Abstract
Septic arthritis of the knee is a potentially life-threatening condition and can be associated with many late complications. The key of success of management of septic arthritis of the knee joint is early aggressive treatment of surgical debridement and decompression and antibiotic therapy. In adults, arthroscopic drainage with synovectomy is the treatment of choice in septic arthritis of the knee, with lower rates of infectious recurrence than needle aspiration and better functional results than open surgery. Repeated arthroscopic debridement and drainage is needed in case of delayed treatment with an advanced arthroscopic stage of the infection, early unfavorable course, or multiresistant germ. In these situations, synovectomy should be as complete as possible to maximize the reduction of the bacterial burden and avoid the need of further debridement. The purpose of this Technical Note is to describe the details of complete arthroscopic synovectomy of the knee joint. This includes 2 circles of circumferential synovectomy. One circle is in the axial plane and includes the intercondylar notch, anterior, posterior, medial, and lateral compartments. The other circle is in the coronal plane and includes the supra-patellar pouch, medial and lateral recesses, and the anterior compartment.
Septic arthritis of the knee is a potentially life-threatening condition and can associate with many late complications, including osteomyelitis, osteonecrosis, joint degeneration, joint instability, arthrofibrosis and ankylosis, shortening or deformity, and thereby an unsatisfactory functional recovery.1, 2, 3, 4
Gächter5 has classified septic arthritis into 4 stages. Stage 1 disease includes opacity of joint fluid, redness of the synovial membrane with possible petechial bleeding, and no radiologic alterations. Stage 2 disease includes severe inflammation, fibrinous deposition, pus, and no radiologic alterations. Stage 3 disease can have thickening of the synovial membrane, compartment formation (“sponge-like” arthroscopic view, especially in the suprapatellar pouch), and no radiologic alterations. Stage 4 disease includes aggressive pannus with infiltration of the cartilage, possibly undermining the cartilage and radiologic signs of subchondral osteolysis, possible osseous erosions, and cysts.5
The key of success of management of septic arthritis of the knee joint is early aggressive treatment of surgical debridement and decompression and antibiotic therapy.4, 6, 7 The choice of joint drainage technique is controversial between needle aspiration, arthrotomy, or arthroscopy.4 In adults, arthroscopic drainage with synovectomy is the treatment of choice in septic arthritis of the knee, with lower rates of infectious recurrence than needle aspiration and better functional results than open surgery.8
Arthroscopy offers significant advantages over arthrotomy because the magnified view in arthroscopy leads to better visibility of gutters and areas not visible by open arthrotomy, and the assessment of joints is better. The high flow of normal saline in close cavity of the joint creates increased intra-articular pressure and distention of joints, resulting in thorough lavage and dislodgement of any necrotic material or pus in the inaccessible areas of joints. The duration of intravenous antibiotics and the hospital stay required is shorter. The hyaline cartilage of joint does not get exposed to the air.2 The blood loss and postoperative scarring is also significantly lesser than arthrotomy. The less postoperative pain allows early mobilization of patients.2, 4, 9, 10, 11
Repeated arthroscopic debridement and drainage is needed in case of delayed treatment with advanced arthroscopic stage of the infection, early unfavorable course, or multidrug-resistant germ.1, 6, 11, 12, 13, 14 In these situations, synovectomy should be as complete as possible to maximize the reduction of the bacterial burden and avoid the need of further debridement.13 Open arthrotomy has been recommended in cases of persistent infections after repeated arthroscopic joint surgery.7 Classic anterior knee arthroscopy does not allow easy access to the posterior recesses.15 The purpose of this Technical Note is to describe the details of complete arthroscopic synovectomy of the knee joint. It is indicated in septic arthritis of the knee recalcitrant to repeated arthroscopic debridement and bacteria-specific antibiotic therapy. The presence of compromised tissue, such as the avascular graft or the presence of hardware (e.g., total knee arthroplasty), promote biofilm formation by pathogens, and may preclude infection control. Initial aggressive treatment of complete arthroscopic synovectomy is indicated to prevent graft or prosthesis failure.15, 16 Contraindications of this technique include presence of Baker cyst, presence of extra-articular abscess, and lack of expertise. The presence of Baker cyst in septic arthritis of the knee joint elicits many problems during arthroscopic surgery, including microbial seeding of the cyst or rupture of the cyst, and spreading of infection to the surrounding tissues (Table 1).17
Table 1.
