Abstract
An estimated 40% of the US population have foot problems.
Of all patients aged over 50 years, 2.5% report degenerative arthritis of the first metatarsophalangeal (MTP) joint, termed ‘hallux rigidus’. First MTP osteoarthritis is the most common arthritic condition in the foot.
Progression of great toe arthritis is associated with pain and loss of motion. Non-surgical intervention begins with shoe modifications and orthotics designed to limit MTP motion.
In patients with mild arthritis, operative procedures focus on removing excess osteophytes (cheilectomy) to prevent dorsal impingement with or without a concomitant osteotomy (Moberg) to improve or shift range of motion into a less painful arc.
In patients with more advanced arthritis, operative management has centred on arthrodesis of the first MTP joint.
A recent Level 1 study shows excellent function and pain relief with a small hydrogel hemi-implant into the metatarsal head
Multiple joint-sparing procedures such as joint arthroplasty or resurfacing have been described with inconsistent results.
Cite this article: EFORT Open Rev 2017;2:13–20. DOI: 10.1302/2058-5241.2.160031
Keywords: great toe arthritis; hemi-arthroplasty; arthrodesis; hydrogel, hallux rigidus
Introduction
An estimated 40% of the United States population have foot problems.1 Of all patients aged over 50 years, 2.5% report degenerative arthritis of the first metatarsophalangeal (MTP) joint, termed ‘hallux rigidus’. First MTP osteoarthritis hallux rigidus is the most common arthritic condition in the foot.
Progression of great toe arthritis is associated with pain and loss of motion. Non-surgical intervention begins with shoe modifications and orthotics designed to limit MTP motion. In patients with mild arthritis, operative procedures focus on removing excess osteophytes (cheilectomy) to prevent dorsal impingement with or without a concomitant osteotomy (Moberg) to improve or shift range of motion into a less painful arc. In patients with more advanced arthritis, operative management has centred on arthrodesis of the first MTP joint. Multiple joint-sparing procedures such as joint arthroplasty or resurfacing have been described with inconsistent results.
Pathophysiology
The cause of hallux rigidus is unclear. While arthritis can be caused by traumatic or iatrogenic injuries that directly cause damage to the articular cartilage of the MTP joint, most commonly the aetiology of hallux rigidus is idiopathic. Previous reports have shown that almost two-thirds of patients have a family history and up to 79% patients have bilateral involvement.2 Coughlin and Shurnas reported an association of hallux rigidus with metatarsal head articular shape, metatarsal adductus and hallux valgus interphalangeus.2 They reported no association with trauma, shoe wear, Achilles tightness or metatarsus primus elevatus.
As hallux rigidus progresses, the normal coupling of the centre of rotation of the proximal phalanx and metatarsal head is disrupted, leading to eccentric gliding of proximal phalanx on the metatarsal head.3 Osteophytes form preferentially on the dorsal surface and are commonly horseshoe-shaped. There is a progressive decrease in range of motion, primarily with dorsiflexion.
Clinical evaluation
Patients typically present with a history of pain and stiffness that is worse with activities, particularly with first MTP dorsiflexion involvement, such as stairs, running or push-ups. Discomfort during ambulation is worse during the heel-rise and toe-off. Symptoms are often improved with stiff sole shoes such as boots and worse with those with a flexible sole such as tennis shoes and sandals. Patients may report numbness and paraesthesiae from compression of the dorsomedial cutaneous nerve between dorsal osteophytes and footwear.
On examination, tenderness is localised to the dorsal joint and osteophytes can often be visualised and palpated. Patients report pain at the extremes of dorsiflexion from impingement of the dorsal osteophytes, and pain on plantarflexion from traction of the extensor hallucis longus (EHL) over the dorsal osteophytes. Pain with compression of the first MTP joint, also known as ‘grind testing’, and pain during the middle of range of motion may indicate more advanced arthritis. Patients may also demonstrate hyperextension of the first interphalangeal (IP) joint as a reaction to limited first MTP dorsiflexion.
Normal first MTP motion consists of approximately 75° of dorsiflexion and 35° of plantarflexion.3 Patients with hallux rigidus have decreased range of motion, with noticeable differences between their affected and normal extremities.
