Abstract
Background
Obesity prevalence is disproportionately high among Hispanic children.
Objectives
The Healthy Families Study assessed the efficacy of a culturally-targeted, family-based weight gain prevention intervention for Hispanic immigrant families with children ages 5–7.
Methods
The study used a two-group, cluster-randomized trial design, assigning 136 families (clusters) to the active intervention (weight gain prevention) and 136 families to attention control (oral health). The active intervention included a four-month intensive phase (eight classes) and an eight-month reinforcement phase (monthly mail/telephone contact). Children’s body mass index z-score (BMI-Z) was the primary outcome.
Results
The BMI-Z growth rate of the active intervention group did not differ from the attention control group at short-term follow-up (median 6 months; 168 families, 206 children) or long-term follow-up (median 16 months; 142 families, 169 children). Dose response analyses indicated a slower increase in BMI-Z at short-term among overweight/obese children who attended more intervention classes. Moderate physical activity on weekends increased at short term. Weekend screen time decreased at short term among those attending at least one class session.
Conclusion
Low class attendance likely impacted intention-to-treat results. Future interventions targeting this population should test innovative strategies to maximize intervention engagement to produce and sustain effects on weight gain prevention.
Trial Registration
ClinicalTrials.gov NCT01156402
Keywords: Overweight, Obesity prevention, Cluster-randomized controlled trial, Children, Hispanics
INTRODUCTION
Obesity prevalence for children has been increasing steadily since the 1970s followed by a plateau in recent years, with around one-third of children ages 2–19 being classified as overweight or obese, although severe obesity among children has continued to rise.1 With obesity starting earlier in life, longer duration of obesity across the life span increases risk of obesity-related health conditions at earlier ages, as well as greater economic costs to society.2 Obesity prevalence is higher, increasing more rapidly, and starts at earlier ages among Hispanic children compared to non-Hispanic white children.1,3
Evidence-based recommendations for primary prevention of childhood obesity encourage population-wide approaches for all children regardless of body weight that target both nutrition and physical activity and combine policy/environmental changes with parent education to implement healthy lifestyle changes in the home, particularly for pre-school and elementary-school aged children.4 Numerous systematic reviews have found moderate evidence supporting combined approaches that target both diet and physical activity and for school-based interventions involving policy and environmental changes.5–7 Moreover, the strength of evidence is low regarding the efficacy of family-based intervention strategies implemented in the community and/or the home, due to a small number of studies with largely non-significant effects.5,6,8,9 Nevertheless, the importance of parents and the family environment in influencing children’s weight has been well established.10 Thus, research should continue to explore which intervention strategies can be most effective to prevent excessive weight gain in young children via parents.6,9
Several obesity prevention or treatment interventions that were culturally-targeted for Hispanics have been tested with pre-schoolers and with children in school settings.11–14 However, only a handful of randomized controlled trials have tested family-based obesity prevention interventions in community settings that are culturally targeted for Hispanic children of elementary school ages in the US.15,16 Community engagement, participatory research, use of lay health promoters, and culturally-targeted intervention content have been recommended as strategies to reduce childhood obesity disparities among Hispanics.17,18 In addition, interventions that target Hispanics and/or non-native English speakers should use content that is accessible for persons with low levels of health literacy.19
The Healthy Families Study assessed the efficacy of a family-based weight gain prevention intervention that was culturally-targeted for Hispanic immigrant families with school-aged children in a community setting, using a community-based participatory research (CBPR) approach. This paper reports on the short-term and long-term outcomes of the intervention. The following hypotheses were tested: 1) The active intervention will result in a slower increase in child BMI z-score (primary outcome) compared to the attention control intervention, and 2) The active intervention will result in improvements in secondary outcomes for children compared to the attention control intervention.
METHODS
Study Design
A detailed description of the trial design and methodology including eligibility criteria, sample size calculation, and recruitment methods has been published elsewhere.20 The study used a two-group cluster randomized controlled trial (RCT) design. Participants were recruited and screened for eligibility from May 2010 to May 2013 in Metropolitan Nashville, Tennessee, USA. One parent or guardian was enrolled per family, and more than one eligible child in each family could be enrolled. Thus, children were clustered within families. Families were randomized to either the active intervention arm focused on weight gain prevention or the attention control intervention arm focused on oral health. The primary outcome was child’s body mass index (kg/m2) z-score (BMI-Z,). Secondary outcomes included absolute BMI, child’s waist circumference, physical activity, screen time, dietary behaviors, and preferences for fruits and vegetables. The Institutional Review Boards of the participating institutions approved the study protocol.
