Abstract
Damage to the medial collateral ligament of the elbow from an instability episode usually heals with non-operative treatment. In some cases, residual instability may occur, leading to functional impairment.
Non-operative management can be successful when bracing, taping and therapy are used to stabilise the elbow.
A recent report detailing the efficacy of platelet-rich plasma in effectively treating ulnar collateral ligament (UCL) injuries in throwers has shown promise. However, there remain specific groups that should be considered for repair or reconstruction. These may include throwing athletes, wrestlers and some individuals involved in highly active physical activity which demands stability of the elbow.
The results of surgical repair and reconstruction allowing a return to sports are quite good, ranging from 84% to 94%. Complications are generally low and mostly centred on ulnar nerve injuries.
This report represents a review of the literature concerning valgus instability over the past five years, supplemented by selective older articles where relevant.
Cite this article: EFORT Open Rev 2017;2:1-6. DOI:10.1302/2058-5241.2.160037.
Keywords: elbow, instability, medial ulnar collateral ligament
Introduction
Valgus instability of the elbow is common in United States baseball pitchers and is not infrequent in gymnasts, javelin throwers, other overhead athletes and wrestlers. Although trauma more commonly affects the lateral side, valgus instability may also occur after traumatic dislocations with fracture. Overall, however, injury to the medial ulnar collateral ligament (MUCL) has become increasingly common.1 Waris2 first described injuries to the MUCL of the elbow in 1946. Over the following years, our understanding of MUCL anatomy and function has increased dramatically. In 1974, Jobe, Stark and Lombardo3 adapted an old method used for polio patients and performed the first successful MUCL reconstruction, changing what was then a career-ending injury into one that could potentially be overcome and allow for a return to play. In 1986, Jobe et al3 described their technique of reconstructing the ligament using an ipsilateral palmaris longus tendon autograft in a figure-of-eight pattern via a flexor pronator mass detachment approach with sub-muscular transposition of the ulnar nerve. Since Jobe’s original description, numerous modifications of surgical technique have been designed to improve athletic performance and decrease patient morbidity.4-9 Erickson et al10 and Vitale and Ahmad8 recently published systematic reviews of all published reports of MUCL reconstruction in overhead athletes.11-27
Anatomy and biomechanics
The main stabilisers for valgus stability are the MUCL (static) and the flexor-pronator mass (dynamic). The MUCL is composed of three separate bundles: anterior; posterior; and transverse (Fig. 1). The anterior bundle is the primary restraint to valgus stress. Some authors describe two separate bundles in the anterior band and others describe simply different tensions within different parts of the MUCL in varying degrees of flexion. The ligament itself has a fan-shaped origin from the most lateral aspect of the anterior distal medial epicondyle, deep to the flexor pronator muscle and just medial to the medial capsule (Fig. 2). The ligament then runs distally to insert on the sublime tubercle of the medial ulna. The posterior and transverse ligaments are not thought to contribute to valgus stability, leaving the anterior bundle to serve as the main restraint. In the overhead throwing motion, the ligament is subjected to repetitive microtrauma, resulting in damage, tearing and insufficiency.
Fig. 1.
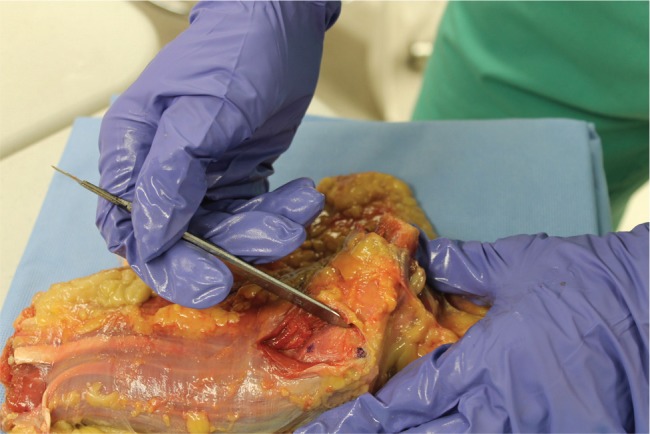
Summary of medial ulnar collateral ligament (MUCL) allograft reconstruction.
