Abstract
Background
Red eye can arise as a manifestation of many different systemic and ophthalmological diseases. The physician whom the patient first consults for this problem is often not an ophthalmologist. A correct assessment of the urgency of the situation is vitally important for the planning of further diagnostic evaluation and treatment.
Methods
This review is based on pertinent publications retrieved by a selective literature search in PubMed in August 2016 as well as on the authors’ own clinical and scientific experience.
Results
Primary care physicians typically see 4–10 patients per week who complain of ocular symptoms. Most of them have red eye as the major clinical finding. A detailed history, baseline ophthalmological tests, and accompanying manifestations can narrow down the differential diagnosis. The duration and laterality of symptoms (uni- vs. bilateral) and the intensity of pain are the main criteria allowing the differentiation of non-critical changes that can be cared for by a general practitioner from diseases calling for elective referral to an ophthalmologist and eye emergencies requiring urgent ophthalmic surgery.
Conclusion
The differential diagnosis of red eye can be narrowed down rapidly with simple baseline tests and targeted questioning. Patients with ocular emergencies should be referred to an ophthalmologist at once, as should all patients whose diagnosis is in doubt.
Every physician has been faced with the symptom “red eye” (1– 3). According to one study, eye problems are the reason for 2 to 3% of visits to primary care physicians and emergency facilities (1). This corresponds to an average of 4 to 10 patients every week (2), the majority of whom have clinically apparent red eye (3). In general emergency rooms or in hospitals without a consulting ophthalmologist, non-specialists are confronted with the challenging decision of whether an urgent ophthalmological referral is necessary or not (1, 2). In the case of a foreign body event or other injury the patient should see an ophthalmologist immediately; the same applies if the cardinal symptom is pain, vision loss, rock-hard eyeball, or corneal involvement. An Australian study found that 64% of patients with red eye treated by primary care physicians were diagnosed incorrectly. In 10% of these cases there were serious clinical consequences (4). Another study from the same country concluded that literature for non-ophthalmologists is in short supply (5).
Learning goals
After reading this article the reader should be familiar with:
The most frequently occurring differential diagnoses of red eye,
the relevant questions to ask the patient and the basic investigations, and
how to proceed in order to assess the urgency of referral to an ophthalmologist for further examination.
History
Incidence.
According to one study, eye problems are the reason for 2 to 3% of visits to primary care physicians and emergency facilities.
In the normal eye the conjunctiva shows a network of very fine blood vessels and the underlying sclera is white. Hyperemia, vascular ectasia, or subconjunctival hemorrhage therefore stand out. The degree of pain and the extent, uni-/bilaterality, location, duration, and course of the reddening must be recorded, together with any accompanying symptoms. Figures 1 and 2, the Table, and eTables 1 and 2 are intended to help the non-specialist arrive at the correct diagnosis.
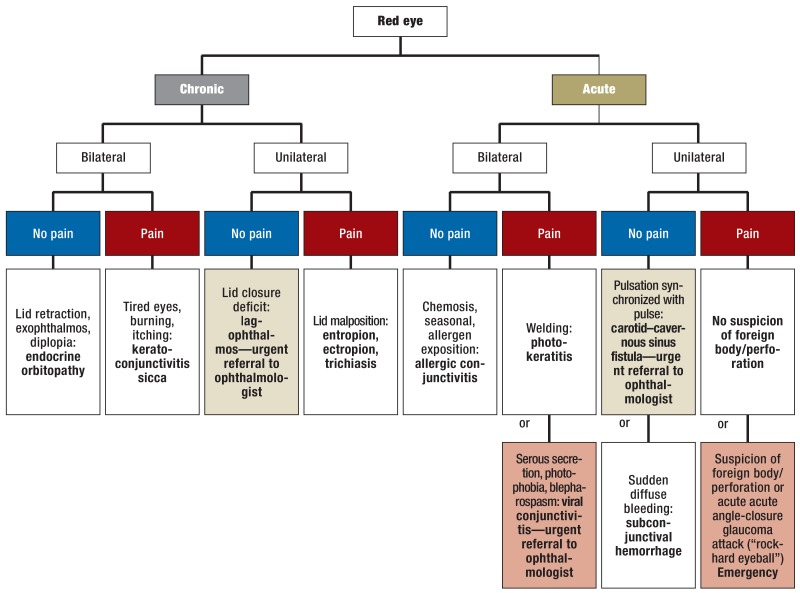
Figure 1.
Flow diagram for classification of red eye and its most frequently occurring causes
Flow diagram for differentiation and classification of causes of red eye for non-specialists. Bilateral findings often begin in one eye and affect the other eye later. “Emergency” means that immediate referral to an ophthalmologist is recommended. Figure modified from Cronau et al. (3)
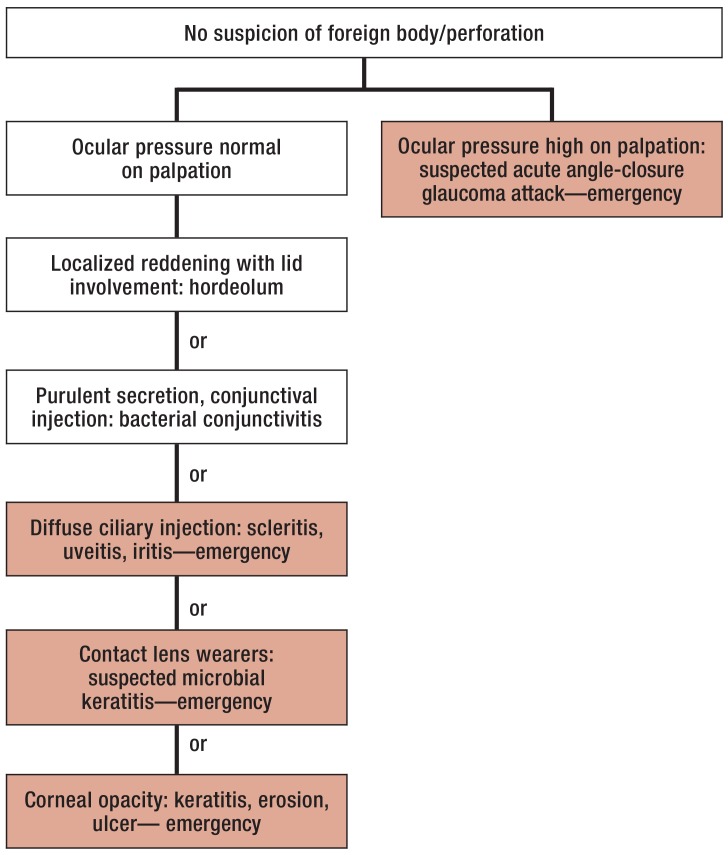
Figure 2.