Active Intervention (Treatment)
The Healthy Families active intervention (Familias Saludables Activas, or Active Healthy Families) is a family-based intervention designed to be culturally-targeted for Hispanic families with elementary school aged children, drawing from social cognitive theory, behavioral choice theory, and food preference theory. A detailed description of the CBPR approach used to develop Familias Saludables Activas and the intervention content for both study arms were published previously.20,21
Familias Saludables Activas aimed to increase physical activity, decrease sedentary behavior, and improve healthy eating behaviors through parental modeling and experiential learning for children. Trained lay community health promoters (CHPs) implemented the intervention in a Hispanic community center over 12 months. The intensive four-month phase, consisted of eight 90-minunte bi-weekly group sessions attended by parents and their children. During the eight-month reinforcement phase families were mailed a bi-monthly newsletter reinforcing intervention content. In the alternating months, CHPs called parents to discuss goal-setting progress, motivate, give social support, and answer questions.
Randomization
An independent biostatistician generated the random group allocation for each family using block randomization and a computerized random number generator. The allocation was concealed until after baseline assessments were completed for each recruitment block. The interventions were delivered in person in groups by separate intervention staff, thus it was not possible to mask participants or interventionists to group assignment. The interviewers were masked to group assignment, and intervention staff did not collect measurements on participants after randomization to reduce information bias.
Assessments
Study staff collected baseline assessments at the initial study visit upon parental consent and child assent, prior to randomization. Short-term follow-up assessments were scheduled after completion of the four-month intensive phase. Long-term follow-up scheduling attempts started at the end of the 12-month period post-randomization, including participants who did not complete short-term follow-up. Given that multiple attempts were required to schedule families and follow-up time varied, we analyzed the short-term outcome for follow-up assessments that occurred up to 9.9 months after baseline, and the long-term outcome for follow-up assessments that took place between 10 to 24 months after baseline.
Assessments included questionnaires and anthropometric measures.20 The operationalization of primary and secondary measures used in the present analysis are summarized in Supplemental Table S1. The original study protocol included collection of a food frequency questionnaire to measure dietary intake; however, due to technical problems, these data were not successfully collected on the majority of participants at follow-up.
Statistical Analysis
The hypotheses were tested using intention-to-treat analyses, in which all study participants were analyzed according to the study arms to which they were randomly assigned and the intended full exposure to the corresponding intervention. Linear mixed-effects models with families as cluster and ordinary least square regression with robust standard errors and family clusters were fit for the outcomes. In these models, baseline outcome and length of follow-up time since baseline were included as covariates, in addition to study arm and an interaction term between study arm and follow-up time. The interaction was used to detect the modification effect of the active intervention on the growth rate of the outcome, to account for variation in follow-up time. For secondary outcomes, we fit similar linear models and generalized linear models. For absolute BMI, baseline age and gender of the child were also included as covariates.
In secondary analyses, per protocol analysis was conducted, repeating the same methods as in hypothesis 1 and 2 but excluding families who did not attend any of the group sessions. We tested for a dose response of the proportion of group sessions attended, by adding this variable and its 2-way and 3-way interactions with length of follow-up time and study arm to the models. In addition, analyses were stratified by child’s baseline weight status (see Supplemental Table S1).
No imputation was used for missing data. All statistical tests were two-sided at a 0.05 nominal significance level. Standard diagnostic plots were used to assess model fit. All analyses were carried out using R 3.1.2, including the Hmisc, rms and nlme packages.
RESULTS
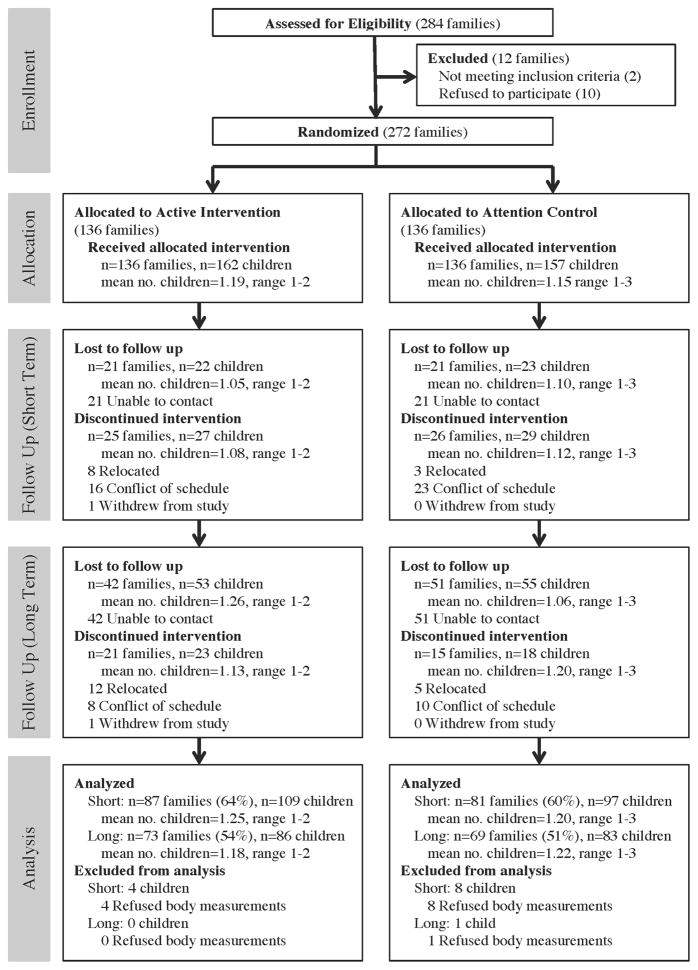
Figure 1 illustrates the flow of study participants. After screening for eligibility, 272 families met criteria and enrolled in the study. After baseline assessments were collected, 136 were families allocated to the active intervention arm and 136 allocated to the attention control arm. There was no known crossover between study arms. For short-term follow-up, 168 families (62%) with 206 children were included in the statistical analyses, along with 142 families (52.3%) with 169 children for long-term follow-up. The mean number of children per family included in analyses was approximately 1.2 for both short-term and long-term follow-up (range 1 to 3).
