Figure 2). The affected branch was embolized with platinum microcoils proximal and distal to the origin of the pseudoaneurysm. The arteriovenous fistula appeared to have resulted directly from the pseudoaneurysm; therefore, exclusion of the entire pseudoaneurysm and feeding artery resulted in exclusion of the arteriovenous fistula. Completion angiogram confirmed absence of flow into both the pseudoaneurysm and arteriovenous fistula (Figure 3). The patient was subsequently discharged in stable condition after the remainder of an uncomplicated hospitalization.
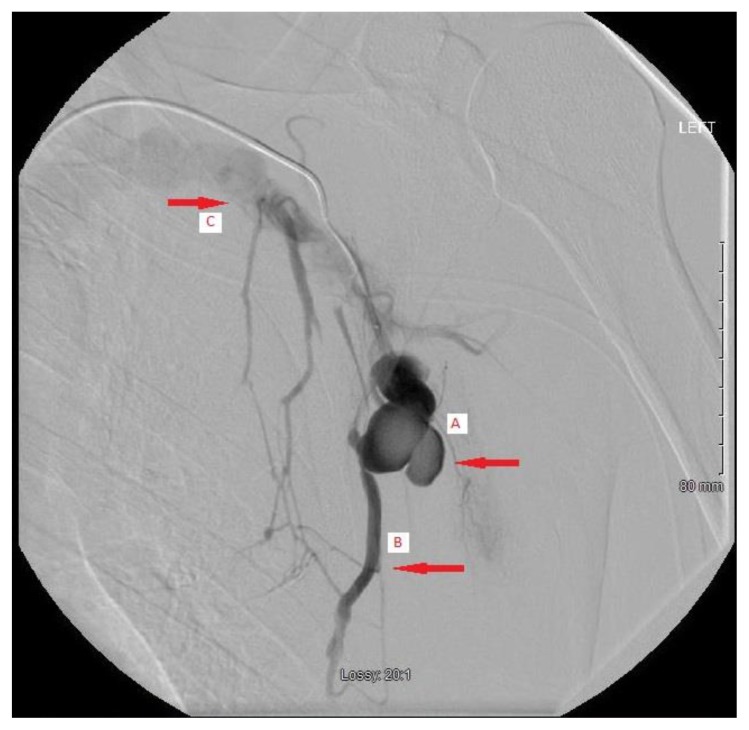
Figure 2.
A 52 year old male status post stabbing with a traumatic left lateral thoracic artery pseudoaneurysm.
Findings: Image: A lobulated pseudoaneurysm of the left lateral thoracic artery (A). Early venous filling his demonstrated (B) indicating arteriovenous fistula formation. Contrast is then seen returning into the central venous system (C).
Technique: Spot radiograph during the venous phase of digital subtraction angiography sequence with injection of iohexol contrast solution through a Renegade Hi-flo microcatheter.
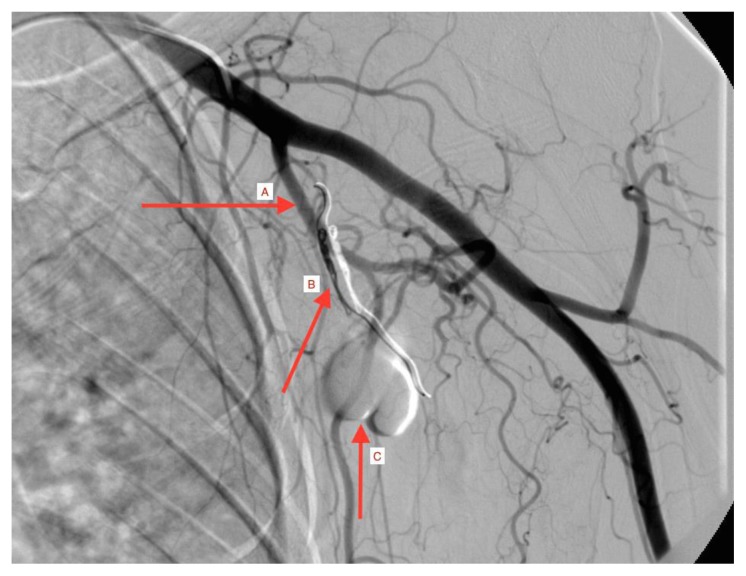
Figure 3.
A 52 year old male status post stabbing with a traumatic left lateral thoracic artery pseudoaneurysm.
Findings: The lateral thoracic artery (A) is cannulated and platinum microcoils have been deployed into the lateral thoracic artery (B). The lobulated pseudoaneurysm (C) is now excluded and devoid of flow.
Technique: Spot radiograph during the arterial phase of digital subtraction angiography sequence with injection of iohexol contrast solution through a Renegade Hi-flo microcatheter.
