Abstract
Objective
Although conscientiousness/disinhibition plays a substantial role in internalizing and externalizing psychopathology, the underlying mechanisms are not well-understood. We aim to clarify facet-level associations, and to examine whether (a) impairment mediates the link of conscientiousness with internalizing and externalizing symptoms, and (b) demoralization (assessed via neuroticism) accounts for their associations.
Method
450 participants (Mage=42; primarily female and Caucasian) who reported current/recent psychiatric treatment completed two measures of domain and facet-level traits (i.e., NEO PI-3, PID-5), as well as interview measures of impairment and disorders. Correlation, regression, and mediation analyses were conducted.
Results
Internalizing disorders (and particularly, the distress disorders) were uniquely associated with facets related to low self-efficacy, whereas externalizing disorders were uniquely associated with risk-taking and disregarding rules. For the internalizing disorders only, these associations were reduced after accounting for neuroticism, though associations with distress disorders remained significant. Impairment mediated the link between conscientiousness and symptoms for internalizing disorders, but not consistently for externalizing disorders.
Conclusions
The internalizing and externalizing disorders are associated with conscientiousness due to different facet-level content. Demoralization and impairment both contribute to the link between internalizing disorders and conscientiousness, whereas neither process accounts substantially for the relation of externalizing disorders with conscientiousness.
Keywords: conscientiousness/disinhibition, facets, impairment, demoralization, internalizing and externalizing disorders
Conscientiousness—and broader related traits such as disinhibition vs. constraint—has long been empirically linked to important health outcomes. For example, conscientiousness is associated with physical health sequelae including longevity, disease, and health-related behaviors (e.g., Bogg & Roberts, 2013). Conscientiousness is also consistently related to externalizing psychopathology, with medium to large meta-analytic effect sizes reported for substance use disorders (Cohen’s ds = −.90 to −1.34 across different substance use disorders, Kotov, Gamez, Schmidt, & Watson, 2010; r = −.32 for any substance use disorder, Ruiz, Pincus, & Schinka, 20081) and for antisocial personality disorder (ASPD) (r = −.30; Ruiz et al., 2008). Although conscientiousness traditionally has not been considered central to internalizing psychopathology (e.g., depression, anxiety), there is emerging evidence that internalizing symptoms may also have substantial links with low conscientiousness. The Kotov et al. meta-analysis found that conscientiousness was uniformly and strongly associated with various depressive and anxiety disorders (ds = .67 to −1.24), with effect sizes only a little weaker than those of the substance use disorders.
Conscientiousness appears to play a substantial role in psychopathology broadly, but the mechanisms underlying this association are not well-understood. One approach for clarifying these mechanisms is to examine more narrow components or facets of conscientiousness that may account for the domain-level association. Although there are different models for the content of these facets, the commonly-used NEO Personality Inventory model (e.g., Costa & McCrae, 1992) includes six conscientiousness facets: competence (i.e., feelings of self-efficacy), order (i.e., preference for tidiness and organization), dutifulness (i.e., following the rules and a strong sense of morality), achievement-striving (i.e., perseverance and strong work ethic), self-discipline (i.e., engaging in tasks and duties promptly), and deliberation (i.e., a planful, cautious approach in one’s behavior/decisions). With regard to externalizing disorders, the Ruiz et al. meta-analysis indicated that low deliberation, low dutifulness, and low self-discipline were the primary conscientiousness facets with which externalizing disorders (i.e., substance use disorders and APSD) were associated. Substance use disorders were also moderately associated with low competence (Ruiz et al., 2008). Thus, traits such as poor impulse control, a failure to plan ahead, and disregard for rules seem to be largely responsible for the link between low conscientiousness and externalizing psychopathology.
Few studies have examined facet-level associations of conscientiousness with the internalizing disorders, but low competence and self-discipline are most consistently associated with these disorders, with achievement-striving also significantly associated in some studies (Bienvenu et al., 2004; Hayward, Taylor, Smoski, Steffens, & Payne, 2013; Rector, Bagby, Huta, & Ayearst, 2012; Rector, Hood, Richter, & Bagby, 2002). Of note, one study found that the association between conscientiousness and social anxiety was almost entirely accounted for by the competence/self-efficacy facet (Kaplan et al., 2015). This limited literature suggests that the internalizing disorders are linked to conscientiousness primarily via beliefs that one is ineffective in initiating and maintaining efforts towards goals in daily life, as opposed to via tendencies towards impulsivity, disregard of rules, or a lack of order.
The above findings are cross-sectional and correlational in nature, and therefore they cannot provide information about the nature of the association between conscientiousness and disorders. Although it is often assumed that personality traits are pre-existing characteristics that contribute to the subsequent development of psychopathology or psychological health (predisposition or vulnerability model), other types of relationships are possible. For example, it may be that symptoms lead to changes in personality (scar or pathoplasty model), a third variable(s) contributes to traits and symptoms, and/or effects are transactional/bidirectional in nature (e.g., Klein, Kotov, & Bufferd, 2011). There is some evidence for bidirectional effects for externalizing disorders: low conscientiousness prospectively predicts greater increases in alcohol use over time, and high alcohol use prospectively predicts greater declines in levels of conscientiousness over time (e.g., Littlefield, Verges, Wood, & Sher, 2012; Quinn, Stappenbeck, & Fromme, 2011; Roberts & Boggs, 2004). However, the nature of the relationship between conscientiousness and the internalizing disorders has not been tested to date.
Despite little empirical research examining why and how conscientiousness is associated with psychopathology, researchers have discussed two (non-mutually exclusive) hypotheses about the conscientiousness-internalizing psychopathology link, which are also relevant to the association between conscientiousness and the externalizing disorders. One hypothesis stems from the fact that individuals with marked psychopathology—and particularly those with high levels of internalizing symptoms— tend to experience demoralization (e.g., Tellegen, 1985), defined as “nonspecific unpleasant experiences” that are common among those seeking mental health treatment (e.g., Noordhof, Sellbom, Eigenhuis, & Kamphuis, 2015; Tellegen et al., 2003). Some have argued, based on theory and empirical evidence, that low scores on facets of conscientiousness that assess perceptions of self-efficacy and competence in part signify current demoralization among those with psychopathology (Kotov et al., 2010; Noordhof et al., 2015). Thus, demoralization may be a confounding variables that partially or fully accounts for the association between conscientiousness and disorders. Although there are few specific measures of demoralization, neuroticism— which is largely defined by generalized negative affect—is strongly linked to demoralization empirically (r = .62 to .81; Noordhof et al., 2015; Sellbom, Ben-Porath, & Bagby, 2008) and may serve as a proxy for it. Therefore, controlling for levels of neuroticism should reduce the conscientiousness-psychopathology association if demoralization partially accounts for the association, and it should be reduced to non-significance if it fully or primarily accounts for the association. Of note, the Kotov et al. (2010) meta-analysis found reduced but still substantial relations between domain-level conscientiousness and disorders after accounting for neuroticism (ds = −.46 to −.87 for internalizing disorders, −.70 to −1.11 for substance use disorders), suggesting that demoralization contributes somewhat but not heavily to the association.
Alternatively, there is evidence that components of low conscientiousness may lead to objective negative life events such as academic, work, or relationship problems (Roberts, Kuncel, Shiner, Caspi, & Goldberg, 2007) and to difficulties in daily functioning (Karsten, Pinninx, Verboom, Nolen, & Hartman, 2013). Thus, it may be that conscientiousness does not directly lead to psychopathology, but that it does so indirectly by contributing to stressful life events and poor functioning that then increase the likelihood of psychopathology (Klein et al., 2011; Kotov et al., 2010; Roberts et al., 2007). Relevant to this hypothesis, there is an interesting discrepancy in the literature on internalizing disorders and conscientiousness. Whereas the Kotov et al. (2010) meta-analysis showed an effect of conscientiousness on internalizing psychopathology in a between-groups context (i.e., comparing individuals diagnosed with a psychological disorder to healthy controls), the associations tend to be weaker or non-significant when dimensional symptoms underlying these disorders are examined (e.g., Chioqueta & Stiles, 2005; Kaplan, Levinson, Rodebaugh, Menatti, & Weeks, 2015; Mezquita et al., 2015; Watson, Gamez, & Simms, 2005; Watson & Naragon-Gainey, 2014). If impairment largely accounts for the association between conscientiousness and psychopathology, we would expect stronger associations with disorders than symptoms because psychosocial impairment is built into the diagnostic criteria (although it is not required if clinically-significant distress is present instead; APA, 2013), but impairment typically is not included in dimensional measures of symptom severity. While this pattern of results is consistent with the impairment hypothesis, it has not been directly tested.