Figure 1.
Flow Diagram of Study Participants
Participant characteristics and summaries of the baseline outcome measures by study arm for 271 families (excluding one family that withdrew) are presented in Table 1. All enrolled parents were immigrants (three-fourths from Mexico), while 94% of children were born in the U.S. Parents reported a low level of English-speaking ability, education and family income. Half of children reported speaking English and Spanish equally often, and almost one-third spoke mostly Spanish. One-quarter of children were overweight and over one-quarter classified as obese. Among parents, over 40% were overweight and over one-third classified as obese.
Table 1.
Healthy Families Study Baseline Sample Characteristics and Outcomes, Nashville, TN
| Variable | Active Intervention Arm | Attention Control Arm | |
|---|---|---|---|
|
| |||
| N | Median (lower, upper quartiles) or % (N) | Median (lower, upper quartiles) or % (N) | |
| PARENTS | n=135 | n=136 | |
| Parent Age (years) | 264 | 33.0 (28.0, 38.0) | 33.0 (29.0, 36.2) |
| Parent Gender | 271 | ||
| Female | 96% (130) | 93% (126) | |
| Male | 2% (3) | 5% (7) | |
| Other (grandparent or other guardian) | 1% (2) | 2% (3) | |
| Mother Country of Birth | 267 | ||
| Mexico | 74% (98) | 72% (97) | |
| Other Latin American Country | 26% (34) | 28% (38) | |
| Parent English-Speaking Ability | 264 | ||
| Not at all | 12% (16) | 14% (18) | |
| A little | 58% (76) | 59% (79) | |
| Somewhat/Good/Very Good | 29% (39) | 28% (36) | |
| Parent Education | 267 | ||
| High school degree or higher | 36% (47) | 33% (45) | |
| Less than high school degree | 64% (85) | 67% (90) | |
| Monthly Family Income | 264 | ||
| Less than $1,000 | 15% (19) | 22% (29) | |
| $1,000 – $1,999 | 60% (78) | 54% (72) | |
| $2,000 or greater | 25% (32) | 24% (35) | |
| Parent BMI (kg/m2) | 265 | 27.7 (25.1, 32.2) | 28.4 (26.1 31.6) |
| Parent Weight Category | 265 | ||
| Underweight (BMI<18.5) | 0% (0) | 0% (0) | |
| Normal weight (18.5≤BMI<25) | 25% (32) | 19% (26) | |
| Overweight (25≤BMI<30) | 38% (49) | 46% (62) | |
| Obese (BMI≥30) | 38% (49) | 35% (47) | |
| CHILDREN | n=161 | n=157 | |
| Child Age (months) | 318 | 75.1 (66.2, 84.5) | 74.1 (66.6, 82.9) |
| Child Gender | 318 | ||
| Girl | 54% (87) | 50% (78) | |
| Boy | 46% (74) | 50% (79) | |
| Child Country of Birth | 313 | ||
| Mexico | 3% (5) | 6% (9) | |
| Other Latin American Country | 3% (4) | 1% (2) | |
| USA | 94% (149) | 93% (146) | |
| Child Usual Language Spoken | 313 | ||
| Mostly/Only Spanish | 33% (52) | 37% (51) | |
| English/Spanish Equally | 53% (83) | 55% (86) | |
| Mostly/Only English | 14% (22) | 19% (29) | |
| Child BMI (kg/m2) | 318 | 17.1 (15.9, 20.0) | 17.3 (16.0, 19.3) |
| Child Weight Category | 318 | ||
| Underweight (BMI percentile<5th) | 1% (2) | 1% (2) | |
| Normal weight (5th≤BMI percentile<85th) | 50% (80) | 43% (67) | |
| Overweight (85th≤BMI percentile<95th) | 20% (32) | 29% (46) | |
| Obese (BMI percentile≥95th) | 29% (47) | 27% (42) | |
| Primary Outcome | |||
