Abstract
Objective
Increasing evidence suggests that chronic exposure to unfair treatment or day-to-day discrimination increases risk for poor health, but data on biological stress mechanisms are limited. This study examined chronic experiences of unfair treatment in relation to allostatic load (AL), a multisystem index of biological dysregulation.
Method
Data are from a sample of 233 African-American adults (37–85 years; 64% women). Perceptions of everyday unfair treatment were measured by questionnaire. An AL index was computed as the sum of 7 separate physiological system risk indices (cardiovascular regulation, lipid, glucose, inflammation, sympathetic nervous system, parasympathetic nervous system, hypothalamic pituitary adrenal axis).
Results
Adjusting for sociodemographics, medication use, smoking status, alcohol consumption, depressive symptoms, lifetime discrimination, and global perceived stress, everyday mistreatment was associated with higher AL.
Conclusions
The results add to a growing literature on the effects of chronic bias and discrimination by demonstrating how such experiences are instantiated in downstream physiological systems.
Keywords: allostatic load, biological processes, chronic discrimination, unfair treatment
A substantial body of evidence implicates self-reported discrimination or unfair treatment as important determinants of mental and physical health. Summative reviews of the literature provide consistent evidence that repeated exposure to unfair treatment disrupts goal pursuit, undermines psychological well-being, and contributes to broad-based morbidity and mortality (Krieger, 1999; Lewis, Cogburn, & Williams, 2015; Schmitt, Branscombe, Postmes, & Garcia, 2014; Williams & Mohammed, 2009). Whereas lifetime unfair treatment refers to acute major experiences of discrimination across a variety of life domains such as being unfairly denied a promotion or being unfairly prevented from moving into a neighborhood, everyday unfair treatment captures the range of chronic day-to-day experiences of discrimination such as being followed around in stores or being treated with less courtesy or respect than others (Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009).
Relative to White Americans, African Americans consistently report more experiences of unfair treatment and discrimination at every level of age, gender, and socioeconomic status (Barnes, Mendes De Leon, Wilson, et al., 2004; Forman, Williams, & Jackson, 1997; Kessler, Mickelson, & Williams, 1999; Lewis, Yang, Jacobs, & Fitchett, 2012). Moreover, growing evidence suggests that coping with chronic, everyday mistreatment triggers a cascade of physiological responses that over time may place demands on the body’s ability to effectively respond to challenges (Lewis et al., 2015; Mays, Cochran, & Barnes, 2007). The concept of allostatic load (AL), introduced by McEwen and Stellar (1993), reflects the cumulative “wear and tear” of chronic stress on the body. According to the allostatic framework (McEwen & Seeman, 1999), chronic stressors can cause dysregulation of interrelated physiological systems, which if prolonged, may ultimately lead to disease. Such dysregulation is characterized by elevated (or reduced) physiological activity across multiple regulatory systems, including the sympathetic nervous system (SNS), hypothalamic–pituitary–adrenal (HPA) axis, immune system, and cardiovascular and metabolic processes. Across studies, higher AL has been shown to predict incident cardiovascular disease, decline in cognitive and physical functioning, and all-cause mortality (Karlamangla, Singer, McEwen, Rowe, & Seeman, 2002; Seeman, McEwen, Rowe, & Singer, 2001; Seeman, Singer, Rowe, Horwitz, & McEwen, 1997).
Although many studies have investigated the relationship between reported experiences of unfair treatment and health among African Americans (for a review, see Mays et al., 2007; Pieterse, Todd, Neville, & Carter, 2012; Williams & Mohammed, 2009), few have related unfair treatment to multisystem functioning. Rather, most studies have focused on individual physiological indicators or preclinical endpoints of poor health. For example, several studies have found unfair treatment and discrimination to be associated with dysregulated blood pressure (Beatty & Matthews, 2009; Smart Richman, Pek, Pascoe, & Bauer, 2010), excess adiposity (Hunte, 2011), coronary artery calcification (Lewis et al., 2006; Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003), and inflammation (Lewis, Aiello, Leurgans, Kelly, & Barnes, 2010). Given that the effects of chronic stress are typically nonspecific (Segerstrom & Miller, 2004), such single system studies cannot adequately capture the cumulative impact of exposure to everyday unfair treatment. In comparison, a multisystems approach is consistent with evidence that many people, particularly at later ages, suffer from multiple, co-occurring chronic conditions which are likely to contribute to increased risks for morbidity and mortality (Yancik et al., 2007). For example, previous analyses from the MacArthur Studies of Successful Aging have shown that although the overall summary measure of AL significantly predicts risk for major health outcomes, none of the individual components is a significant independent risk factor (Seeman et al., 2004; Seeman, Singer, Ryff, Dienberg Love, & Levy-Storms, 2002). This accumulative process is also captured in life-course risk models (Lynch & Smith, 2005) and theories of weathering (Geronimus, Hicken, Keene, & Bound, 2006), which posit that greater exposure to chronic stress accumulates to increase vulnerability to disease-related outcomes in later life. To our knowledge, only two studies have examined the effects of unfair treatment on AL among African Americans. In a longitudinal study involving 331 rural African American adolescents, Brody and colleagues (2014) observed a prospective effect of discriminatory treatment on higher AL levels. Using a community-based sample of middle-aged African American women, Upchurch et al. (2015) found that chronic exposure to everyday discrimination was predictive of higher AL levels. Thus, with rare exception, studies examining links between unfair treatment and multisystem biological dysregulation (e.g., AL) in African Americans is critically lacking.