Imaging should consist of standing anteroposterior (AP), oblique and lateral radiographs. On the AP view, decreased joint space with flattening and widening of the metatarsal head with subchondral sclerosis may be visualised. On the lateral view, dorsal osteophytes over the base of the proximal phalanx and the metatarsal head can be seen, along with joint-space narrowing. Hattrup and Johnson defined a classification system for hallux rigidus based on radiographs with three different grades (Table 1).4 CT and MRI are not necessary for evaluation.
Table 1.
Hattrup and Johnson radiographic classification of hallux rigidus
| Grade | Radiographic findings |
|---|---|
| I | Preservation of joint space, mild osteophyte formation |
| II | Mild to moderate joint-space narrowing, moderate osteophyte formation, subchondral sclerosis and cysts |
| III | Severe joint-space narrowing, significant osteophyte formation, loose bodies, subchondral sclerosis and cysts |
The most commonly used classification for hallux rigidus was introduced by Coughlin and Shurnas, and uses both clinical and radiographic findings.5
Non-operative management
Treatment of hallux rigidus should begin with non-operative measures aimed at pain relief. Non-steroidal anti-inflammatory drugs may alleviate acute episodes of exacerbation. Activity modifications include avoiding those that involve extreme dorsiflexion of the first MTP, such as stairs or running.
Orthotics are designed to limit motion across the first MTP joint while providing cushioning and plantar pressure distribution. While a carbon fibre footplate provides coverage of the entire foot, a Morton’s extension leaves the lesser toe MTP joints uncovered, which may be desirable in young and active patients (Fig. 1). Carbon fibre inserts are paired with overlying soft fabric over-the-counter insoles that provide cushioning and comfort.
Fig. 1.

Morton’s extension.
Shoe modifications include high and wide toe boxes to prevent compression of dorsal osteophytes. A rocker bottom sole can also be added to decrease dorsiflexion motion of the first MTP joint by rocking the foot from heel-strike to toe-off.
Injections of steroids or hyaluronic acid into the first MTP joint may provide temporary relief. Pons et al found improvement in pain and function in a prospective randomised trial of 37 patients comparing steroid and hyaluronic acid injections at three months.6 While no differences between groups were found in rest pain or clinical examination, the hyaluronic acid group demonstrated improved gait pain at 28 days and 56 days.
Non-operative treatment can be successful for many patients. Grady et al reported a 55% success rate with non-operative treatment including orthotics, corticosteroid injections and shoe modifications in a retrospective review of 772 patients.7
Operative management
Cheilectomy
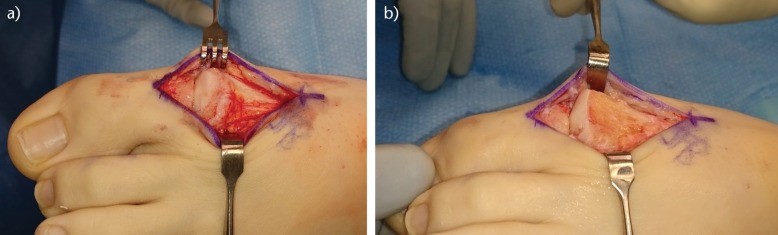
For patients with grade 1 or 2 hallux rigidus, a cheilectomy is a good option. First described in 1959 by DuVries, it involves resection of the dorsal one-third of the articular surface of the metatarsal head, along with dorsal osteophytes of the metatarsal head and proximal phalanx (Fig. 2).8 The ideal patient for a cheilectomy has primarily dorsal symptoms from impingement, large dorsal osteophytes on radiographs and minimal to mild joint-space narrowing. It is important to avoid resection greater than one-third of the dorsal metatarsal head, as this can lead to dorsal subluxation of the proximal phalanx.9
Fig. 2.
Cheilectomy. a) Dorsal osteophyte with dorsal and lateral arthritic changes to the metatarsal head, b) resection of dorsal osteophyte and 30% of the metatarsal head.
Long-term results of cheilectomies have been favourable, with high satisfaction and low rates of conversion to arthrodesis. In a retrospective study of 89 patients treated with cheilectomy with average 9.6-year follow-up, Coughlin and Shurnas reported 97% good to excellent results and 92% success in pain relief and function.5 Six patients (7%) required conversion to arthrodesis. Similarly, Nawoczenski et al reported 91% satisfaction and 1.7 (out of 10) average VAS pain scores in a prospective study of 11 patients at average 6.2-year follow-up.10 One patient (9%) required conversion to arthrodesis and three patients (27%) reported limitations in physical activities.