Fig. 2.
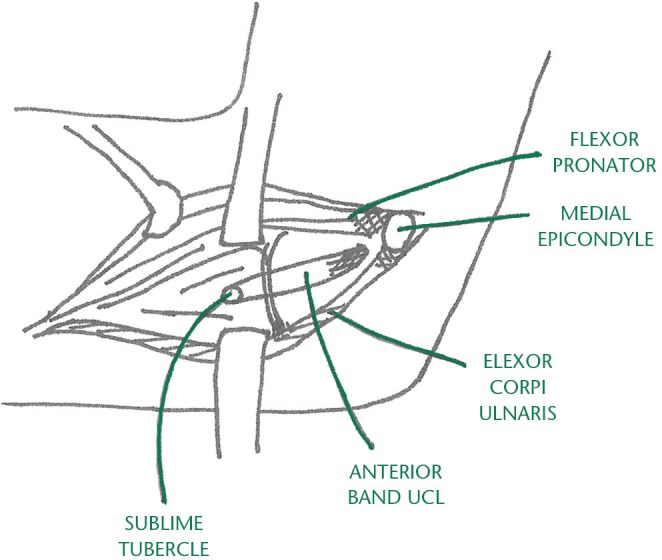
Anatomy of the medial ulnar collateral ligament (MUCL) via a muscle-split approach.
History and physical examination
The most common complaint is medial elbow pain with activity. Throwing athletes may describe loss of velocity or accuracy, while grapplers will describe a ‘giving way’ of the elbow. There is usually a cessation of pain when not performing physical activity.
Examination of the elbow will reveal normal contour and musculature. Medial swelling may be present in acute injuries but is not common in the chronic situation. Patients are usually point-tender medially over the course of the ligament. A careful examination can differentiate the tenderness as proximal, middle or distal. Motion is usually not limited in acute and subacute cases, but chronic overuse injuries may produce a loss of extension due to medial olecranon spurring and posterior impingement.
Instability testing, including valgus stress at 30°, 60° and 90°; the “Milk” tests; the moving valgus stress test; and the valgus extension overload test will usually reproduce pain and feelings of instability. There is usually only a subtle side-to-side difference in these various examination manoeuvres, but when all manoeuvres are used a diagnosis may be made with relative certainty.
The ulnar nerve should be very carefully evaluated for location and subluxation by palpation and with Tinel’s compression test for inflammation.
Imaging
Standard posterioanterior and lateral radiographs are usually normal, although in chronic cases posterior and medial olecranon osteophytes may be noted. Valgus stress radiographs may show a side-to-side difference. Plain MRI testing can show damage to the MUCL, but the gold standard of advanced imaging is the MR arthrogram. Cicotti21 has recently reported on the efficacy of static and dynamic ultrasound in the diagnosis of injuries to the ligament.
Management
Non-operative management
Although non-operative treatment is commonly used, Rettig et al28 reviewed a series of baseball players managed with rest and rehabilitation. Only 42% were able to return to sports activity at a mean time of six months from diagnosis. Podesta et al29 recently reported improved results using platelet-rich plasma (PRP) in a series of partial MUCL tears. In our review of a series of 25 athletes with significant injuries to the proximal or distal end of the MUCL managed with bracing, therapy and a series of leuckocyte-rich PRP injections, 21 of 22 primary injuries were shown to have healed or reconstituted their MUCL on post-treatment MRI testing.30 However, only one of three patients with successful prior surgery who re-injured the same elbow was able to heal the new injury with this treatment regimen.
Operative repair
Savoie et al31 have reported on the repair of proximal or distal avulsion injuries in younger athletes with a 97% return-to-sport result. This was a younger group of patients with an otherwise normal ligament, certainly a factor in the successful return to play. Surgery was performed by the medial muscle-splitting approach developed by Smith et al30 with direct repair to an anchor. Dugas32 recently presented a series of acute repairs performed with an internal brace supplemented with collagen-impregnated tape with excellent return-to-play results.