Indications and Contraindications of Complete Arthroscopic Synovectomy in Management of Recalcitrant Septic Arthritis of the Knee Joint
| Indications | Contraindications |
|---|---|
| 1. Septic arthritis of the knee recalcitrant to repeated arthroscopic debridement and bacteria-specific antibiotic therapy | 1. Septic arthritis of the knee joint in presence of Baker cyst |
| 2. Septic arthritis of the knee in the presence of compromised tissue, such as the avascular graft or the presence of hardware, e.g., total knee arthroplasty | 2. Presence of extra-articular abscess |
| 3. Lack of expertise |
Technique
Preoperative Assessment and Patient Positioning
Preoperative magnetic resonance imaging is sometimes useful to identify the areas of collection inside the knee joint (Fig 1) and exclude the periarticular and intraosseous abscess.18
Fig 1.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. Sagittal plane magnetic resonance imaging of the knee shows effusion of the posterior compartment, with the distended posterior capsule (PC) abutting the popliteal artery (PA).
The patient is in supine position. A thigh tourniquet is applied to provide a bloodless operative field. A 4.0-mm 30° arthroscope (Dyonics; Smith & Nephew, Andover, MA) is used for this procedure.
Portal Placement
Six portals are used for complete synovectomy of the knee joint. The posterolateral portal19, 20 is located at the lateral joint line, just anterior to the biceps femoris tendon. The lateral portal is at the lateral joint line, just anterior to the lateral collateral ligament. The anterolateral portal is at the lateral joint line, 1 cm lateral to the lateral border of the patellar tendon. The anteromedial portal is at the medial joint line, 1 cm medial to the medial border of the patellar tendon. The superolateral portal is at the intersection point between the superior and lateral borders of the patella. The posteromedial portal19, 20 is located at the posteromedial corner of the knee joint and is established by inside-out (Wissinger rod) technique.
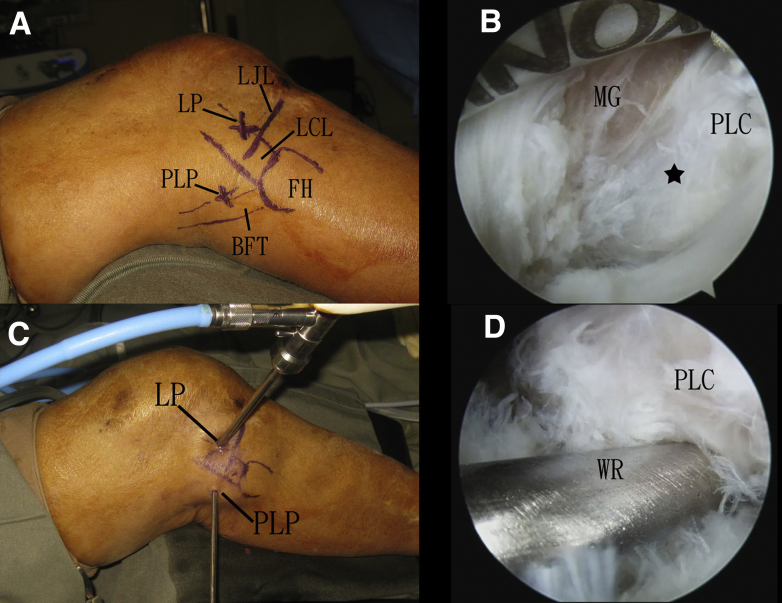
Establishment of Posterior Portals via Posterolateral Knee Endoscopy
Posterolateral knee endoscopy is performed with the posterolateral and lateral portals. Five-millimeter longitudinal incisions are made at the portals. The subcutaneous tissue is bluntly dissected to the joint capsule. The lateral portal is the viewing portal, and the posterolateral portal is the working portal. The dissection should not be posterior to the biceps femoris tendon to avoid injury to the common peroneal nerve. The medial head of the gastrocnemius is identified and the posterolateral capsule of the knee joint can be seen anterior to the gastrocnemius. The posterolateral capsule is perforated by the tip of a hemostat. The entry to the knee joint can be confirmed by flow-out of turbid joint fluid and extrusion of inflamed synovium. This is the posterolateral capsular portal. A 4.0-mm Wissinger rod (Dyonics, Smith & Nephew) is inserted into the posterolateral capsular portal via the posterolateral skin portal (Fig 2). An arthroscope cannula is inserted into the posterolateral portal along the rod. The rod is removed and a 4.0-mm 30° arthroscope is inserted into the cannula. The entry into the posterior knee compartment is confirmed arthroscopically. The arthroscope is removed and a trocar is inserted into the cannula. The cannula trocar is advanced medially along the lateral and medial femoral condyles and the posteromedial capsule is penetrated. A 5-mm incision is made at the tip of the trocar, and the posteromedial portal is created.
Fig 2.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) Posterolateral knee endoscopy is performed with the posterolateral (PLP) and lateral (LP) portals. (B) The lateral portal is the viewing portal, and the posterolateral portal is the working portal. The dissection should not be posterior to the biceps femoris tendon to avoid injury to the common peroneal nerve. The medial head of the gastrocnemius (MG) is identified and the posterolateral capsule (PLC) of the knee joint can be seen anterior to the gastrocnemius. The star indicates the point of posterolateral capsular portal. (C) A 4.0-mm Wissinger rod into the posterolateral skin portal. (D) The Wissinger rod (WR) passes through the posterolateral capsular portal. (BFT, biceps femoris tendon; FH, fibular head; LCL, lateral collateral ligament; LJL, lateral joint line.)
