Abstract
We present a case of a woman who was diagnosed with a hepatic abscess secondary to a migrated fish bone. As the patient did not improve after percutaneous drainage of the abscess, image-guided percutaneous transhepatic removal of the fish bone was performed. Fish bones in hepatic abscesses are typically removed surgically, with the fish bone left in situ in a number of cases. There has been only another reported case of percutaneous transhepatic fish bone removal. We conclude that in the rare case of a hepatic abscess complicating fish bone migration, image-guided percutaneous transhepatic removal of the offending foreign body is a feasible alternative to surgery, especially in high surgical risk patients.
Keywords: Fish bone, hepatic abscess, percutaneous removal, intervention, foreign body migration
CASE REPORT
An 85-year-old Chinese woman with a history of ischaemic heart disease presented to our institution’s emergency department with chest pain and epigastric discomfort. At the time of presentation, she had a low-grade fever but was hemodynamically stable. Initial investigations ruled out cardiac causes for her symptoms. She was admitted to the general medicine department for further evaluation.
On examination, her abdomen was soft with mild epigastric tenderness. Blood tests demonstrated an inflammatory process. Laboratory investigations revealed a raised C-reactive protein of 168 mg/dl (0.2–8.8 mg/dl), haemoglobin level of 10.3 g/dl (12.0–16.0 g/dl), white blood cell count of 7.64 (4.0–10.0 × 109/L) and borderline elevated aspartate transaminase (AST) of 34 UI/L (15–33 UI/L). The alanine transaminase (ALT) and alkaline phosphatase (ALP) were normal. Blood cultures were negative.
A computed tomography (CT) scan of the abdomen and pelvis was also requested by the attending clinician as an epigastric mass was felt clinically.
CT demonstrated a low-density, rim enhancing left hepatic lobe mass containing linear radiodense opacity (Figure 1). The thickened and edematous pylorus of the stomach was seen to closely abutting the hepatic mass (Figure 2). A diagnosis of left hepatic lobe abscess secondary to migration of a foreign body (thought to be a fish bone) from the stomach to the liver was thus made. The abscess measures 4.1 × 4.0 × 4.6 cm. The patient was then commenced on a course of intravenous antibiotics (ceftriaxone and metronidazole) and referred to us for percutaneous drainage of the abscess. We deployed an 8 French (F) drainage catheter into the abscess under ultrasound and fluoroscopic guidance with minimal difficulty. Pus culture and sensitivity was performed and grew streptococcus milleri with sensitivity covered by the given antibiotics.
Figure 1.
85-year-old female patient with liver abscess from fish bone. Initial CT abdomen and pelvis with intravenous contrast.
FINDINGS: Coronal (A), axial (B) and sagittal (C) sections demonstrate a high density linear foreign body (arrow) within a hypodense mass with thick and irregular enhancing rim compatible with abscess in the left lobe of the liver. The abscess measures 4.1 × 4.0 × 4.6 cm. Note that the distal stomach closely abuts this mass.
TECHNIQUE: 3mm axial with coronal and sagittal reconstruction computed tomography images obtained on a Siemens® SOMATOM® 64 slice spiral CT scanner at 256mAS, 1.2 KV and 500 msec.
Figure 2.
85-year-old female patient with liver abscess from fish bone. Initial coronal CT abdomen and pelvis with intravenous contrast.
FINDINGS: White circle illustrates the thickened and edematous pylorus of the stomach which was seen to closely abutting the hepatic abscess.
TECHNIQUE: 3mm coronal reformatted computed tomography images obtained on a Siemens® SOMATOM® 64 slice spiral CT scanner at 256mAS, 1.2 KV and 500 msec.
Over the next few days, the patient deteriorated clinically and progressed to septic shock. As it was felt that the fish bone was acting as a nidus for infection, the patient was again referred to us, this time for percutaneous removal of the foreign body, as the patient was considered a high-risk surgical candidate.
Prior to the procedure, CT of the abdomen was performed in the interventional radiology suite to reassess the size of the abscess which had become smaller measuring 1.5 × 1.2 × 1.6 cm, as well as to confirm the position of the foreign body and drainage catheter (Figure 3). The existing 8F drainage catheter was then removed over a Teflon wire, and an 8F vascular sheath advanced into the abscess cavity. A Teflon safety wire was also placed coaxially parallel to the sheath to maintain access.
Figure 3.
85-year-old female patient with liver abscess from fish bone. Non-contrast CT abdomen and pelvis.