| Child BMI z-score | 318 | 1.03 (0.39 1.81) | 1.17 (0.43, 1.70) |
| Secondary Outcomes | |||
| Child BMI (kg/m2) | 318 | 17.1 (15.9, 20.0) | 17.3 (16.0, 19.3) |
| Waist Circumference | |||
| Child Waist-to-Height Ratio | 318 | 0.509 (0.48, 0.55) | 0.51 (0.49, 0.56) |
| Child Waist-to-Hip Ratio | 318 | 0.901 (0.88, 0.93) | 0.91 (0.87, 0.95) |
| Child Physical Activity (Accelerometry) | |||
| % of time in moderate activity – weekdays | 247 | 6.65 (4.96, 8.92) | 6.95 (5.17, 10.42) |
| % of time in moderate activity – weekend | 230 | 7.35 (5.20, 9.99) | 8.16 (4.90, 12.13) |
| % of time in vigorous activity – weekdays | 247 | 1.41 0.87, 2.08) | 1.25 (0.81, 2.05) |
| % of time in vigorous activity – weekend | 230 | 1.04 (0.62, 2.35) | 1.41 (0.61, 2.68) |
| Child Screen Time | |||
| Hours per day level on weekdays | 313 | ||
| Not at all | 2% (3) | 1% (1) | |
| Less than 1 hour | 8% (12) | 11% (17) | |
| 1 hour per day | 27% (43) | 27% (42) | |
| 2 hours per day | 34% (53) | 31% (49) | |
| 3 hours per day | 11% (18) | 15% (23) | |
| 4 hours per day | 5% (8) | 8% (13) | |
| 5 or more hours per day | 13% (20) | 7% (11) | |
| Hours per day level on weekends | 310 | ||
| Not at all | 6% (10) | 8% (12) | |
| Less than 1 hour | 9% (14) | 10% (16) | |
| 1 hour per day | 15% (24) | 21% (32) | |
| 2 hours per day | 22% (34) | 25% (38) | |
| 3 hours per day | 25% (39) | 15% (24) | |
| 4 hours per day | 11% (17) | 11% (17) | |
| 5 or more hours per day | 11% (17) | 10% (16) | |
| Water intake (number of glass last week) | 293 | 14 (7, 21) | 14 (7, 19) |
| Fruit/Vegetable Preferences | |||
| Preference score for fruits | 303 | 1.73 (1.36, 2.00) | 1.64 (1.36, 2.00) |
| Preference score for vegetables | 293 | 1.20 (0.80, 1.53) | 1.20 (0.75, 1.60) |
| Preference score for fruits and vegetables | 303 | 1.38 (1.12, 1.62) | 1.38 (1.12 1.65 |
This includes one child who was accidentally enrolled three weeks before turning 5 years old.
Note: Some percentages total to more than 100% due to rounding error.
Of the 318 participating children (271 families), 254 (213 families) had any follow-up data, including 94 with only one follow-up and 160 with two follow-ups. Retention was similar across the two study arms. There was no evidence of difference in personal characteristics at baseline between those who did and did not complete follow-up assessment, both within and across study arms (data not shown).
Results of short-term and long-term effect intention-to-treat analyses for the primary outcome (BMI-Z) are reported in Table 2. Since the linear mixed-effects model and linear regression yielded very similar results, we report results only from the latter approach unless specified. We did not find a short-term difference in child’s BMI-Z growth rate between the two study arms in the overall sample (estimated difference 0.07 BMI-Z/month [95% CI, -0.02 to 0.15, p-value 0.11]), nor when stratifying the analysis by normal weight versus overweight/obese (results not shown). Similarly, we did not observe a long-term effect of the active intervention for BMI-Z.
Table 2.
