Abstract
To describe the policies and procedures used by 11 urban tuberculosis control programs to conduct contact investigations, written policies were reviewed and semi-structured interviews were conducted with program managers and staff. Qualitative analysis showed that contact investigation policies and procedures vary widely. Most policies address risk factor assessment and contact prioritization; however, none of the policies provide comprehensive guidance for the entire process. Staffing patterns vary, but, overall, staff receive little formal training; informal monitoring practices predominate. Comprehensive guidelines and programmatic support are needed to improve the quality of contact investigation processes.
Keywords: contact investigation, policy, tuberculosis
Background
Since the end of the resurgence of tuberculosis (TB) in the United States in 1992, the number of cases of TB has steadily declined. This trend has been attributed to successful efforts by TB programs to promptly identify and appropriately treat persons with TB. Owing to this recent success, TB programs have been able to expand their efforts toward the prevention of new TB cases. One important means of prevention is the contact investigation (CI), the process of identifying and evaluating persons exposed to infectious TB patients and, if appropriate, treating these persons for active TB disease or latent TB infection (LTBI). Leading the way, the Advisory Council for the Elimination of Tuberculosis recommends enhancing the effectiveness of CIs.1
The CI is an essential function of TB control in the United States.2,3 Although the general steps for performing CIs have been outlined,4,5 no official recommendations address CI policy development. The processes and infrastructure supports that are necessary for effective CIs have seldom been studied. A few researchers6–8 have described how individual TB programs established CI processes as part of their TB control strategy in their communities. One study9 demonstrated that many contacts were not being identified in a timely manner during the CI process. In another research effort10 focusing on patient and staff perceptions of the CI, results confirmed the widespread existence of communication difficulties and demonstrated the need for additional staff training. One recent study11 compared practices in one state with general guidelines and showed that systematic failures in processes, such as in conducting CIs, resulted in missed opportunities for TB prevention. These studies, however, did little to provide insights that can be turned into policies at the local level.
Many questions remain about the effectiveness of CIs. To address these questions the Centers for Disease Control and Prevention (CDC) undertook a multisite, retrospective study of a sample of infectious TB patients and all their reported contacts at 11 urban TB programs in the United States.12 Analysis of data collected from chart reviews showed that outcomes such as completion of testing and treatment for LTBI were less than optimal at all study sites. During visits to the 11 sites, data addressing policy and procedural structures also were obtained. Specifically, program managers and staff were interviewed about CI-related procedures, and written program policies were collected. To ascertain the standards and levels of guidance provided by policy infrastructure within the TB programs, these data were analyzed using qualitative methods. This article presents the findings and describes the range of program structures, policies and procedures, staffing, and monitoring practices occurring at the study sites.
Methods
The 11 urban areas that participated in the study12 were selected based on the estimated number of contacts to infectious TB patients from July 1996 through June 1997. The sites and their respective number of reported TB cases in 1997 were: Chicago, Illinois: 599; Fulton County, Georgia: 165; Houston, Texas: 572; Newark, New Jersey: 108; New York City, New York: 1,730; Los Angeles County: 558, San Diego County: 193, San Francisco: 241, and Santa Clara County, California: 174; Seattle-King County, Washington: 81; and Shelby County, Tennessee: 120.13 Data were collected at each of the sites between June 1998 and January 1999 from two major sources: (1) interviews with program managers and staff and (2) written documents including policies and procedures that were in place during the study period.
At each site, the TB program director was asked to review the interview guide and identify knowledgeable staff to participate in the interviews. On-site, semi-structured interviews were then conducted with key informants from the TB program. Interviews addressed program organization and administration, staffing, training, policies, procedures and practices, data collection and management, monitoring, and challenges as they related to CIs. Notes were transcribed and imported into CDC EZ-text qualitative software14 for a systematic content analysis by two trained analysts. Through this process, the analysts independently identified and coded common themes. Although initial inter-rater agreement was relatively high (kappa = .86), all coding discrepancies were jointly resolved before completing the analysis.