FINDINGS: Axial section demonstrates the drainage catheter (thick arrow) and a high density foreign body (thin arrow).
TECHNIQUE: 3mm axial computed tomography images obtained on a Siemens® SOMATOM® 64 slice spiral CT scanner at 256mAS, 1.2 KV and 500 msec.
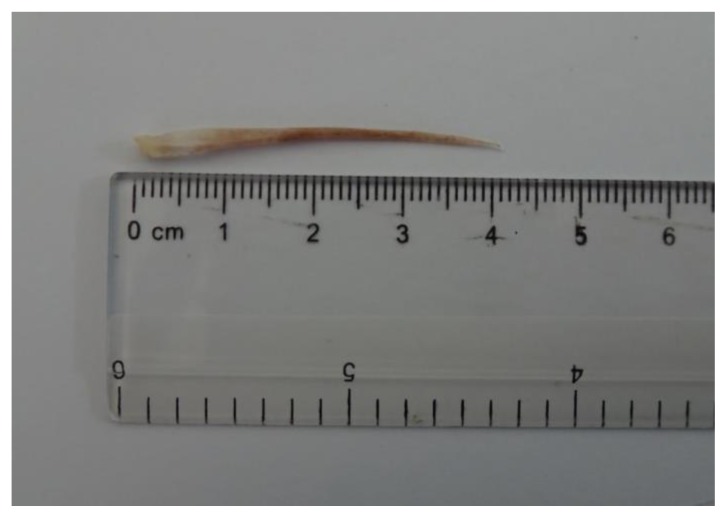
Using a combination of fluoroscopic and ultrasound guidance, removal of the foreign body was initially attempted with a 9–15mm Ensnare device, but this was unsuccessful (Figure 4). An Argon endomyocardial biopsy forceps was then used (Figure 5), and this time, the foreign body, a fish bone, was successfully removed together with the vascular sheath. A new 8F Skater catheter was then placed into the abscess cavity over the safety wire (Figure 6). Post procedure CT (Figure 7) was obtained to confirm that the fish bone (Figure 8) had been removed in its entirety. The patient tolerated the procedure well, with no immediate complications noted.
Figure 4.
Percutaneous retrieval of fish bone in an 85-year-old female patient with liver abscess in the left lobe.
FINDINGS: Fluoroscopic image showing removal of the foreign body (short arrow) which was initially attempted with a 9–15mm Ensnare device (long arrow), but this was unsuccessful.
TECHNIQUE: Diagnostic/therapeutic fluoroscopy in the PA projection (patient supine), 80 kV, 3mAs.
Figure 5.
Percutaneous retrieval of fish bone in an 85-year-old female patient with liver abscess in the left lobe.
FINDINGS: Fluoroscopic image showing the Argon endomyocardial biopsy forceps (long arrow) grasping the fish bone (short arrow).
TECHNIQUE: Diagnostic/therapeutic fluoroscopy in the PA projection (patient supine), 80 kV, 3mAs.
Figure 6.
Percutaneous retrieval of fish bone in an 85-year-old female patient with liver abscess in the left lobe.
FINDINGS: Fluoroscopic image showing a new 8F Skater catheter was then placed back into the abscess cavity over the safety wire. A small amount of contrast was injected and excluded free extravasation.
TECHNIQUE: Diagnostic/therapeutic fluoroscopy in the PA projection (patient supine), 80 kV, 3mAs.
Figure 7.
85-year-old female patient with liver abscess from fish bone. Non-contrast CT abdomen and pelvis.
FINDINGS: Axial section at the same level as Figure 3 demonstrates the new drainage catheter (arrow) and the previously seen high density foreign body has been removed. Small amount of injected contrast is noted in the vicinity.
TECHNIQUE: 3mm axial computed tomography images obtained on a Siemens® SOMATOM® 64 slice spiral CT scanner at 256mAS, 1.2 KV and 500 msec.
Figure 8.
85-year-old female patient with liver abscess from fish bone. Clinical images showing the retrieved fish bone.
The patient improved clinically over the next week. Unfortunately, on the day before planned discharge, the patient collapsed and passed away despite best resuscitative efforts. A post-mortem diagnosis of acute anterior myocardial infarction was established.
DISCUSSION
Hepatic abscess secondary to perforation of the gastrointestinal tract by a fish bone has been reported previously [1–5]. The abscess is typically drained either surgically or percutaneously, and the fish bone is usually removed surgically but has been left in situ in a few reported cases [3,4]. Percutaneous transhepatic fish bone removal has been reported in only one case in the existing literature [5]. This is another case of image-guided percutaneous transhepatic removal of a fish bone from a hepatic abscess following percutaneous drainage of the abscess.