The current study adds to our understanding of the health disparities that adversely affect African Americans in at least three important ways. First, this study builds on prior work on AL (Gruenewald et al., 2012; Seeman, Epel, Gruenewald, Karlamangla, & McEwen, 2010) by examining the relationship between chronic exposure to everyday mistreatment and AL in a sample of middle-aged African Americans. Midlife may be an important point in the life span for examining these processes, because it ushers in a period of markedly rising risk for acute and chronic illness (House, Lantz, & Herd, 2005; Karlamangla, Singer, & Seeman, 2006). As such, there is a strong need to explore biological stress mechanisms among middle-aged African Americans, a population particularly at risk for a broad-spectrum of stress-related disorders, including diabetes, cardiovascular disease, hypertension, and obesity (Geronimus et al., 2006; Krieger, 1990; Mays et al., 2007). Second, the study considers the important role of confounding variables. Lewis et al. (2015) recently called for more systematic research on the role of depressive symptoms as a potential confounder in studies of discrimination and health. A number of prior studies with African Americans have documented strong and consistent associations between reports of everyday discrimination and elevated depressive symptoms (e.g., Brown et al., 2000; Soto, Dawson-Andoh, & BeLue, 2011). Additionally, both major depression and elevated depressive symptoms have been implicated in higher AL (McEwen, 2000, 2003). Thus, we also sought to evaluate the contribution of depressive symptoms as a possible confounder of the association between everyday unfair treatment and AL. Finally, the study has the potential to shed light on the extent to which unfair treatment independently predicts AL after adjustments for other sources of stress, such as major discriminatory experiences (Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009) and global perceived stress (Brody et al., 2014; Upchurch et al., 2015). Accordingly, we tested the hypothesis that independent of major discrimination and perceived stress, exposure to day-to-day experiences of mistreatment would have incremental effects on AL.
Method
Data and Analytic Sample
Data are from a sample of African Americans (34–85 years, n = 592) collected in Milwaukee County, Wisconsin, as part of the Midlife in the United States (MIDUS) study (Brim, Ryff, & Kessler, 2004). MIDUS is a probability sample of noninstitutionalized, English-speaking adults. Respondents were first interviewed in 1995–1996 and followed up in in 2004–2006. To oversample African Americans in the second wave of the MIDUS data collection, a supplemental sample of African Americans was drawn in the Milwaukee area. Using a stratified sampling frame, the Milwaukee data consisted of U.S. census tracts in which at least 40% of residents were African American. Inclusionary criteria required that respondents self-identified as Black/African American, lived in a noninstitutionalized setting, were able to speak English with sufficient literacy to complete a self-administered questionnaire, and were healthy enough to complete a 40-min interview. Data were collected via a computer-assisted personal interview protocol and with subsequent, mailed self-administered questionnaires. Response rate for the Milwaukee sample was 70.7% for the in-person interview and 70.3% for the mail-back questionnaire. Additional details about the sampling procedure are described elsewhere (Ryff et al., 2008a, 2008b).
The analytic sample for the current study consisted of 233 African American adults (64% women) aged 37–85 years at MIDUS II who participated in a biomarker substudy (Dienberg Love, Seeman, Weinstein, & Ryff, 2010). Biomarker data were collected during an overnight visit at a regional medical center in Madison, Wisconsin, between 2004 and 2009. Study participants provided a complete medical history, underwent a physical examination, and provided blood, urine, and saliva samples, along with cardiovascular and heart rate variability measurements. Fasting blood was collected at 07:00 (before caffeine or nicotine consumption). Urine was collected during a 12-hr (19:00 h to 07:00) overnight stay (for details, see Dienberg Love et al., 2010). Data collection for the MIDUS, Milwaukee, and biomarker studies were approved by Institutional Review Boards at each participating site, and all participants provided informed consent.
Measures
Biomarker measurement
A comprehensive range of biological and anthropometric measurements representing seven physiological systems were collected during the study visit. Measures of (a) cardiovascular functioning included resting systolic and diastolic blood pressure and resting pulse. Indicators of (b) lipid metabolism included high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, body mass index, and waist-to-hip ratio. Levels of (c) glycosylated hemoglobin, fasting glucose, and the homeostasis model of insulin resistance, served as measures of glucose metabolism. Measures of (d) chronic inflammation included plasma C-reactive protein, fibrinogen, and serum measures of interleukin-6 and the soluble adhesion molecules E-selectin and intracelleular adhesion molecule-1. Changes in peripheral autonomic nervous system activity were assessed with measures of sympathetic and parasympathetic activation. Indicators of (e) SNS activity included overnight urinary measures of epinephrine and norepinephrine. Measures of (f) parasympathetic nervous system activity included the following heart rate variability parameters: low- and high-frequency spectral power, the standard deviation of heartbeat-to-heartbeat intervals, and the root mean square of successive differences. Indicators of (7) HPA activity included an overnight urinary measure of the hormone cortisol and a serum measure of the hormone dehydroepiandrosterone sulfate. Additional details about laboratory assays and heart-rate variability measurement are available elsewhere (Crowley et al., 2011; Dienberg Love et al., 2010).
Allostatic load
An AL score, designed to summarize dysregulation across multiple physiological systems, was computed as the sum of seven system-level (cardiovascular, lipid, glucose metabolism, inflammation, SNS, parasympathetic nervous system, HPA) risk scores. Following previous work, system risk scores were computed as the proportion of individual biomarker indicators for each system for which participant values fell into high-risk quartile ranges (Gruenewald et al., 2012). High risk was defined as the upper or lower quartile depending on whether high or low values of the biomarker typically confer greater risk for poor health. System risk scores could range from 0 to 1 (indicating 0–100% of system biomarkers in high-risk range) and were computed for individuals with values on at least half of the system biomarkers. An AL score (possible range: 0–7) was computed for participants with information on at least six of the seven systems.