Intention-to-treat analysis of estimated short-term and long-term effects of the intervention on primary and secondary outcomes
| Variable | N | Intervention Effect on Growth Ratea | Overall effect | ||
|---|---|---|---|---|---|
|
| |||||
| Estimate | 95% CI | P value | P value (df=2) | ||
| Short-Term Effects | |||||
|
| |||||
| Primary Outcome | |||||
| Child BMI-Zc | 206 | 0.068 | −0.016, 0.153 | 0.11 | 0.24 |
| Secondary Outcomes | |||||
| Child BMI (kg/m2)b | 206 | 0.084 | −0.121, 0.288 | 0.42 | 0.72 |
| Waist Circumference | |||||
| Child Waist-to-Height Ratio | 203 | −0.004 | −0.01, 0.002 | 0.15 | 0.35 |
| Child Waist-to-Hip Ratio | 203 | 0.005 | −0.003, 0.012 | 0.24 | 0.45 |
| Child Physical Activity (Accelerometry) | |||||
| % of time in moderate activity – weekdays | 129 | 0.100 | −0.81, 1.01 | 0.83 | 0.83 |
| % of time in moderate activity – weekend | 112 | 1.306 | 0.194, 2.417 | 0.02 | 0.06 |
| % of time in vigorous activity – weekdays | 129 | −0.353 | −1.051, 0.345 | 0.32 | 0.58 |
| % of time in vigorous activity – weekend | 112 | 0.293 | −0.371, 0.956 | 0.39 | 0.21 |
| Child Screen Time | |||||
| Hours per day level on weekdays | 202 | −0.056 | −0.35, 0.238 | 0.71 | 0.79 |
| Hours per day level on weekends | 201 | −0.257 | −0.646, 0.132 | 0.20 | 0.20 |
| Water intake (number of glass last week) | 167 | −0.439 | −2.37, 1.492 | 0.66 | 0.71 |
| Fruit/Vegetable Preferences | |||||
| Preference score for fruits | 188 | −0.058 | −0.131, 0.015 | 0.12 | 0.21 |
| Preference score for vegetables | 181 | −0.015 | −0.103, 0.074 | 0.75 | 0.94 |
| Preference score for fruits and vegetables | 188 | −0.036 | −0.099, 0.027 | 0.26 | 0.53 |
|
| |||||
| Long-Term Effects | |||||
|
| |||||
| Primary Outcome | |||||
| Child BMI-Ze | 169 | 0.023 | −0.016, 0.063 | 0.25 | 0.43 |
| Secondary Outcomes | |||||
| Child BMI (kg/m2)d | 169 | 0.067 | −0.051, 0.186 | 0.27 | 0.38 |
| Waist Circumference | |||||
| Child Waist-to-Height Ratio | 169 | 0.000 | −0.004, 0.003 | 0.97 | 0.98 |
| Child Waist-to-Hip Ratio | 169 | 0.006 | 0.001, 0.011 | 0.02 | 0.04 |
| Child Physical Activity (Accelerometry) | |||||
| % of time in moderate activity – weekdays | 102 | 0.183 | −0.124, 0.491 | 0.25 | 0.48 |
| % of time in moderate activity – weekend | 81 | 0.196 | −0.344, 0.736 | 0.48 | 0.75 |
| % of time in vigorous activity – weekdays | 102 | −0.005 | −0.087, 0.077 | 0.91 | 0.75 |
| % of time in vigorous activity – weekend | 81 | −0.021 | −0.195, 0.153 | 0.82 | 0.88 |
| Child Screen Time | |||||
| Hours per day level on weekdays | 167 | 0.038 | −0.074, 0.15 | 0.51 | 0.50 |
| Hours per day level on weekends | 165 | −0.002 | −0.151, 0.146 | 0.97 | 0.57 |
| Water intake (number of glass last week) | 153 | 0.504 | −0.373, 1.38 | 0.26 | 0.32 |
| Fruit/Vegetable Preferences | |||||
| Preference score for fruits | 134 | 0.008 | −0.029, 0.045 | 0.68 | 0.37 |
| Preference score for vegetables | 132 | 0.001 | −0.047, 0.049 | 0.97 | 0.78 |
| Preference score for fruits and vegetables | 134 | 0.001 | −0.031, 0.033 | 0.94 | 0.97 |
The estimated growth rate difference between the active intervention arm and the control arm. The growth rate is each outcome variable divided by the number of months between baseline and follow up.
Intracluster (within-family) correlation: rho=0.257
Intracluster (within-family) correlation: rho=0.393
Intracluster (within-family) correlation: rho=0.064
Intracluster (within-family) correlation: rho=0.142
The short- and long-term effects of the intervention on secondary outcomes from intention-to-treat analyses are presented in Table 2. Time spent in moderate physical activity on weekends increased in the short term for the active intervention arm (estimated difference 1.31 percent of time [95% CI 0.19 to 2.42, p-value=0.02]), although this difference became insignificant in the long term. In stratified analyses, the short-term effect of weekend moderate physical activity was only significant for overweight/obese children (estimated difference 1.73 percent of time [95% CI 0.57 to 2.88, p-value<0.01], not shown in tables). The results for waist-to-hip ratio were not in the expected direction in the long-term analysis, being higher in the intervention group than in active intervention group (estimated difference 0.006 [95% CI 0.001 to 0.011, p-value=0.02]), with no effect in the stratified analyses.