ETIOLOGY & DEMOGRAPHICS
Most cases of foreign body ingestion usually pass without obstruction in the gastrointestinal tract in a week. In cases where the obstruction occurs, it can occur usually at the esophagus causing local injury. Rare cases of mediastinal abscesses have been reported. Foreign bodies tend to lodge at the oesophageal sphincters, pyloric canal, duodenum, ileocaecal valve and anus [3]. In the majority of the cases of fish bone migration, however, it occurs through the stomach and the duodenum. Other foreign bodies previously described as causing liver abscesses are chicken bones and toothpicks [1]. Overall, fish bones are the most common foreign bodies, and the stomach is the most common site of perforation, as previously reported [3]. Fishbone migration was found to be the commonest type of foreign body as the culprit in the development of liver abscesses [1]. Incidence is rare with less than 20 cases reported [3]. The type of foreign body ingestion may be influenced by geography as it is reported that fish bones ingestion forms a unique subgroup more commonly seen in Asian and Pacific populations, where consumption of fish largely exceeds that of Northern European populations [6].
CLINICAL & IMAGING FINDINGS
Liver abscess is common and presents with a range of different clinical manifestations and the classic triad of presentation of liver abscesses consisting of fever, abdominal pain and jaundice are uncommon. Liver abscess caused by migrated foreign body pose a further diagnostic challenge as most patients have nonspecific presentations and patients often cannot recall swallowing a foreign body [3]. Liver abscesses from foreign body migration usually develop in the left lobe of the liver due to its anatomical proximity with the stomach [1, 6].
CT is the imaging modality of choice for investigation due to its high resolution and accuracy in the diagnosis of the presence of a foreign body [1]. Chicken bones and most meat bones are opaque on radiographs but the majority of fish bones are not, even though some fish bones are readily apparent. Examples of other opaque materials include most metallic objects, some soil fragments, sand, gravel, and mineral fragments whereas examples of other nonopaque materials include most woods, splinters, and most plastics [7].
TREATMENT & PROGNOSIS
Management of reported cases in the literature usually involves surgical removal of the fish bone, along with either percutaneous or surgical drainage of the abscess [1, 2]. Successful medical management of the hepatic abscess has been reported in two cases, with the fish bone left in the patient [3, 4]. Percutaneous transhepatic removal of the fishbone has only been reported once previously [5]. As the hepatic abscess itself is often drained percutaneously, it would make sense to use the same approach and tract to attempt retrieval of the fish bone under ultrasound and fluoroscopic guidance. In this case, successful removal was performed using an endomyocardial biopsy forceps, and post procedure CT within the interventional suite helped to confirm that the entire fish bone had been removed.
The treatment of pyogenic liver abscess per se (not secondary to foreign body migration) remains controversial, and options include antimicrobial therapy, percutaneous drainage, and open surgery. A treatment algorithm suggested that antimicrobial monotherapy can be attempted for patients with liver abscesses < 5.0 cm and for liver abscesses ≥ 5.0 cm, percutaneous drainage is generally recommended as the first-line treatment. Surgical drainage is usually considered in patients with multiloculated hepatic abscesses, associated biliary pathology or abscess rupture [3].
DIFFERENTIAL DIAGNOSIS
History is crucial in determining the etiology of liver abscess. A pyogenic abscess can occur through 5 major routes. The biliary route is usually secondary to ascending cholangitis and obstruction which is commonly due to choledocholithiasis. The portal vein route is due to conditions such as diverticulitis, appendicitis, proctitis and inflammatory bowel disease. Infection can also spread via the hepatic artery from causes such as bacterial endocarditis, pneumonitis, and osteomyelitis. Direct extension as the etiology is also possible from conditions such as perforated gastric or duodenal ulcer, subphrenic abscess, and pyelonephritis. Traumatic causes may be from blunt or penetrating injuries, surgery or as demonstrated in this case, a migrated foreign body.
Differential diagnosis of liver abscess includes hepatic metastases, amebic abscess, hepatic hydatid cyst and cystadenocarcinoma. However, these conditions can usually be distinguished from liver abscess secondary to foreign body migration with the presence of a radiopaque object in an abscess or inflammatory mass. Other imaging signs such as wall thickening, surrounding soft tissue stranding, and extraluminal air may be associated with visceral perforation by foreign bodies on CT.