Everyday unfair treatment
Everyday unfair treatment was assessed with the nine-item Detroit Area Study Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997). Respondents reported on the frequency of various forms of interpersonal unfair treatment in their daily lives. Items included being treated with less courtesy or respect than others; receiving poorer service than others at restaurants or stores; being called names, insulted, threatened, or harassed; having people act afraid of the respondent; having people act as if the respondent was dishonest, not smart, or not as good as they were. The frequency of each type of mistreatment was assessed using a 4-point scale (1 = never; 2 = rarely; 3 = sometimes; 4 = often). Responses were averaged to form an Everyday Unfair Treatment Index (Cronbach’s alpha’s for the nine-item index was .91). Participants who responded either “sometimes” or “often” to at least one of the nine items on the Unfair Treatment scale were asked to respond to an additional item inquiring about the reason(s) for their experience(s). Response categories included race, ethnicity, gender, age, income level, language, physical appearance, sexual orientation, and other. In accord with prior MIDUS II study findings (e.g., Fuller-Rowell, Doan, & Eccles, 2012; Kessler et al., 1999), the majority (81.1%) of African-American respondents in the current study reported race as a reason for at least one of the unfair treatment events they experienced.
Lifetime unfair treatment
Reports of lifetime occurrences of unfair treatment were assessed across 11 settings that included academics (discouraged from continuing education, denied scholarship), employment (not hired or promoted, fired), financial services (denied a ban loan, prevented from renting or buying a home, given inferior service), and experiences of social hostility (forced out of a neighborhood, hassled by the police; Kessler et al., 1999). Respondents indicated how many times they experienced each event “because of such things as your race, ethnicity, gender, age, religion, physical appearance, sexual orientation, or other characteristics.” Due to high skewness in the data, we calculated a summary index of lifetime mistreatment by recoding responses into three categories (none, one to two instances, three or more instances), similar to previous MIDUS studies of discrimination (Friedman, Williams, Singer, & Ryff, 2009; Mays & Cochran, 2001).
Covariates
Sociodemographic, medical, health behavior, and psychosocial covariates were selected based on their potential for either confounding or mediating the associations between unfair treatment and AL. Sociodemographic covariates included age (in years), gender, and educational attainment (continuous, using categories 1 = no school/some grade school [1–6] to 12 = PhD (Doctor of Philosophy), EdD (Doctor of Education), MD (Doctor of Medicine), DDS (Doctor of Dental Surgery), LLD (Doctor of Law), JD (Juris Doctor), or other professional degree). Medical covariates included use of antihypertensive, cholesterol lowering, steroid, and antidepressant medications to lower clinical risk. Health behavior covariates included smoking status (coded as nonsmoker, ex-smoker, or current smoker) and the presence of alcohol problems, as assessed by a five-item modified version of the Michigan Alcohol Screening Test (Selzer, 1971). Responses on the Michigan Alcohol Screening Test were summed (α = .60) and then dichotomized (0 = no alcohol problems, 1 = otherwise).
Psychosocial covariates included depression symptomatology and global perceived stress. Depressive symptoms were assessed via the General Distress Depressive Symptoms (12 items) subscale from the Mood and Anxiety Questionnaire (Clark & Watson, 1991). The items assess distress symptoms commonly associated with depression (e.g., “felt discouraged”; “felt pessimistic about the future”). Responses are based on a 5-point Likert-like scale (1 = not at all to 5 = extremely). Cronbach’s alpha for the 12-item General Distress Depressive Symptoms was .90. Perceived stress was measured with the 10-item Perceived Stress Scale. The items assess stress in the past month (e.g., “felt unable to control important things in your life”; “felt difficulties were piling up so high that I couldn’t overcome them”). Responses are based on a 5-point Likert-like scale (1 = never to 5 = very often). Cronbach’s alpha for the 10-item Perceived Stress Scale was .69 in the current data.
Statistical Analyses
Regression analyses were used to examine the association between everyday unfair treatment and AL, adjusting for the effects of covariates described above. Multiple imputation procedures were used to impute missing values on covariates (Graham, 2009; Royston, 2005). The relationship between everyday unfair treatment and AL was examined using a series of multivariate-adjusted models. Five models were fitted in all. In Model 1, AL scores were regressed on unfair treatment, omitting any covariates. This model provides a comparison of results obtained using multiple predictors to those obtained from simpler, univariate analyses in which the outcome is regressed separately on each predictor variable (Cohen, West, & Aiken, 2003, p. 425). Model 2 included adjustments for sociodemographic factors (age, gender, education). Model 3 added medical covariates (antihypertensive, cholesterol lowering, steroid, and antidepressant medications). Health behaviors (smoking, alcohol problems) were added in Model 4, and psychosocial factors (depression, life mistreatment, and perceived stress) were included in Model 5. Finally, interactions of unfair treatment with age, gender, and education were tested. All results are presented as unstandardized regression coefficients (B) with 95% confidence intervals (CIs) based on pooled estimates from five imputed data sets. Values of R2 are based on the application of Rubin’s (1987) rules after Fisher’s Z transformation following Harel (2009).
Results
Descriptive Statistics
Descriptive data are presented in Tables 1 and 2. Respondents were on average 53.6 years (SD = 10.4) of age and 67% female at the second MIDUS wave. The majority of respondents (54.5%) had some college education or at least a bachelor’s degree. Approximately half of the sample used blood pressure medications. On average, level of AL was moderate in the sample (M = 1.91, SD = 1.01; observed range 0 – 4.90; possible range of 0–7). Moreover, the seven system-level scores that contribute to AL had means between 0.17 (SD = 0.31) and 0.43 (SD = 0.38), and were not highly correlated with each other; pairwise correlation coefficients ranged from −0.10 to 0.37 (median = 0.10). Pairwise correlations between the seven system-level risk scores and overall AL index ranged from 0.29 to 0.56. Finally, in the current data, the correlation between the two measures of unfair treatment (i.e., everyday and lifetime) was moderate (r =.44).