The second source of data, written documentation, included program policies, organizational charts, and CI forms. To facilitate comparison among the programs, relevant information was abstracted and analyzed using templates15 based on the program components identified in the CDC training module on CI practices.16 Policies were analyzed to determine the presence or absence of a concept and the degree of explicit instruction detailed in the policy. Concepts were categorized as “general” if the policy made reference to the activity but provided no further instruction on how to accomplish the activity. Concepts were described as “specific” if substantive direction or guidance was provided. Concepts mentioned on the CI form but not referenced in other policies also were noted.
Findings
At each of the 11 sites, unique programs and processes for conducting CIs have been instituted. Some of the programs have been ongoing for several years, while others have been formalized more recently. At 10 of the 11 sites, TB services are under the supervision of a single TB control administrative system, though services are often provided at multiple locations within a jurisdiction. At one site, three independent health care facilities provide TB services to the community, overseen by the state TB program. The extensive variation among the policies and practices related to staffing, training, and monitoring, as well as reported challenges, is described below.
Policies and procedures
All 11 sites have some formal policies instituted to provide uniform guidance for conducting CIs. Six programs use locally developed policies, while five use state policies in conjunction with locally produced documents or forms. Documents range from three- to four-page forms or checklists to more elaborate, multichaptered documents. The number of patients served by the program did not correlate with policy length or comprehensiveness. Policies vary widely in their content, but most policies make general reference to the major steps typically considered part of a CI. However, as Table 1 illustrates, many specific actions within these broad steps are not addressed, and none of the policies address a comprehensive range of CI activities. Policies often mention a step to be accomplished without providing instructions or guidance. Terms may not be defined or used consistently. The major CI steps and the extent of guidance provided by the 11 policies are discussed below, along with innovative practices undertaken by the sites.
Table 1.
Contact investigation (CI) policies and procedures
| CI steps | TB control jurisdictions
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Medical record review | ❍ | ❏ | ❏ | ❍ | ❏ | ● | ❍ | ❍ | ❏ | ||
| Period of infectiousness assessed | ❍ | ❍ | ❍ | ❍ | |||||||
| Patient interview conducted | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ||
| Confidentiality | ❍ | ❍ | ❍ | ❍ | |||||||
| Patient education | ❍ | ❍ | ● | ❍ | ❍ | ||||||
| Second interview | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ||||
| Field visits required | ❍ | ❍ | ◆ | ❍ | ● | ❍ | ❍ | ❍ | ◆ | ||
| Routine TST in field | ❍ | ❍ | ❍ | ◆ | ❍ | ❍ | |||||
| Contact education | ❍ | ❍ | ❍ | ❍ | ❍ | ◆ | ◆ | ||||
| Risk assessment for TB transmission | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ |
| Prioritizing contacts | ● | ● | ● | ❍ | ● | ● | ❍ | ❍ | ❍ | ● | ❍ |
| Steps to locate contacts | ❍ | ❍ | ❍ | ❍ | ❍ | ||||||
| HIV risk assessments and referrals to testing | ❍ | ❍ | ❍ | ❍ | ● | ||||||
| Evaluating contacts | ❍ | ❍ | ● | ● | ● | ❍ | ● | ● | ❍ | ||
| Second TST | ❍ | ❍ | ❍ | ❏ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | |
| Screen patients with history of TST+ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | |||||
| Treatment and follow-up of contacts | ❍ | ❍ | ❍ | ❍ | ● | ❍ | ❍ | ❍ | ❍ | ||
| Specialized treatment for children | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ❍ | ◆ | |||
| Specialized treatment for HIV+ individuals | ❏ | ❍ | ❍ | ❍ | ❍ | ❍ | |||||
| Barriers to adherence identified | ❍ | ❏ | ❏ | ❍ | ❍ | ❏ | |||||
| Rules for expansion | ❍ | ❍ | ❍ | ||||||||
| Concentric circle approach | ❍ | ❍ | ❍ | ◆ | ❍ | ||||||
● Specific ❍General ❏ Form only ◆ Special circumstances/populations
Review medical records
Although a TB patient’s medical record provides valuable information for a CI about health history and period of infectiousness, a review of medical records is only briefly mentioned in four policies, as Table 1 shows. Policies in four sites state the period of infectiousness should be assessed.