DISCUSSION
Etiology & Demographics
Pseudoaneurysms are common vascular insults with the majority of cases being seen at vascular anastomotic sites [1]. They are also documented in the setting of both penetrating and blunt trauma, but are typically associated with other injuries [2]. These lesions result from a disruption in an arterial wall and subsequent pressurized extravasation of blood. Disruption in the muscular layer of the vessel precludes proper vascular contraction in response to the inciting injury. This, in turn, prevents sealing of the defect and blood extravasates, forms a clot and eventually a fibrinous wall, which is prone to rupture [3]. Arterial pseudoaneurysms are common complications of vascular access; however, isolated pseudoaneurysms from penetrating trauma are very rare [4]. Pseudoaneurysms of the lateral thoracic artery have presented in the setting of blunt force trauma, however, none have been documented in the setting of penetrating trauma. Here we present the case of a left lateral thoracic artery pseudoaneurysm with an associated arteriovenous fistula presenting as the sole injury after a stab wound to the chest.
Clinical & Imaging Findings
Pseudoaneurysms are often missed as they do not frequently present like most arterial trauma. However, a missed diagnosis in the trauma bay can result in life threatening immediate, or delayed hemorrhage [4]. Traumatic pseudoaneurysms should be suspected after a patient develops pain and/or swelling over a muscular compartment that contains a so-called ‘named’ artery, or if any soft and/or hard signs of vascular trauma are evident without frank bleeding. “Hard signs” of vascular injury include an expanding hematoma, palpable thrill, audible bruit, pulsatile bleeding, absent distal pulses or a cool distal limb. “Soft signs” include peripheral nerve deficits or reduced peripheral pulses. Depending on the aneurysm site, associated symptoms such as paresthesias or numbness may be present secondary to nearby nerve compression by the aneurysmal sac [7–10]. Signs and symptoms may be delayed and present weeks to months after the inciting injury, unlike typical vascular injuries. Delayed findings may even include skin necrosis [6].
A strong clinical suspicion accompanied by a thorough history and physical examination is key to timely diagnosis. In trauma, contrast enhanced computed tomography scans are frequently obtained and can identify the exact location and the extent of the lesion. They appear as saccular, contrast-filled, arterial dilations and may demonstrate associated contrast extravasation into surrounding tissues. They are frequently accompanied by surrounding tissue edema and hematoma. In non-trauma settings, the ideal imaging is ultrasound which will show a hallmark “to and fro” pattern; blood entering the false lumen in systole and re-entering the native vessel in diastole [11]. Brightness and M-mode duplex imaging can also demonstrate vascular extravasation and arteriovenous fistula formation [5,6]. Nevertheless, angiography remains the gold standard in diagnosis, and it is both diagnostic and potentially therapeutic.
Treatment & Prognosis
Treatment options for traumatic pseudoaneurysms include both operative and non-operative modalities. While many injuries can be managed non-operatively, surgical intervention is indicated in the presence of “hard signs” of vascular injury [5,6]. While small, 2–3 centimeter pseudoaneurysms do exhibit spontaneous thrombosis [6], it is not uncommon to intervene on said lesions given the catastrophic magnitude of the potential complications. Ultrasound guided compression results in successful thrombosis 74–86% of the time; however, invasive procedures such as ultrasound guided fibrin injection or angiographic coil embolization also demonstrate high thrombosis rates with lower recurrence rates and no change in hospital length of stay or complication rates [6,12–14]. Another less common intervention is endovascular stent deployment and exclusion of the pseudoaneurysm neck [6]. If the patient develops overlying soft tissue infection or mass effects (i.e. compression of adjacent neurovascular structures) surgical hematoma evacuation and arterial reconstruction are indicated [5,6]. If identified in a timely fashion and treated accordingly, traumatic arterial pseudoaneurysms have an excellent prognosis.
Differential Diagnoses
Arterial Aneurysm
Traumatic arterial aneurysms may present in a very similar fashion to pseudoaneurysms; however, aneurysm sacs are focal outpouchings that are still bordered by all the true layers of the vascular wall. Pseudoaneurysms are generally only bordered by a false boundary, therefore making them more prone to rupture. This diagnosis can only be differentiated by imaging.
Hematoma
Traumatic hematomas appear as subcutaneous swelling in the region of trauma. They may also create a mass effect resulting from compression of adjacent neurovascular structures. However, these lesions do not demonstrate a palpable thrill or pulsation, nor is there an associated bruit. Diagnostic imaging will reveal a collection of blood outside the artery in the absence of arterial malformation or contrast extravasation.
Compartment Syndrome
The development of compartment syndrome may mimic a traumatic pseudoaneurysm of an extremity. Compartment syndrome presents with a tense muscle compartment with associated exquisite pain on passive movement of the associated extremity. Paresthesias and loss of pulses are frequently a late clinical finding. Additionally, compartment syndrome may develop as result of a traumatic hematoma or pseudoaneurysm. In the absence of vascular trauma, imaging will only demonstrate soft tissue edema.