Principal causes of unilateral acute red eye, in the absence of suspicion of foreign body/perforation
Table. Common ophthalmological terms used to describe the findings (in alphabetical order).
| Term | Meaning |
| Blepharospasm | Involuntary contraction/twitching of the eyelids |
| Chemosis | Glassy edema of the conjunctiva |
| Epiphora | Overflow of tear fluid |
| Halos | Colored rings around light sources |
| Injection | Vasodilatation with hyperemia |
| Lagophthalmos | Incomplete lid closure |
| Photophobia | Extreme sensitivity to light |
| Trichiasis | Chafing of the eyeball by inverted ‧lashes |
eTable 1. Classification of the causes of red eye by disease site.
| Characteristics | Diseases of the ocular surface | ||||||||
| Conjunctivitis | Allergy | Dry eye | Subconjunctival hemorrhage | Erosion | Corneal ulcer | Photokeratitis | Episcleritis/scleritis | ||
| Bacterial | Viral | ||||||||
| Incidence | +++ | + | +++ | +++ | + | ++ | – | ++ | – |
| (U)nilateral/ (B)ilateral |
U/B | U/B | B | B | U | U | U | B | U |
| Worsening of vision |
+ | +++ | + | + | – | ++ | ++ | +++ | + |
| Photophobia | (+) | +++ | + | (+) | – | + | + | +++ | + |
| (L)ocalized/ (D)iffuse reddening |
D | D | D | D | L | D | D | D | L |
| (S)uperficial/ (D)eep reddening |
S | S | S | S | S | S | S | S | S/D |
| Secretion: (P)urulent/ (W)atery/ (M)ucinous |
P | W | W | M/W | – | W | W/P | W | W |
| Conjunctival hemorrhage |
– | (+) | – | – | + | – | – | – | – |
| Conjunctival chemosis |
+ | +++ | ++ | – | – | – | – | +++ | (+) |
| Corneal lesions | (+) | – | (+) | + | – | + | ++ | + | – |
| Foreign body event |
– | – | – | – | + / – | + / – | – | – | – |
| Elevated ocular pressure |
– | – | – | – | – | – | – | – | – |
| Further features | Gradual onset, often initially unilateral | Extreme symptoms, first on one side and then bilaterally | Ask about causative agent, seasonal accumulation, general history: atopy | Chronic problem, often with a long history | Arterial hypertension, blood pressure crises, trauma, foreign body event | Trauma, foreign body, eyelid malposition, eyelid closure defect | Nerve palsy, eyelid malposition, eyelid closure defect | Welding in the previous 6–8 h | Frequently recurrent, deep injection of the sclera, investigate for systemic diseases |
| Urgency of definitive diagnosis | Normal referral to ophthalmologist | Immediate referral to ophthalmologist following notification and hygiene measures | Normal referral to ophthalmologist | Normal referral to ophthalmologist | Normal referral to ophthalmologist | Urgent referral to ophthalmologist | Emergency, consult ophthalmologist immediately | Normal referral to ophthalmologist | Urgent referral to ophthalmologist |
Incidence: +++ very often, ++ often, + occasionally, – rarely
Remainder of table: (+) may occur, +/– can occur with or without changes
eTable 2. Classification of the causes of red eye by disease site.
| Characteristics | Intraocular diseases | Diseases of the ocular adnexa | ||
|
Iritis/ iridocyclitis |
Acute angle-closure glaucoma |
Hordeolum |
Carotid–cavernous sinus fistula |
|
| Incidence | – | – | ++ | – |
| (U)nilateral/ (B)ilateral |
U | U | U | U |
| Worsening of vision |
++ | +++ | (+) | + |
| Photophobia | ++ | ++ | – | – |
| (L)ocalized/ (D)iffuse reddening |
D | D | + | D |
| (S)uperficial/ (D)eep reddening |
S/D | S/D | Eyelid | D |
| Secretion: (P)urulent/ (W)atery/ (M)ucinous |
– | – | P | – |
| Conjunctival hemorrhage |
– | – | – | – |
| Conjunctival chemosis |
(+) | – | – | (+) |
| Corneal lesions | – | + | – | – |
| Foreign body event |
– | – | – | – |
| Elevated ocular pressure |
– | +++ | – | + |
| Further features | Rheumatic underlying disease | Halos, extreme pain, flattened anterior chamber, opaque cornea, unresponsive pupil; NB: general symptoms | Localized reddening and swelling of the eyelids | Conjunctival tortuosity, headache, rushing sound, pulsatile exophthalmos |
| Urgency of definitive diagnosis | Urgent referral to ophthalmologist | Emergency, immediate referral to eye surgery center | Normal referral to ophthalmologist | Urgent referral to ophthalmologist |
Incidence: +++ very often, ++ often, + occasionally, – rarely
Remainder of table: (+) may occur, +/– can occur with or without changes
Diagnostic work-up
Diagnosis.
The duration and laterality of red eye and the presence and severity of pain are the cornerstones of diagnosis.
The diagnostic work-up begins with ascertaining whether the red eye is an acute or chronic phenomenon. “Acute” is understood to mean duration of 7 days or less (figure 1).
Diagnostic work-up.
Are both eyes affected?
Is the red eye chronic or acute?
Both eyes should always be examined, as the laterality of red eye may be relevant to the diagnosis. The patient should also be asked about the occurrence of pain. Duration, laterality, and the presence and severity of pain are the cornerstones of diagnosis. In a patient with painful acute unilateral red eye, presence of a foreign body must be ruled out. Any patient with a positive history of a foreign body or trauma should be referred as an emergency to an eye hospital. If no foreign body is suspected, the cornea must be inspected more closely. Superficial changes such as corneal erosion or deeper structural defects such as a corneal ulcer can often be discerned with the naked eye. If no such lesions are identified, the internal ocular pressure should be assessed by palpation, comparing the two eyes, to exclude an acute glaucoma attack (emergency). Should the internal ocular pressure be normal in a patient with painful acute unilateral red eye, one must consider inflammation of the sclera, uvea, or iris as a cause. Contact lens wearers who have painful acute unilateral red eye accompanied by diffuse ciliary injection and/or corneal opacity must be admitted for urgent treatment.
Conjunctivitis.
The typical signs are red eye and eyelids stuck together on waking.
Painful acute bilateral red eye is often caused by viral conjunctivitis. As a rule the affected patients show a serous/clear secretion (overflow of tears = epiphora), photophobia, and blepharospasm. This also constitutes an ophthalmological emergency.
Any patient with non-painful acute unilateral red eye should be seen by an ophthalmologist within 24 h for exclusion of a carotid–cavernous sinus fistula. Urgent ophthalmological referral is also advisable for pain-free chronic unilateral red eye with lagophthalmos. Moreover, any patient with red eyes soon after ocular surgery should be referred to an ophthalmologist immediately.
Disorders of the cornea and conjunctiva
The term conjunctivitis refers to an inflammation of the conjunctiva alone, while keratoconjunctivitis is used to mean inflammation of the cornea and conjunctiva together. In both conjunctivitis and keratoconjunctivitis there is an inflammatory process of the ocular surface with widening of blood vessels (conjunctival injection), cellular infiltration, and watery, slimy, or purulent exudation (6). The typical signs are red eye and eyelids stuck together on waking; the eye may show glassy edema (chemosis) (figure 3). The patient is particularly bothered by the sensation of a foreign body and a feeling of pressure, often in combination with photophobia and epiphora. If, in addition, an eyelid is affected by blepharospasm, corneal involvement is likely.