Surgical technique for MUCL reconstruction
The most common method of treatment of valgus instability is reconstruction. A variety of graft choices are available, including ipsilateral and contralateral palmaris or gracilis tendons, toe extensors and allografts. There is no clear difference in using various grafts according to the reports.
An examination under anaesthesia is performed to evaluate the degree of instability and range of motion (ROM) and to compare both with the opposite side. Most patients had a diagnostic arthroscopy in either the prone or lateral position to confirm the instability and manage any intra-articular pathology followed by open ligament reconstruction.
An incision of approximately 6 cm is made from the posterior proximal tip of the medial epicondyle, extending distally past the location of the sublime tubercle. Although the location of the incision minimises risk to the medial antebrachial cutaneous nerve, the subcutaneous tissue is dissected bluntly to identify and protect this nerve and prevent painful neuroma formation.
An incision is then made in the flexor-pronator fascia between its middle and posterior bands, just posterior to the medial conjoined tendon, and the underlying muscle belly is divided longitudinally. The MUCL is visualised and the damage confirmed. A longitudinal incision is made at the anterior aspect of the ligament, then remnants of the native MUCL are reflected posteriorly off the sublime tubercle and the medial epicondyle to reveal the anatomical origin and insertion of the ligament. The initial reflection allows for direct visual assessment of medial joint line opening with valgus stress. If the pre-operative assessment of instability and ligament damage is confirmed, the graft is then harvested, if necessary, and prepared. On the ulnar side, there are two basic options: one is to place standard Jobe-converging tunnels around the sublime tubercle using a 3.2 mm drill bit and the other is to place a single ulnar tunnel and fix the middle of the graft with an interference screw. If a single tunnel is used, it is centred on the sublime tubercle and angled towards supinator crest of the lateral ulna. Unicortical reaming over a guide pin using either a 4.5 mm or a 5.0 mm reamer is performed. The graft is then attached to an interference screw via a suture through the screw using a previously described technique33 and then manually inserted into the ulnar tunnel.
The proximal reconstruction is performed, either with a classic Jobe technique through ‘Y’ type drill holes with the graft often pulled back through the central humeral tunnel to create a tripled graft or with a docking technique. The elbow is cycled and the grafts tensioned in 70° of flexion, then forearm supination with a varus stress is applied to the elbow. Any remnant of the native ligament is sutured to the allograft. The flexor pronator fascia is closed with absorbable suture.
Post-operative management
The patient is placed in a removable hinged brace on the first post-operative visit, usually one week after surgery, and begins scapular retraction exercises. Gentle, pain-free ROM is allowed while out of the brace, which is initially set to restrict motion from 60° to 90°. Grip-strengthening and forearm-stretching exercises are encouraged at this time. The patients are allowed to add 10° to both flexion and extension on a weekly basis as the pain-free arc improves. Six weeks post-operatively, ROM is expected to be equal to the pre-operative arc of motion. Physical therapy at this six-week mark is performed while within the brace and emphasises strength and flexibility, core strengthening, and scapular retraction and shoulder rehabilitation, including posterior capsule and rotator cuff stretching and strengthening. The 12-week visit is considered a key landmark in post-operative rehabilitation. If there is no swelling, ROM is equal to or better than the pre-operative visit, and posture and core strength are satisfactory, then a throwing programme is initiated with the brace in place. If any of these milestones are not in place, the throwing programme is delayed. The most common reason for delay is usually persistent scapular dyskinesis, treated with a combination of bracing, taping and continued rehabilitation. The throwing programme is then continued in the hinged elbow brace for at least the next six to eight weeks. Barring any setbacks in pain, swelling in the elbow or recurrence of shoulder/core/posture issues, the throwing programme is restarted at 4.5 to 5 months without the brace and progressed according to normal return-to-throwing protocols.6
We recently reported on our series of MUCL reconstructions using a gracilis allograft.34 We performed a retrospective review of a consecutive series of patients involved in throwing sports (baseball, softball and javelin) undergoing allograft reconstruction of the MUCL between 2005 and 2009, to correct symptomatic instability, functional impairment and an inability to return to sport despite extensive non-operative management. In total, 116 of 123 (95%) patients were contacted more than 24 months after the surgery. Seven patients (5%) could not be contacted and were excluded. The pre-operative examination revealed evidence of valgus instability, a positive physical examination finding of 1 to 3+ laxity and a positive moving valgus extension overload test in all patients. ROM was normal in 81 patients and abnormal in 35, the latter of which had flexion contractures of between 5° and 25°. Initial radiographs were normal in 81 patients, 15 appeared to have minor changes in the olecranon tip and fossa, and 20 had moderate changes.