Recurrence of dorsal osteophytes has been reported at 31% in a retrospective study of 75 feet by Easley et al.11 A total of 43% of these patients had pain at the middle of range of motion, suggesting that recurrence may be principally a result of progression of arthritis.
Cheilectomies have traditionally been limited to patients with grade 1 or 2 hallux rigidus and previous studies have reported decreased success in patients with more advanced hallux rigidus. Easley et al reported on 12 retrospective cases of cheilectomy with Hattrup and Johnson grade 3 hallux rigidus on radiographs.11 Three cases (25%) required conversion to arthrodesis at average 6.9-year follow-up. Coughlin et al found similar results in nine cases with grade 3 hallux rigidus on radiographs, with five cases (56%) requiring conversion to arthrodesis at average 9.6-year follow-up.5 While patients with more advanced arthritis can have success with cheilectomy, they must be cautioned regarding the high rates of revision surgery.
Although many patients show radiographic evidence of arthritis progression after cheilectomy, this does not appear to affect clinical outcomes. Feltham et al examined 67 patients who underwent cheilectomy and found on radiographs that 6/17 grade I and 24/39 grade II patients progressed to grade III at average 5.4-year follow-up.12 However, none of these patients required additional surgery.
It is important to counsel patients pre-operatively that a cheilectomy is a pain-relief procedure. It provides only mild improvements in range of motion and patients must be cautioned that their motion will not return to normal. While intra-operative dorsiflexion often reaches 80° to 90°, clinical dorsiflexion is much lower at around 21° to 39°.11,13 Nawoczenski et al prospectively evaluated 20 patients with grades I to III hallux rigidus before and after cheilectomy, and found that dorsiflexion during gait improved by 12° while abduction increased by 5°.10 Smith et al prospectively evaluated 17 patients with stage I and stage II hallux rigidus after cheilectomy, and found an average improvement of 16.7° in functional first MTP range of motion with gait analysis.14 However, clinical evaluation of first MTP range of motion is difficult, and Vulcano et al demonstrated that clinical measurement can underestimate range of motion seen on radiographs by an average of 13°.13
Moberg osteotomy
A Moberg osteotomy consists of a dorsiflexion osteotomy of the proximal phalanx and was first described by Bonney and Macnab in 1952.15 It is a closing-wedge osteotomy and acts to shift the arc of motion of the first MTP joint into more dorsiflexion by sacrificing plantarflexion. Cadaveric analysis by Kim et al demonstrated that the Moberg osteotomy also shifts the contact pressure of the proximal phalanx more plantarwards on the metatarsal head without changing peak pressure or joint contact area.16 In the majority of patients with mild arthritis, cartilage damage is predominantly dorsal and the Moberg osteotomy may serve to offload contact pressure over diseased cartilage.
The Moberg osteotomy has been added to a standard cheilectomy with good results, even in patients with advanced radiographic disease. Thomas and Smith retrospectively reviewed 17 patients with grade I and II radiographic hallux rigidus at average 2.5-year follow-up and found a 99% satisfaction rate without any complications or repeat surgery.17 O’Malley retrospectively examined 81 patients with grade III radiographic hallux rigidus and reported 85% satisfaction after cheilectomy with a Moberg osteotomy.18 Four (4.9%) patients required conversion to an arthrodesis and no patients developed IP joint arthritis.
While the Moberg osteotomy has demonstrated good long-term results, conversion to arthrodesis after a Moberg osteotomy is potentially challenging. Because the proximal phalanx has been extended, the use of a contoured MTP arthrodesis plate may lead to excessive dorsiflexion of the MTP joint. For this reason, previous authors have recommended placement of lag screws to stabilise MTP alignment prior to placement of any dorsal plate.18
Keller resection arthroplasty
The Keller resection arthroplasty consists of removal of the base of the proximal phalanx to decompress the joint and increase dorsiflexion while sacrificing joint stability. While some reports have demonstrated effective pain relief, complications include weakness with toe-off, transfer metatarsalgia and cock-up deformity of the great toe.19,20 This profile makes this procedure a less desirable option for most patients.