Interview the patient
To promote prompt identification and treatment of contacts, interviews should be conducted with a patient in a timely manner when there is a suspicion or diagnosis of TB.16 Most study site policies require that a patient be interviewed within three days; however, others are less explicit. Follow-up interviews to obtain additional contacts are acknowledged by seven sites. Content of the interviews, according to program managers, is typically left to the discretion of the interviewer; critical issues, such as education and confidentiality, are seldom acknowledged by policy. One site provides patients with educational materials and a signed form acknowledging their understanding.
Conduct field visits
Visiting the TB patient’s home or other environment enables CI staff to obtain additional information about risk of transmission and possible additional contacts. However, field visits are not mandated at four sites. Policies typically provide little detail on what should be accomplished during a visit, and only one policy directs the CI staff to make note of ventilation, room size, and eating and sleeping arrangements. However, to ensure appropriate assessment of airflow and ventilation at work sites or schools, one site uses a trained team to conduct certain environmental assessments.
Assess risk of transmission
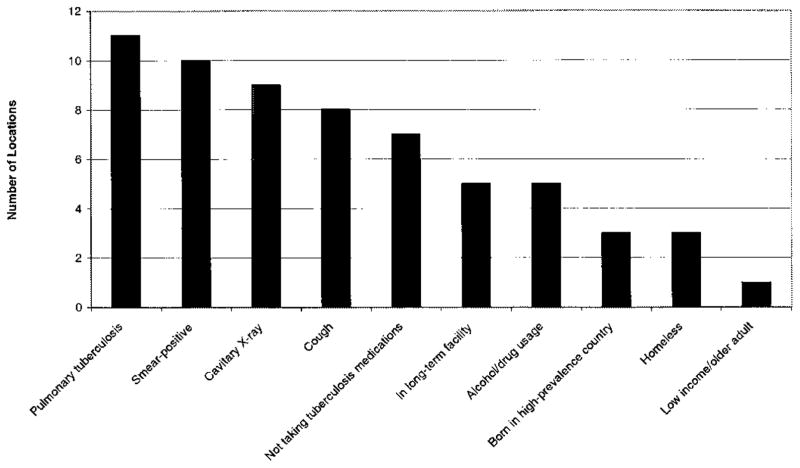
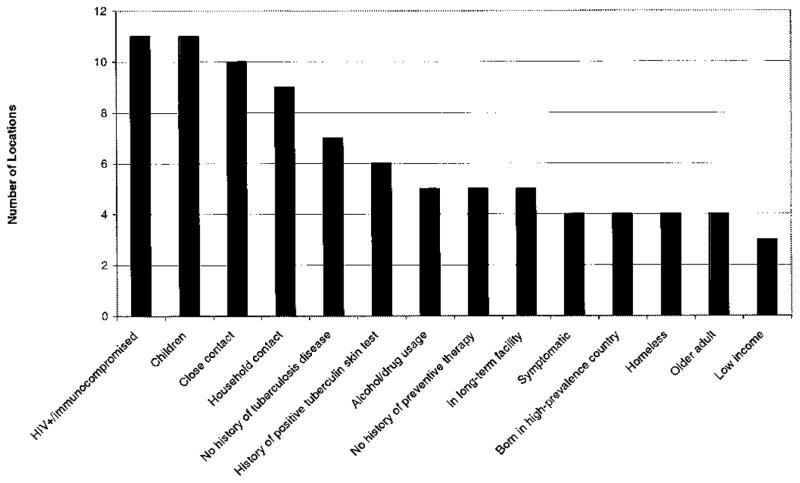
The risk of TB transmission is dependent on a number of factors, including the infectiousness of the TB case, the susceptibility of the contact, and the environment in which the exposure occurs.5 As shown in Figures 1 and 2, all sites acknowledge case and contact risk factors in the assessment process. Most address environmental factors, such as ventilation (10 sites) and room size (8 sites), especially for work-site investigations. However, these factors typically appear in policies in a list format, without accompanying instructions for carrying out the assessment process. Further, forms typically do not have designated space for systematically recording this information.