Table 1.
Sample Characteristics
| Characteristic | n | % or Range | M | SD |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age (years) | 233 | 37–85 | 53.59 | 10.41 |
| Male | 76 | 32.6% | ||
| Female | 157 | 67.4% | ||
| Education (%) | 233 | |||
| ≤High school | 106 | 45.5% | ||
| Some college | 81 | 34.8% | ||
| ≥University University degree | 46 | 19.7% | ||
| Health behaviors | ||||
| Smoking | 189 | |||
| Nonsmoker | 56 | 29.6% | ||
| Ex-smoker | 67 | 35.4% | ||
| Current smoker | 66 | 34.9% | ||
| Alcohol problems | 231 | 0–1 | .08 | .28 |
| Medication use (% yes) | ||||
| Blood pressure | 109 | 46.8% | ||
| Cholesterol | 48 | 20.6% | ||
| Steroid | 24 | 10.3% | ||
| Depression | 16 | 6.9% | ||
| Mental health | ||||
| Anxiety | 230 | 12.00–52.00 | 20.07 | 7.99 |
| Depression | 229 | 11.00–40.00 | 17.34 | 6.41 |
| Lifetime mistreatment | ||||
| Never | 55 | 23.6% | ||
| 1–2 instances | 62 | 26.6% | ||
| 3 or more | 116 | 49.8% | ||
| Everyday mistreatment | 230 | 9.00–32.00 | 14.97 | 6.58 |
Table 2.
Descriptive Statistics, Cut Points, and Correlations Between System-Level and Allostatic Load Scores
| Biomarkers by system | M | SD | Cut points | r |
|---|---|---|---|---|
| Cardiovascular regulation | .40** | |||
| Resting SBP (mm Hg) | 133.86 | 20.47 | ≥145.00 | |
| Resting DBP (mm Hg) | 79.11 | 11.75 | ≥86.00 | |
| Resting heart rate (beats per min) | 73.53 | 10.87 | ≥80.30 | |
| Lipid metabolism | .47** | |||
| BMI (kg/m2) | 32.47 | 7.84 | ≥37.38 | |
| Waist-to-hip circumference ratio | .89 | .09 | ≥.96 | |
| Serum triglycerides (mg/dL) | 111.04 | 66.77 | ≥132.00 | |
| HDL cholesterol (mg/dL) | 59.16 | 19.23 | ≤45.00 | |
| LDL cholesterol (mg/dL) | 101.20 | 35.54 | ≥121.36 | |
| Glucose metabolism | .56** | |||
| Blood glycated hemoglobin (HbA1c) | 6.14 | .64 | ≥6.49 | |
| Fasting blood glucose (mg/dL) | 101.27 | 15.43 | ≥107.00 | |
| Homeostasis model insulin resistance | 3.73 | 2.68 | ≥5.24 | |
| Inflammation | .54** | |||
| Serum C-reactive protein (mg/L) | 2.89 | 2.48 | ≥4.12 | |
| Serum IL6 (ng/mL) | 3.41 | 1.99 | ≥4.70 | |
| Fibrinogen (mg/dL) | 384.09 | 87.78 | ≥439.00 | |
| E-selectin (ng/mL) | 50.45 | 25.93 | ≥63.72 | |
| ICAM-1 (ng/mL) | 266.58 | 138.09 | ≥356.14 | |
| Sympathetic nervous system | .41** | |||
| Urine epinephrine (mg/g of creatine) | 1.59 | 1.08 | ≥1.86 | |
| Urine norepinephrine (mg/g of creatine) | 24.64 | 11.90 | ≥29.83 | |
| Parasympathetic nervous system | .48** | |||
| R–R interval standard deviation (ms) | 38.15 | 17.61 | ≤24.95 | |
| Root mean square successive differences (ms) | 27.39 | 16.01 | ≤16.32 | |
| Low-frequency spectral power (ms2) | 353.59 | 291.89 | ≤116.25 | |
| High-frequency spectral power (ms2) | 291.07 | 248.17 | ≤99.80 | |
| Hypothalamic-pituitary-adrenal axis | .29** | |||
| Urine cortisol (mg/g of creatine) | 10.31 | 8.18 | ≥14.00 | |
| Blood DHEA-S (μg/dL) | 99.66 | 68.47 | ≥137.00 | |
| AL | 1.91 | 1.01 |
Note. r = pairwise correlations between the system-level risk scores and allostatic load (AL) summary index and are based on pooled estimates from multiple imputation; SBP = systolic blood pressure; DBP = diastolic blood pressure; BMI = body mass index; HDL = high-density lipoprotein; LDL = low-density lipoprotein; IL6 = interleukin-6; ICAM-1 = intracelleular adhesion molecule-1; R–R = heartrate-to-heartrate; DHEA-S = dehydroepiandrosterone sulfate.
p <.01.
Everyday Unfair Treatment and Allostatic Load
Associations between unfair treatment and AL were highly consistent across all five models. Results of regression analyses are summarized in Table 3. The unadjusted model (Model 1) indicated that unfair treatment was associated with higher levels of AL (B = .022, 95% CI [0.003, 0.04]). The adjusted base model (Model 2) indicated that net of sociodemographic factors, unfair treatment predicted significantly higher levels of AL (B = .028, 95% CI [0.01, 0.05]). This is illustrated in the solid bars in Figure 1. Adjusted for age, gender, race, and education, AL scores were on average 8% greater in the highest compared with the lowest tertile of exposure to everyday mistreatment. Adding medical covariates (Model 3), health behaviors (Model 4), and psychosocial factors (Model 5) to the base model did not alter these results. The association between unfair treatment and AL was attenuated (reduced by 14–32%), but remained significant across all models (see Table 3). The final model accounted for approximately 26% of the variance in AL scores.