In secondary analyses (Supplemental Table S2), the results of per protocol analysis for short-term effects were similar to the intention-to-treat results, with the exception that there was a significant intervention effect on reducing weekend screen time (estimated difference −0.40 percent of time [95% CI −0.77 to −0.04, p-value=0.03]). In addition, the intervention effect on weekend moderate physical activity was larger among the per protocol participants (estimated difference 1.93 percent of time [95% CI 0.29 to 3.56, p-value=0.02]) than in the intention-to-treat analysis. The per protocol analysis for long-term effects did not yield any significant differences (data not shown).
Finally, dose response analyses assessed whether higher levels of attendance to group sessions were associated with a slower increase in BMI-Z or greater improvements in secondary outcomes at short-term or long-term follow-up. For child’s BMI-Z at short-term follow-up, the estimated growth rate tended to be slower with increasing exposure dose (especially at higher dose of 3 to 4), but it was only statistically significant for the strata of overweight/obese children (Supplemental Table S3). The trend of dose effects on BMI-Z at long-term follow-up were not as apparent as that of the short term dose effect. There was no clear trend of slower increase in other secondary outcomes’ growth rate with increasing exposure dose level (data not shown).
DISCUSSION
The Healthy Families Study tested a one-year family-based, behavioral intervention that was culturally-targeted for Hispanic families to prevent excessive weight gain in children ages 5–7. Intention-to-treat analyses and per protocol analyses did not show evidence of significant improvement in BMI-Z growth rate, either at the short-term or the long-term follow-up. However, dose response analyses suggested a trend toward a slower increase in BMI-Z among participants who attended more group sessions, with statistically significant dose effects for overweight/obese children at short-term follow-up. The active intervention demonstrated significant increases in weekend moderate physical activity in the overall sample and among overweight/obese children, as well as reduced weekend screen time in the per protocol analyses.
The dose response results suggested that inadequate intervention exposure may have limited the impact of the active intervention for many participants. In the active intervention arm, 25.6% of participants did not attend any group sessions, and 20.6% attended only one or two sessions. When the CHPs made weekly calls to remind them of upcoming classes, common reasons for absences included having other family commitments, having to work in the evening, and not having access to a car or ride. Parents of elementary school-aged children in general have many competing demands on their time, making it challenging to attend in-person classes every two weeks.
Other barriers to participation were unique to the Hispanic immigrant community. Given the strong influence of traditional gender roles in this community,22 some mothers could not come after work because they had to cook for their families. Many mothers did not know how to drive and depended on their spouse/partner to drive them if they arrived in time from work. Transportation was particularly a problem for undocumented Hispanic immigrants because obtaining a Tennessee driver’s license requires providing proof of legal status. Further, during the study period, the 287(g) program was in effect in Nashville/Davidson County, Tennessee, which made driving without a license a deportable offense for undocumented immigrants.
Evidence from pediatric weight loss interventions has suggested that more than 24 contact hours are needed to achieve weight loss,23 although comparable evidence of ideal contact time is not available for pediatric weight-gain prevention. This study highlighted low attendance as a challenge for engaging Hispanic families of elementary school-aged children in group-based obesity prevention programs in real-world settings. In a similar obesity prevention trial with 41% Hispanic parents of children ages 5–8,16 the family component included four group classes (two per year), a home visit, mailings, and phone calls, combined with a recreation center component. The authors observed low participation in group classes and noted the challenge of exposing families to a sufficient dose of the intervention, which likely contributed to their non-significant results. A multi-level intervention with Mexican-origin children ages 3–8 combined 10 parent classes per year with new school curricula and economic incentives to purchase fruits and vegetables, and had a significant effect on BMI-Z only for the subset of obese boys after one year.24 Several other family-based weight-gain prevention RCTs that target Hispanic, elementary-school aged children are in progress but have not published outcome findings to date.25–28
A handful of obesity prevention interventions involving parent-directed intervention components have been targeted for younger, preschool-aged Hispanic children. A child-care based intervention including curricular modules and weekly newsletters and homework assignments for parents for 14 weeks had non-significant results.11 However, one consisting of 12 group classes at a recreation center reported a significant effect on BMI at four-month follow-up,13 and another providing nine parent classes found a significant effect on BMI-Z at one-year follow-up among a subset of participants with BMI≥50th percentile. Preschool could be a more effective age than elementary school for engaging in-person parent participation for this population.
Culturally-targeted weight-loss treatment interventions with obese Hispanic children have been more successful for slowing BMI growth than weight-gain prevention interventions.15,29 Perhaps parents of obese children are more concerned about their children’s weight and more motivated to attend sessions and make changes in the family, which would be consistent with our dose response results and previous studies reporting significant effects only among overweight children.