Love et al prospectively reviewed 75 feet after Keller resection arthroplasty with an average follow-up of 31 months in low-demand patients over the age of 50 years.20 They reported pain relief in 91% of patients with a 77% satisfaction rate. A cock-up toe deformity was found in 41% of patients. Schneider et al retrospectively reviewed 87 cases after Keller resection arthroplasty at average follow-up of 23 years and found a mean American Orthopedic Foot and Ankle Society (AOFAS) score of 83.21 While 94% of patients would have their surgery again and the revision rate was 5%, due to the advancement in other treatments, this procedure is rarely performed.
Interpositional arthroplasty
Interpositional arthroplasty consists of combining a limited Keller resection arthroplasty with placement of a biological spacer into the joint. While retrospective studies using this technique demonstrate moderate results, with AOFAS scores of 71.6 to 93.6, complications included transfer metatarsalgia and hallux weakness.22,23 Modifications of technique consisted of decreased resection of the proximal phalanx, with preservation of the flexor hallucis brevis (FHB) insertion. This decreased instability, with Can Akgun et al reporting no cock-up deformities or hallux push-off weakness in 11 patients.23 Coughlin and Shurnas reviewed seven patients using a similar technique using gracilis tendon as a biological spacer at average 3.5-year follow-up, and reported decreased pain and improved function.24 However, 57% of patients had mild metatarsalgia.
Mackey et al further modified the Keller resection arthroplasty by suturing the dorsal capsule and extensor hallucis brevis (EHB) to the plantar plate instead of using a free interpositional graft.25 They prospectively compared ten patients using this modified technique with arthrodesis with average follow-up of 5.3 years, and found increased AOFAS score in the arthroplasty cohort but no differences in Foot and Ankle Ability Measure (FAAM) scores. The arthroplasty cohort had an average active range of motion of 30° and lower peak plantar pressures during walking compared with the arthrodesis group. These results are promising, although larger studies are needed.
MTP arthroplasty
MTP arthroplasty began historically with silastic implants and progressed to all-metal implants and, more recently, synthetic cartilage implants. Both first and second generation silastic implants have been found to be associated with high rates of osteolysis with implant subsidence, and immune reactions to the implants.26,27 While satisfaction rates ranged from 64% to 83%, failure of these implants presents a difficult challenge for conversion to arthrodesis due to the large associated loss of bone stock.
Metallic implants attempted to replicate total hip and total knee designs in the first MTP joint. They consisted of a cobalt-chrome metatarsal prosthesis with a polyeythene insert and a titanium proximal phalanx prosthesis. While patients reported moderate satisfaction at 78% and improvement in VAS pain scores, these implants have been similarly plagued by osteolysis and implant subsidence.28,29 Pulavarti reported a revision rate of 5.5% and implant subsidence rate of 33% at average 3.9-year follow-up in a prospective study of 32 patients.28 Gibson and Thomson reported on 63 patients in a randomised control trial comparing arthrodesis to arthroplasty and found that 49% of patients had radiographic loosening at one year with a 15% revision rate at two years.29
Ceramic implants have been evaluated as an alternative, with similarly poor results. Nagy et al retrospectively examined 31 second-generation ceramic MTP arthroplasties and reported 68% implant survival at nine years.30 Similarly, Dawson-Bowling reported a 26% re-operation rate at eight years with 52% of implants showing evidence of loosening in a retrospective study of 32 cases.31
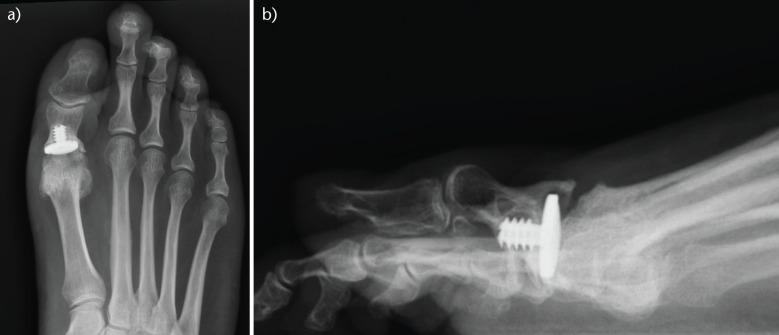
Hemi-arthroplasty involves a metallic implant of either the proximal phalanx or the metatarsal head. Townley et al reported on a retrospective series of 279 patients with eight-month to 33-year follow-up of a metal hemi-arthroplasty of the proximal phalanx.32 They found good to excellent results in 95% of patients. However, other studies could not replicate these results and reported poor outcomes. Konkel et al reported subsidence and radiolucencies in all ten patients retrospectively reviewed at 37 to 105 months after a proximal phalanx hemi-arthroplasty.33 Raikin et al retrospectively reviewed 21 metatarsal head hemi-arthroplasties at average 6.6-year follow-up and found a revision rate of 24% with decreased satisfaction, AOFAS scores and higher VAS pain scores compared with a cohort of 27 arthrodesis patients.34 While bone loss in conversion to arthrodesis is potentially decreased when using silastic and all metal implants, it is still a complicating factor that may require a bone block (Fig. 3).