Figure 3.
Chemosis
Chemosis of the conjunctiva in infectious conjunctivitis
The many different possible causes of conjunctivitis (6) are divided into infectious and non-infectious factors. The latter include external irritants (smoke, dust, etc.), reduced production of tear fluid, eyelid malposition with mechanical irritation, and uncorrected refractive errors. The principal primary measure in the treatment of non-infectious conjunctivitis is avoidance of the triggering factor. Vasoconstrictive eye drops (active ingredient: tetrazoline) should be prescribed for no more than a few days as a supportive measure, because they treat only the symptoms, not the cause, and may lead to tachyphylaxis, as described over 20 years ago in a case series of 11 patients (7). The opinion of an ophthalmologist should be obtained.
Vasoconstrictive eye drops.
These should be prescribed for no more than a few days as a supportive measure, because they treat only the symptoms, not the cause, and may lead to tachyphylaxis.
Infectious conjunctivitis is generally bacterial or viral. In the German-speaking area most cases of bacterial conjunctivitis are caused by staphylococci, streptococci, or pneumococci (6, 8, 9). Pain, pronounced reddening of the eye, and a mucopurulent secretion with formation of a yellowish crust are the typical signs. In principle, any available antibiotic can be considered for topical treatment of acute bacterial conjunctivitis, as randomized controlled trials and meta-analyses have demonstrated similar treatment effects (3, e1– e4). Two frequently used topical agents are gentamycin (an aminoglycoside antibiotic) and ofloxacin (a fluorochinolone antibiotic). The recommended minimum dosage is 3 × daily for 5 days. If no improvement is seen after 5 days, the patient should be be referred to an ophthalmologist for urgent investigation.
Contact lens wearers
Contact lens wearers often suffer from a special form of bacterial (kerato-)conjunctivitis. For example, they may be infected with acanthomoebae or Pseudomonas aeruginosa (10, 11). Particularly with pseudomonads, hyperacute red eye with corneal ulceration may occur. The ulcer typically shows greenish-yellow mucus. The pathogens are frequently found in the contact lens fluid and/or container, and are often resistant to commonly used antibiotics. For timely diagnosis, the patient must provide the unwashed contact lens container together with the fluid and the lens itself and an ophthalmologist must obtain a direct swab from the focus of infection for microbiological analysis as part of an urgent ophthalmological consultation. Microbial keratitis can lead after just a few hours to corneal perforation and permanent visual loss or even to morphological loss of the eye (10). Keratoplasty “à chaud” (therapeutic corneal transplantation) with a prognosis of reduced visual acuity is then often the only possible form of treatment, as confirmed by a large retrospective case–control study published in 2015 (11). If corneal perforation is suspected, the eye should be protected by a non-compressive dressing with a compress secured at forehead and cheek.
Viral conjunctivitis
Contact lens wearers.
Contact lens wearers often suffer from a special form of bacterial (kerato-)conjunctivitis. For confirmation of diagnosis, the unwashed contact lens container together with the fluid and the lens itself must be analyzed for pathogens.
In contrast to bacterial conjunctivitis, bilateral red eye with a watery mucous secretion and itching should always arouse suspicion of a viral agent or an allergy. Viral conjunctivitis begins in one eye. Viral infection (most often by herpes simplex virus [12]) is accompanied by typical groups of herpetiform vesicles on reddened skin around the eye. In contrast to infection with varicella zoster virus, the skin lesions seen with herpes simplex do not respect the boundaries between dermatomes. Herpes simplex infection of the eye almost always represents a recurrence—the primary infection is often occult. Keratitis caused by fungi (keratomycosis) can only be confirmed by ophthalmological and microbiological investigation (e5).
Viral conjunctivitis.
Viral eye diseases such as epidemic keratoconjunctivitis are highly contagious. They tend to be seasonal, caused by smear infection with adenoviruses, and manifest after an incubation period of 8 to 10 days.
Viral eye diseases such as epidemic keratoconjunctivitis are highly contagious (13, 14). They tend to be seasonal, caused by smear infection with adenoviruses, and manifest after an incubation period of 8 to 10 days (15). A patient with all the symptoms suffers severe pain in both eyes, accompanied by itching, light sensitivity, reddening, and tear overflow. Healing generally occurs after 2 weeks, usually with no consequences (15). Avoidance of contact is crucial: no handshakes, no sharing of the same flannel or towel, and strict observance of hygiene. All areas of the treating physician’s office entered by the patient must be decontaminated according to specific hygiene/disinfection standards. To prevent transmission, patients with red eye should be asked to wait in a separate room and should be given disposable gloves. The patient must strictly avoid contact with other people until the diagnosis is confirmed by an ophthalmologist and should not go to work. When a patient is referred for confirmation of the diagnosis, information should be provided in a brief telephone call. German law (§ 7, para. 1 of the Infection Protection Act) stipulates notification of the identity of the patient to the local health authority within 24 h of the direct demonstration of adenovirus in a conjunctival swab (e6). While epidemic keratoconjunctivitis is treated topically with moistening agents (15), herpetic (kerato-)conjunctivitis is treated topically and/or orally with a virostatic agent (e7– e10).
Non-infectious (kerato-)conjunctivitis
Infection prophylaxis in the office.
To prevent transmission, patients with red eye should be asked to wait in a separate room and to put on disposable gloves.
Topical treatment.
While epidemic keratoconjunctivitis is treated symptomically, herpetic (kerato-)conjunctivitis is treated topically and/or orally with a virostatic agent.
Non-infectious inflammation also requires timely treatment. Typical examples of non-infectious keratopathy are neurotrophic keratopathy and keratopathy due to lagophthalmos (see section entitled “Eyelid malposition”). In neurotrophic keratopathy the sensitivity of the cornea is greatly reduced, so that there is often a discrepancy between the patient’s subjective sensation of pain and the actual findings (16). Patients typically have a history of surgery of the head (trigeminal neuralgia, acoustic neuroma), diseases that compromise the trigeminal nerve (tumor, brainstem hemorrhage), or infection with varicella zoster virus. Other possible causes are diabetes mellitus and multiple sclerosis. The treatment must include adequate moistening of the corneal surface with artificial tears and eye ointments (e.g., dexpanthenol) to avoid exposure keratopathy. Application of an occluding eye bubble moisture chamber at night, forming a moisture chamber, is still recommended. Potential new forms of treatment, e.g., topically applied nerve growth factors, are currently being tested in randomized controlled trials (e11, e12).
Allergic reactions
Non-infectious (kerato-)conjunctivitis.
Typical examples of non-infectious keratopathy are neurotrophic keratopathy and keratopathy due to lagophthalmos.
Allergic reactions.
The acute symptoms are bilateral swelling of the eyelids, epiphora, itching, and conjunctival hyperemia with chemosis.