In the current study, we explored these issues in a diagnostically-heterogeneous sample of adults who currently or recently received outpatient treatment for mental health concern. We had three aims: (1) To clarify the unique facet-level associations of conscientiousness and the related trait disinhibition across a broad range of internalizing disorders (i.e., fear disorders such as social anxiety and panic, as well as distress disorders such as depression and GAD; Watson, 2005) and externalizing disorders (i.e., alcohol use disorders, substance use disorders, antisocial personality disorder). Based on prior research reviewed above, we expected that internalizing disorders would be most strongly associated with facets related to self-efficacy, competence, and discipline, whereas the externalizing disorders would be most closely associated with facets such as impulsivity, deliberation, and dutifulness; (2) To examine whether associations between conscientiousness/disinhibition and psychopathology are reduced in magnitude after accounting for neuroticism (a proxy for demoralization), consistent with the demoralization hypothesis; (3) To test whether impairment has a significant indirect effect on the association between conscientiousness/disinhibition and these disorders, consistent with the impairment mediation hypothesis. We also examine a mediation model that includes neuroticism as a covariate, to determine the unique effects of demoralization and impairment in the conscientiousness-disorder association.
Symptoms and impairment were assessed via clinical interview, whereas personality traits were assessed with self-report. We used two omnibus measures of personality, and a comparison of results across measures serves as an internal replication of findings. One measure was developed within the normal personality framework and includes Conscientiousness facets (i.e., NEO Personality Inventory-3 [NEO PI-3]; McCrae, Costa, & Martin, 2005), whereas the other assesses abnormal personality, including Disinhibition and its facets (i.e., Personality Inventory for DSM-5 [PID-5]; Krueger, Derringer, Markon, Watson, & Skodol, 2012). While several studies have found that these measures are closely associated and generally assess similar constructs (Griffin & Samuel, 2014; Suzuki, Samuel, Pahlen, & Krueger, 2015; Wright & Simms, 2014), they are also complementary in that each measure covers certain content better than the other. Table 1 describes the Conscientiousness/Disinhibition facets for each measure, indicating pairs of facets that are highly similar across measures and facets that are unique to one measure, based on content and prior research.
Table 1.
Content Summary of the NEO PI-3 and PID-5 Conscientiousness/Disinhibition Domains and Facets
| Inventory and Scale | Corresponding cross- inventory scale | Description |
|---|---|---|
| NEO Conscientiousness | ||
| Competence | None | Perceptions of self-efficacy, confidence in one’s abilities |
| Order | PID-5 Rigid Perfectionism | Want surroundings to be ordered, no deviation from plans, concern with things being done the “right” way |
| Dutifulness | PID-5 Irresponsibility | Fulfills moral obligations and other commitments, follows the rules |
| Achievement Striving |
None | Strong drive for setting and reaching goals, willingness to work hard |
| Self-Discipline | PID-5 Distractibility | Initiates tasks and follows through, without procrastination or derailment |
| Deliberation | PID-5 Impulsivity | Words and actions are premeditated, plans ahead |
| PID-5 Disinhibition | ||
| Irresponsibility | NEO Dutifulness | Failure to carry out and/or respect commitments to others |
| Impulsivity | NEO Deliberation | Acting without forethought or consideration of distal outcomes, responding impulsively in times of emotional distress |
| Distractibility | NEO Self-Discipline | Difficulty concentrating on tasks and maintaining effort towards goals |
| Risk Taking | None | Enacting risky behaviors without regard for potential negative consequences |
| Rigid Perfectionism |
NEO Order | Inflexible expectations and demands that self and other adhere to unrealistically-high standards, rigidity in attitudes and behavior, over-attention to detail (reverse-keyed) |
Method
Participants and Procedure
We analyzed data collected as part of a larger study to develop a new measure of personality pathology traits (CAT-PD; see Simms et al., 2011, for further details). Participants were recruited from mental health treatment centers in Western New York, and they were eligible to participate if they were 18 years of age or older and reported receiving psychiatric treatment within the past two years. The final sample consisted of 628 participants. For the current study, samples sizes vary across analyses, as 266 participants completed the NEO PI-3 and 450 completed the PID-5 (265 participants completed both measures). For the largest subgroup analyzed here (n = 450), the mean age was 41.9 years (SD = 12.5), and the majority of the sample was female (65%). Most participants identified primarily as Caucasian (68%) or African American (30%). Sixty-four percent of the sample reported currently receiving psychiatric treatment, whereas the rest of the sample reported having done so within the past two years. There were no significant differences in the above variables between the sample analyzed in the current study and the full sample of 628 participants (all ps > .10).
Based on the MINI interview (described below), participants in the subsample analyzed here met criteria for DSM-5 current diagnoses at the following rates: GAD = 195 individuals (43%), major depressive disorder = 150 (33%), bipolar disorder I or II = 133 (30%), antisocial personality disorder = 130 (29%), OCD = 110 (24%), alcohol use disorder = 99 (22%), PTSD = 94 (21%), substance use disorder = 81 (18%), social anxiety disorder = 77 (17%), panic disorder = 59 (13%), persistent depressive disorder = 48 (11%), agoraphobia = 44 (10%), and psychotic disorder = 43 (10%).
Participants came to the lab for a four-hour session that included the completion of self-report questionnaires and clinical interviews, and they received $50 plus the cost of transportation as compensation. We describe below the measures that were analyzed for the current study.
Measures
Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998)
The MINI is a structured diagnostic interview that includes a range of diagnoses; the current study focuses on depressive, anxiety, and substance use disorders, as well as antisocial personality disorder (ASPD). We adapted the MINI (with permission) to assess DSM-5 criteria for the sample disorders. We analyzed symptom counts, rather than dichotomous diagnoses, because they yield greater information and variability; note that the impairment/distress criterion was not included in these symptom counts. The MINI has demonstrated good interrater reliability, as well as good convergent and discriminant validity with other diagnostic interviews (Sheehan et al., 1998). In the present study, trained interviewers, typically clinical psychology doctoral students, conducted MINI interviews. Interviewers received extensive training and ongoing supervision by the second author (LJS), which included weekly case conferences and tape review throughout the course of the study. Independent raters recoded 120 interviews with excellent reliability: MINI disorder-level kappas were strong, Mdn K = .96, range = .66–1.00.
NEO Personality Inventory-3 First Half (NEO PI-3FH; McCrae et al., 2005)
The NEO PI-3FH was developed within the Five Factor Model tradition, wherein each domain is the sum of six lower-order facets (here, we only report domain-level scores and the conscientiousness facets, with content described in Table 1). This measure includes only the first half of the full NEO PI-3 to reduce participant burden and required administration time. Thus, the NEO PI-3FH has 120 items, with four items assessing each of the 30 facets, and it demonstrates adequate internal consistency (median alpha = .64) and a similar overall structure as the full measure (McCrae & Costa, 2007). In the current study, internal consistencies were low for some of the facet scales but generally adequate (alphas = .50 to .80; mean = .67), and internal consistencies were good for domain scales (mean alpha for domains = .82).
Personality Inventory for DSM-5 (PID-5 et al., 2012)
The PID-5 was designed to assess 25 lower-order traits relevant to personality pathology as conceptualized for Section III of DSM-5. These lower-order scales can be grouped into one of five domains (i.e., Negative Affectivity, Detachment, Disinhibition, Antagonism, Psychoticism) that are consistent with the Five Factor Model (corresponding to neuroticism, extraversion, conscientiousness, agreeableness, and openness, respectively). The current study reports scores on the five lower-order scales relevant to Disinhibition (i.e., Distractibility, Impulsivity, Irresponsibility, Rigid Perfectionism, and Risk-Taking; see Table 1), as well as the other domain-level scales. The domain-level Disinhibition scale is the sum of the Distractibility, Irresponsibility, and Impulsivity scales. The PID-5 uses a four-point Likert-type response scale and contains a total of 220 items. Previous studies have reported acceptable internal consistency, ranging from .72 to .96 across scales (median alpha = .86; Krueger et al., 2012). The scales analyzed here demonstrated good internal consistency in our sample (mean alpha for domains = .94; mean alpha for Disinhibition facets = .87).