Figure 1.
Case factors for prioritizing investigations.
Figure 2.
Contact factors for prioritizing investigations.
Prioritize contacts
Prioritizing contacts and then focusing on the high-priority contacts are critical activities in conducting efficient, successful CIs; however, sites do not consistently define a “close” contact. Of sites providing some level of guidance on how to prioritize contacts, policies recommend the following:
assessing closeness in terms of number of hours of contact
focusing on household contacts
focusing on family contacts
asking the TB case to determine who is “close”
In addition, to some extent all policies address prioritization of children under 4 years of age and people with human immunodeficiency virus (HIV) infection or other immunocompromising conditions because of their high risk for developing disease, regardless of the extent of exposure. Despite the importance of specialized care for persons with HIV infection, few policies specify that contacts be asked about their HIV status, offered testing, or assessed regarding risk factors. Program managers and staff, when interviewed, occasionally noted difficulties in obtaining adequate information about these risk factors from patients or contacts.
Although multidrug-resistant TB (MDR TB) cases have been reported in all of the states represented in this study,13 only three sites specify protocols for dealing with MDR TB cases. These policies state that patients with MDR TB should receive priority in the investigative process; only one policy addresses special treatment needs for contacts of MDR TB cases.
Evaluate contacts
CIs require that contacts be located and evaluated to determine the presence of TB symptoms, history of TB infection or disease, and high-risk factors for disease and possible nonadherence to treatment. For contacts with no documented history of TB infection or disease, nine sites have policies that require that a Mantoux tuberculin skin test (TST) be placed, and many sites have charts or diagrams to help staff decide when to refer contacts for additional screening, including medical examinations and chest radiographs.
Provide treatment and follow-up
LTBI treatment and/or follow-up assessment for appropriate contacts is addressed by policies at nine sites. In addition, the increased risk of rapid disease development in both young children and immunocompromised persons17–19 is addressed in the policies of most sites.
To improve overall patient treatment, a few sites have innovative policies related to the referral of persons infected with HIV to specific programs and services, signing contracts with patients to promote adherence, and providing directly observed therapy for LTBI in schools.
Expand investigations
It is generally acknowledged that CIs should be expanded when evidence of recent transmission is indicated and should be stopped when there is no indication of additional transmission.5 Five policies refer to the concentric circle approach for expanding CIs, but offer little guidance on how to apply it. Interview respondents reported that, in practice, expansion is decided on a case-by-case basis by the worker directly responsible for the investigation at six sites and, at four other sites, by a CI supervisor. One site convenes a formal meeting to make the decision. At two sites, respondents reported that limited resources force workers to routinely exclude casual contacts from the investigation.
Organizational structure, staffing, and training
Organizational structure
Four basic organizational systems for conducting CI processes emerge from the data. Each of these systems, summarized below, defines how staff resources are allocated.
TB program staff provide CI services within the context of overall TB services. Typically, a multidisciplinary team performs a wide range of TB services, including CI activities. This is the most common system for conducting CIs, seen at five sites.
Dedicated CI teams are the most specialized system for conducting CIs. In this system, CIs are conducted by a team of paraprofessionals who conduct interviews and locate and evaluate contacts but do not perform other TB services. Three sites use this model.
Public health nurses (PHNs) conduct CIs. As part of a broad range of health services that they provide to the community, including services for other communicable diseases, PHNs conduct CIs. This type of system operates at two of the sites.