Fig. 3.
Failed hemiarthroplasty. a and b) anteroposterior and lateral radiographs demonstrating subsidence with angular and plantar migration of the implant.
Newer generation metatarsal head resurfacing implants consist of a metatarsal head implant that attempts to recreate the contour of the articular surface with cobalt chrome. Kline and Hasselman reviewed a retrospective series of 26 patients treated with metallic resurfacing with average 2.3-year follow-up. They reported improvements in ROM, AOFAS and SF-36 scores with 100% satisfaction and a revision rate of 13% at five years. While these results are promising, conversion to arthrodesis similarly remains difficult due to decreased bone stock of the metatarsal head.
Recently, a synthetic cartilage implant has been introduced that shows promising results (Fig. 4). In a multicentre prospective randomised trial of 202 patients a 8-mm to 10-mm synthetic cartilage implant placed in the first MT head and compared with a first MTP arthrodesis at two-year follow-up. Baumhauer et al reported equivalent reduction in VAS pain scores and improvement in FAAM sports functional scores with the synthetic implant and first MTP arthrodesis.35 Synthetic cartilage patients had an average of 4° of improvement in dorsiflexion and a revision rate of 9.2% to arthrodesis. While longer survivorship analysis is planned, this implant offers encouraging results. Additionally, because the implant removes only 8 to10 mm of bone surrounding the metatarsal head, revision to arthrodesis is less challenging with minimal loss of length of the first metatarsal.
Fig. 4.
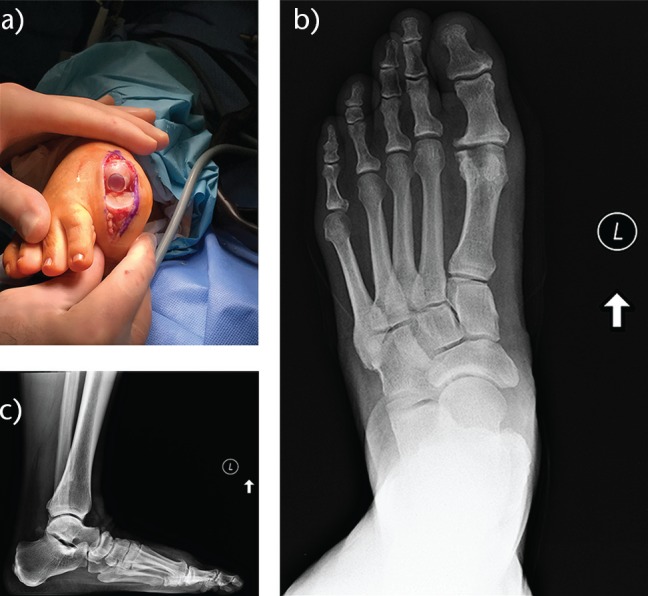
Synthetic cartilage replacement. a) Intra-operative example of a synthetic cartilage replacement with preservation of collateral ligaments (photograph courtesy of Dr Christopher Blundell), b and c) anterior, posterior and lateral radiograhs after synthetic cartilage replacement.