World Health Organization Disability Assessment Schedule-II (WHODAS-II; World Health Organization, 2000) measures impairment in functioning across six domains: Communication, Mobility, Self-Care, Interpersonal, Work, and Participation in Society. We interviewed participants using the 12-item version of the WHODAS-II to assess functioning across six domains (i.e., communication, mobility, self-care, getting along, life activities, and participation in society). For the present a study, we computed a single global score, with higher scores indicating greater disability. Inter-rater reliability for these scores was strong (intraclass correlation between raters = .98).
Data Analysis
As noted previously, samples sizes varied across measures, which led to different sample sizes across analyses. Data were analyzed using SAS© software, version 9.4. Correlations, semipartial correlations, and simultaneous multiple regressions were used to examine the associations between traits and symptoms. Semiparital correlations were selected to test the demoralization hypothesis because they account for the shared variance between neuroticism/negative affectivity and conscientiousness/disinhibition, but leave the criterion variable (i.e., symptoms) unaltered. Prior to calculating the mean of correlations, the individual correlations were transformed using Fisher’s r to z transformation, averaged, and then transformed back to the r metric. The Williams modification of the Hotelling test (see Kenny, 1987) tested whether two correlations involving a common variable differed significantly in magnitude. To examine direct and indirect effects in mediation analyses, we used Hayes’ (2013) PROCESS macro, version 2.13. Bias-corrected 95% confidence intervals for indirect effects were generated using 10,000 bootstrap samples.
Results
Zero-order correlations among the NEO PI-3 domains, PID-5 domains, and conscientiousness facets from both inventories are shown in Table 2. NEO PI-3 Conscientiousness and PID-5 Disinhibition demonstrated good convergent validity (r = −.73). Both had substantial secondary associations with Neuroticism/Negative Affectivity (mean absolute r = .58), and these correlations were particularly strong for PID-5 Disinhibition.
Table 2.
Zero-0rder Correlations among NEO and PID-5 Domains and Conscientiousness Facets
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. NEO Neuroticism | ||||||||||||||||||||
| 2. NEO Extraversion | −.48 | |||||||||||||||||||
| 3. NEO Conscientious | −.58 | .32 | ||||||||||||||||||
| 4. NEO Agreeableness | −.25 | .00 | .15 | |||||||||||||||||
| 5. NEO Openness | −.06 | .34 | .04 | .25 | ||||||||||||||||
| 6. PID-5 Negative Aff. | .81 | −.33 | −.42 | −.31 | −.09 | |||||||||||||||
| 7. PID-5 Detachment | .50 | −.74 | −.36 | −.20 | −.33 | .53 | ||||||||||||||
| 8. PID-5 Disinhibition | .62 | −.23 | −.73 | −.40 | −.09 | .68 | .53 | |||||||||||||
| 9. PID-5 Antagonism | .10 | .17 | −.17 | −.70 | −.09 | .32 | .24 | .47 | ||||||||||||
| 10. PID-5 Psychoticism | .39 | −.15 | −.39 | −.40 | .07 | .58 | .48 | .67 | .50 | |||||||||||
| 11. NEO Competence | −.67 | .41 | .83 | .20 | .16 | −.53 | −.46 | −.70 | −.15 | −.44 | ||||||||||
| 12. NEO Order | −.14 | .10 | .62 | −.15 | −.09 | −.06 | −.04 | −.28 | .00 | −.11 | .31 | |||||||||
| 13. NEO Dutifulness | −.44 | .21 | .79 | .38 | .10 | −.36 | −.29 | −.66 | −.34 | −.36 | .65 | .28 | ||||||||
| 14. NEO Achievement | −.46 | .43 | .82 | −.02 | .10 | −.28 | −.39 | −.47 | .03 | −.21 | .64 | .46 | .57 | |||||||
| 15. NEO Discipline | −.57 | .29 | .90 | .06 | −.06 | −.42 | −.33 | −.69 | −.11 | −.35 | .74 | .50 | .68 | .74 | ||||||
| 16. NEO Deliberation | −.44 | .04 | .70 | .33 | .01 | −.35 | −.22 | −.66 | −.31 | −.38 | .59 | .25 | .58 | .40 | .52 | |||||
| 17. PID-5 Distractibility | .64 | −.32 | −.64 | −.21 | .00 | .66 | .53 | .87 | .27 | .58 | −.62 | −.28 | −.50 | −.47 | −.68 | −.44 | ||||
| 18. PID-5 Impulsivity | .48 | −.04 | −.59 | −.44 | −.07 | .55 | .36 | .86 | .46 | .60 | −.58 | −.28 | −.52 | −.29 | −.49 | −.74 | .58 | |||
| 19. PID-5 Irresponsibility | .47 | −.25 | −.69 | −.40 | −.17 | .33 | .47 | .84 | .51 | .55 | −.63 | −.27 | −.74 | −.48 | −.64 | −.54 | .61 | .61 | ||
| 20. PID-5 Perectionism | .32 | −.15 | .16 | −.38 | −.19 | .50 | .38 | .33 | .34 | .44 | −.09 | .49 | .01 | .18 | .08 | −.02 | .31 | .29 | .25 | |
| 21. PID-5 Risk-Taking | .01 | .22 | −.19 | −.42 | .10 | .09 | .00 | .34 | .43 | .35 | −.12 | −.06 | −.30 | .04 | −.10 | −.44 | .12 | .48 | .27 | .10 |
Note. N = 265–266 for correlations with NEO scales (r > |.12| are significant at p < .05), N = 463 for correlations among PID-5 scales (r > |.09| are significant at p < .05). Correlations greater than or equal to |.50| are shown in boldface.
Based on facet content, we expected convergent associations of specific pairs of NEO PI-3 Conscientiousness and PID-5 Disinhibition facets (i.e., Distractibility with Discipline, Impulsivity with Deliberation, Irresponsibility with Dutifulness, and Perfectionism with Order; see Table 1). In 35 of the 36 comparisons tested, the convergent correlations were significantly stronger than the other nine corresponding discriminant facet correlations (zs = 1.88 to 15.46; ps < .05). The only exception was that the correlation between Irresponsibility and Discipline was not significantly different than that of Distractibility and Discipline, z = 1.06, p > .05. Given the above evidence of convergent validity of facets across the two inventories, we utilized these pairs in subsequent analyses as a test of replicability of effects across measures. Of the remaining facets that did not show specific associations with a facet in the other inventory, NEO PI-R Competence and Achievement were broadly related to the three core PID-5 Disinhibition scales, although the associations were larger for Competence than for Achievement. Lastly, PID-5 Risk-Taking was most closely but only moderately associated with NEO PI-3 Deliberation.
Associations of Facets with Disorders, Symptoms, and Impairment
Zero-order associations
Cohen’s ds comparing individuals with each disorder to those without an internalizing or externalizing disorder (Table 3) ranged from small to large effect sizes for NEO PI-3 Conscientiousness (ds = −.32 for panic disorder to −1.02 for PTSD; mean d = −.66) and consistently large effect sizes for PID-5 Disinhibition (ds = .97 for persistent depressive disorder to 1.88 for PTSD; mean d = 1.38). Zero-order correlations between continuous symptoms and conscientiousness facets are shown in the top portion of Table 4; the magnitudes of associations were generally small to moderate in size. Mirroring the diagnostic data, the PID-5 scales consistently displayed larger effect sizes with symptoms than did the NEO PI-3 scales.
Table 3.