Table 3.
Parameter Estimates From Unadjusted and Adjusted Multiple Regression Models Predicting Allostatic Load
|
B [95% CI]
|
|||||
|---|---|---|---|---|---|
| Predictor | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 |
| Everyday mistreatment | .022 [.003, .040]* | .028 [.010, .046]** | .023 [.006, .040]** | .024 [.007, .043]** | .019 [.001, .038]* |
| Sociodemographic | |||||
| Age | .023 [.012, .033]** | .009 [−.002, .002] | .010 [−.005, .020] | .011 [−.001, .022] | |
| Gender (reference = male) | −.259 [−.494, −.025]* | −.185 [−.408, .037] | −.208 [−.604, −.106] | −.188 [−.418, .041] | |
| Education | .058 [−.101, .016]** | .054 [−.094, −.014]** | .048 [−.089, .005] | .048 [−.091, .006]* | |
| Medication use | |||||
| Blood pressure | −.703 [−.940, −.465]** | −.692 [−.929, −.455]** | −.680 [−.919, −.442]** | ||
| Cholesterol | −.055 [−.320, .210] | −.061 [−.325, .204] | −.072 [−.338, .194] | ||
| Corticosteroid | .042 [−.297, .380] | .040 [−.300, .379] | .016 [−.326, .359] | ||
| Depression | −.618 [−.989, −.247]** | −.617 [−.991, −.244]** | −.604 [−.987, −.222]** | ||
| Health behaviors | |||||
| Smoking | .057 [−.100, .214] | .047 [−.116, .209] | |||
| Alcohol use | .279 [−.123, .681] | .269 [−.136, .674] | |||
| Psychosocial factors | |||||
| Depressive symptoms | −.001 [−.018, .015] | ||||
| Lifetime mistreatment | .018 [.016, .053] | ||||
| Global perceived stress | .008 [−.013, .028] | ||||
| R2 | .018 | .111 | .249 | .257 | .262 |
| F for change in R2 | 5.37* | 10.271** | 13.427** | 1.599 | .512 |
Note. CI = confidence interval. Model parameters are based on pooled estimates from multiple imputation.
p <.05.
p <.01.
Figure 1.
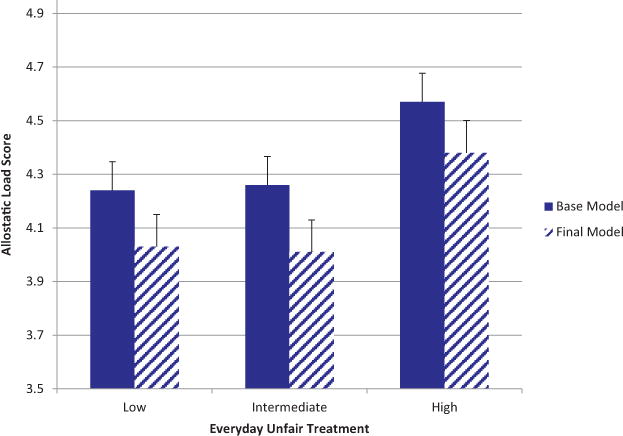
Bar graph shows mean levels of allostatic load in low, intermediate, and high unfair treatment tertiles. Base model (solid bars) adjusted for age, gender, and education. Final model (hatched bars) represent additional adjustment for medication use, smoking status, alcohol problems, depression scores, lifetime unfair treatment, and global perceived stress. Error bars are standard error of the mean. See the online article for the color version of this figure.
Supplemental Analyses
Parallel analyses tested for possible interactions between everyday unfair treatment and major sociodemographic factors. There was no evidence that the adjusted association between mistreatment scores and AL varied as a function of age (B = 0.001, 95% CI [−0.001, 0.002]), gender (B = 0.001, 95% CI [−0.037, 0.035]), or education (B = − 0.002, 95% CI [−0.009, 0.005]). Examination of unfair treatment by individual system risk scores indicated that greater everyday unfair treatment was associated with higher scores on each of the AL subsystem risk scores, with the exception of SNS and glucose metabolism. Moreover, and further supporting the robustness of our results, a sensitivity analysis with an alternatively scored AL measure that used fewer biomarker indicators (original 10-item formulation used in Seeman et al., 1997) yielded similar results. The adjusted association between unfair treatment and AL scores remained significant (B = 0.04, 95% CI [0.007, 0.070]). Finally, attributions to racial/ethnic discrimination for experiences of unfair treatment were not associated with AL scores (B = 0.003, 95% CI [−0.280, 0.286]). Thus, in the current study, everyday unfair treatment overall, regardless of the attributed cause, was associated with higher AL among African-American adults.
Discussion
Extensive evidence suggests that chronic exposure to unfair treatment increases risk for premature morbidity and mortality (Lewis et al., 2015; Mays et al., 2007; Williams & Mohammed, 2009). Findings from the current study provide support for the hypothesis that among African Americans the experience of everyday mistreatment contributes to greater overall physiological dysregulation. Whereas previous work has focused on individual physiological risk measures (e.g., Beatty & Matthews, 2009; Troxel et al., 2003), this study extends prior work by examining the association between everyday unfair treatment and a multisystem index of cumulative, biological “wear and tear” or AL.
Our findings also provide additional empirical footing for the distinction between major and day-to-day forms of mistreatment and their unique effects on AL. Although there was some shared variance between the two types of constructs, there was independent covariation to justify the inclusion of both types of measures in the current study (Kessler et al., 1999; Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009). The larger literature on stress assessment points to important distinctions between major life events and daily stressors. Studies in this area have typically found that ambient strains or “daily hassles” account for a greater portion of the variance in symptomatology than is explained by the occurrence of major life events (DeLongis, Coyne, Dakof, Folkman, & Lazarus, 1982; Kanner, Coyne, Schaefer, & Lazarus, 1981). There has been little effort, however, to develop psychological hypotheses that could capture the relative impact of major versus everyday forms of mistreatment on physical health outcomes within African American samples (Mays et al., 2007; Ong, Fuller-Rowell, & Burrow, 2009; Williams et al., 1997). Taken together, these findings build upon existing literature by pointing to the significance of chronic everyday discrimination in the lives of Africans Americans and by illustrating how social conditions external to the individual “get under the skin” to affect later health and disease outcomes.