Mixed system. A mixed system is one in which most CIs are conducted by PHNs, while complicated and extensive CIs are handled by a dedicated CI team. One site uses this system.
Staffing
All sites use substantial staff resources to conduct CIs. Allocation of staff mirrors organizational structure. For example, within PHN systems, each PHN devotes less than 20 percent of his or her time to CIs. In systems with dedicated CI teams, few other staff persons serve as resources for CIs. Two of the sites with dedicated CI teams serve over 500 TB cases a year. Five sites designate a case manager for each CI who oversees its completion.
Educational background varies for staff involved in conducting CIs. The two PHN systems require nursing degrees, but only two sites require college degrees for their paraprofessional staff. The remaining sites require only a high school education, with managers noting that language and cultural skills are key requirements for CI staff. In fact, respondents at three sites reported recruiting staff for their ethnic/ cultural backgrounds and relevant language skills.
Training
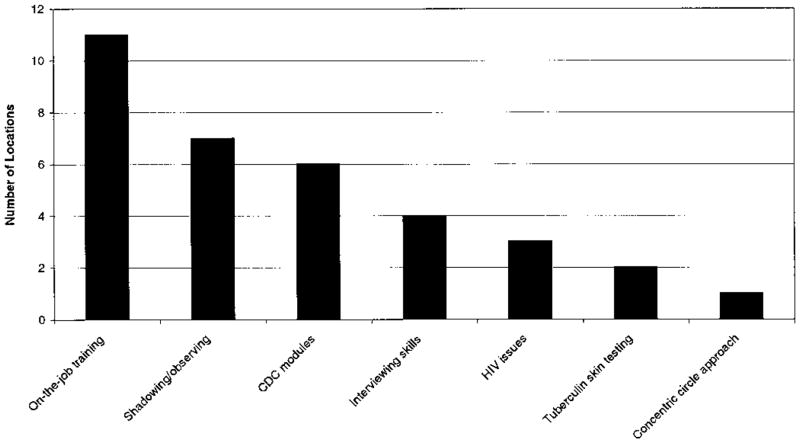
Across the 11 sites, staff receive very limited formal CI training. Informal, on-the-job training or training obtained by shadowing more experienced CI staff is offered at all sites. As Figure 3 illustrates, however, formal training is often confined to general TB knowledge training, providing little practical direction for conducting CIs. Four sites offer training in interviewing skills.
Figure 3.
Training topics and methods for contact investigation staff.
None of the interview respondents reported use of a proactive system to identify staff training needs. Several respondents reported that limited funds for training compelled them to use publicly available materials, such as CDC modules, or internal sources for training. Two sites, however, reported that they had worked with a local university to obtain training.
Data collection and management
Data collection
Staff at all 11 sites collect CI data at the individual level using locally developed forms to help organize the data. However, the content of forms varies widely, as does the extent to which forms are completed. Information on contacts is typically recorded on a single form that is filed in the TB patient’s chart. Other approaches to data collection include the following:
charts opened for all contacts identified
charts opened only for contacts receiving LTBI treatment
“family” files opened on all contacts identified within a family unit
Data management
Only three sites maintain a computer database of individual contacts. Three additional sites use computers to track aggregate information locally. Five sites use paper-based systems for managing local data. Information needed for program reporting to CDC is typically hand tallied and sent to the state TB program in aggregate form. Programs serving a larger number of TB cases were typically more automated than those serving fewer cases.
Monitoring
Respondents at nine sites reported having formal monitoring procedures to assess the quality of CIs conducted. Review of forms and charts by supervisors is the most common means of formal monitoring. Other methods, which vary across sites, include the following:
case management meetings
audits
reviews of daily plans
field observations of staff
Most monitoring focuses on timeliness of CI procedures. Site staff typically use the date of the first patient interview and the number of contacts identified per case to assess CI quality, with several sites reporting that identification of zero contacts is unacceptable.