Most case of acute allergic conjunctivitis are triggered by immunoglobulin-E-reactive antigens (type I: immediate-type allergy; classic “hay fever”). Chronic conjunctivitis, usually severe, is caused not by IgE but by T lymphocytes, which is why it is also sometimes referred to as a “cell-associated reaction” (type IV: delayed-type allergy). Examples of this type are vernal and atopic keratoconjunctivitis. The acute symptoms comprise bilateral swelling of the eyelids, epiphora, itching, and conjunctival hyperemia with chemosis. Further exposure to the allergen should be avoided, and acute local and systemic antihistamines can be used. For long-term prophylaxis, mast cell stabilizers (sodium cromoglycate, lodoxamide) or H1 blockers of the second or third generation (e.g., olopatadine) can be prescribed, as shown in recently published reviews (17, e13). If the symptoms are severe, short-term local steroids (fluorometholone, loteprednol) can be given and a desensitization process initiated (18, 19). In the case of clinically meaningful type-IV sensitization after long-term use of eye drops containing preservative agents or sensitivity to ingredients of facial care products and cosmetics, avoidance of further contact with the allergen is mandatory. Systemic steroids or immunosuppressants can be used in the most severe cases. Epicutaneous testing to identify the allergen concerned should be arranged. As a rule the treatment of allergic reactions is interdisciplinary (18). Detailed information on dry eye disease can be found in the CME article by E.M. Messmer in issue 5/2015 of this journal (20).
Subconjunctival hemorrhage
Sudden subconjunctival hemorrhage (figure 4) occurs particularly often in patients receiving oral anticoagulants and in those with poorly regulated or untreated arterial hypertension. The patients often report Valsalva maneuvers shortly beforehand (going to the toilet, gardening, etc.). In every “simple” subconjunctival hemorrhage, the patient’s blood pressure should be measured in the office to rule out an acute blood pressure crisis. The patient should be referred to an internist, because a large population-based study reported an elevated risk (hazard ratio 1.33) of (late) cardiovascular complications following subconjunctival hemorrhage (e14). The blood is resorbed spontaneously over a period of 2 to 4 weeks.
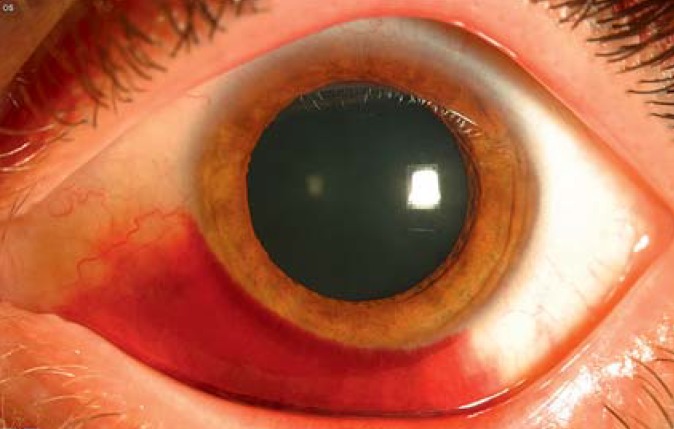
Figure 4.
Subconjunctival hemorrhage
The arterial blood pressure should be measured to exclude a hypertensive crisis. If trauma cannot be ruled out, ophthalmosurgical exploration is required.
On the slightest suspicion of blunt or penetrating trauma, the patient must be transferred to an eye surgery center for operative exploration.
Corneal erosion/ulceration
Erosion of the cornea is a superficial defect of the epithelium. Pain, foreign body sensation, photophobia, and epiphora with blepharospasm are typical symptoms. The patients can usually describe the cause clearly.
Subconjunctival hemorrhage.
Sudden subconjunctival hemorrhage occurs particularly often in patients receiving oral anticoagulants and in those with poorly regulated or untreated arterial hypertension. The patients often report Valsalva maneuvers beforehand.
If these symptoms occur after working with a drill or angle grinder, a metallic foreign body is often the cause. On the cornea, even after after just a few hours in situ, such a fragment of metal leads to a rust ring that must be promptly removed by an ophthalmologist. Patients with no foreign body are referred to an ophthalmologist and can, if it seems advisable, be treated with an antibiotic eye ointment (e.g., chloramphenicol) in the meantime (e15). In the case of doubt, the patient should see an ophthalmologist without delay so that a penetrating injury can be ruled out. A special case is represented by red eye after surgery involving intubation anesthesia or in long-term ventilation on the intensive care unit. In these situations corneal erosion with reddening of the conjunctiva, usually in the lower third of the cornea, is caused by “dehydration” of the cornea due to incomplete closure of the eyelids (21).
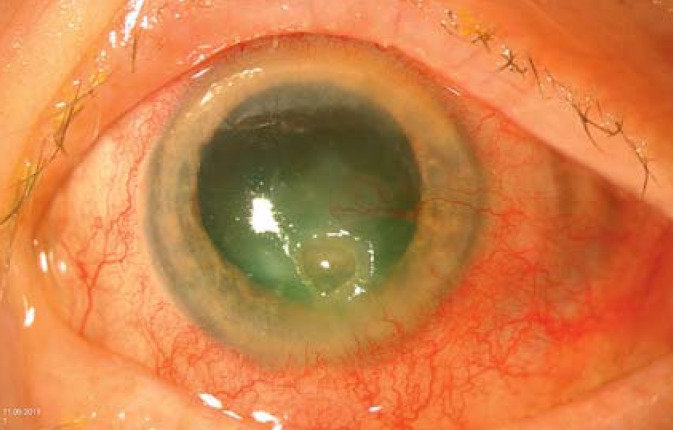
Deeper inflammation of the cornea can develop into keratitis or an ulcer (figure 5). At this point there is a danger of corneal perforation. Therapeutic corneal transplantation often becomes necessary. Overall, the visual prognosis is unfavorable. Healing of the ulcer frequently leads to extensive scarring of the cornea and irregular astigmatism.
Figure 5.
Corneal ulcer
White or gray discoloration of the cornea with an obvious tissue defect
Photokeratitis
In photokeratitis the corneal inflammation is caused by ultraviolet rays. UV-C irradiation leads to acute necrosis of the epithelium over the exposed ocular surface. The typical situations include welding without goggles or a trip to a mountainous area without the necessary UV protection (e16, e17). Most patients present around 6 to 8 h after the event because the initially moderate, almost always bilateral pain and other symptoms (foreign body sensation, photophobia, epiphora) become unbearable and—due to the resulting blepharospasm—may lead to transitory functional blindness for up to 48 h. Although it is obvious what has happened, the patient should be seen by an ophthalmologist in a timely manner. The pronounced bilateral blepharospasm can be briefly interrupted by means of a single application of a topical local anesthetic (e.g., eye drops with oxybuprocaine hydrochloride 0.4%). There are no studies with high-level evidence, but oral analgesics should be given at the first contact with a physician, the patient should not rub his or her eyes, and vitamin A eye ointment should be used. The regeneration time of the damaged corneal epithelium is 24 to 48 h. Topical local anesthetics should not be prescribed.