First MTP arthodesis
Arthodesis of the first MTP joint has demonstrated consistently good results in the literature and is the current ‘gold standard’ of treatment for patients with advanced arthritis (Hattrup and Johnson grade 3 or Coughlin and Shurnas grade 3 and 4). Arthrodesis is also the procedure of choice in patients with concomitant hallux valgus, hallux varus, rheumatoid arthritis and neuromuscular disorders. In patients with rheumatoid arthritis, the progressive nature of the disease with articular erosion and unreliable connective tissue stability limits relief from joint-sparing procedures. With hallux valgus, hallux varus or neuromuscular disorders, maintaining alignment with joint-sparing procedures is unpredictable and prone to failure.
Optimal position of the first MTP joint is with neutral rotation, 5° to 15° of valgus and 10° to 15° of dorsiflexion relative to the floor (20° to 25° relative to the first metatarsal). Valgus alignment should leave the great toe in a physiological position of slight valgus that is adjacent to the second toe. Dorsiflexion is determined intra-operatively by simulating weight-bearing with a flat plate (Fig. 5). The tip of the great toe should rest on the flat plate, but allow elevation by approximately one finger width (5 mm) above the flat plate (toe to floor distance).
Fig. 5.
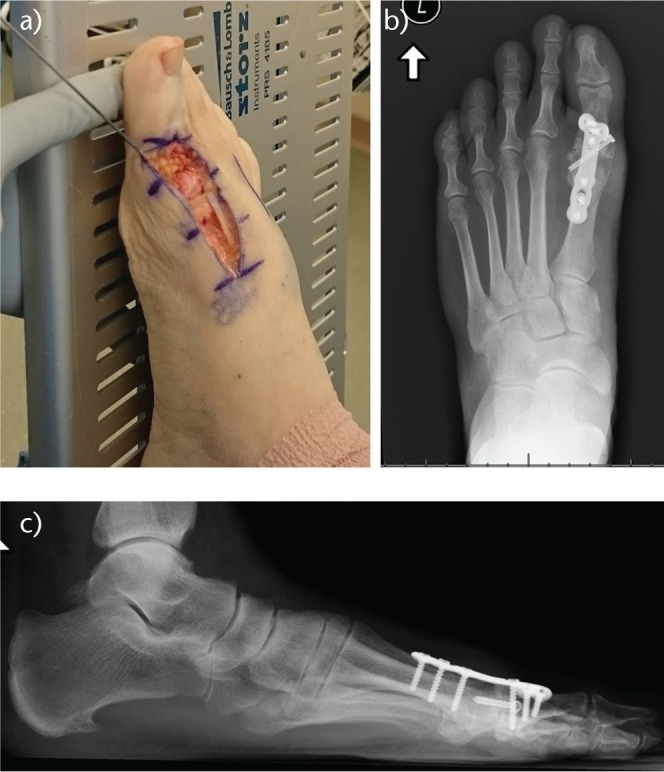
Metatarsophalangeal (MTP) arthrodesis. a) Clinical evaluation of MTP positioning with toe-to-floor distance with simulated weight-bearing on a flat plate. b and c) Radiographs demonstrating MTP fusion with a lag screw and dorsal plate.
There are multiple techniques for arthrodesis. The joint can be prepared with flat cuts or with conical reamers. Flat cuts are more technically demanding and have an increased risk of shortening the first ray. While conical reamers require specialised instrumentation, they allow more freedom to change first MTP alignment while maintaining bony contact. Fixation can include crossed lag screws or a lag screw with a dorsal plate (Fig. 5). Biomechanical testing has shown that a lag screw with a dorsal plate offers the most stable construct, although at the expense of increased cost of $604 versus $374 for crossed screws.36,37 While pre-contoured dorsal plates can offer a template to set first MTP dorsiflexion, correct positioning should be confirmed by examining toe-to-floor distance. Misplacement of these implants too proximally can lead to excessive dorsiflexion and radiographic analysis shows low correlation between the dorsal plate angle and toe-to-floor distance.38,39
Previous results for arthrodesis have been favourable. Goucher and Coughlin reported on 50 patients prospectively after first MTP arthrodesis using conical reamers and fixation with a lag screw and dorsal plate. Patients had a 96% satisfaction rate, 92% union rate and 4% revision rate at average 1.3-year follow-up.40 Doty et al used a similar technique in 49 patients with minimum one-year follow-up and reported 89% good to excellent results with 98% union rate.41 Bennett and Sabetta prospectively evaluated 200 patients treated with a dorsal plate with one-year follow-up and reported a 99% union rate and a 1% revision rate.42 Brodsky et al examined sports participation in 53 patients at average 3.7-year follow-up and found that patients were able to return to hiking 92% of the time, golf 80% of the time, tennis 75% of the time and jogging 75% of the time.43
Gait analysis by DeFrino et al after first MTP arthrodesis in nine patients demonstrated restoration of weight-bearing to the first ray with improved maximum force at toe-off, although step length and ankle plantarflexion at toe-off was still decreased compared to the non-operative limb.44 Brodsky et al further showed increased maximum ankle push-off power and single-limb support time in gait analysis of 23 patients.45