Initial management in all patients included a period of medication, rest and rehabilitation of at least six weeks. The 28 patients underwent bracing after the initial visit in an attempt to allow healing of the injured MUCL. All patients had either an MRI or MRA which was positive for MUCL disruption. There was a mixture of professional (n = 23), collegiate (n = 48) and high school (n = 45) athletes. The mean age at the time of MUCL reconstruction was 20.4 years (14 to 32). All reconstructions were performed through a split in the flexor-pronator mass, as described by Rohrbough et al,35 and no ulnar nerve transpositions were performed. Others have reported similar results.36-40
Results of our technique
The results of our study were fairly representative of the literature and showed that 110 of the 116 patients contacted were able to return to play. Six of the 116 did not return to play. Three of these six patients volunteered that their failure to return to overhead sports was unrelated to elbow symptoms, but they did not give specific reasons for not returning to sport. The three others that did not return to sport were due to sequelae of a medial epicondyle fracture (one patient), a new flexor-pronator tear (one patient) and inability to recover velocity with ongoing pain when throwing (one patient). The average time until the patients began throwing in a structured return-to-pitch programme was 5.5 months (3 to 8) and the average time to return to competition was 9.9 months (4.5 to 18). Seventy patients stated that they had reached their point of maximum recovery at fewer than ten months post-operatively, 29 patients stated maximum recovery between ten and 12 months, and 17 felt that recovery required more than one year, feeling much better in the second season back to throwing. Of the 110 patients who had resumed competition, 33 patients (30%) were competing at a level of competition above their pre-operative level, 64 (58%) patients at the same level and 13 (12%) at a level below their pre-injury level. Conway-Jobe scores were calculated as excellent in 93 patients (80%), good in 15 patients (13%) and fair in eight patients (7%); no patient outcome was rated as poor. Of the 116 patients, 114 (98%) reported being satisfied with the results of their reconstruction and reported it as being successful. Two patients were not satisfied with their final result, one due to persistent pain and one due to complications from a medial epicondyle fracture. There were no intra-operative complications. Post-operative complications occurred in seven (6%) patients. One patient had post-operative motor and sensory ulnar neuropathy that resolved over time and did not affect his ultimate satisfactory result. Two patients developed late (> 2 years) post-operative sensory neuropathy; one of these required ulnar nerve release. Both patients returned to play. Two patients developed post-operative wound issues; one required a local debridement of a haematoma and one an oral antibiotic for a stitch abscess. Both of these patients returned to play. One patient sustained a medial epicondyle fracture after return to sport and did not resume throwing after this injury. One patient sustained a flexor-pronator muscle and tendon tear 14 months post-operatively and returned at a lower level of play once this healed. Among the 116 patients evaluated, none of the MUCL allograft reconstructions clinically failed and no revision reconstructions were performed.