Episcleritis
Episcleritis is a moderately painful inflammation of the connective tissue between the sclera and the conjunctiva with reddening usually confined to one sector and predominantly conjunctival injection (figure 6). Scleritis, in contrast, is characterized by a markedly painful eyeball, often accompanied by impaired vision (22). Furthermore, the hyperemia in scleritis is not suppressed by the diagnostic (!) administration of a vasoconstrictor (figure 7).
Figure 6.
Episcleritis
Inflammation of the connective tissue between sclera and conjunctiva with reddening, typically confined to one sector, and distinct dilatation of the episcleral vessels
Figure 7.
Scleritis
Typical appearance of scleritis: diffuse, “washed-out” red eye with dilatation of deep and superficial vessels
Photokeratitis.
In photokeratitis the corneal inflammation is caused by ultraviolet rays. UV-C irradiation leads to acute necrosis of the epithelium over the exposed ocular surface.
While episcleritis is generally triggered by exogenous factors (22), an underlying systemic disease (e.g., rheumatoid arthritis or vasculitis) can be demonstrated in up to 50% of patients with scleritis. In 20% of these cases, the systemic disease is of infectious origin (e.g., varicella zoster virus). (22– 24). The patient should always be urgently seen by an ophthalmologist. Episcleritis is usually self-limiting but may recur. Systemic comorbidity is rare. The treatment begins with moistening eye drops and non-steroidal antirheumatic/-phlogistic drugs (NSARD), e.g., diclofenac (e18, e19). The treatment of scleritis ensues in stages (e18, e19). The underlying condition often has to be treated with anti-inflammatory drugs and immunosuppressants. Under certain conditions, new treatment strategies employing biologics/biosimilars such as tocilizumab or rituximab can be pursued (25, 26). Any delay in commencing treatment may result in a sharp increase in mortality from the underlying systemic disease (e20, e21). For instance, Foster et al. reported 10-year mortality of 30% in patients with rheumatoid arthritis (e22).
Intraocular disorders
Iritis and iridocyclitis (inflammation of the iris with involvement of the ciliary body and the anterior vitreous) are collectively referred to as anterior uveitis. Iritis is the most frequently occurring form of uveitis. In many cases no obvious causative factor is identified; nevertheless, immunological causes are more common than infections (e.g., syphilis or borreliosis) (27, 28). Rheumatic disorders, such as Bekhterev disease and Behçet syndrome, are particularly often associated with anterior uveitis (29). Furthermore, there is an association with inflammatory multisystem diseases such as sarcoidosis and juvenile idiopathic arthritis (30). The cardinal symptoms of iritis are photophobia, ciliary injection, and absence of the secretion typical of primary conjunctivitis.
Patients with a rheumatic disease or suspicion of anterior uveitis should be seen by an ophthalmologist within 24 h to avoid complications owing to exudative fibrinous inflammatory reactions. The treatment regimen for anterior uveitis depends on the etiology: frequent topical application of eye drops containing steroids, accompanied by pupil-dilating drops 2 or 3 times daily, is often sufficient (e23, e24).
Primary acute angle-closure glaucoma
Acute angle-closure glaucoma (“glaucoma attack”) is an acute ophthalmological emergency most often caused by pupillary block. The peripheral iris becomes attached to the cornea, leading to displacement of aqueous humor outflow with a resulting marked increase in internal ocular pressure (31).
Episcleritis.
Episcleritis is a moderately painful inflammation of the connective tissue between the sclera and the conjunctiva with reddening usually confined to one sector and predominantly conjunctival injection.
Pain can radiate into the head and the teeth and also lead to secondary abdominal symptoms, cardiac rhythm disorders, and nausea via vagus stimulation. The cardinal symptom is the unilateral “rock-hard” eyeball, detectable by palpation of one eye and then the other: with the patient looking downwards, the eyeball is pressed down into the orbital fatty tissue with the index finger of one hand, holding it as still as possible, and the sclera is carefully indented with the index finger of the other hand. The deterioration in vision and the perception of colored rings around light sources (halos) are due to the corneal expansion (32). The increased internal ocular pressure causes intraocular ischemia and paralysis of the sphincter muscle of the pupil, so that the pupil is no longer round, moderately wide, and unresponsive to light. With the aid of a diagnostic pen light shone from the side, one can discern the flattening of the anterior chamber of the eye with approximation of the iris to the cornea.
Systemic and local treatment to lower the internal ocular pressure should be initiated without delay (e25). Many patients also require surgical intervention to deal with the angle closure (e26).
Disorders of the ocular adnexa
Hordeolum
Hordeolum (stye) occurs commonly in all age groups (1, 33). A usually acute bacterial inflammation of sebaceous or sweat glands at the margin of the eyelid manifests—in most cases painfully—as a raised red nodule (figure 8). The exact incidence cannot be quantified (34). The recommended treatment comprises dry heat (e.g., from an infrared lamp) and an antibiotic ointment (e.g., gentamycin or ofloxacin, 3 × daily for a week), although no randomized clinical trials have been carried out. If there is no improvement, the patient should be referred to an ophthalmologist to exclude other possible diagnoses (e.g., sebaceous gland carcinoma) (1, 33).
Figure 8.
Hordeolum
Acute, painful bacterial inflammation of sebaceous or sweat glands at the margin of the eyelid
Eyelid malposition
Primary acute angle-closure glaucoma.
Acute angle-closure glaucoma (“glaucoma attack”) is an acute ophthalmological emergency most often caused by pupillary block.
The common malpositions of the lower eyelids are ectropion and entropion, both usually a result of age-related slackening of the lid-retaining apparatus (35). In entropion the lid margin is inverted towards the eyeball and the eyelashes chafe against the surface of the eye (trichiasis). The danger is that defects of the corneal epithelium may arise, perhaps even a corneal ulcer. The test to determine whether entropion can be provoked, the patient should be asked to close the eye hard. In ectropion (figure 9) the lower lid is rotated outwards and the tear fluid can no longer properly moisten the ocular surface, again resulting in defects of the cornea. One typical form of non-infectious keratopathy is lagophthalmic keratopathy, in which the eyelids close only incompletely or not at all. The most common cause is paralysis of the orbicular muscle of the eye in peripheral facial palsy.
Figure 9.
Lower-lid ectropion
External rotation of the lower lid, so that the tear fluid can no longer properly moisten the ocular surface. Conjunctival hyperemia owing to lagophthalmos is the result.
In all of these situations the patient should be seen by an ophthalmologist. Surgical correction of the lid malposition is usually necessary.