Numerous comparative studies have reported favourable results of arthrodesis compared with hemi-arthroplasty or arthroplasty. Raikin et al retrospectively compared arthrodesis with a metal hemi-arthroplasty implant with average 6.6-year follow-up.34 They found higher satisfaction, AOFAS scores and lower VAS pain scores in the arthrodesis group.34 All arthrodesis patients achieved fusion with a 7% rate of hardware removal while the hemi-arthroplasty group had a revision rate of 24%. Gibson and Thomson reported on 63 patients in a randomised control trial comparing arthrodesis with arthroplasty with two-year follow-up. They found that the arthrodesis group had greater improvements in pain with half the associated cost and no cases of revision surgery. In contrast, the arthroplasty group had a 15% revision rate due to component loosening.29
Conservative treatment should be attempted for hallux rigidus and is successful for approximately half of patients. Cheilectomy provides consistent results for patients with mild to moderate hallux rigidus. For patients with severe hallux rigidus, the ‘gold standard’ remains first MTP arthrodesis, where retrospective series as well as comparative studies have shown consistent success. Newer techniques of interpositional arthroplasty as well as new hemi-arthroplasty designs, including metal resurfacing and synthetic cartilage implants, offer potentially promising options for preservation of motion. In particular, synthetic cartilage implants have demonstrated similar pain relief and function to arthrodesis with preservation of motion while minimising challenges in conversion to arthrodesis. However, the long-term results of these options remain to be seen.
Footnotes
ICMJE Conflict of interest statement: JB has received financial support outside of this work in the form of Consultancy fees from Best Doctors, Cartiva Medical, DJO, Ferring Pharma, Nextremity Solutions, Wright Medical and Novostep.
Funding
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non- profit organisation with which one or more of the authors are associated.
References
- 1. Gould N, Schneider W, Ashikaga T. Epidemiological survey of foot problems in the continental United States: 1978-1979. Foot Ankle 1980;1:8-10. [DOI] [PubMed] [Google Scholar]
- 2. Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int 2003;24:731-743. [DOI] [PubMed] [Google Scholar]
- 3. Shereff MJ, Bejjani FJ, Kummer FJ. Kinematics of the first metatarsophalangeal joint. J Bone Joint Surg [Am] 1986;68-A:392-398. [PubMed] [Google Scholar]
- 4. Hattrup SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res 1988;226:182-191. [PubMed] [Google Scholar]
- 5. Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg [Am] 2003;85-A:2072-2088. [PubMed] [Google Scholar]
- 6. Pons M, Alvarez F, Solana J, Viladot R, Varela L. Sodium hyaluronate in the treatment of hallux rigidus. A single-blind, randomized study. Foot Ankle Int 2007;28:38-42. [DOI] [PubMed] [Google Scholar]
- 7. Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc 2002;92:102-108. [DOI] [PubMed] [Google Scholar]
- 8. DuVries H. Surgery of the Foot. St. Louis: Mosby Year Book, 1959:392-399.[[bibmisc]] [Google Scholar]
- 9. Heller WA, Brage ME. The effects of cheilectomy on dorsiflexion of the first metatarsophalangeal joint. Foot Ankle Int 1997;18:803-808. [DOI] [PubMed] [Google Scholar]
- 10. Nawoczenski DA, Ketz J, Baumhauer JF. Dynamic kinematic and plantar pressure changes following cheilectomy for hallux rigidus: a mid-term followup. Foot Ankle Int 2008;29:265-272. [DOI] [PubMed] [Google Scholar]