Effect Sizes by Diagnosis and Simultaneous Multiple Regressions of Conscientiousness Facets on Symptoms
| DEP | PDD | PTSD | GAD | PAN | AGOR | SOC | OCD | ALC | SUB | ASPD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohen’s d | |||||||||||
| NEO Conscientious. | −.64 | −.51 | −1.02 | −.63 | −.32 | −.49 | −.85 | −.63 | −.73 | −.73 | −.67 |
| PID-5 Disinhibition | 1.66 | .97 | 1.88 | 1.22 | 1.03 | 1.58 | 1.63 | 1.33 | 1.29 | 1.34 | 1.24 |
| Regression Coefficients | |||||||||||
| NEO Competence | −.18 (.04)*** | −.14 (.04)** | −.32 (.09)*** | −.11 (.04)** | −.12 (.11) | .02 (.03) | −.07 (.03)* | −.04 (.02)** | −.05 (.05) | .03 (.05) | .02 (.05) |
| NEO Order | .04 (.03) | .06 (.03)* | .11 (.06)* | .06 (.03)* | .04 (.06) | .02 (.02) | .03 (.02) | .01 (.01) | .02 (.03) | −.01 (.03) | .06 (.03) |
| NEO Dutifulness | .03 (.04) | .01 (.04) | .03 (.09) | .03 (.04) | .18 (.11) | .01 (.03) | .03 (.03) | .02 (.02) | −.11 (.04)* | −.17 (.05)*** | −.11 (.05)* |
| NEO Achievement | −.03 (.03) | −.03 (.03) | -−.01 (.07) | .01 (.03) | .01 (.08) | −.04 (.02) | −.03 (.02) | .00 (.01) | .05 (.04) | .06 (.04) | .03 (.04) |
| NEO Discipline | −.03 (.04) | −.02 (.04) | −.03 (.08) | −.07 (.04)* | −.19 (.09) | −.01 (.02) | −.01 (.03) | .00 (.01) | .04 (.04) | .02 (.04) | .04 (.04) |
| NEO Deliberation | −.01 (.03) | −.01 (.03) | −.11 (.07) | .04 (.03) | −.01 (.08) | −.01 (.02) | .00 (.02) | −.02 (.01) | −.05 (.03) | −.06 (.04) | −.11 (.04)** |
| R2 | .196 | .145 | .172 | .092 | .024 | .018 | .094 | .064 | .078 | .078 | .082 |
| PID-5 Distractibility | .92 (.20)*** | .65 (.20)*** | 1.62 (.41)*** | .74 (.20)*** | .93 (.50) | .21 (.14) | .66 (.13)*** | .11 (.07) | −.68 (.22)** | −.95 (.24)*** | −.62 (.21)** |
| PID-5 Impulsivity | .82 (.23)*** | .45 (.22)* | 1.53 (.47)*** | .20 (.22) | .72 (.57) | .07 (.16) | .01 (.15) | .17 (.09)* | .68 (.26)** | .80 (.27)** | .62 (.25)* |
| PID-5 Irresponsibility | .66 (.27)* | .76 (.26)** | 1.40 (.55)* | .52 (.26)* | .31 (.66) | .01 (.18) | .18 (.17) | .09 (.10) | .81 (.29)** | 1.69 (.31)*** | .96 (.29)*** |
| PID-5 Perfectionism | .37 (.16)* | .53 (.16)*** | .93 (.33)*** | .49 (.16)** | .94 (.41)* | .19 (.11) | .37 (.10)*** | .21 (.06)*** | .24 (.18) | −.17 (.19) | .56 (.18)** |
| PID-5 Risk-Taking | −.57 (.22)* | −.42 (.22) | −.10 (.45) | −.33 (.21) | .40 (.55) | −.09 (.15) | −.14 (.14) | −.01 (.08) | .57 (.24)* | .57 (.26)* | .71 (.24)** |
| R2 | .279 | .212 | .282 | .167 | .075 | .028 | .174 | .112 | .105 | .163 | .155 |
Note. N = 247–450.
p < .05,
p < .01,
p < .001.
The top of the table shows Cohen’s ds, comparing scores of those diagnosed with the specified disorder and those who were not. Unstandardized regression weights are shown in the bottom portion of the table, with standard errors in parentheses. DEP = major depression, PDD = persistent depressive disorder, PTSD = posttraumatic stress disorder, PAN = panic, AGOR = agoraphobia, SOC = social anxiety, OCD = obsessive-compulsive disorder, ALC = alcohol use, SUB = substance use, ASPD = antisocial personality disorder.
Table 4.
Zero-Order and Semipartial Correlations (Holding Constant Neuroticism/Negative Affectivity) of Conscientiousness/Disinhibition and its Facets with Symptoms
| Con./Dis. (domain) | Discipline/Distract. | Order/Perfect. | Dutiful./Irrespon. | Delib/Impul. | Achieve. | Comp. | Risk | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NEO | PID-5 | NEO | PID-5 | NEO | PID-5 | NEO | PID-5 | NEO | PID-5 | NEO | NEO | PID-5 | |
| MDD | −.36*** | .51*** | −.34*** | .47*** | −.08 | .26*** | −.28*** | .41*** | −.27*** | .41*** | −.30*** | −.43*** | .06 |
| PDD | −.27*** | .43*** | −.25*** | .40*** | .01 | .27*** | −.24*** | .37*** | −.22*** | .34*** | −.23*** | −.35*** | .05 |
| PTSD | −.30*** | .52*** | −.27*** | .46*** | −.01 | .27*** | −.26*** | .43*** | −.30*** | .44*** | −.22*** | −.39*** | .16*** |
| GAD | −.17** | .36*** | −.21*** | .36*** | .03 | .25*** | −.14* | .30*** | −.08 | .26*** | −.14* | −.25*** | .02 |
| M distress disorders | −.28*** | .46*** | −.27*** | .42*** | −.01 | .26*** | −.23*** | .38*** | −.22*** | .36*** | −.22*** | −.36*** | .07 |
| Panic | −.07 | .25*** | −.09 | .22*** | −.01 | .18*** | .00 | .19*** | −.04 | .22*** | −.07 | −.10 | .11* |
| Agoraphobia | −.05 | .14*** | −.05 | .14** | .01 | .12** | −.04 | .10* | −.05 | .10* | −.10 | −.03 | .01 |
| Social anxiety | −.23*** | .35*** | −.21*** | .38*** | −.03 | .26*** | −.16* | .27*** | −.15* | .24*** | −.22*** | −.28*** | .02 |
| OCD | −.14* | .29*** | −.11 | .25*** | .00 | .25*** | −.09 | .23*** | −.18** | .27*** | −.09 | −.22*** | .11* |
| M fear disorders | −.12 | .26*** | −.12 | .25*** | −.01 | .20*** | −.07 | .20*** | −.11 | .21*** | −.12 | −.16** | .06 |
| Alcohol use | −.11 | .19*** | −.05 | .05 | .05 | .11* | −.19** | .21*** | −.19** | .25*** | −.01 | −.15* | .23*** |
| Substance use | −.13* | .25*** | −.08 | .07 | −.03 | .03 | −.23*** | .31*** | −.18** | .28*** | −.02 | −.10 | .25*** |
| ASPD | −.05 | .26*** | .00 | .11* | .12 | .21*** | −.17** | .27*** | −.22*** | .30*** | .03 | −.07 | .28*** |
| M external. disorders | −.10 | .23*** | −.04 | .08 | .05 | .12 | −.20*** | .26*** | −.20*** | .28*** | .00 | −.11 | .25*** |
|
| |||||||||||||
| Semipartial Correlations Controlling for Neuroticism/Negative Affectivity | |||||||||||||
| MDD | −.06 | .17*** | −.04 | .14*** | .00 | −.02 | −.04 | .13*** | −.03 | .12** | −.07 | −.09 | .01 |
| PDD | −.02 | .13** | −.01 | .10* | .07 | .03 | −.05 | .13** | −.03 | .08 | −.04 | −.09 | .00 |
| PTSD | −.03 | .17*** | .00 | .10** | .06 | −.01 | −.04 | .14*** | −.10 | .16*** | .00 | −.09 | .12** |
| GAD | .13* | .01 | .08 | .02 | .09 | −.01 | .09 | .03 | .14** | −.03 | .09 | .10 | −.02 |
| M distress disorders | .01 | .12** | .01 | .09 | .06 | .00 | −.01 | .11* | .00 | .08 | .00 | .00 | .03 |
| Panic | .14* | .01 | .11 | −.03 | .03 | .00 | .16** | −.01 | .11 | .02 | .09 | .15** | .08 |
| Agoraphobia | .04 | −.03 | .04 | −.01 | .03 | .01 | .04 | −.03 | .02 | −.03 | −.03 | .09 | −.01 |
| Social anxiety | .04 | .05 | .05 | .10* | .04 | .04 | .05 | .03 | .05 | −.02 | −.02 | .03 | −.01 |
| OCD | .03 | .11* | .07 | .06 | .04 | .10* | .05 | .08 | −.05 | .11* | .05 | −.03 | .08 |
| M fear disorders | .06 | .04 | .07 | .03 | .04 | .04 | .08 | .02 | .03 | .02 | .02 | .06 | .04 |
| Alcohol use | −.08 | .15** | −.02 | −.04 | .06 | .06 | −.18** | .17*** | −.18** | .22*** | .03 | −.14* | .23*** |
| Substance use | −.13* | .21*** | −.08 | −.03 | −.03 | −.05 | −.24*** | .28*** | −.18** | .25*** | −.01 | −.10 | .24*** |
| ASPD | −.01 | .18*** | .05 | −.02 | .14* | .13** | −.14* | .20*** | −.20** | .24*** | .08 | −.02 | .26*** |
| M external. disorders | −.07 | .18*** | −.02 | .02 | .06 | .05 | −.19*** | .22*** | −.19*** | .24*** | .03 | −.09 | .24*** |
Note. N = 244–455.
p < .05,
p < .01,
p < .001.