Carotid–cavernous sinus fistula
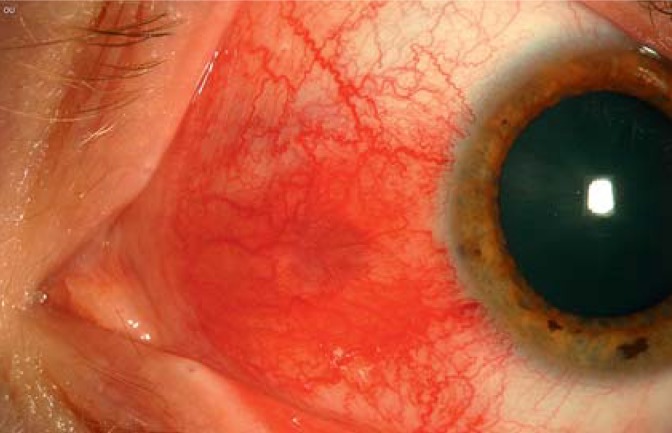
A communication between the internal carotid artery and the cavernous sinus may occur spontaneously or result from trauma. In some cases the fistula is associated with bilateral massive, tortuous dilatation of the conjunctival and episcleral vessels (figure 10). Further findings may include deterioration of vision, pulsatile exophthalmos, double vision, headache, and the perception of a rushing sound in the orbit that is audible on auscultation (36). The patient should be referred for urgent ophthalmological examination in an interdisciplinary center equipped to perform modern imaging modalities (e.g., magnetic resonance angiography).
Figure 10.
Carotid–cavernous sinus fistula
Bilateral massive dilatation of the conjunctival and episcleral vessels
Red eye in systemic diseases
Lid malposition.
In entropion the lid margin is inverted towards the eyeball and the eyelashes chafe against the surface of the eye. The danger is that defects of the corneal epithelium may arise, perhaps even a corneal ulcer.
Unilateral or bilateral red eye is frequently found in association with primarily systemic diseases. The systemic dermatological diseases in which red eye occurs include rosacea, molluscum contagiosum, and, commonly, severe atopy. Interdisciplinary management of these patients must not be neglected, as the ocular involvement may extend as far as sterile corneal perforation (37).
Further information on CME.
This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education. Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire. See the following website: cme.aerzteblatt.de.
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
This CME unit can be accessed until 25 June 2017, and earlier CME units until the dates indicated:
„Aneurysmal Subarachnoid Hemorrhage“ (issue 13/2017) bis zum 25 June 2017,
“ADHD” (Issue 9/2017) until 28 May 2017,
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the most appropriate answer.
Question 1
Why should vasoconstrictive eye drops be prescribed as a supportive measure for no more than a few days?
Because they lead to enduring blepharospasm
Because they lead to photophobia
Because they may lead to tachyphylaxis
Because they lead to hyperemia
Because they lead to increased internal ocular pressure
Question 2
What step should be taken immediately whenever bacterial conjunctivitis is suspected in a contact lens wearer?
Treatment with local steroids
A watch and wait strategy
Prescription of new contact lenses
Exclusion of accompanying viral disease
Referral to an ophthalmologist
Question 3
With which disease is anterior uveitis most often associated?
Multiple sclerosis
Bekhterev disease
Glaucoma
Diabetes mellitus type 2
Gout
Question 4
What are the typical symptoms of scleritis?
Marked epiphora, sclera tending towards hyperemia, no accompanying systemic findings
Slight, motion-dependent eyeball pain with purulent exudation
Diffuse, “washed-out” red eye with severe eyeball pain
Corneal opacity, usually pronounced circular corneal vascularization
Tired, burning eyes, diplopia
Question 5
With what is spontaneous subconjunctival hemorrhage often associated?
Diabetes mellitus type 2
Intake of oral antihypertensives
Existing arterial hypertension
Perforating ocular injury
Non-infectious conjunctivitis
Question 6
What should one do immediately in every case of simple subconjunctival hemorrhage?
Examine the fundus of the eye
Determine the visual acuity
Check the visual field
Administer an antibiotic ointment
Measure the blood pressure
Question 7
What are the typical symptoms of an acute “glaucoma attack”?
Rock-hard eyeball, purulent exudation, reduced visual contrast
Soft eyeball, worsened vision, incipient myasthenia gravis
Rock-hard eyeball, worsened vision, perception of colored rings around light sources
Normal eyeball, worsened vision, restricted visual field
Rock-hard eyeball, transient improvement in vision due to hyperemia, night blindness
Question 8
What should be the first step in red eye of unknown origin and suspicion of viral conjunctivitis?
Ophthalmological assessment after the symptoms have worn off
Microbiological exclusion of acanthamoebae
First-line treatment with, as a rule, steroid eye drops
otification to the authorities within 48 h, even in isolated cases
Put the patient in a separate waiting area, give him/her disposable gloves to wear
Question 9
A patient presents with painful acute unilateral red eye. The diagnostic work-up does not confirm the suspicion of a foreign body or perforation. The ocular pressure is high on palpation. What is one possible diagnosis?
Uveitis
Acute glaucoma attack
Bacterial conjunctivitis
Endocrine orbitopathy
Seasonal chemosis
Question 10
A patient with known Behçet syndrome reports a 24-h history of severe eye pain on exposure to light. What is the first differential diagnosis that comes to mind?