Arthroscopic Synovectomy of Posterior Compartment
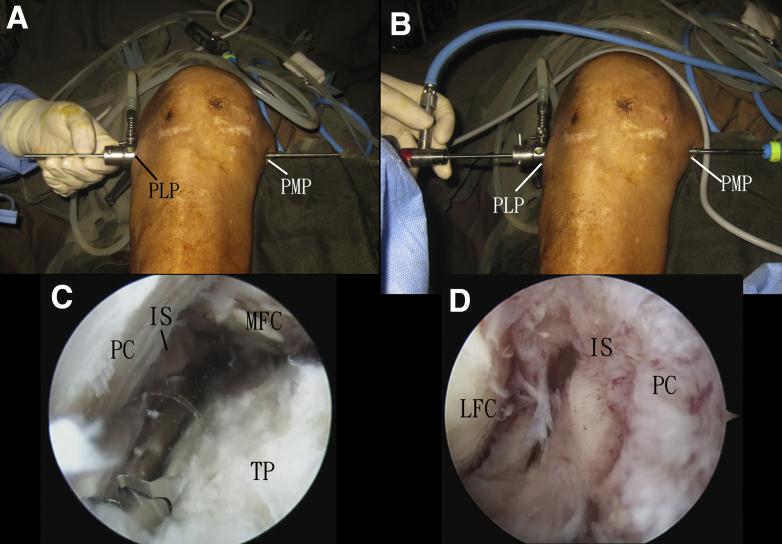
The cannula trocar passes through both the posterolateral and posteromedial portals. The trocar is removed and the arthroscopic shaver (Dyonics; Smith & Nephew) is inserted halfway into the cannula via the posteromedial portal. The trocar is kept in position, and the cannula is withdrawn and incorporated with the arthroscope. This maneuver can ensure that both the arthroscope and the shaver are inside the posterior compartment. The septum between the posteromedial and posterolateral compartments is carefully resected, with the shaver starting just behind the posterior cruciate ligament.20 After creation of this trans-septal portal, the posteromedial compartment can be well seen with the posterolateral portal as the viewing portal. The inflamed synovium, damaged cartilage, and posterior horn of the medial meniscus are resected with the shaver. After completion of debridement of the posteromedial compartment, the arthroscope is advanced medially and exits the posteromedial portal. The arthroscope is removed and the cannula is kept in situ. The Wissinger rod is inserted into the cannula. The cannula is removed and inserted along the rod via the posteromedial portal. The cannula passes through both the posteromedial and posterolateral portals and the rod is removed. The shaver is inserted half way into the cannula via the posterolateral portal. The shaver is kept in position and the cannula is withdrawn and incorporated into the arthroscope. The posteromedial portal is then the viewing portal, and debridement of the posterolateral compartment is performed with the shaver via the posterolateral portal (Fig 3). The posterior capsule should not be perforated during the debridement.
Fig 3.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) Wissinger rod technique for switching the position of the arthroscope cannula. The rod passes through both the posterolateral (PLP) and posteromedial (PMP) portals. The cannula is inserted along the rod via the posterolateral portal so that the posterolateral portal will become the viewing portal. (B) The cannula passes through both the posterolateral (PLP) and posteromedial (PMP) portals. The arthroscopic shaver is then inserted half-way into the cannula via the posteromedial portal. The trocar is kept in position and the cannula is withdrawn and incorporated with the arthroscope. This maneuver can ensure that both the arthroscope and the shaver are inside the posterior compartment. (C) The posterolateral portal is the viewing portal and posteromedial portal is the working portal, and the posteromedial compartment is debrided. (D) The posteromedial portal is the viewing portal, and the posterolateral compartment is assessed. (IS, inflamed synovium; LFC, lateral femoral condyle; MFC, medial femoral condyle; PC, posterior capsule; TP, tibial plateau.)