Correlations greater than or equal to |.30| are shown in boldface. Con. = Conscientiousness; Dis. = Disinhibition; Distract. = Distractibility; Perfect. = Perfectionism; Dutiful. = Dutifulness; Irrespon. = Irresponsibility; Delib. = Deliberation; Impul. = Impulsivity; Achieve. = Achievement; Comp. = Competence; Risk = Risk-Taking; MDD = major depression, PDD = persistent depressive disorder, PTSD = posttraumatic stress disorder, OCD = obsessive-compulsive disorder, ASPD = antisocial personality disorder, external. = externalizing.
To simplify the presentation of facet-level associations with symptom counts, we calculated mean correlations for each trait scale and symptom and collapsed estimates within the distress disorders (i.e., depression, persistent depressive disorder, PTSD, GAD), the fear disorders (i.e., panic, agoraphobia, social anxiety, OCD), and the externalizing disorders (i.e., alcohol use, substance use, ASPD). At the domain level, NEO PI-3 Conscientiousness and PID-5 Disinhibition were more strongly associated with the distress disorders than with the fear and externalizing disorders (zs ranged from 2.51 to 5.27, p < .01). Patterns of associations with symptoms generally were replicated across the paired facet scales from both inventories. Specifically, facets related to perceived self-efficacy (i.e., NEO PI-3 Discipline and PID-5 Distractibility, NEO PI-3 Dutifulness and PID-5 Irresponsibility, as well as NEO PI-3 facets Competence and Achievement) all were more closely associated with the distress disorders than with the fear or externalizing disorders (zs ranged from 1.96 to 9.07, p < .05), with the sole exception of NEO PI-3 Dutifulness. The distress disorders and fear disorders had stronger correlations with PID-5 Perfectionism than did the externalizing disorders (zs ranged from 2.02 to 2.66, p < .05), but the corresponding NEO facet (Order) was not significantly correlated with any of the symptoms. The last pair of facets, PID-5 Impulsivity and NEO PI-3 Deliberation, generally were more strongly associated with the distress disorders and externalizing disorders than with the fear disorders, though this difference was significant only for PID-5 Impulsivity (zs ranged from 2.19 to 3.77, p < .05). Finally, the only facet that was most strongly associated with the externalizing disorders was Risk-Taking (zs ranged from 3.41 to 5.46, p < .001).
Simultaneous regressions
To examine which facets were uniquely associated with symptoms, beyond shared higher-order variance among the facets, we next conducted separate simultaneous multiple regressions for the Conscientiousness/Disinhibition facets in each inventory, with each symptom dimension as the dependent variable (Table 3). As expected given the zero-order correlations, the PID-5 facets accounted for a larger proportion of the variance in symptoms than did the NEO PI-3 facets (R2 ranged from .018 to .196 for NEO PI-3, R2 ranged from .028 to .282 for PID-5). In both inventories, analyses predicting depression, persistent depressive disorder, and PTSD yielded particularly large R2 values.
NEO PI-3 Competence was the primary (and often, sole) significant predictor for the distress disorders and for two of the fear disorders (i.e., social anxiety and OCD). In addition, several distress disorders had significant positive (suppressor) associations with Order, and low Discipline made a weak but significant contribution to predicting GAD. None of the NEO PI-3 facets were significant unique predictors of panic or of agoraphobia. Low Dutifulness was the primary predictor for the externalizing disorders, and ASPD was also predicted by low levels of Deliberation.
In contrast to the above analyses with NEO PI-3 facets as predictors, the PID-5 facets demonstrated more unique associations with symptoms. The distress disorders all were significantly predicted by PID-5 Distractibility, Impulsivity, Irresponsibility, and Perfectionism; the only exception was that Impulsivity did not significantly predict symptoms of GAD. Depression also was predicted by low levels of Risk-Taking. The primary predictor for the fear disorders was Perfectionism, with Distractibility contributing to social anxiety and Impulsivity to OCD. Last, the externalizing disorders all were significantly and positively predicted by Impulsivity, Irresponsibility, and Risk-Taking, and negatively predicted by Distractibility; in addition, ASPD was predicted by Perfectionism.
Test of the Demoralization Hypothesis
To test the demoralization hypothesis, we computed semipartial correlations between each facet and symptoms, accounting for levels of NEO PI-3 Neuroticism or PID-5 Negative Affectivity as a proxy for demoralization. Results are shown in the bottom portion of Table 4. For the internalizing disorders, semipartial correlations were reduced in magnitude relative to the corresponding zero-order correlations, suggesting that demoralization contributes to the conscientiousness-internalizing association. These correlations were reduced to non-significance for most of the fear disorders, but numerous significant small to medium effect sizes remained for the distress disorders. Specifically, all of the distress disorders except GAD remained significantly associated with PID-5 Disinhibition, Distractibility, and Irresponsibility. In addition, PTSD and MDD were associated with PID-5 Impulsivity, and PTSD was also associated with PID-5 Risk-Taking. Both GAD and panic only had a few significant positive (suppressor) associations with NEO scales. Among the fear disorders, OCD remained significantly associated with PID-5 Disinhibition, Perfectionism, and Impulsivity in the expected direction.
In contrast to the internalizing disorders, the semipartial correlations between the externalizing disorders and traits after accounting for Neuroticism/Negative Affectivity were not substantially reduced (compared to the zero-order correlations), indicating that demoralization did not contribute more than negligibly to this association. All three externalizing disorders remained significantly and moderately associated with PID-5 Disinhibition, NEO Dutifulness and PID-5 Irresponsibility, NEO Deliberation and PID-5 Impulsivity, and PID-5 Risk-Taking. ASPD also was associated positively with the NEO Order/PID-5 Perfectionism pair.
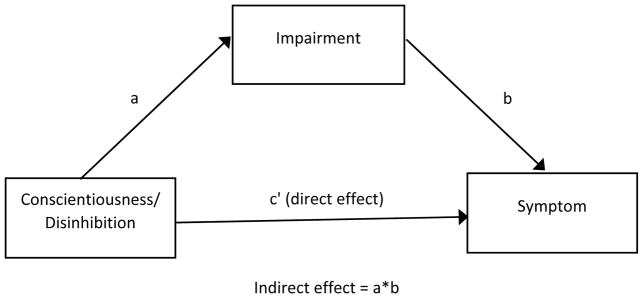
Test of the Impairment Mediation Hypothesis
Mediation analyses were conducted to examine the size and significance of the indirect effects of conscientiousness/disinhibition on each symptom via impairment (i.e., the association of conscientiousness with symptoms that is due to impairment), as well as the direct effects of conscientiousness/disinhibition on each symptom (i.e., the association of conscientiousness with symptoms that is due to sources other than impairment) (see Figure 1). Partial mediation occurs when there are significant direct and indirect effects, whereas full mediation occurs when the indirect effect entirely accounts for the association (that is, there is not a significant direct effect).
Figure 1.
Mediation Model for Conscientiousness/Disinhibition, Symptoms, and Impairment
Results are shown in Table 5, including 95% bias-corrected confidence intervals around the indirect effects. Findings were similar across both inventories for the internalizing disorders. Specifically, impairment partially mediated the association between conscientiousness/disinhibition and most of the distress disorders; an exception was that impairment fully mediated the association of GAD with NEO PI-3 Conscientiousness. For the fear disorders, impairment partially mediated (in the case of PID-5 analyses predicting panic, social anxiety, and OCD) or fully mediated (all other fear disorder analyses) the association between conscientiousness/disinhibition and symptoms.
Table 5.