An additional aim was to examine the role of depressive symptoms, major discrimination, and global perceived stress as potential confounders of the association between unfair treatment and AL. Previous reviews have pointed to the importance of controlling for the effects of depressive symptoms (Lewis et al., 2015; Pascoe & Smart Richman, 2009) and global perceived stress (Brody et al., 2014; Upchurch et al., 2015) in studies of discrimination and physical health. Notably, we found the effect of unfair treatment on AL remained significant after including depressive symptoms, lifetime mistreatment, and perceived stress in the model, indicating that although statistical adjustment for these confounding factors attenuated the association between everyday mistreatment and AL, they do not completely explain the effect in the current data. Thus, it is likely that other behavioral or physiological pathways are at play. Given research demonstrating that unfair treatment is associated with lower levels of health care seeking (for a review, see Williams & Mohammed, 2009) and access to health care explains a significant amount of variance in ethnic/racial disparities in health (Blendon, Aiken, Freeman, & Corey, 1989; Williams & Rucker, 2000), future studies should examine the role of medical care and health care seeking behaviors (e.g., interactions with health care providers, adherence to treatment advice) as potential pathways linking everyday unfair treatment and AL among African Americans.
Finally, although the majority African Americans in the current study attributed experiences of unfair treatment to race, attributions of mistreatment due to race were not associated with AL scores. These findings are consistent with studies showing that irrespective of attribution, experiences of unfair treatment may lead to negative health outcomes (De Vogli, Ferrie, Chandola, Kivimaki, & Marmot, 2007; Troxel et al., 2003). For example, Lewis and colleagues (2006) found that everyday mistreatment in general, rather than racial/ethnic discrimination, was positively associated with coronary artery calcification among African American women. Similarly, in a study of African American women, Roberts, Vines, Kaufman, and James (2008) observed nonracial attributions of mistreatment were more strongly associated with hypertensive status than were racial attributions. Because African Americans consistently report higher levels of overall discrimination compared with Whites (Schulz et al., 2000; Williams et al., 1997), it is possible that their vulnerability to the health consequences of mistreatment may be a function of the frequency of exposure rather than the attribution of the type of discrimination experienced (Beatty & Matthews, 2009). Research on “intersectionalities” (Lewis et al., 2015) suggests that occupying multiple disadvantaged statuses (e.g., African American and female) may shape both the experiences and consequences of everyday unfair treatment. It is noteworthy that this work has largely focused on subjective, self-reported health. Thus, studies examining the impact of multiple group identities on objective physical health outcomes represent an important priority for future research.
By contrast, Brody et al. (2014) found that high and stable levels of discrimination due to race was associated with higher AL across adolescence. The discrepancy in findings may be partly explained by differences in the measure of unfair treatment and age cohort sampled. Specifically, the approach to measuring discrimination used in the Brody et al. (2014) study was to ask explicitly about experiences with racial/ethnic discrimination. In contrast, the Everyday Discrimination Scale (Williams et al., 1997) used in the current research inquires about discriminatory experiences as a form of unfair treatment more broadly and then follows-up with a question regarding attribution after a general response has been endorsed. As reviewed in Lewis et al. (2015), these two approaches make different assumptions about how best to query respondents and, thus, have unique limitations and strengths. For example, although it is not possible to ascertain how many of the participants reported mistreatment due exclusively to racial/ethnic discrimination using the Everyday Discrimination Scale, a strength of the scale is that it does not require respondents to engage in the challenging cognitive task of attributing cause at the same time as they recall and report experiences of discrimination (Williams & Mohammed, 2009). Future research should contrast approaches that ask about recent everyday unfair treatment with those that ask about recent everyday racial and ethnic discrimination (Lewis et al., 2015) and assess their effects on physical health among African Americans.
Our conclusions are necessarily limited by some features of our methods and analyses. First, although we conceptualized unfair treatment as a risk marker for increased AL, in the absence of longitudinal data, it is possible that a reverse association exists whereby high levels of AL contribute to increase reports of everyday unfair treatment. Thus, prospective studies with multiple-wave assessments of unfair treatment and AL are needed to understand the directionality and time-course of these relationships. Longitudinal designs may reveal, for example, whether repeated exposure to everyday mistreatment piles up over time to prospectively influence subsequent AL, in addition to the mechanisms underlying these effects. Second, our measures of unfair treatment were based on self-report and did not include comprehensive assessments of structural or institutional discrimination (e.g., residential segregation, socioeconomic mobility). Third, our study was limited to a relatively small sample of fairly educated African American middle-aged adults, and the findings cannot be assumed to generalize beyond this sociodemographic group. Additional research in this area is warranted.
Despite the study limitations, the findings shed light on the biological underpinnings of chronic exposure to unfair treatment. To our knowledge, the present analysis is among the first to consider the cumulative effects of unfair treatment across a comprehensive 22 biomarker measure of multisystem biological dysregulation (i.e., AL) within a community-based sample of middle-aged African American adults. Additionally, the study adjusts for potential confounding factors (depressive symptoms, major discrimination, global perceived stress) in the association between unfair treatment and AL. Finally, the findings add to increasing evidence suggesting that the exclusive focus on racial and ethnic discrimination should be broadened to include experiences of unfair treatment that are at the intersection of multiple group identities, such as race/ethnicity, religion, gender, income, physical appearance, and age (Lewis et al., 2006, 2013; Roberts et al., 2008; Troxel et al., 2003). Although the mechanisms underlying the observed association have yet to be determined, these findings add to the growing literature linking everyday unfair treatment to key regulatory physiological systems.