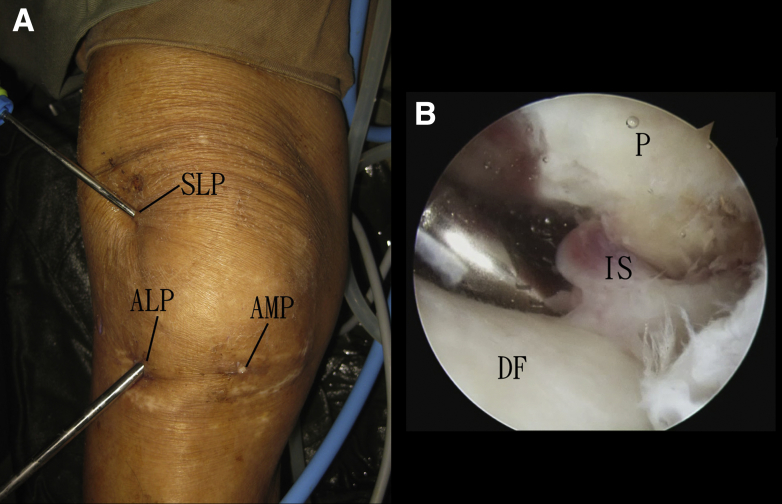
Arthroscopic Synovectomy of the Suprapatellar Pouch
Both the anterolateral and anteromedial portals serve as the viewing portals. Debridement of the suprapatellar pouch via the anterolateral and anteromedial portals will be hindered by the patella, especially during debridement close to the superior pole of the patella. This can be overcome when the superolateral portal is used as the working portal. Complete synovectomy of the suprapatellar pouch can be achieved with the shaver via the superolateral portal (Fig 4).
Fig 4.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) The anterolateral portal (ALP) is the viewing portal, and debridement of the suprapatellar pouch is performed with the arthroscopic shaver via the superolateral portal (SLP). (B) arthroscopic view shows resection of the inflamed synovium (IS) of the supra-patellar pouch. (AMP, anteromedial portal; DF, distal femur; P, patella.)
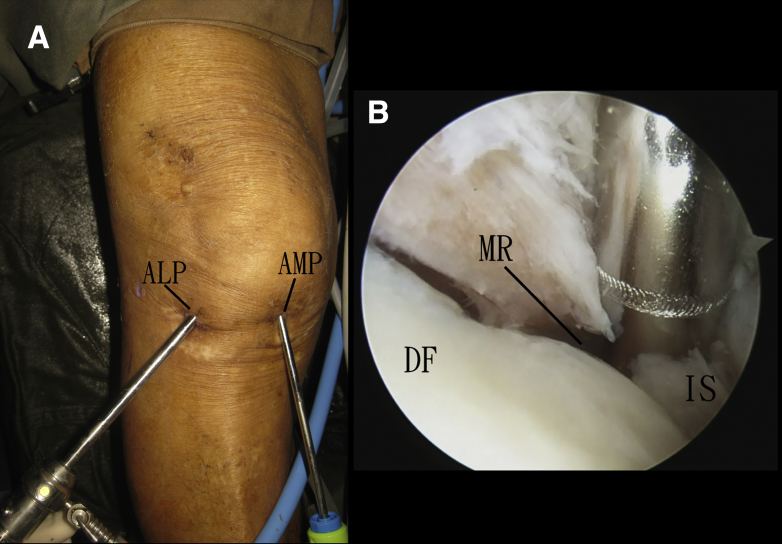
Arthroscopic Synovectomy of the Medial Recess
The medial recess is a tight space between the medial femoral condyle and the medial collateral ligament. The anterolateral portal is the viewing portal. Synovectomy of the medial recess is performed with the shaver via the anteromedial portal (Fig 5). It is important not to injure the medial collateral ligament, especially its femoral insertion.
Fig 5.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) The anterolateral portal (ALP) is the viewing portal and the anteromedial portal (AMP) is the working portal. (B) Synovectomy of the medial recess (MR) is performed with the arthroscopic shaver via the anteromedial portal. (DF, distal femur; IS, inflamed synovium.)
Arthroscopic Synovectomy of the Medial Compartment
The anterolateral portal is the viewing portal. The anteromedial and the posteromedial portals are the working portals. The inflamed synovium and damaged cartilage is resected. The space underneath the medial meniscus should also be examined and any inflamed synovium at this space should also be resected (Fig 6).
Fig 6.
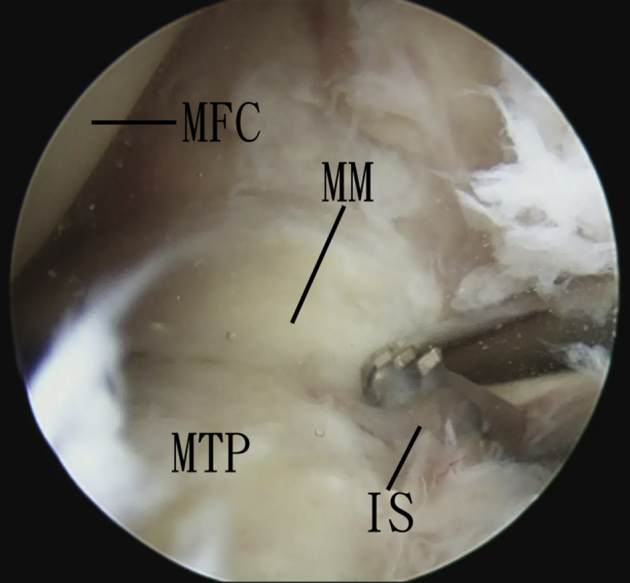
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The inflamed synovium (IS) underneath the medial meniscus (MM) is resected. (MFC, medial femoral condyle; MTP, medial tibial plateau.)