Direct and Indirect Effects of Conscientiousness/Disinhibition on Symptoms via Impairment, with and without Controlling for Neuroticism/Negative Affectivity
| N | a | b | c′ | Indirect effect | 95% CIindirect | R2 | |
|---|---|---|---|---|---|---|---|
| MDD (NEO) | 257 | −.195 (.039)*** | .082 (.007)*** | −.016 (.005)*** | −.016* | −.022, −.011 | .120 |
| MDD (PID) | 450 | 5.317 (.486)*** | .072 (.005)*** | .415 (.062)*** | .382* | .034, .466 | .251 |
| PDD (NEO) | 255 | −.196 (.039)*** | .070 (.007)*** | −.009 (.005)* | −.014* | −.019, −.009 | .071 |
| PDD (PID) | 447 | 5.344 (.487)*** | .052 (.006)*** | .356 (.065)*** | .275* | .212, .346 | .186 |
| PTSD (NEO) | 254 | −.195 (.039)*** | .160 (.015)*** | −.024 (.010)* | −.031* | −.044, −.021 | .090 |
| PTSD (PID) | 444 | 5.264 (.491)*** | .111 (.011)*** | 1.068 (.133)*** | .584* | .434, .752 | .268 |
| GAD (NEO) | 257 | −.195 (.039)*** | .050 (.008)*** | −.004 (.005) | −.010* | −.014, −.006 | .029 |
| GAD (PID) | 450 | 5.317 (.486)*** | .042 (.006)*** | .297 (.067)*** | .221* | . 158, .294 | .133 |
| PAN (NEO) | 257 | −.195 (.039)*** | .119 (.019)*** | .009 (.012) | −.023* | −.034, −.015 | .005 |
| PAN (PID) | 450 | 5.317 (.486)*** | .097 (.015)*** | .347 (.170)* | .518* | .359, .698 | .062 |
| AGOR (NEO) | 257 | −.195 (.039)*** | .018 (.005)*** | .001 (.003) | −.004* | −.006, −.001 | .003 |
| AGOR (PID) | 450 | 5.317 (.486)*** | .020 (.004)*** | .019 (.048) | .107* | .063, .160 | .018 |
| SOC (NEO) | 257 | −.195 (.039)*** | .037 (.005)*** | −.005 (.003) | −.007* | −.011, −.004 | .050 |
| SOC (PID) | 450 | 5.317 (.486)*** | .072 (.004)*** | .187 (.045)*** | .145* | .100, .196 | .123 |
| OCD (NEO) | 257 | −.195 (.039)*** | .013 (.003)*** | −.002 (.002) | −.003* | −.004, −.001 | .021 |
| OCD (PID) | 450 | 5.317 (.486)*** | .006 (.002)** | .122 (.026)*** | .032* | .010, .058 | .087 |
| ALC (NEO) | 257 | −.195 (.039)*** | −.013 (.009) | −.012 (.006)* | .003* | .001, .006 | .012 |
| ALC (PID) | 450 | 5.317 (.486)*** | −.019 (.007)** | .402 (.082)*** | −.103* | −.175, −.038 | .036 |
| SUB (NEO) | 256 | −.195 (.039)*** | −.001 (.010) | −.013 (.006)* | .000 | −.004, .004 | .016 |
| SUB (PID) | 447 | 5.306 (.488)*** | −.003 (.008) | .440 (.089)*** | −.016 | −.095, .062 | .061 |
| ASPD (NEO) | 257 | −.195 (.039)*** | .015 (.009) | .002 (.006) | −.002 | −.007, .001 | .000 |
| ASPD (PID) | 450 | 5.317 (.486)*** | .015 (.007)* | .265 (.080)*** | .081* | .011, .162 | .050 |
|
| |||||||
| Controlling for Neuroticism/Negative Affectivity | |||||||
| MDD (NEO) | 257 | −.047 (.045) | .070 (.007)*** | −.002 (.005) | −.003 | −.009, .002 | .293 |
| MDD (PID) | 450 | 2.958 (.644)*** | .065 (.005)*** | .178 (.075)* | .191* | .114, .278 | .335 |
| PDD (NEO) | 255 | −.047 (.045) | .061 (.007)*** | .001 (.005) | −.003 | −.007, .002 | .195 |
| PDD (PID) | 447 | 3.008 (.650)*** | .045 (.006)*** | .125 (.079) | .135* | .077, .203 | .259 |
| PTSD (NEO) | 254 | −.049 (.045) | .137 (.015)*** | .001 (.011) | −.007 | −.018, .004 | .237 |
| PTSD (PID) | 444 | 2.944 (.648)*** | .093 (.011)*** | .468 (.157)** | .274* | .155, .455 | .364 |
| GAD (NEO) | 257 | −.047 (.045) | .031 (.008)*** | .015 (.005)** | −.002 | −.005, .001 | .257 |
| GAD (PID) | 450 | 2.958 (.644)*** | .031 (.006)*** | −.068 (.078) | .091* | .048, .148 | .273 |
| PAN (NEO) | 257 | −.047 (.045) | .091 (.019)*** | .039 (.014)** | −.004 | −.013, .002 | .129 |
| PAN (PID) | 450 | 2.958 (.644)*** | .079 (.015)*** | −.266 (.206) | .234* | .123, .379 | .140 |
| AGOR (NEO) | 257 | −.047 (.045) | .016 (.005)** | .003 (.004) | −.001 | −.002, .001 | .025 |
| AGOR (PID) | 450 | 2.958 (.644)*** | .017 (.004)*** | −.089 (.059) | .050* | .023, .091 | .054 |
| SOC (NEO) | 257 | −.047 (.045) | .028 (.005)*** | .005 (.004) | −.001 | −.004, .001 | .214 |
| SOC (PID) | 450 | 2.958 (.644)*** | .022 (.004)*** | −.003 (.054) | .064* | .033, .106 | .218 |
| OCD (NEO) | 257 | −.047 (.045) | .009 (.003)** | .002 (.002) | −.000 | −.002, .000 | .092 |
| OCD (PID) | 450 | 2.958 (.644)*** | .004 (.002) | .067 (.032)* | .013* | .002, .029 | .111 |
| ALC (NEO) | 257 | −.047 (.045) | −.015 (.009) | −.009 (.007) | .001 | −.000, .003 | .011 |
| ALC (PID) | 450 | 2.958 (.644)** | −.020 (.007)** | .385 (.101)*** | −.059* | −.113, −.020 | .037 |
| SUB (NEO) | 256 | −.045 (.045) | .002 (.011) | −.016 (.007)* | −.000 | −.002, .001 | .019 |
| SUB (PID) | 447 | 2.852 (.648)*** | −.002 (.008) | .492 (.111)*** | −.004 | −.051, .041 | .062 |
| ASPD (NEO) | 257 | −.047 (.045) | .014 (.010) | .003 (.007) | −.001 | −.003, .000 | .003 |
| ASPD (PID) | 450 | 2.958 (.634)*** | .015 (.007)* | .275 (.100)** | .046* | .006, .108 | .051 |
p < .05,
p < .01,
p < .001.
MDD = major depression, PDD = persistent depressive disorder, PTSD = posttraumatic stress disorder, PAN = panic, AGOR = agoraphobia, SOC = social anxiety, OCD = obsessive-compulsive disorder, ALC = alcohol use, SUB = substance use, ASPD = antisocial personality disorder, IMP = impairment. See Figure 1 for the specification of path coefficients (a, b, c′, indirect effect).
Evidence of mediation was less consistent for the externalizing disorders. Specifically, conscientiousness/disinhibition had only direct effects on substance use. The association between conscientiousness/disinhibition and alcohol use was partially mediated by impairment, but notably the indirect effects were in the opposite direction of the direct effect (e.g., higher levels of conscientiousness were indirectly associated with higher levels of substance use). Impairment fully mediated the association between PID-5 Disinhibition and ASPD, but there were no significant direct or indirect effects in the parallel analysis with NEO Conscientiousness.
We also conducted mediation analyses with Neuroticism/Negative Affectivity as a covariate, to test the unique roles of impairment and demoralization in the conscientiousness-disorder association. Results are shown in the bottom portion of Table 5. The only remaining significant direct or indirect effect in NEO PI-3 analyses was a direct suppressor association with panic and GAD, and a direct effect for substance use. In contrast, impairment fully mediated the association between PID-5 Disinhibition and most of the distress and fear disorders, and impairment partially mediated the association for MDD, PTSD, and OCD. Finally, the associations of PID-5 Disinhibition with alcohol use and ASPD were partially mediated by impairment, whereas Disinhibition had a direct effect only on substance use. As in the analyses without a covariate, lower levels of Disinhibition were indirectly associated with greater alcohol use.