Contributor Information
Anthony D. Ong, Department of Human Development, Cornell University and Division of Geriatrics and Palliative Medicine, Weill Cornell Medical College
David R. Williams, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health, Harvard University
Ujuonu Nwizu, Africana Studies and Research Center, Cornell University.
Tara L. Gruenewald, Davis School of Gerontology, University of Southern California
References
- Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older blacks and whites. Journal of Aging and Health. 2004;16:315–337. doi: 10.1177/0898264304264202. http://dx.doi.org/10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]
- Beatty DL, Matthews KA. Unfair treatment and trait anger in relation to nighttime ambulatory blood pressure in African American and White adolescents. Psychosomatic Medicine. 2009;71:813–820. doi: 10.1097/PSY.0b013e3181b3b6f8. http://dx.doi.org/10.1097/PSY.0b013e3181b3b6f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ, Aiken LH, Freeman HE, Corey CR. Access to medical care for black and white Americans. A matter of continuing concern. Journal of the American Medical Association. 1989;261:278–281. http://dx.doi.org/10.1001/jama.1989.03420020132045. [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC, editors. How healthy are we? A national study of well-being at midlife. Chicago, IL: University of Chicago Press; 2004. [Google Scholar]
- Brody GH, Lei MK, Chae DH, Yu T, Kogan SM, Beach SRH. Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Development. 2014;85:989–1002. doi: 10.1111/cdev.12213. http://dx.doi.org/10.1111/cdev.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TN, Williams DR, Jackson JS, Neighbors HW, Torres MM, Sellers SL, Brown KT. “Being black and feeling blue”: The mental health consequences of racial discrimination. Race and Society. 2000;2:117–131. http://dx.doi.org/10.1016/S1090-9524(00)00010-3. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. http://dx.doi.org/10.1037/0021-843X.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cohen J, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Erlbaum Publishers; 2003. [Google Scholar]
- Crowley OV, McKinley PS, Burg MM, Schwartz JE, Ryff CD, Weinstein M, Sloan RP. The interactive effect of change in perceived stress and trait anxiety on vagal recovery from cognitive challenge. International Journal of Psychophysiology. 2011;82:225–232. doi: 10.1016/j.ijpsycho.2011.09.002. http://dx.doi.org/10.1016/j.ijpsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis A, Coyne JC, Dakof G, Folkman S, Lazarus RS. Relationship of daily hassles, uplifts, and major life events to health status. Health Psychology. 1982;1:119–136. http://dx.doi.org/10.1037/0278-6133.1.2.119. [Google Scholar]
- De Vogli R, Ferrie JE, Chandola T, Kivimäki M, Marmot MG. Unfairness and health: Evidence from the Whitehall II Study. Journal of Epidemiology and Community Health. 2007;61:513–518. doi: 10.1136/jech.2006.052563. http://dx.doi.org/10.1136/jech.2006.052563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienberg Love G, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS national study: Protocol, measures, sample, and comparative context. Journal of Aging and Health. 2010;22:1059–1080. doi: 10.1177/0898264310374355. http://dx.doi.org/10.1177/0898264310374355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman TA, Williams DR, Jackson JS. Race, place, and discrimination. Perspectives on Social Problems. 1997;9:231–261. [Google Scholar]
- Friedman EM, Williams DR, Singer BH, Ryff CD. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: The MIDUS study. Brain, Behavior, and Immunity. 2009;23:684–692. doi: 10.1016/j.bbi.2009.01.002. http://dx.doi.org/10.1016/j.bbi.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Doan SN, Eccles JS. Differential effects of perceived discrimination on the diurnal cortisol rhythm of African Americans and Whites. Psychoneuroendocrinology. 2012;37:107–118. doi: 10.1016/j.psyneuen.2011.05.011. http://dx.doi.org/10.1016/j.psyneuen.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. http://dx.doi.org/10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. http://dx.doi.org/10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall C, Koretz B, Seeman TE. History of socioeconomic disadvantage and allostatic load in later life. Social Science & Medicine. 2012;74:75–83. doi: 10.1016/j.socscimed.2011.09.037. http://dx.doi.org/10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harel O. The estimation of R2 and adjusted R2 in incomplete data sets using multiple imputation. Journal of Applied Statistics. 2009;36:1109–1118. http://dx.doi.org/10.1080/02664760802553000. [Google Scholar]
- House JS, Lantz PM, Herd P. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study) The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2005;60:15–26. doi: 10.1093/geronb/60.special_issue_2.s15. http://dx.doi.org/10.1093/geronb/60.Special_Issue_2.S15. [DOI] [PubMed] [Google Scholar]
- Hunte HE. Association between perceived interpersonal everyday discrimination and waist circumference over a 9-year period in the Midlife Development in the United States cohort study. American Journal of Epidemiology and Community Health. 2011;173:1232–1239. doi: 10.1093/aje/kwq463. http://dx.doi.org/10.1093/aje/kwq463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. Journal of Behavioral Medicine. 1981;4:1–39. doi: 10.1007/BF00844845. http://dx.doi.org/10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Singer BH, McEwen BS, Rowe JW, Seeman TE. Allostatic load as a predictor of functional decline. Mac-Arthur studies of successful aging. Journal of Clinical Epidemiology. 2002;55:696–710. doi: 10.1016/s0895-4356(02)00399-2. http://dx.doi.org/10.1016/S0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosomatic Medicine. 2006;68:500–507. doi: 10.1097/01.psy.0000221270.93985.82. http://dx.doi.org/10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. http://dx.doi.org/10.2307/2676349. [PubMed] [Google Scholar]