One limitation of the study was a low response rate for the accelerometry, with valid data successfully collected from 78% of children at baseline, 63% at short-term, and 60% at long-term follow-up. Commonly children reported they forgot to wear the accelerometer, lost it, or did not want to wear accelerometers at the waist with the belt provided. Furthermore, the study was limited by not having data at follow-up to assess a range of dietary intake outcomes.
Several limitations common to community-based behavioral trials may also have contributed to the limited significant effects of the intervention, such as the Hawthorne effect, subject reactivity to repeated assessment processes, self-selection bias, social desirability for self-reported data, and cross-contamination. While the attention control arm focused on a different topic (oral health), its emphasis on prevention could have had a bleed-over effect, stimulating parents to engage in other preventive behaviors to benefit their child’s health. Part of the oral health intervention encouraged participants to avoid sugar as a cause of cavities, not for nutritional reasons. Nevertheless, this message could have led to lower consumption of sugary beverages and foods in the control group, which research has been associated with BMI reduction.30
In conclusion, only a few family-level interventions for children have been efficacious to date,6,8,9 thus more research is needed. Effective family-based interventions are needed to complement policy and environmental interventions for a multi-level approach to promoting healthy weight gain in children, in particular targeting Hispanic youth and other groups with the fastest growing prevalence of obesity. The Healthy Families Study tested the efficacy of a culturally-targeted weight gain prevention intervention in children in a community setting using lay CHPs. The trial expanded the small pool of family-based childhood obesity prevention interventions targeted for Hispanic immigrant families with elementary school-aged children in community settings. Traditional health education strategies that require families to attend multiple classes may not be effective in achieving sustained engagement of parents, particularly Hispanic immigrants, with children in this age range due to competing demands on time and transportation-related barriers. Future research could develop alternative intervention strategies other than attending multiple classes, such as technology-assisted interventions, to achieve greater intervention engagement among parents and children and produce sustainable behavior changes.
Supplementary Material
What is already known about this subject?
Obesity prevalence is higher and increasing more rapidly among Hispanic children compared to non-Hispanic white children.
The strength of evidence is low regarding the efficacy of family-based intervention strategies that are implemented in the community and/or the home, due to a small number of studies and largely non-significant effects
Only a handful of randomized controlled trials have tested family-based obesity prevention interventions in community settings for elementary school-age Hispanic children from immigrant families in the US.
What does this study add?
This paper reports on the short-term (median 6 month follow-up) and long-term (median 16 month follow-up) outcomes of a culturally-targeted, family-based weight gain prevention intervention for Hispanic immigrant families with children ages 5–7.
Overall the growth rate of child BMI z-score did not differ between the active intervention and attention control arms, although a slower increase in BMI z-score was observed among overweight/obese children who attended more intervention classes.
The intervention led to increased moderate physical activity on weekends at short term, and weekend screen time decreased at short term among children in the active intervention arm who attended at least one class session.
Acknowledgments
We would like to thank the Nashville Latino Health Coalition and Progreso Community Center for their collaboration as partners in developing and implementing this study. We are also grateful to Jaden Harris and Caree McAfee for editing and bibliographic assistance. All authors were involved in writing the paper and approved the final paper as submitted. RZ and PH led the study, developed the research questions, and drafted the paper. PH and JC led intervention development, data collection, and intervention implementation. MB, JC, and BB contributed to the development of the research question and the analytic plan and made contributions to writing and revising the paper. LD and TK carried out the data analysis, interpreted results, and contributed to revisions. This research was supported by the National Institutes of Health, grant number P20 MD000516 National Institute on Minority Health and Health Disparities, grant number UL1 RR024975 National Center for Research Resources, grant number UL1 TR000445 National Center for Advancing Translational Sciences, grant numbers R01 DK69465 and P60 DK20593 National Institute of Diabetes and Digestive and Kidney Diseases, and grant numbers P30 CA068485 and U54 CA163072 National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest Statement