Arthroscopic Synovectomy of the Intercondylar Notch
The anteromedial and anterolateral portals are interchangeable as the viewing and working portals. The inflamed synovium at the notch and surrounding the cruciate ligaments are resected (Fig 7). Loose bony fragments are removed. Any damaged parts of the cruciate ligaments are also resected.
Fig 7.
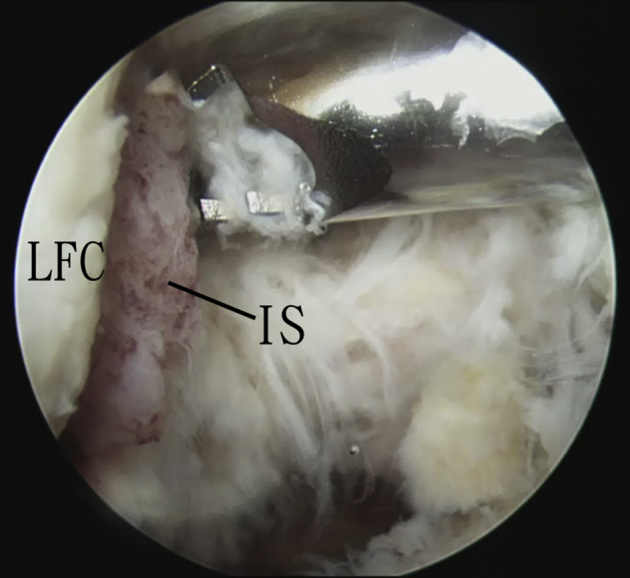
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. The anterolateral portal is the viewing portal. The anteromedial portal is the working portal. The inflamed synovium (IS) of the intercondylar notch is resected. (LFC, lateral femoral condyle.)
Arthroscopic Synovectomy of the Anterior Compartment
The arthroscopic view is turned from the intercondylar notch to the anterior capsule. Inflamed synovium of the anterior capsule is resected (Fig 8). The anteromedial and anterolateral portals are again interchangeable as the viewing and working portals.
Fig 8.
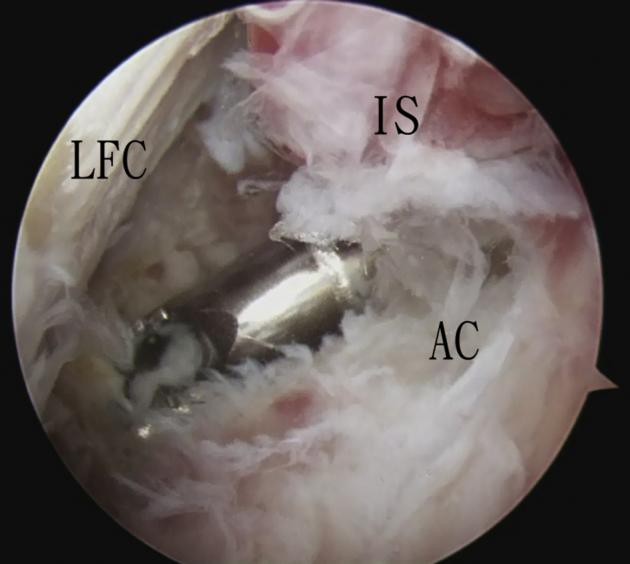
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The inflamed synovium (IS) of the anterior compartment is resected. (AC, anterior capsule; LFC, lateral femoral condyle.)
Arthroscopic Synovectomy of the Lateral Compartment
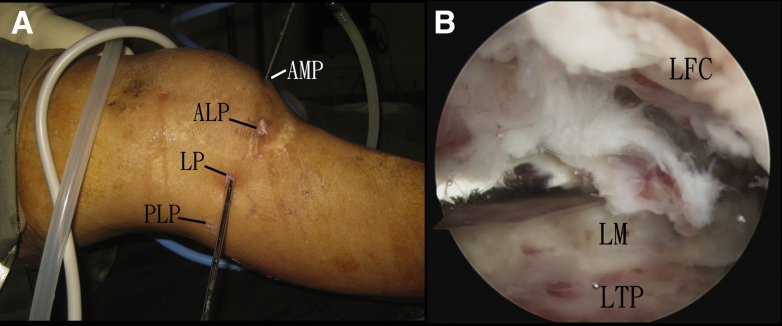
The anteromedial portal is the viewing portal. The anterolateral, lateral, and posterolateral portals are working portals. The inflamed synovium (including those invading the surface of the lateral meniscus) and damaged cartilage is resected. The space underneath the lateral meniscus should also be examined, and any inflamed synovium at this space should also be resected (Fig 9).