- Krieger N. Racial and gender discrimination: Risk factors for high blood pressure? Social Science & Medicine. 1990;30:1273–1281. doi: 10.1016/0277-9536(90)90307-e. http://dx.doi.org/10.1016/0277-9536(90)90307-E. [DOI] [PubMed] [Google Scholar]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. http://dx.doi.org/10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. http://dx.doi.org/10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. http://dx.doi.org/10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN Heart Study. Psychosomatic Medicine. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. http://dx.doi.org/10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychology. 2013;32:810–819. doi: 10.1037/a0029938. http://dx.doi.org/10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Yang FM, Jacobs EA, Fitchett G. Racial/ethnic differences in responses to the everyday discrimination scale: A differential item functioning analysis. American Journal of Epidemiology. 2012;175:391–401. doi: 10.1093/aje/kwr287. http://dx.doi.org/10.1093/aje/kwr287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annual Review of Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. http://dx.doi.org/10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- Mays VM, Cochran SD. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health. 2001;91:1869–1876. doi: 10.2105/ajph.91.11.1869. http://dx.doi.org/10.2105/AJPH.91.11.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. http://dx.doi.org/10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–124. doi: 10.1016/S0893-133X(99)00129-3. http://dx.doi.org/10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Mood disorders and allostatic load. Biological Psychiatry. 2003;54:200–207. doi: 10.1016/s0006-3223(03)00177-x. http://dx.doi.org/10.1016/S0006-3223(03)00177-X. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. http://dx.doi.org/10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–2101. http://dx.doi.org/10.1001/archinte.1993.00410180039004. [PubMed] [Google Scholar]
- Ong AD, Fuller-Rowell T, Burrow AL. Racial discrimination and the stress process. Journal of Personality and Social Psychology. 2009;96:1259–1271. doi: 10.1037/a0015335. http://dx.doi.org/10.1037/a0015335. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. http://dx.doi.org/10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse AL, Todd NR, Neville HA, Carter RT. Perceived racism and mental health among Black American adults: A meta-analytic review. Journal of Counseling Psychology. 2012;59:1–9. doi: 10.1037/a0026208. http://dx.doi.org/10.1037/a0026208. [DOI] [PubMed] [Google Scholar]
- Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: The Pitt County Study. American Journal of Epidemiology. 2008;167:624–632. doi: 10.1093/aje/kwm334. http://dx.doi.org/10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values: Update. The Stata Journal. 2005;5:188–201. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987. http://dx.doi.org/10.1002/9780470316696. [Google Scholar]
- Ryff CD, Almeida DM, Ayanian JS, Carr DS, Cleary PD, Coe C, Williams DR. Field report–Midlife development in the United States (MIDUS II): Milwaukee African American sample, 2005–2006. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2008a. [Google Scholar]
- Ryff CD, Almeida DM, Ayanian JS, Carr DS, Cleary PD, Coe C, Williams DR. National Survey of Midlife Development in the United States (MIDUS II), 2004–2006. Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2008b. (ICPSR04652-v6). [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin. 2014;140:921–948. doi: 10.1037/a0035754. http://dx.doi.org/10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Social Science & Medicine. 2000;51:1639–1653. doi: 10.1016/s0277-9536(00)00084-8. http://dx.doi.org/10.1016/S0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, Reuben DB. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Social Science & Medicine. 2004;58:1985–1997. doi: 10.1016/S0277-9536(03)00402-7. http://dx.doi.org/10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS. Socio-economic differentials in peripheral biology: Cumulative allostatic load. Annals of the New York Academy of Sciences. 2010;1186:223–239. doi: 10.1111/j.1749-6632.2009.05341.x. http://dx.doi.org/10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:4770–4775. doi: 10.1073/pnas.081072698. http://dx.doi.org/10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—Allostatic load and its health consequences. MacArthur studies of successful aging. Archives of Internal Medicine. 1997;157:2259–2268. http://dx.doi.org/10.1001/archinte.1997.00440400111013. [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Ryff CD, Dienberg Love G, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosomatic Medicine. 2002;64:395–406. doi: 10.1097/00006842-200205000-00004. http://dx.doi.org/10.1097/00006842-200205000-00004. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130:601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer ML. The Michigan alcoholism screening test: The quest for a new diagnostic instrument. The American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. http://dx.doi.org/10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressure and affective responses to interpersonal stress modeled over 24 hours. Health Psychology. 2010;29:403–411. doi: 10.1037/a0019045. http://dx.doi.org/10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- Soto JA, Dawson-Andoh NA, BeLue R. The relationship between perceived discrimination and generalized anxiety disorder among African Americans, Afro Caribbeans, and non-Hispanic Whites. Journal of Anxiety Disorders. 2011;25:258–265. doi: 10.1016/j.janxdis.2010.09.011. http://dx.doi.org/10.1016/j.janxdis.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. http://dx.doi.org/10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Upchurch DM, Stein J, Greendale GA, Chyu L, Tseng CH, Huang MH, Seeman T. A longitudinal investigation of race, socioeconomic status, and psychological mediators of allostatic load in midlife women: Findings from the study of women’s health across the nation. Psychosomatic Medicine. 2015;77:402–412. doi: 10.1097/PSY.0000000000000175. http://dx.doi.org/10.1097/PSY.0000000000000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. http://dx.doi.org/10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financing Review. 2000;21:75–90. [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. http://dx.doi.org/10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Yancik R, Ershler W, Satariano W, Hazzard W, Cohen HJ, Ferrucci L. Report of the national institute on aging task force on comorbidity. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2007;62:275–280. doi: 10.1093/gerona/62.3.275. http://dx.doi.org/10.1093/gerona/62.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]