TEACHING POINT
In the case of a hepatic abscess complicating fish bone migration from the gastrointestinal tract, image-guided percutaneous removal of the fish bone is a feasible alternative to surgical removal, particularly if the patient is considered to be at high surgical risk.
Table 1.
Summary table for liver abscess secondary to migrated foreign body.
| Etiology | Liver abscess secondary to migrated foreign body. |
| Incidence | Rare; less than 20 cases reported. |
| Gender ratio | No specific sex predilection. |
| Age predilection | No specific age predilection. |
| Risk factors | Elongated or sharp foreign body. |
| Treatment | Open surgery, percutaneous transhepatic removal. |
| Prognosis | Variable from recovery to death. |
| Imaging findings | The hyperdense foreign body within abscess in the liver commonly detected using CT. |
Table 2.
Differential diagnosis table for liver abscess.
| Ultrasound | CT | MRI | |
|---|---|---|---|
| Hepatic metastases | May appear hypoechoic, hyperechoic, target appearance, cystic or calcified (markedly echogenic with acoustic shadowing) | May appear isodense, hypodense or hyperdense. Hypovascular metastases may have low attenuation center with peripheral rim enhancement whilst hypervascular metastases are hyperdense in late arterial phase. |
T1W- hypointense (melanoma metastases hyperintense due to melanin) T2W- hyperintense |
| Hepatic amebic abscess | Round/oval sharply defined hypoechoic mass | Round/oval hypodense mass. Unilocular or multilocular with peripheral rim enhancement. |
T1W- hypointense T2W- hyperintense |
| Hepatic hydatid cyst | Predominately anechoic cyst with echogenic debris. Can be multiseptated with daughter cysts and echogenic material between cysts. | Uni or multilocular well-defined cysts. Contain multiple peripheral “daughter” cysts of lower density than “mother” cyst. Curvilinear ring-like calcification of pericyst wall. Enhancement of cyst wall and septa. |
T1W- Pericyst-hypointense (fibrous content). “Mother” cyst-intermediate signal (hydatid matrix). T2W- Pericyst-hypointense (fibrous content). “Mother” cyst-hyperintense. |
| Biliary cystadenocarcinoma | Large, well-defined, multiloculated, anechoic mass. Echogenic septa. May have a mural or septal calcification and fluid levels. | Large, well-defined, homogeneous, hypodense, water-density mass. Mural or septal calcification. Enhancement of internal septa and papillary excrescences. |
T1W- variable signal depending on fluid content. Hyperintense (mucoid or hemorrhagic). Hypointense (serous fluid). T2W- Hyperintense (serous fluid). Hypointense (mucoid fluid). |
ABBREVIATIONS
- CT
Computed Tomography
- F
French
- PA
Posterior Anterior
REFERENCES
- 1.Masoodi I, Alsayari K, Al Mohaimeed K, Ahmad S, Almtawa A, Alomair A, Alqutub A, Khan S. Fishbone migration: An unusual cause of liver abscess. BMJ Case Rep. 2012 Mar;8:2012. doi: 10.1136/bcr.09.2011.4838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang H, Liu OQ, Ai XB, Zhu DQ, Liu JL, Wang A, Gong FY, Hu C. Recurrent upper quadrant pain: a fish bone secondary to gastric perforation and liver abscess. Case Rep Gastroenterol. 2011 Sep;5(3):663–6. doi: 10.1159/000335211. Epub 2011 Dec 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng CT, Htoo A, Tan SY. Fish bone-induced hepatic abscess: medical treatment. Singapore Med J. 2011;52(3):e56. [PubMed] [Google Scholar]
- 4.Yang CY, Kao JH, Liu KL, Chen SJ. Medical treatment of fish bone-related liver abscess. Clin Infect Dis. 2005 Dec 1;41(11):1689–90. doi: 10.1086/498034. [DOI] [PubMed] [Google Scholar]
- 5.Horii K, Yamazaki O, Matsuyama M, Higaki I, Kawai S, Sakaue Y. Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today. 1999;29(9):922–6. doi: 10.1007/BF02482788. [DOI] [PubMed] [Google Scholar]
- 6.Laterre PF, Dangoisse C. Tracking the foreign body, a rare cause of hepatic abscess. BMC Gastroenterol. 2014;14:167. doi: 10.1186/1471-230X-14-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunter TB, Taljanovic MS. Foreign bodies. Radiographics. 2003 May-Jun;23(3):731–57. doi: 10.1148/rg.233025137. [DOI] [PubMed] [Google Scholar]