Posterior uveitis
Cataract
Glaucoma attack
Anterior uveitis
Photokeratitis
Acknowledgments
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Pflipsen M, Massaquoi M, Wolf S. Evaluation of the painful eye. Am Fam Physician. 2016;93:991–998. [PubMed] [Google Scholar]
- 2.Teo MA. Improving acute eye consultations in general practice: a practical approach. BMJ Qual Improv Rep. 2014;3 doi: 10.1136/bmjquality.u206617.w2852. pii: u206617.w2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cronau H, Kankanala RR, Mauger T. Diagnosis and management of red eye in primary care. Am Fam Physician. 2010;81:137–144. [PubMed] [Google Scholar]
- 4.Statham MO, Sharma A, Pane AR. Misdiagnosis of acute eye diseases by primary health care providers: incidence and implications. Med J Aust. 2008;189:402–404. doi: 10.5694/j.1326-5377.2008.tb02091.x. [DOI] [PubMed] [Google Scholar]
- 5.O‘Connor PM, Crock CT, Dhillon RS, Keeffe JE. Resources for the management of ocular emergencies in Australia. Emerg Med Australas. 2011;23:331–336. doi: 10.1111/j.1742-6723.2011.01411.x. [DOI] [PubMed] [Google Scholar]
- 6.Azari AA, Barney NP. Conjunctivitis: a systematic review of diagnosis and treatment. JAMA. 2013;310:1721–1729. doi: 10.1001/jama.2013.280318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abelson MB, Butrus SI, Weston JH, Rosner B. Tolerance and absence of rebound vasodilation following topical ocular decongestant usage. Ophthalmology. 1984;91:1364–1367. doi: 10.1016/s0161-6420(84)34140-9. [DOI] [PubMed] [Google Scholar]
- 8.Alfonso SA, Fawley JD, Alexa Lu X. Conjunctivitis. Prim Care. 2015;42:325–345. doi: 10.1016/j.pop.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Messmer EM. Keratitis—infectious or autoimmune? Klin Monbl Augenheilkd. 2016;233:808–812. doi: 10.1055/s-0042-105155. [DOI] [PubMed] [Google Scholar]
- 10.Fernandes M, Vira D, Medikonda R, Kumar N. Extensively and pan-drug resistant pseudomonas aeruginosa keratitis: clinical features, risk factors, and outcome. Graefes Arch Clin Exp Ophthalmol. 2016;254:315–322. doi: 10.1007/s00417-015-3208-7. [DOI] [PubMed] [Google Scholar]
- 11.Vazirani J, Wurity S, Ali MH. Multidrug-resistant pseudomonas aeruginosa keratitis: risk factors, clinical characteristics, and outcomes. Ophthalmology. 2015;122:2110–2114. doi: 10.1016/j.ophtha.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Tsatsos M, MacGregor C, Athanasiadis I, Moschos MM, Hossain P, Anderson D. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Experiment Ophthalmol. 2016;44:824–837. doi: 10.1111/ceo.12785. [DOI] [PubMed] [Google Scholar]
- 13.Adhikary AK, Banik U. Human adenovirus type 8: the major agent of epidemic keratoconjunctivitis (EKC) J Clin Virol. 2014;61:477–486. doi: 10.1016/j.jcv.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Jhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB. Adenoviral keratoconjunctivitis. Surv Ophthalmol. 2015;60:435–443. doi: 10.1016/j.survophthal.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Meyer-Rüsenberg B, Loderstädt U, Richard G, Kaulfers PM, Gesser C. Epidemic keratoconjunctivitis—the current situation and recommendations for prevention and treatment. Dtsch Arztebl Int. 2011;108:475–480. doi: 10.3238/arztebl.2011.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chi JJ. Management of the eye in facial paralysis. Facial Plast Surg Clin North Am. 2016;24:21–28. doi: 10.1016/j.fsc.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Castillo M, Scott NW, Mustafa MZ, Mustafa MS, Azuara-Blanco A. Topical antihistamines and mast cell stabilisers for treating seasonal and perennial allergic conjunctivitis. Cochrane Database Syst Rev. 2015;6 doi: 10.1002/14651858.CD009566.pub2. CD009566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schröder K, Finis D, Meller S, Buhren BA, Wagenmann M, Geerling G. Seasonal and perennial allergic rhinoconjunctivitis. Klin Monbl Augenheilkd. 2014;231:496–504. doi: 10.1055/s-0034-1368397. [DOI] [PubMed] [Google Scholar]
- 19.Messmer EM. Ocular allergies. Ophthalmologe. 2005;102:527–543. doi: 10.1007/s00347-005-1181-y. [DOI] [PubMed] [Google Scholar]
- 20.Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112:71–81. doi: 10.3238/arztebl.2015.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roth S, Thisted RA, Erickson JP, Black S, Schreider BD. Eye injuries after nonocular surgery A study of 60,965 anesthetics from 1988 to 1992. Anesthesiology. 1996;85:1020–1027. doi: 10.1097/00000542-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Sobolewska B, Zierhut M. Episkleritis und Skleritis. Augenheilkunde up2date. 2015;5:51–62. doi: 10.1055/s-0033-1358100. [DOI] [PubMed] [Google Scholar]
- 23.Diaz JD, Sobol EK, Gritz DC. Treatment and management of scleral disorders. Surv Ophthalmol. 2016;61:702–717. doi: 10.1016/j.survophthal.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Dunn JP. Uveitis. Prim Care. 2015;42:305–323. doi: 10.1016/j.pop.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Silpa-Archa S, Oray M, Preble JM, Foster CS. Outcome of tocilizumab treatment in refractory ocular inflammatory diseases. Acta Ophthalmol. 2016;94:e400–e406. doi: 10.1111/aos.13015. [DOI] [PubMed] [Google Scholar]
- 26.Suhler EB, Lim LL, Beardsley RM, et al. Rituximab therapy for refractory scleritis: results of a phase I/II dose-ranging, randomized, clinical trial. Ophthalmology. 2014;121:1885–1891. doi: 10.1016/j.ophtha.2014.04.044. [DOI] [PubMed] [Google Scholar]
- 27.D‘Ambrosio EM, Cava M, Tortorella P, Gharbyia M, Campanella M, Iannetti L. Clinical features and complications of the HLA-B27-associated acute anterior uveitis: a metanalysis. Semin Ophthalmol. 2016;12:1–13. doi: 10.3109/08820538.2016.1170158. [DOI] [PubMed] [Google Scholar]
- 28.Pathanapitoon K, Dodds EM, Cunningham ET Jr, Rothova A. Clinical spectrum of HLA-B27-associated ocular inflammation. Ocul Immunol Inflamm. 2016;18:1–8. doi: 10.1080/09273948.2016.1185527. [DOI] [PubMed] [Google Scholar]
- 29.Stavropoulos PG, Soura E, Kanelleas A, Katsambas A, Antoniou C. Reactive arthritis. J Eur Acad Dermatol Venereol. 2015;29:415–424. doi: 10.1111/jdv.12741. [DOI] [PubMed] [Google Scholar]
- 30.Heiligenhaus A, Minden K, Föll D, Pleyer U. Uveitis in juvenile idiopathic arthritis. Dtsch Arztebl Int. 2015;112:92–100. doi: 10.3238/arztebl.2015.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle-closure glaucoma: an update. Acta Ophthalmol. 2016;94:217–225. doi: 10.1111/aos.12784. [DOI] [PubMed] [Google Scholar]
- 32.Schwenn O. Acute angle closure, chronic angle-closure glaucoma and their differential diagnoses. Klin Monbl Augenheilkd. 2011;228:95–104. doi: 10.1055/s-0031-1280025. [DOI] [PubMed] [Google Scholar]
- 33.Carlisle RT, Digiovanni J. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2015;92:106–112. [PubMed] [Google Scholar]