At all 11 sites, respondents noted the importance of informal feedback. Supervisors typically have an “open door” policy with staff to promote communication and early identification of problems.
Respondents reported making little use of collected data to assess CI quality or operations, and only three sites reported using the data for policy development and planning. However, managers at one site use computerized data extensively to assess goals, objectives, and staff productivity and to determine when staff transfers are appropriate.
Challenges
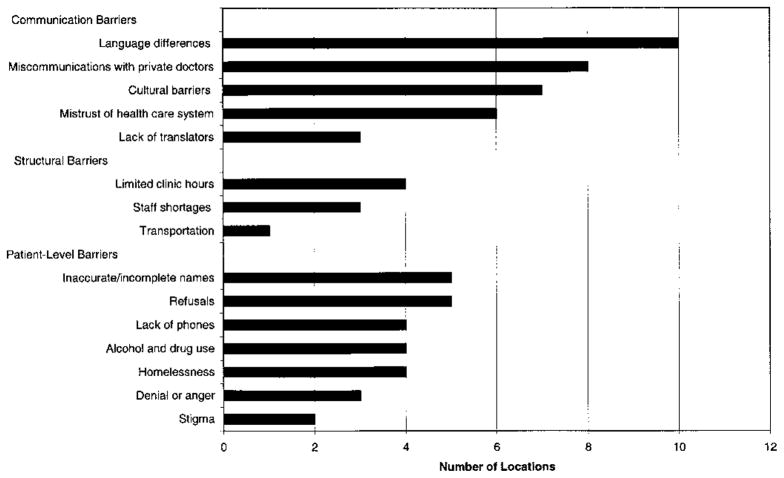
Although CI policies and procedures vary widely, many of the barriers reported by the 11 TB programs are shared across sites, as shown in Figure 4. These generally fall under three categories:
Figure 4.
Reported challenges to contact investigations.
Communication barriers, particularly between patients and program staff. Although programs seek to hire multilingual staff, respondents reported that it is difficult to meet all of the language needs of their diverse communities, and translators or bilingual professionals are often unavailable. Similarly, cultural barriers were noted between the TB program staff and the communities they serve. For example, a respondent at one site noted that a local population’s strong faith in homeopathic treatment hinders acceptance of Western medical treatment. At another site, a respondent noted that males from one local community are often unsupportive of medical care for their women and children. In addition, respondents at several sites cited communication barriers with private providers, especially pertaining to treatment regimens and reporting protocols.
Structural barriers, including limited clinic hours, transportation services, and adequate staffing.
Patient-level barriers, including alcohol and other drug use, mistrust of the health care system, anger and denial, and real or feared stigma. Respondents also noted that some TB patients, such as homeless persons, are unable to provide complete and correct names and addresses for contacts. Lack of a telephone was a common barrier.
Discussion
The findings from this study indicate wide variation among sites in CI policies, procedures, and practices. Although CI has been acknowledged as an important strategy to achieve TB prevention and control since the 1960s, neither the CDC nor the American Thoracic Society has issued any formal recommendations. Consequently, TB programs have had little guidance in developing their own CI systems. It is well documented that neither within TB control20 nor within the public health arena in general21 have program managers focused much attention on developing policies designed to prevent disease. The findings of this study support the literature, which indicates the focus is generally placed on patient-level issues rather than at the level of policy and program operations.
While the wide program variations and organizational structures limit the ability to compare programs directly, TB programs could clearly benefit from establishing a comprehensive CI infrastructure or system. CI staff could benefit from greater or more explicit guidance through their programs’ written policies. Training could be expanded and proactive methods developed to identify ongoing training needs. Similarly, the establishment of formal monitoring activities would reinforce CI policies and help guide systematic CI procedural improvements.