The authors have no financial conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16(10):2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 3.Rendall MS, Weden MM, Fernandes M, Vaynman I. Hispanic and black US children’s paths to high adolescent obesity prevalence. Pediatr Obes. 2012;7(6):423–435. doi: 10.1111/j.2047-6310.2012.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoelscher DM, Kirk S, Ritchie L, Cunningham-Sabo L Academy Positions Committee. Position of the Academy of Nutrition and Dietetics: interventions for the prevention and treatment of pediatric overweight and obesity. J Acad Nutr Diet. 2013;113(10):1375–1394. doi: 10.1016/j.jand.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics. 2013;132(1):e201–e210. doi: 10.1542/peds.2013-0886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;(12):CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Zhou YE, Emerson JS, Levine RS, Kihlberg CJ, Hull PC. Childhood obesity prevention interventions in childcare settings: systematic review of randomized and nonrandomized controlled trials. Am J Health Promot. 2014;28(4):e92–103. doi: 10.4278/ajhp.121129-LIT-579. [DOI] [PubMed] [Google Scholar]
- 8.Showell NN, Fawole O, Segal J, et al. A systematic review of home-based childhood obesity prevention studies. Pediatrics. 2013;132(1):e193–200. doi: 10.1542/peds.2013-0786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Cai L, Wu Y, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16(7):547–565. doi: 10.1111/obr.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santiago-Torres M, Cui Y, Adams AK, et al. Familial and individual predictors of obesity and insulin resistance in urban Hispanic children. Pediatr Obes. 2016;11(1):54–60. doi: 10.1111/ijpo.12020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14(9):1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- 12.Slusser W, Frankel F, Robison K, Fischer H, Cumberland WG, Neumann C. Pediatric overweight prevention through a parent training program for 2–4 year old Latino children. Child Obes. 2012;8(1):52–59. doi: 10.1089/chi.2011.0060. [DOI] [PubMed] [Google Scholar]
- 13.Barkin SL, Gesell SB, Po’e EK, Escarfuller J, Tempesti T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics. 2012;130(3):445–456. doi: 10.1542/peds.2011-3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gatto NM, Martinez LC, Spruijt-Metz D, Davis JN. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr Obes. 2016 Feb; doi: 10.1111/ijpo.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Branscum P, Sharma M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obes Rev. 2011;12(5):e151–e158. doi: 10.1111/j.1467-789X.2010.00809.x. [DOI] [PubMed] [Google Scholar]
- 16.Elder JP, Crespo NC, Corder K, et al. Childhood obesity prevention and control in city recreation centres and family homes: the MOVE/me Muevo Project. Pediatr Obes. 2014;9(3):218–231. doi: 10.1111/j.2047-6310.2013.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koplan J, Liverman CT, Kraak VI, Wisham SL. Progress in Preventing Childhood Obesity: How Do We Measure Up? Washiington, DC: National Academies Press; 2007. [Accessed June 3, 2014]. http://www.nap.edu/catalog/11722/progress-in-preventing-childhood-obesity-how-do-we-measure-up. [Google Scholar]
- 18.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 19.McKinney J, Kurtz-Rossi S. Culture, health, and literacy: a guide to health education materials for adults with limited English literacy skills. 2000 Nov; http://healthliteracy.worlded.org/docs/culture/
- 20.Zoorob R, Buchowski MS, Beech BM, et al. Healthy Families Study: design of a childhood obesity prevention trial for Hispanic families. Contemp Clin Trials. 2013;35(2):108–121. doi: 10.1016/j.cct.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hull PC, Reece MC, Patton M, et al. A community-based oral health self-care intervention for Hispanic families. Int J Public Health. 2014;59(1):61–66. doi: 10.1007/s00038-013-0470-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerchow L, Tagliaferro B, Squires A, et al. Latina food patterns in the United States: a qualitative metasynthesis. Nurs Res. 2014;63(3):182–193. doi: 10.1097/NNR.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 23.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 24.Sadeghi B, Kaiser LL, Schaefer S, et al. Multifaceted community-based intervention reduces rate of BMI growth in obese Mexican-origin boys. Pediatr Obes. 2016 doi: 10.1111/ijpo.12135. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Azevedo KJ, Mendoza S, Fernandez M, et al. Turn Off the TV and Dance! participation in culturally tailored health interventions: implications for obesity prevention among Mexican American girls. Ethn Dis. 2013;23(4):452–461. [PMC free article] [PubMed] [Google Scholar]
- 26.Ayala GX, Ibarra L, Binggeli-Vallarta A, et al. Our Choice/Nuestra Opción: the Imperial County, California, Childhood Obesity Research Demonstration study (CA-CORD) Child Obes. 2015;11(1):37–47. doi: 10.1089/chi.2014.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flattum C, Draxten M, Horning M, et al. HOME Plus: program design and implementation of a family-focused, community-based intervention to promote the frequency and healthfulness of family meals, reduce children’s sedentary behavior, and prevent obesity. Int J Behav Nutr Phys Act. 2015;12:53. doi: 10.1186/s12966-015-0211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoelscher DM, Butte NF, Barlow S, et al. Incorporating primary and secondary prevention approaches to address childhood obesity prevention and treatment in a low-income, ethnically diverse population: study design and demographic data from the Texas Childhood Obesity Research Demonstration (TX CORD) study. Child Obes. 2015;11(1):71–91. doi: 10.1089/chi.2014.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnston CA, Tyler C, Fullerton G, et al. Results of an intensive school-based weight loss program with overweight Mexican American children. Int J Pediatr Obes. 2007;2(3):144–152. doi: 10.1080/17477160701305864. [DOI] [PubMed] [Google Scholar]
- 30.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14(8):606–619. doi: 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.