- 34.Lindsley K, Nichols JJ, Dickersin K. Interventions for acute internal hordeolum. Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD007742.pub3. CD007742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Press UP. The aging eyelid. Klin Monbl Augenheilkd. 2010;227:15–19. doi: 10.1055/s-0028-1109968. [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez Castro LN, Colorado RA, Botelho AA, Freitag SK, Rabinov JD, Silverman SB. Carotid-cavernous fistula: a rare but treatable cause of rapidly progressive vision loss. Stroke. 2016;47:207–209. doi: 10.1161/STROKEAHA.116.013428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nivenius E, Montan P. Spontaneous corneal perforation associated with atopic keratoconjunctivitis: a case series and literature review. Acta Ophthalmol. 2015;93:383–387. doi: 10.1111/aos.12617. [DOI] [PubMed] [Google Scholar]
- E1.Behrens-Baumann W, Quentin CD, Gibson JR, Calthrop JG, Harvey SG, Booth K. Trimethoprim-polymyxin B sulphate ophthalmic ointment in the treatment of bacterial conjunctivitis: a double-blind study versus chloramphenicol ophthalmic ointment. Curr Med Res Opin. 1988;11:227–231. doi: 10.1185/03007998809114240. [DOI] [PubMed] [Google Scholar]
- E2.Jauch A, Fsadni M, Gamba G. Meta-analysis of six clinical phase III studies comparing iomefloxacin 03% eye drops twice daily to five standard antibiotics in patients with acute bacterial conjunctivitis. Graefes Arch Clin Exp Ophthalmol. 1999;237:705–713. doi: 10.1007/s004170050300. [DOI] [PubMed] [Google Scholar]
- E3.Lohr JA, Austin RD, Grossman M, Hayden GF, Knowlton GM, Dudley SM. Comparison of three topical antimicrobials for acute bacterial conjunctivitis. Pediatr Infect Dis J. 1988;7:626–629. doi: 10.1097/00006454-198809000-00005. [DOI] [PubMed] [Google Scholar]
- E4.Protzko E, Bowman L, Abelson M, Shapiro A. Phase 3 safety comparisons for 10% azithromycin in polymeric mucoadhesive eye drops versus 0.3% tobramycin eye drops for bacterial conjunctivitis. Invest Ophthalmol Vis Sci. 2007;48:3425–3429. doi: 10.1167/iovs.06-1413. [DOI] [PubMed] [Google Scholar]
- E5.Messmer EM. Keratitis—infectious or autoimmune? Klin Monbl Augenheilkd. 2016;233:808–812. doi: 10.1055/s-0042-105155. [DOI] [PubMed] [Google Scholar]
- E6.Robert Koch-Institut. Adenovirus-Konjunktivitis: RKI-Ratgeber für Ärzte. www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Adenovirus_Konjunktivitis.html#doc2393452bodyText16 (last accessed on 3 January 2017) [Google Scholar]
- E7.Tsatsos M, MacGregor C, Athanasiadis I, Moschos MM, Hossain P, Anderson D. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol. 2016:;44:824–837. doi: 10.1111/ceo.12785. doi: 10.1111/ceo.12785. [DOI] [PubMed] [Google Scholar]
- E8.Wilhelmus KR. Interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev. 2003;3 doi: 10.1002/14651858.CD002898. CD002898. Update in: Cochrane Database Syst Rev 2007; 1: CD002898. [DOI] [PubMed] [Google Scholar]
- E9.Vrcek I, Choudhury E, Durairaj V. Herpes zoster ophthalmicus: a review for the internist. Am J Med. 2017,;130:21–26. doi: 10.1016/j.amjmed.2016.08.039. [DOI] [PubMed] [Google Scholar]
- E10.Schuster AK, Harder BC, Schlichtenbrede FC, Jarczok MN, Tesarz J. Valacyclovir versus acyclovir for the treatment of herpes zoster ophthalmicus in immunocompetent patients. Cochrane Database Syst Rev. 2016;11 doi: 10.1002/14651858.CD011503.pub2. CD011503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol. 2014;8:571–579. doi: 10.2147/OPTH.S45921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Yanai R, Nishida T, Chikama T, Morishige N, Yamada N, Sonoda KH. Potential new modes of treatment of neurotrophic keratopathy. Cornea. 2015;34:121–127. doi: 10.1097/ICO.0000000000000587. [DOI] [PubMed] [Google Scholar]
- E13.Kam KW, Chen LJ, Wat N, Young AL. Topical olopatadine in the treatment of allergic conjunctivitis: a systematic review and meta-analysis. Ocul Immunol Inflamm. 2016;18:1–15. doi: 10.3109/09273948.2016.1158282. [DOI] [PubMed] [Google Scholar]
- E14.Wang TJ, Keller JJ, Sheu JJ, Lin HC. A 3-year follow-up study on the risk of stroke among patients with conjunctival haemorrhage. Acta Ophthalmol. 2013;91:226–230. doi: 10.1111/j.1755-3768.2011.02359.x. [DOI] [PubMed] [Google Scholar]
- E15.Barequet IS, Harizman N, Ziv H, Rosner M. Healing rate of corneal erosions: comparison of the effect of chloramphenicol eye drops and ointment and high-concentration hyaluronic acid in an animal model. Cornea. 2014;33:1080–1082. doi: 10.1097/ICO.0000000000000215. [DOI] [PubMed] [Google Scholar]
- E16.Cullen AP. Photokeratitis and other phototoxic effects on the cornea and conjunctiva. Int J Toxicol. 2002;21:455–464. doi: 10.1080/10915810290169882. [DOI] [PubMed] [Google Scholar]
- E17.Ting MA, Saha K, Robbie S. Mass photokeratitis following ultraviolet light exposure at a nightclub. Cont Lens Anterior Eye. 2016;39:316–317. doi: 10.1016/j.clae.2016.01.009. [DOI] [PubMed] [Google Scholar]
- E18.Tappeiner C, Walscheid K, Heiligenhaus A. Diagnosis and treatment of episcleritis and scleritis. Ophthalmologe. 2016;113:797–810. doi: 10.1007/s00347-016-0344-3. [DOI] [PubMed] [Google Scholar]
- E19.Daniel Diaz J, Sobol EK, Gritz DC. Treatment and management of scleral disorders. Surv Ophthalmol. 2016;61:702–717. doi: 10.1016/j.survophthal.2016.06.002. [DOI] [PubMed] [Google Scholar]
- E20.Cocho L, Gonzalez-Gonzalez LA, Molina-Prat N, Doctor P, Sainz-de-la-Maza M, Foster CS. Scleritis in patients with granulomatosis with polyangiitis (Wegener) Br J Ophthalmol. 2016;100:1062–1065. doi: 10.1136/bjophthalmol-2015-307460. [DOI] [PubMed] [Google Scholar]
- E21.Generali E, Cantarini L, Selmi C. Ocular involvement in systemic autoimmune diseases. Clin Rev Allergy Immunol. 2015;49:263–270. doi: 10.1007/s12016-015-8518-3. [DOI] [PubMed] [Google Scholar]
- E22.Foster CS, Forstot SL, Wilson LA. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis Effects of systemic immunosuppression. Ophthalmology. 1984;91:1253–1263. doi: 10.1016/s0161-6420(84)34160-4. [DOI] [PubMed] [Google Scholar]
- E23.Jaffe GJ, Dick AD, Brézin AP, et al. Adalimumab in patients with active noninfectious uveitis. N Engl J Med. 2016;375:932–943. doi: 10.1056/NEJMoa1509852. [DOI] [PubMed] [Google Scholar]
- E24.Thurau S, Pleyer U. Differential diagnosis of anterior uveitis. Ophthalmologe. 2016;113:879–892. doi: 10.1007/s00347-016-0328-3. [DOI] [PubMed] [Google Scholar]
- E25.Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle-closure glaucoma: an update. Acta Ophthalmol. 2016;94:217–225. doi: 10.1111/aos.12784. [DOI] [PubMed] [Google Scholar]
- E26.Liebmann JM, Ritch R. Laser surgery for angle closure glaucoma. Semin Ophthalmol. 2002;17:84–91. doi: 10.1076/soph.17.2.84.14720. [DOI] [PubMed] [Google Scholar]