Fig 9.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) The anteromedial portal (AMP) is the viewing portal, and the lateral portal (LP) is the working portal. (B) The lateral compartment is debrided. (ALP, anterolateral portal; LFC, lateral femoral condyle; LM, lateral meniscus; LTP, lateral tibial plateau; PLP, posterolateral portal.)
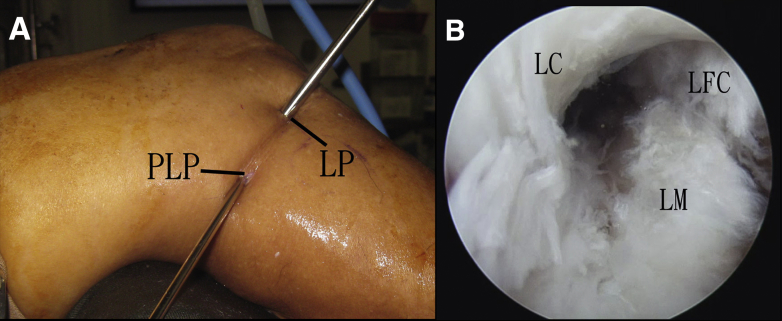
Arthroscopic Synovectomy of the Lateral Recess
The lateral recess is a tight space between the lateral femoral condyle and the lateral collateral ligament. The lateral portal is the viewing portal. Synovectomy of the lateral recess is performed with the shaver via the posterolateral portal (Fig 10). It is important not to injure the lateral collateral ligament, especially its femoral insertion.
Fig 10.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) The lateral portal (LP) is the viewing portal, and the posterolateral portal (PLP) is the working portal. (B) arthroscopic view of the lateral recess after synovectomy. (LC, lateral capsule; LFC, lateral femoral condyle; LM, lateral meniscus.)
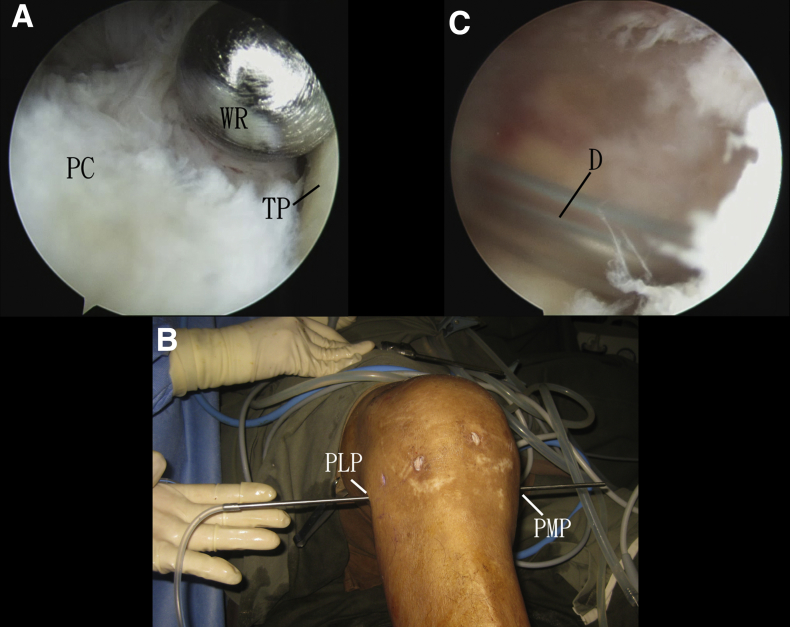
Insertion of a Drain Into the Posterior Compartment
Posterolateral portal is the viewing portal. The Wissinger rod is inserted into the posterior compartment via the posteromedial portal. The arthroscope is partially withdrawn from the cannula. The Wissinger rod is inserted into the cannula under arthroscopic guidance. The cannula is then removed and the rod passes through both the posteromedial and posterolateral portals. A 4-mm drain is incorporated into the lateral end of the rod, and the rod is withdrawn medially. This maneuver brings the drain into the posterior compartment of the knee joint, which is the dependent part of the joint when the patient lies down (Fig 11, Video 1, Table 2).
Fig 11.
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. (A) The posterolateral portal is the viewing portal. The Wissinger rod (WR) is inserted into the posterior compartment via the posteromedial portal. (B) The rod passes through both the posteromedial (PMP) and posterolateral (PLP) portals. A 4-mm drain is incorporated into the lateral end of the rod, and the rod is withdrawn medially. (C) The anteromedial portal is the viewing portal. The drain (D) lies in the posterior compartment of the knee joint, which is the dependent part of the joint when the patient lies down. (PC, posterior capsule; TP, tibial plateau.)
Table 2.