Discussion
The vast majority of MUCL injuries occur in overhead throwing athletes, especially baseball pitchers.3 Jobe3 described MUCL reconstruction in 1986, changing the MUCL injury from career-ending to one with a chance of recovery and return to sport. The original technique by Jobe et al3 described a figure-of-eight reconstruction using a palmaris longus autograft. The flexor-pronator mass was elevated and the ulnar nerve was routinely transposed. Many modifications of the ‘classic’ Jobe technique have emerged since the original description.8 The two most commonly performed modifications are the docking technique, described by Althchek, and the Andrews technique. Both of these techniques have been shown to be quite successful in returning athletes to play.13,30,35
Complications are relatively rare. The most common problem is a failure to return to the same level of play, which occurs 5% to 32% of the time. Complications stemming from autograft harvest include harvest-site superficial infections, symptoms related to scarring and occasional cutaneous tenderness. Much more significant injuries, including at least six cases4,5,7,9 of median nerve harvest, have also been reported. In their outcome review study, Vitale et al8 showed an overall 10% complication rate in MUCL reconstructions, ranging from 3% to 25% between studies, with 1% of all complications stemming from graft harvest alone.8 Cain reported an overall complication rate of 20%, with 4% due to donor site problems. Vitale et al8 reported an 83% (excellent) Conway-Jobe rating in their literature review of 328 MUCL autograft reconstructions.
In our series using allograft, 83% of patients also received a Conway-Jobe rating of excellent. Vitale et al8 documented a return to sport between 9.8 and 26.4 months throughout the studies. Several studies have reported an earlier return to play with a more advanced post-operative protocol. This protocol was based, at least in part, on the authors’ perception that the MUCL is an extra-articular ligament, not an anterior cruciate ligament (ACL), and that rehabilitation should be closer to the medial collateral ligament of the knee than to an ACL. Earlier post-surgical rehabilitation of the hip, back, scapula and shoulder, while the elbow reconstruction is protected by a brace, may allow an earlier return to play.
Valgus instability of the elbow is not uncommon in overhead-throwing athletes. Surgical management has an excellent return-to-play result in most studies. Various modifications of the original Jobe technique3 have been described, but in each case the results seem to be satisfactory.
Footnotes
ICMJE Conflict of Interest Statement: FS has received financial support outside of this work in the form of speaker fees from Mitek and Smith & Nephew and from royalties from Exactech. MO’B has received financial support outside of this work in the the form of consultancy fees from Smith & Nephew, DePuy and Mitek.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004;32:1158-1164. [DOI] [PubMed] [Google Scholar]
- 2. Waris W. Elbow injuries in javelin throwers. Acta Chir Scand 1946;93:563-575. [PubMed] [Google Scholar]
- 3. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg [Am] 1986;68-A:1158-1163. [PubMed] [Google Scholar]
- 4. Geldmacher J. Median nerve as free tendon graft. Hand 1972;4:56. [DOI] [PubMed] [Google Scholar]
- 5. Kovácsy A. [Removal of the median nerve instead of the palmaris longus tendon]. Magy Traumatol Orthop Helyreallito Seb 1980;23:156-158. (Article in Hungarian) [PubMed] [Google Scholar]
- 6. Paletta GA, Jr, Wright RW. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med 2006;34:1594-1598. [DOI] [PubMed] [Google Scholar]
- 7. Vastamäki M. Median nerve as free tendon graft. J Hand Surg Br 1987;12:187-188. [DOI] [PubMed] [Google Scholar]
- 8. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med 2008;36:1193-1205. [DOI] [PubMed] [Google Scholar]
- 9. Weber RV, Mackinnon SE. Median nerve mistaken for palmaris longus tendon: restoration of function with sensory nerve transfers. Hand (N Y) 2007;2:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erickson BJ, Harris JD, Chalmers PN, et al. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health 2015;7:511-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmad CS, Grantham WJ, Greiwe RM. Public perceptions of Tommy John surgery. Phys Sportsmed 2012;40:64-72. [DOI] [PubMed] [Google Scholar]