Conclusion
While infrequent, traumatic pseudoaneurysms present a potentially life threatening complication from seemingly innocuous trauma. Lesions of the lateral thoracic artery are not insignificant and hemorrhage from this artery has been associated with catastrophic outcomes [15]. Cases such as these strengthen the argument for more aggressive use of contrast enhanced computed tomography scans targeting musculoskeletal regions of the body affected by trauma. In the presence of swelling, an intact pulse exam or absence of a thrill or bruit does not exclude the presence of a pseudoaneurysm. Once diagnosed, we recommend a multidisciplinary approach to treatment involving prompt, if not emergent, consultation with interventional radiology or vascular surgery. Successful management of these lesions prevents immediate, as well as delayed hemorrhagic complications.
TEACHING POINT
Pseudoaneurysms represent a potentially fatal complication of trauma. They are readily identified by use of computed tomography and can be treated successfully by ultrasound-guided techniques or selective radiological procedures. Several therapeutic options exist and a multidisciplinary approach with interventional radiology can frequently obviate the need for surgical intervention.
Table 1.
Summary table for Pseudoaneurysm.
| Etiology |
|
| Incidence |
|
| Gender Ratio |
|
| Age Predilection |
|
| Risk Factors |
|
| Treatment |
|
| Prognosis |
|
| Imaging Findings |
|
Table 2.
Differential Diagnosis table for Pseudoaneurysm.
| Pseudoaneurysm |
|
| Hematoma |
|
| Compartment Syndrome |
|
| Aneurysm |
|
ABBREVIATIONS
- CT
Computed tomography
- MRI
Magnetic Resonance Imaging
- US
Ultrasound
REFERENCES
- 1.Zitsman JL. Pseudoaneurysm after penetrating trauma in children and adolescents. J Ped Surg. 1998;33(10):1574–1577. doi: 10.1016/s0022-3468(98)90504-8. [DOI] [PubMed] [Google Scholar]
- 2.Kalapatapu VR, Shelton KR, Ali AT, Moursi MM, Eidt JF. Pseudoaneurysm: a review. Curr Treat Options Cardiovasc Med. 2008;10:173–83. doi: 10.1007/s11936-008-0019-8. [DOI] [PubMed] [Google Scholar]
- 3.Feliciano DV, Mattox KL. Traumatic aneurysms. In: Rutherford RB, editor. Vascular Surgery. ed 3. Philadelphia, PA: Saunders; 1989. pp. 996–1003. [Google Scholar]
- 4.Counihan M, Pontell ME, Selvan B, Trebelev A, Nunez A. Delayed presentation of a lumbar artery pseudoaneurysm resulting from isolated penetrating trauma. J Surg Case Rep. 2015;2015(7) doi: 10.1093/jscr/rjv083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frykberg ER, Vines FS, Alexander RH. The natural history of clinically occult arterial injuries: a prospective evaluation. J Trauma. 1989;29:577–583. doi: 10.1097/00005373-198905000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad F, Turner SA, Torrie P, Gibson M. Iatrogenic femoral artery pseudoaneurysm: A review of current methods of treatment. Clinical Radiology. 2008;63:1310–1316. doi: 10.1016/j.crad.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Lalak NJ, Farmer E. Traumatic pseudoaneurysm of the superficial temporal artery associated with nerve palsy. J Cardiovasc Surg. 1996;37:119–123. [PubMed] [Google Scholar]
- 8.Yip KM, Yurianto H, Lin J. False aneurysm with median nerve palsy after iatrogenic brachial artery puncture. J Postgrad Med. 1997;73:43–44. doi: 10.1136/pgmj.73.855.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robbs JV, Naidoo KS. Nerve compression injuries due to traumatic false aneurysm. Ann Surg. 1984;200:80–82. doi: 10.1097/00000658-198407000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benzel EC, Prejean CA, Hadden TA. Pulsatile dysesthesia and an axillary artery pseudoaneurysm associated with a penetrating axillary artery injury. Surg Neurol. 1989;b31:400–401. doi: 10.1016/0090-3019(89)90075-x. [DOI] [PubMed] [Google Scholar]
- 11.Jaff M. Pseudoaneurysms. Clinical Treatment Options in Cardiovascular Medicine. 2002;4:239–245. doi: 10.1007/s11936-002-0004-6. [DOI] [PubMed] [Google Scholar]
- 12.Jeans WD, Leven HO. A new technique for nonsurgical repair of peripheral pseudoaneurysm. Acta Radiol. 1995;36:100–101. [PubMed] [Google Scholar]
- 13.Edwards H, Martin E, Nowygrod R. Nonoperative management of a traumatic peroneal artery false aneurysm. J Trauma. 1982;22:323–326. doi: 10.1097/00005373-198204000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Tisi PV, Callam MJ. Treatment for femoral pseudoaneurysms. Cochrane Database Syst Rev. 2009;2:CD004981. doi: 10.1002/14651858.CD004981.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Lee TH, Park YS, Chung DJ, Kim JH, Kim SM, Im EH, et al. Spontaneous rupture of the lateral thoracic artery in patients with liver cirrhosis. The Korean Journal of Internal Medicine. 2008;23:152–155. doi: 10.3904/kjim.2008.23.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]