Discussion
The aims of this study were to clarify which specific conscientiousness/disinhibition facets are primarily responsible for the observed domain-level associations with the internalizing and externalizing disorders, as well as to test the roles of demoralization and functional impairment in explaining these associations in a psychiatric sample. With regard to the first aim, results generally were consistent with our hypotheses and the prior literature (e.g., Bienvenu et al., 2004; Hayward et al., 2013; Rector et al., 2002, 2012; Ruiz et al., 2008). Though the magnitude of associations differed across personality inventories, it is important to note that the pattern of effects was similar across measures, providing an internal replication of results and increased confidence that findings are not idiosyncratic to a particular instrument. Within the internalizing disorders, the distress disorders were most closely related to core conscientiousness facets assessing perceived self-efficacy (e.g., Competence, Distractibility), as were some of the fear disorders (i.e., social anxiety, OCD). In contrast, externalizing disorders were specifically associated with facets involving risk-taking and disregard of rules. Finally, facets assessing perfectionism and impulsivity were broadly and similarly associated with most of the disorders studied here. Associations generally remained in regression analyses that statistically controlled for the shared variance among facets, providing evidence for the relevance of the unique predictive value of these facets. These results emphasize the importance of examining conscientiousness-psychopathology associations at the facet-level, as domain-level analyses are likely to obscure heterogeneous and differential associations with symptoms.
It is striking that the strongest facet correlates of the distress disorders (and some fear disorders) had secondary associations with neuroticism/negative affectivity, whereas the strongest facet correlates of the externalizing disorders had secondary associations with agreeableness/antagonism (see Table 2). Structural analyses of the Big Five have found evidence of two higher-order factors, one of which (called Alpha or Stability) consists of the covariance among (low) neuroticism, conscientiousness, and agreeableness (e.g., Digman, 1997; Markon, Krueger, & Watson, 2005). These analyses, consistent with research linking internalizing disorders to high neuroticism and externalizing disorders to low agreeableness (e.g., Kotov et al., 2010), suggest that the conscientiousness content associated with distress disorders and externalizing disorders is tipped towards neuroticism and towards agreeableness, respectively.
Our second aim was to test whether demoralization (operationalized here as neuroticism) accounts for or contributes to the association between conscientiousness and disorders. That is, is the conscientiousness-disorder association primarily or partially due to concomitant demoralization, which is associated with the belief that one is generally not competent or effective in life and is reflected in relevant conscientiousness facet ratings? There was evidence to support this hypothesis for the internalizing disorders, as correlational analyses between facets and internalizing disorders that controlled for neuroticism/negative affectivity largely were non-significant (in the case of the NEO) or substantially reduced (PID-5). Thus, aligned with the results of Kotov et al. (2010), it appears that demoralization/neuroticism substantially contributes to but does not entirely explain the conscientiousness-internalizing association. In particular, significant domain and facet-level associations (i.e., Distractibility, Irresponsibility) remained for most of the distress disorders and for OCD. In contrast, partial correlations with the externalizing disorders remained largely unchanged, suggesting that demoralization does not play a major role in the conscientiousness-externalizing link. This is consistent with prior results indicating that demoralization and neuroticism are more closely related to the internalizing disorders than to the externalizing disorders (e.g., Noordhof et al., 2015).
A third aim was to examine whether impairment mediated the association between conscientiousness and disorders; we discuss findings for internalizing and externalizing disorders separately here due to different patterns of results. We found support for this hypothesis for the internalizing disorders (both distress and fear) across both inventories, as significant indirect effects were consistently present. These results may explain why conscientiousness is more strongly linked to internalizing disorder vs. control status (wherein the groups have clear mean level differences in impairment) than with internalizing symptom severity (which may not precisely covary with degree of impairment). In general, direct effects from conscientiousness to symptoms were present for most distress disorders but not for most fear disorders, indicating that other unmeasured processes contributed to the conscientiousness-disorder association in distress disorders but impairment largely accounted for the association in the fear disorders. After holding constant levels of neuroticism, impairment was still a significant mediator for analyses involving the PID-5 (but not the NEO), and most direct effects between conscientiousness and distress disorders were eliminated in the PID-5 analyses. Thus, it appears that demoralization/neuroticism may be responsible for much of the remaining association between conscientiousness and the distress disorders, after accounting for the role of impairment. Importantly, both demoralization and impairment accounted for unique variance in this association, suggesting that the conscientiousness-internalizing disorder link is not primarily or solely due to demoralization and overly negative self-perceptions, but rather is also accounted for by fairly objective difficulties in different domains of daily functioning (rated by an interviewer) that are associated with participants’ ratings of their conscientiousness.
Although causal associations cannot be inferred from these cross-sectional data, the results of the mediation analyses are consistent with the hypothesis that low conscientiousness leads to problems in daily functioning, which in turn lead to internalizing symptoms such as depression and anxiety. However, it will be important for future studies to examine the temporal dynamics and precedence of these constructs. Specifically, both long-term longitudinal designs (e.g., several assessments over the course of 5 years) and intensive longitudinal methods (e.g., day-to-day associations over one month) are needed to clarify whether low conscientiousness is truly a risk factor for impairment and subsequent psychopathology. If longitudinal studies do not reveal such temporal precedence, it is possible that low ratings of facets such as self-efficacy primarily reflect the (perhaps accurate) perception that one is currently struggling in daily life, rather than implying any causal role. On the other hand, if low conscientiousness is truly a temporal risk factor for these symptoms, this may be a novel target for intervention and treatment efforts. In addition, different plausible models with alternate temporal orderings (e.g., impairment could lead to disorders via low conscientiousness; disorders could lead to low conscientiousness via impairment; disorders could lead to impairment via low conscientiousness) should be compared to draw precise conclusions about how these processes unfold over time.2
In contrast to the internalizing disorders, the externalizing disorders showed consistent direct effects from conscientiousness, but less consistent evidence for mediation via impairment, suggesting that their association with conscientiousness is primarily due to processes other than impairment (or demoralization). In particular, there were significant indirect effects for alcohol use disorders, but these were in a counterintuitive direction, such that higher levels of conscientiousness were indirectly associated with greater alcohol use symptoms. Overall, these findings indicate that tendencies such as irresponsibility, impulsivity, and risk-taking are not necessarily associated with externalizing symptoms due to impairment, but rather a temperamental tendency towards short-term reward-seeking may directly increase the likelihood of problematic substance use and antisocial or risk behavior (e.g., Geier. 2013). However, it is also plausible that those with marked externalizing symptoms may have been less likely to report or to have insight into impairment in their functioning, as compared to those with primarily internalizing symptoms. Furthermore, Table 4 indicates that domain-level conscientiousness score in these inventories more heavily include content relevant to internalizing than to externalizing disorders, which may have influenced the mediation analyses.
Our results have assessment implications for researchers and clinicians. Specifically, domain-level associations are likely to vary depending on which conscientiousness facets a specific domain-level instrument taps most heavily, as well as the extent to which these facets correlate with neuroticism or agreeableness. It is notable that the NEO consistently yielded weaker associations with symptoms than did the PID-5. Prior studies have not compared these two measures in relation to internalizing and externalizing symptoms, so it is unclear to what extent these results may generalize to other samples and this effect needs to be replicated. However, one obvious difference between the measures is that they are keyed in opposite directions, with the NEO designed to assess normal personality and PID-5 to assess abnormal personality. Thus, it is plausible that the PID-5 may provide better assessment of abnormal traits that are most relevant to psychopathology. But counter to this assertion, a study found that the conscientiousness/disinhibition domains of these two measures did not markedly differ in terms of item difficulty or discrimination (Suzuki et al., 2015). Another possibility is that the smaller sample size for the NEO analyses and/or lower reliability of these facets our data may have attenuated associations. However, the scale reliability does not appear to account substantially for the observed discrepancy, as posthoc analyses that disattenuated correlations for measure unreliability did not impact the differential magnitudes of correlations. It is also notable that accounting for neuroticism generally eliminated conscientiousness-internalizing disorder associations for the NEO but not the PID-5, suggesting that the NEO conscientiousness facets may be more heavily saturated with content relevant to demoralization/general negative affect. Overall, these results indicate that researchers should select the specific personality measures with care depending on which components of conscientiousness are of most interest, and it may be helpful to include multiple inventories to examine robustness of patterns (and magnitudes) of associations across inventories.