- 12. Ahmad CS, Lee TQ, ElAttrache NS. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med 2003;31:332-337. [DOI] [PubMed] [Google Scholar]
- 13. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med 1995;23:407-413. [DOI] [PubMed] [Google Scholar]
- 14. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med 2000;28:16-23. [DOI] [PubMed] [Google Scholar]
- 15. Bica D, Armen J, Kulas AS, Youngs K, Womack Z. Reliability and precision of stress sonography of the ulnar collateral ligament. J Ultrasound Med 2015;34:371-376. [DOI] [PubMed] [Google Scholar]
- 16. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg 2010;19:110-117. [DOI] [PubMed] [Google Scholar]
- 17. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med 2010;38:2426-2434. [DOI] [PubMed] [Google Scholar]
- 18. Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med 2003;31:621-635. [DOI] [PubMed] [Google Scholar]
- 19. Carrino JA, Morrison WB, Zou KH, et al. Noncontrast MR imaging and MR arthrography of the ulnar collateral ligament of the elbow: prospective evaluation of two-dimensional pulse sequences for detection of complete tears. Skeletal Radiol 2001;30:625-632. [DOI] [PubMed] [Google Scholar]
- 20. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg 2001;9:99-113. [DOI] [PubMed] [Google Scholar]
- 21. Ciccotti MG, Atanda A, Jr, Nazarian LN, et al. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med 2014;42:544-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg [Am] 1992;74-A:67-83. [PubMed] [Google Scholar]
- 23. Dargel J, Küpper F, Wegmann K, et al. Graft diameter does not influence primary stability of ulnar collateral ligament reconstruction of the elbow. J Orthop Sci 2015;20:307-313. [DOI] [PubMed] [Google Scholar]
- 24. Dick R, Sauers EL, Agel J, et al. Descriptive epidemiology of collegiate men’s baseball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train 2007;42:183-193. [PMC free article] [PubMed] [Google Scholar]
- 25. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med 2007;35:2039-2044. [DOI] [PubMed] [Google Scholar]
- 26. Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med 2009;37:566-570. [DOI] [PubMed] [Google Scholar]
- 27. Dines JS, Jones KJ, Kahlenberg C, et al. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med 2012;40:148-151. [DOI] [PubMed] [Google Scholar]
- 28. Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med 2001;29:15-17. [DOI] [PubMed] [Google Scholar]
- 29. Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med 2013;41:1689-1694. [DOI] [PubMed] [Google Scholar]
- 30. Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A muscle-splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am J Sports Med 1996;24:575-580. [DOI] [PubMed] [Google Scholar]
- 31. Savoie FH, III, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med 2008;36:1066-1072. [DOI] [PubMed] [Google Scholar]
- 32. Dugas J. Repair of UCL injuries of the elbow utilizing an internal brace: a preliminary report. Lecture presented at the AANA Fall Course; Dallas, Texas, USA, 2015. Jan. www.aana.org [Google Scholar]
- 33. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med 2000;28:16-23. [DOI] [PubMed] [Google Scholar]
- 34. Savoie FH, III, Morgan C, Yaste J, Hurt J, Field L. Medial ulnar collateral ligament reconstruction using hamstring allograft in overhead throwing athletes. J Bone Joint Surg [Am] 2013;95:1062-1066. [DOI] [PubMed] [Google Scholar]
- 35. Rohrbough JT, Altchek DW, Hyman J, Williams RJ, III, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med 2002;30:541-548. [DOI] [PubMed] [Google Scholar]
- 36. Conway JE. The DANE TJ procedure for elbow medial ulnar collateral ligament insufficiency. Tech Shoulder Elbow Surg 2006;7:36-43. [Google Scholar]
- 37. Dodson CC, Thomas A, Dines JS, et al. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med 2006;34:1926-1932. [DOI] [PubMed] [Google Scholar]
- 38. Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy 2006;22:1187-1191. [DOI] [PubMed] [Google Scholar]
- 39. Safran M, Ahmad CS, Elattrache NS. Ulnar collateral ligament of the elbow. Arthroscopy 2005;21:1381-1395. [DOI] [PubMed] [Google Scholar]
- 40. Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg 2001;10:152-157. [DOI] [PubMed] [Google Scholar]