Pearls and Pitfalls of Correction of Complete Arthroscopic Synovectomy in Management of Recalcitrant Septic Arthritis of the Knee Joint
| Pearls | Pitfalls |
|---|---|
| 1. Posterolateral capsular portal should be created under endoscopic guidance. | 1. Instrumentation posterior to the biceps femoris tendon should be avoided. |
| 2. Superolateral portal is an effective working portal for synovectomy of the suprapatellar pouch. | 2. The posterior knee capsule should not be perforated. |
| 3. The medial and lateral recesses should be debrided. | 3. The femoral origins of the medial and lateral collateral ligaments should be preserved during debridement of the recesses. |
| 4. The spaces deep to the menisci should be debrided. | |
| 5. The drain can be put in the posterior knee compartment under arthroscopic guidance. |
Discussion
The arthroscopic complete synovectomy of the knee joint includes 2 circles of circumferential synovectomy. One circle is in the axial plane and includes the intercondylar notch and the anterior, posterior, medial, and lateral compartments. The other circle is in the coronal plane and includes the suprapatellar pouch, the medial and lateral recesses, and the anterior compartment. The posterior compartment is difficult to access via the anterior knee arthroscopy. Incorporation of the posterior knee arthroscopy in this technique allows direct access and debridement of the posterior compartment. It also allows arthroscopically guided placement of the drain to the posterior compartment. It can achieve better drainage of the joint because it is in the most dependent part of the joint when the patient is in supine position. Creation of the posterolateral portal via the posterolateral knee endoscopy allows accurate placement of the capsular portal. The common peroneal nerve is protected by the biceps femoris tendon in this procedure. Although other parts of the knee joint are readily approached via anterior knee arthroscopy, several areas can be missed during arthroscopic assessment. The anterior capsule between the anteromedial and anterolateral portals may not be well seen through these 2 portals, especially when a 30° arthroscope is used. Moreover, the medial and lateral recesses are tightly bound by the collateral ligaments, and inflamed synovium in these areas can be missed. Finally, inflamed synovium can present underneath the menisci, and synovectomy should also be performed at these areas.
The advantages of this arthroscopic technique include complete synovectomy, better visibility of gutters and areas not visible by open arthrotomy, and less postoperative pain allowing early mobilization. The potential risks of this technique include injury to the popliteal artery, common peroneal nerve, saphenous nerve and its branches, and femoral origins of the collateral ligaments (Table 3). The posterior knee arthroscopy is technically demanding and should be reserved for the experienced knee arthroscopists.
Table 3.
Advantages and Risks of Complete Arthroscopic Synovectomy in Management of Recalcitrant Septic Arthritis of the Knee Joint
| Advantages | Risks |
|---|---|
| 1. Complete synovectomy | 1. Injury to the popliteal artery |
| 2. Better visibility of gutters and areas not visible by open arthrotomy | 2. Injury to the common peroneal nerve |
| 3. Less postoperative pain allowing early mobilization | 3. Injury to the saphenous nerve and its branches |
| 4. Injury to the femoral origins of the collateral ligaments |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. The posterolateral capsular portalis is established via posterolateral knee endoscopy. The posteromedial portal is established by Wissinger rod technique. Debridement of the posterior compartment is performed via the posteromedial and posterolateral portals, which are interchangeable as the viewing and working portals. The next step is synovectomy of the suprapatellar pouch with the anteromedial and anterolateral portals as the viewing portals and the superolateral portal as the working portal. The third step is debridement of the medial recess with the anterolateral portal as the viewing portal and the anteromedial portal as the working portal. The fourth step is debridement of the lateral compartment. This is followed by debridement of the intercondylar notch and the anterior compartment. Then, the lateral compartment and lateral recess are debrided. After completion of debridement, a drain is inserted into the posterior compartment under arthroscopic guidance.