Strengths of this study include the use of a heterogeneous clinical sample, in which we simultaneously examined multiple disorders across two inventories, and a direct test of two processes that may explain the conscientiousness-disorder association. In addition, inflation of associations due to shared method variance was minimized by using self-reported personality traits and clinical interview assessments of disorders and impairment. However, several limitations also should be considered when interpreting these results. First, as described previously, the cross-sectional design of this study does not allow us to conclude whether symptoms negatively impact functioning or whether problems with functioning lead to psychopathology (or both). Second, we did not have observer reports or objective behavioral coding of personality, impairment, or symptoms. It is also important to note that our samples size varied by measure and disorder, and the internal consistency of some NEO facets was low, such that there was likely greater error variance in some analyses than others. Finally, we examined the frequency/severity of antisocial behavior and substance use, but not the function of these behaviors. Future studies should examine whether associations of externalizing behavior with conscientiousness and impairment may vary depending on whether the behaviors primarily serve to reduce negative affect or to increase positive affect.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. Preparation of this manuscript was supported by a grant from the National Institute of Mental Health (R01 MH080086, Simms). The opinions expressed are solely those of the authors and not necessarily those of the funding source.
Footnotes
Note that Kotov et al. corrected for the unreliability of each personality measure in their analyses, whereas Ruiz et al. did not, likely contributing to the smaller effect sizes found by Ruiz et al.
We examined analyses testing a model wherein symptoms predict conscientiousness via impairment (i.e., a scar model) in our data. The pattern of results was similar to that of the mediator analyses reported in Table 5: nearly all of the models that included internalizing symptoms had significant indirect effects of impairment, whereas those that included externalizing symptoms generally did not. Thus, these analyses reinforce the fact that our findings are consistent with several models and cannot firmly distinguish between them.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Bienvenu OJ, Samuels JF, Costa PT, Reti IM, Eaton WW, Nestadt G. Anxiety and depressive disorders and the five-factor model of personality: A higher- and lower-order personality trait investigation in a community sample. Depression and Anxiety. 2004;20:92–97. doi: 10.1002/da.20026. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts BW. The case for conscientiousness: Evidence and implications for a personality trait marker of health and longevity. Annals of Behavioral Medicine. 2013;45:278–288. doi: 10.1007/s12160-012-9454-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chioqueta AP, Stiles TC. Personality traits and the development of depression, hopelessness, and suicide ideation. Personality and Individual Differences. 2005;38:1283–1291. [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Digman JM. Higher-order factors of the Big Five. Journal of Personality and Social Psychology. 1997;73:1246–1256. doi: 10.1037//0022-3514.73.6.1246. [DOI] [PubMed] [Google Scholar]
- Geier CF. Adolescent cognitive control and reward processing: Implications for risk taking and substance use. Hormones and Behavior. 2013;64:333–342. doi: 10.1016/j.yhbeh.2013.02.008. [DOI] [PubMed] [Google Scholar]
- Griffin SA, Samuel DB. A closer look at the lower-order structure of the Personality Inventory for DSM-5: Comparison with the five-factor model. Personality Disorders: Theory, Research, and Treatment. 2014;5:406–412. doi: 10.1037/per0000074. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hayward RD, Taylor WD, Smoski MJ, Steffens DC, Payne ME. Association of five-factor model personality domains and facets with presence, onset, and treatment outcomes of major depression in older adults. American Journal of Geriatric Psychiatry. 2013;1:88–96. doi: 10.1016/j.jagp.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SC, Levinson CA, Rodebaugh TL, Menatti A, Weeks JW. Social anxiety and the Big Five personality traits: The interactive relationship of trust and openness. Cognitive Behaviour Therapy. 2015;44:212–222. doi: 10.1080/16506073.2015.1008032. [DOI] [PubMed] [Google Scholar]
- Karsten J, Penninx BW, Verboom CE, Nolen WA, Hartman CA. Course and risk factors of functional impairment in subthreshold depression and anxiety. Depression and Anxiety. 2013;30:386–394. doi: 10.1002/da.22021. [DOI] [PubMed] [Google Scholar]
- Kenny DA. Statistics for the social and behavioral sciences. Boston: Little, Brown; 1987. [Google Scholar]
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine. 2012;42:1879–1890. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Verges A, Wood PD, Sher KJ. Transactional models between personality and alcohol involvement: a further examination. Journal of Abnormal Psychology. 2012;121:778–783. doi: 10.1037/a0026912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Brief versions of the NEO PI-3. Journal of Individual Differences. 2007;28:116–128. [Google Scholar]
- McCrae RR, Costa PT, Martin TA. The NEO PI-3: A more readable Revised NEO Personality Inventory. Journal of Personality Assessment. 2005;84:261–270. doi: 10.1207/s15327752jpa8403_05. [DOI] [PubMed] [Google Scholar]
- Mezquita L, Ibanez MI, Villa H, Fananas L, Moya-Higueras J, Ortet G. Five-factor model and internalizing and externalizing syndromes: A 5-year prospective study. Personality and Individual Differences. 2015;79:98–103. [Google Scholar]
- Noordhof A, Sellbom M, Eigenhuis A, Kamphuis JH. Distinguishing between demoralization and specific personality traits in clinical assessment with the NEO PI-R. Psychological Assessment. 2015;27:645–656. doi: 10.1037/pas0000067. [DOI] [PubMed] [Google Scholar]
- Quinn PD, Stappenbeck CA, Fromme K. Collegiate heavy drinking prospectively predicts change in sensation-seeking and impulsivity. Journal of Abnormal Psychology. 2011;120:543–556. doi: 10.1037/a0023159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Bogg T. A longitudinal study of the relationships between conscientiousness and the social environmental factors and substance use behaviors that influence health. Journal of Personality. 2004;72:325–353. doi: 10.1111/j.0022-3506.2004.00264.x. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives in Psychological Science. 2007;2:313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector NA, Bagby RM, Huta V, Ayearst L. Examination of the trait facets in the five-factor model in discriminating specific mood and anxiety disorders. Psychiatry Research. 2012;199:131–139. doi: 10.1016/j.psychres.2012.04.027. [DOI] [PubMed] [Google Scholar]
- Rector NA, Hood K, Richter MA, Bagby RM. Obsessive-compulsive disorder and the five-factor model of personality: Distinction and overlap with major depressive disorder. Behaviour Research and Therapy. 2002;40:1205–1219. doi: 10.1016/s0005-7967(02)00024-4. [DOI] [PubMed] [Google Scholar]
- Ruiz MA, Pincus AL, Schinka JA. Externalizing pathology and the five-factor model: a meta-analysis of personality traits associated with antisocial personality disorder, substance use disorder, and their co-occurrence. Journal of Personality Disorders. 2008;22:365–388. doi: 10.1521/pedi.2008.22.4.365. [DOI] [PubMed] [Google Scholar]
- Sellbom M, Ben-Porath YS, Bagby RM. Personality and psychopathology: Mapping the MMPI-2 Restructured Clinical (RC) scales onto the five factor model of personality. Journal of Personality Disorders. 2008;22:291–312. doi: 10.1521/pedi.2008.22.3.291. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecubrier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Supp 20):22–33. [PubMed] [Google Scholar]
- Simms LJ, Goldberg LR, Roberts JE, Watson D, Welte J, Rotterman JH. Computerized adaptive assessment of personality disorder: Introducing the CAT-PD project. Journal of Personality Assessment. 2011;93:380–389. doi: 10.1080/00223891.2011.577475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T, Samuel DB, Pahlen S, Krueger RF. DSM-5 alternative personality disorder model traits as maladaptive extreme variants of the five-factor model: An item-response theory analysis. Journal of Abnormal Psychology. 2015;124:343–354. doi: 10.1037/abn0000035. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In: Tuma AH, Masere JS, editors. Anxiety and Anxiety Disorders. Hillsdale, NJ: Erlbaum; 1984. pp. 681–706. [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM–V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their r relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Watson D, Naragon-Gainey K. Personality, emotions, and the emotional disorders. Clinical Psychological Science. 2014;2:422–442. doi: 10.1177/2167702614536162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment. 2014;5:43–54. doi: 10.1037/per0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]