A clear plan articulating how CI activities are intended to meet program objectives would help translate objectives into meaningful program reform for quality improvement, and thus enable assessment of quality and efficacy of CIs.22 The importance of developing the CI infrastructure has been illustrated in recent studies, which have shown that clarifying screening policies and monitoring their implementation have a positive impact on TB prevention,23 as have improved training and formalized procedures.24
Since the time of this study, several sites have recognized the need for stronger infrastructures and, consequently, have revised their policies, bolstered staff training, and modified monitoring practices. In addition, new training materials, such as CDC’s recently published CI module,16 and training provided by the national TB Model Centers, may help standardize the practice of CI. National policy recommendations, if published, also would provide common terms and practices, thus enabling programs to share information and lessons learned effectively. The development of such a framework would enable program managers to assess the extent to which CI practices are appropriately implemented and to evaluate the impact of targeted CI interventions on improving the efficiency and quality of their programs. Given that CIs are labor and resource intensive, the ability to identify and implement “what works” can prevent costly problems as well as reduce the burden of TB.
Acknowledgments
The authors acknowledge the following tuberculosis program staff for making this study possible: William Paul and Jim McAuly in Chicago, IL; Beverly DeVoe, Brian Palmer, and Ruby Lewis Hardy in Fulton County, GA; Marcos Longoria and Kathy Penrose in Houston, TX; Charles Nolan and Kim Field in Seattle–King County, WA; Paul Davidson, Sue Gerber, Kathryn Koski, and Laura Knowles in Los Angeles County, CA; Paula Fujiwara, Chris Larkin, and Marie Dorsinville in New York City, NY; Eileen Napolitano and Akilah Ain in Newark, NJ; Kathy Moser in San Diego County, CA; Masae Kawamura and Tony Paz in San Francisco, CA; Karen Smith in Santa Clara County, CA; and William Moore and Linda Hamer in Shelby County, TN. The authors also thank Kathryn Koski and Linda Hamer for their assistance in reviewing this article; CDC staff Chuck Gaines, Gail Burns Grant, Andy Heetderks, Olga Joglar, Scott Jones, and Dan Ruggiero for facilitating project implementation; and Ann Lanner for editorial assistance.
Contributor Information
Maureen Wilce, Behavioral Scientist in the Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), in Atlanta, Georgia.
Robin Shrestha-Kuwahara, Behavioral Scientist in the Division of Tuberculosis Elimination, CDC, Atlanta, Georgia.
Zachary Taylor, Chief, Field Services Branch, Division of Tuberculosis Elimination, CDC, Atlanta, Georgia.
Noreen Qualls, Health Scientist in the Division of Tuberculosis Elimination, CDC, Atlanta, Georgia.
Suzanne Marks, Epidemiologist in the Division of Tuberculosis Elimination, CDC, Atlanta, Georgia.
References
- 1.Centers for Disease Control and Prevention. Tuberculosis Elimination Revisited: Obstacles, Opportunities, and a Renewed Commitment. MMWR. 1999;48(RR-9):1–12. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Essential Components of a Tuberculosis Control Program. MMWR. 1995;44(RR-11):3–17. [Google Scholar]
- 3.American Lung Association. Tuberculosis Elimination Programming in the 1990s, a Guide and Assessment Tool for Lung Associations. Chicago, IL: American Lung Association; 1991. [Google Scholar]
- 4.American Thoracic Society. Control of Tuberculosis in the United States. American Review of Respiratory Disease. 1992;146:1623–1633. doi: 10.1164/ajrccm/146.6.1623. [DOI] [PubMed] [Google Scholar]