References
- 1.Vispo Seara J.L., Barthel T., Schmitz H., Eulert J. Arthroscopic treatment of septic joints: Prognostic factors. Arch Orthop Trauma Surg. 2002;122:204–211. doi: 10.1007/s00402-001-0386-z. [DOI] [PubMed] [Google Scholar]
- 2.Shukla A., Beniwal S.K., Sinha S. Outcome of arthroscopic drainage and debridement with continuous suction irrigation technique in acute septic arthritis. J Clin Orthop Trauma. 2014;5:1–5. doi: 10.1016/j.jcot.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunter J.G., Gross J.M., Dahl J.D., Amsdell S.L., Gorczyca J.T. Risk factors for failure of a single surgical debridement in adults with acute septic arthritis. J Bone Joint Surg Am. 2015;97:558–564. doi: 10.2106/JBJS.N.00593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wirtz D.C., Marth M., Miltner O., Schneider U., Zilkens K.W. Septic arthritis of the knee in adults: treatment by arthroscopy or arthrotomy. Int Orthop (SICOT) 2001;25:239–241. doi: 10.1007/s002640100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gächter A. The joint infection. Inform Arzt. 1985;6:35–43. [Google Scholar]
- 6.Yanmis I., Ozkan H., Koca K., Kilincoglu V., Bek D., Tunay S. The relation between the arthroscopic findings and functional outcomes in patients with septic arthritis of the knee joint, treated with arthroscopic debridement and irrigation. Acta Orthop Traumatol Turc. 2011;45:94–99. doi: 10.3944/AOTT.2011.2258. [DOI] [PubMed] [Google Scholar]
- 7.Ateschrang A., Albrecht D., Schröter S., Hirt B., Weise K., Dolderer J.H. Septic arthritis of the knee: Presentation of a novel irrigation-suction system tested in a cadaver study. BMC Musculoskelet Disord. 2011;12:180. doi: 10.1186/1471-2474-12-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agout C., Lakhal W., Fournier J., de Bodman C., Bonnard C. Arthroscopic treatment of septic arthritis of the knee in children. Orthop Traumatol Surg Res. 2015;101:S333–S336. doi: 10.1016/j.otsr.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Peres L.R., Marchitto R.O., Pereira G.S., Yoshino F.S., de Castro Fernandes M., Matsumoto M.H. Arthrotomy versus arthroscopy in the treatment of septic arthritis of the knee in adults: A randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2016;24:3155–3162. doi: 10.1007/s00167-015-3918-8. [DOI] [PubMed] [Google Scholar]
- 10.Bohler C., Dragana M., Puchner S., Windhager R., Holinka J. Treatment of septic arthritis of the knee: A comparison between arthroscopy and arthrotomy. Knee Surg Sports Traumatol Arthrosc. 2016;24:3147–3154. doi: 10.1007/s00167-015-3659-8. [DOI] [PubMed] [Google Scholar]
- 11.Bussiere F., Beaufils P. Role of arthroscopy in the treatment of pyogenic arthritis of the knee in adults. Report of 16 cases. Rev Chir Orthop Reparatrice Appar Mot. 1999;85:803–810. [in French] [PubMed] [Google Scholar]
- 12.Stutz G., Kuster M.S., Kleinstück F., Gächter A. Arthroscopic management of septic arthritis: stages of infection and results. Knee Surg Sports Traumatol Arthrosc. 2000;8:270–274. doi: 10.1007/s001670000129. [DOI] [PubMed] [Google Scholar]
- 13.Aïm F., Delambre J., Bauer T., Hardy P. Efficacy of arthroscopic treatment for resolving infection in septic arthritis of native joints. Orthop Traumatol Surg Res. 2015;101:61–64. doi: 10.1016/j.otsr.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Dave O.H., Patel K.A., Andersen C.R., Carmichael K.D. Surgical procedures needed to eradicate infection in knee septic arthritis. Orthopedics. 2016;39:50–54. doi: 10.3928/01477447-20151222-05. [DOI] [PubMed] [Google Scholar]
- 15.Ilahi O.A., Al-Habbal G.A., Bocell J.R., Tullos H.S., Huo M.H. Arthroscopic debridement of acute periprosthetic septic arthritis of the knee. Arthroscopy. 2005;21:303–306. doi: 10.1016/j.arthro.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Abdel-Aziz A., Radwan Y.A., Rizk A. Multiple arthroscopic debridement and graft retention in septic knee arthritis after ACL reconstruction: A prospective case–control study. Int Orthop. 2014;38:73–82. doi: 10.1007/s00264-013-2123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eichinger J.K., Bluman E.M., Sides S.D., Arrington E.D. Surgical management of septic arthritis of the knee with a coexistent popliteal cyst. Arthroscopy. 2009;25:696–700. doi: 10.1016/j.arthro.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 18.Bancroft L.W. MR imaging of infectious processes of the knee. Radiol Clin North Am. 2007;45:931–941. doi: 10.1016/j.rcl.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Pace J.L., Wahl C.J. Arthroscopy of the posterior knee compartments: Neurovascular anatomic relationships during arthroscopic transverse capsulotomy. Arthroscopy. 2010;26:637–642. doi: 10.1016/j.arthro.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Lee Y.S., Ahn J.H., Min B.H., Nha K.W. Arthroscopic loose body removal and cyst decompression using a posterior trans-septal portal in the blind spot during knee arthroscopy—Technical report. Knee. 2011;18:55–58. doi: 10.1016/j.knee.2010.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the right knee joint. The patient is in supine position with the legs spread. The posterolateral capsular portalis is established via posterolateral knee endoscopy. The posteromedial portal is established by Wissinger rod technique. Debridement of the posterior compartment is performed via the posteromedial and posterolateral portals, which are interchangeable as the viewing and working portals. The next step is synovectomy of the suprapatellar pouch with the anteromedial and anterolateral portals as the viewing portals and the superolateral portal as the working portal. The third step is debridement of the medial recess with the anterolateral portal as the viewing portal and the anteromedial portal as the working portal. The fourth step is debridement of the lateral compartment. This is followed by debridement of the intercondylar notch and the anterior compartment. Then, the lateral compartment and lateral recess are debrided. After completion of debridement, a drain is inserted into the posterior compartment under arthroscopic guidance.