- 5.Etkind SC. Contact Tracing in Tuberculosis. In: Reichman L, Herschfield E, editors. TB: A Comprehensive International Approach. Lung Biology in Health and Disease. New York: Marcel Dekker; 1993. [Google Scholar]
- 6.Glaser T, Simmons C. Investigation of Contacts to Tuberculosis Cases Symposium Summary. New York: New York City Department of Health, Bureau of Tuberculosis Control; 1996. Contact Investigation in New York City; pp. 13–18. [Google Scholar]
- 7.Holcome JM. Investigation of Contacts to Tuberculosis Cases Symposium Summary. New York: New York City Department of Health, Bureau of Tuberculosis Control; 1996. Contact Investigation in a Rural Setting: A State Perspective; pp. 20–25. [Google Scholar]
- 8.Ruben FL, Lynch DC. Tuberculosis Control through Contact Investigation. Pennsylvania Medicine. 1996;99(5):22–23. [PubMed] [Google Scholar]
- 9.Chin DP, et al. Spread of Mycobacterium Tuberculosis in a Community Implementing Recommended Elements of Tuberculosis Control. JAMA. 2000;283(22):2968–2974. doi: 10.1001/jama.283.22.2968. [DOI] [PubMed] [Google Scholar]
- 10.Shrestha-Kuwahara R, et al. Patient-Provider Communication during TB Contact Investigation. International Journal of Tuberculosis and Lung Disease. 1999;3(9):S139. [Google Scholar]
- 11.McAnulty JM, et al. Missed Opportunities for Tuberculosis Prevention. Archives of Internal Medicine. 1995;155:713–716. [PubMed] [Google Scholar]
- 12.Marks SM, et al. Outcomes of Contact Investigations of TB Patients. American Journal of Respiratory Critical Care Medicine. 2000;162(6):2033–2038. doi: 10.1164/ajrccm.162.6.2004022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 1997. Atlanta, GA: CDC; 1998. [Google Scholar]
- 14.Carey JS, et al. CDC EZ_Text: Software for Collection, Management, and Analysis of Semistructured Qualitative Databases, Version 3.05. Atlanta, GA: Conwal, Inc., for the Centers for Disease Control and Prevention; 1997. [Google Scholar]
- 15.Loucks-Horsley S. The Design of Templates as Tools for Formative Evaluation. New Directions for Evaluation. 1996;72:5–24. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Self-Study Modules on Tuberculosis: Contact Investigations for Tuberculosis. Atlanta, GA: CDC; 1999. [Google Scholar]
- 17.Advisory Committee for the Elimination of Tuberculosis. The Use of Preventive Therapy for Tuberculosis Infection in the United States. Atlanta, GA: Government Printing Office; 1996. [Google Scholar]
- 18.Centers for Disease Control and Prevention. Core Curriculum on Tuberculosis. Atlanta, GA: CDC; 2000. [Google Scholar]
- 19.Bass JB, et al. Treatment of Tuberculosis and Tuberculosis Infection in Adults and Children. American Journal of Respiratory Disease. 1994;149:1359–1374. doi: 10.1164/ajrccm.149.5.8173779. [DOI] [PubMed] [Google Scholar]
- 20.Walt G. The Politics of Tuberculosis: The Role of Process and Power. In: Porter J, Grange J, editors. Tuberculosis: An Interdisciplinary Perspective. London: Imperial College Press; 1999. pp. 67–98. [Google Scholar]
- 21.Brownson RC, et al. Policy Research for Disease Prevention: Challenges and Practical Recommendations. American Journal of Public Health. 1997;87(5):735–739. doi: 10.2105/ajph.87.5.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wholey JS. Assessing the Feasibility and Likely Usefulness of Evaluation. In: Wholey JS, Hatry HP, Newcomer KE, editors. Handbook of Practical Program Evaluation. San Francisco, CA: Jossey-Bass; 1994. pp. 15–39. [Google Scholar]
- 23.MacIntyre CR, Plant AJ. Impact of Policy and Practice on Effectiveness of Contact Screening for Tuberculosis. Preventive Medicine. 1998;27:830–837. doi: 10.1006/pmed.1998.0366. [DOI] [PubMed] [Google Scholar]
- 24.Jasmer RM, et al. A Molecular Epidemiologic Analysis of Tuberculosis Trends in San Francisco, 1991–1997. Annals of Internal Medicine. 1999;130(12):971–978. doi: 10.7326/0003-4819-130-12-199906150-00004. [DOI] [PubMed] [Google Scholar]