- 11. Easley ME, Davis WH, Anderson RB. Intermediate to long-term follow-up of medial-approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int 1999;20:147-152. [DOI] [PubMed] [Google Scholar]
- 12. Feltham GT, Hanks SE, Marcus RE. Age-based outcomes of cheilectomy for the treatment of hallux rigidus. Foot Ankle Int 2001;22:192-197. [DOI] [PubMed] [Google Scholar]
- 13. Vulcano E, Tracey JA, III, Myerson MS. Accurate measurement of first metatarsophalangeal range of motion in patients with hallux rigidus. Foot Ankle Int 2016;37:537-541. [DOI] [PubMed] [Google Scholar]
- 14. Smith SM, Coleman SC, Bacon SA, Polo FE, Brodsky JW. Improved ankle push-off power following cheilectomy for hallux rigidus: a prospective gait analysis study. Foot Ankle Int 2012;33:457-461. [DOI] [PubMed] [Google Scholar]
- 15. Bonney G, Macnab I. Hallux valgus and hallux rigidus; a critical survey of operative results. J Bone Joint Surg [Br] 1952;34-B:366-385. [DOI] [PubMed] [Google Scholar]
- 16. Kim PH, Chen X, Hillstrom H, et al. Moberg osteotomy shifts contact pressure plantarly in the first metatarsophalangeal joint in a biomechanical model. Foot Ankle Int 2016;37:96-101. [DOI] [PubMed] [Google Scholar]
- 17. Thomas PJ, Smith RW. Proximal phalanx osteotomy for the surgical treatment of hallux rigidus. Foot Ankle Int 1999;20:3-12. [DOI] [PubMed] [Google Scholar]
- 18. O’Malley MJ, Basran HS, Gu Y, Sayres S, Deland JT. Treatment of advanced stages of hallux rigidus with cheilectomy and phalangeal osteotomy. J Bone Joint Surg [Am] 2013;95-A:606-610. [DOI] [PubMed] [Google Scholar]
- 19. Beertema W, Draijer WF, van Os JJ, Pilot P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: long-term follow-up. J Foot Ankle Surg 2006;45:244-251. [DOI] [PubMed] [Google Scholar]
- 20. Love TR, Whynot AS, Farine I, et al. Keller arthroplasty: a prospective review. Foot Ankle 1987;8:46-54. [DOI] [PubMed] [Google Scholar]
- 21. Schneider W, Kadnar G, Kranzl A, Knahr K. Long-term results following Keller resection arthroplasty for hallux rigidus. Foot Ankle Int 2011;32:933-939. [DOI] [PubMed] [Google Scholar]
- 22. Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int 2001;22:462-470. [DOI] [PubMed] [Google Scholar]
- 23. Can Akgun R, Sahin O, Demirors H, Cengiz Tuncay I. Analysis of modified oblique Keller procedure for severe hallux rigidus. Foot Ankle Int 2008;29:1203-1208. [DOI] [PubMed] [Google Scholar]
- 24. Coughlin MJ, Shurnas PJ. Soft-tissue arthroplasty for hallux rigidus. Foot Ankle Int 2003;24:661-672. [DOI] [PubMed] [Google Scholar]
- 25. Mackey RB, Thomson AB, Kwon O, Mueller MJ, Johnson JE. The modified oblique keller capsular interpositional arthroplasty for hallux rigidus. J Bone Joint Surg [Am] 2010;92-A:1938-1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cracchiolo A, III, Weltmer JB, Jr, Lian G, Dalseth T, Dorey F. Arthroplasty of the first metatarsophalangeal joint with a double-stem silicone implant. Results in patients who have degenerative joint disease failure of previous operations, or rheumatoid arthritis. J Bone Joint Surg [Am] 1992;74-A:552-563. [PubMed] [Google Scholar]
- 27. Sebold EJ, Cracchiolo A., III Use of titanium grommets in silicone implant arthroplasty of the hallux metatarsophalangeal joint. Foot Ankle Int 1996;17:145-151. [DOI] [PubMed] [Google Scholar]
- 28. Pulavarti RS, McVie JL, Tulloch CJ. First metatarsophalangeal joint replacement using the bio-action great toe implant: intermediate results. Foot Ankle Int 2005;26:1033-1037. [DOI] [PubMed] [Google Scholar]
- 29. Gibson JN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int 2005;26:680-690. [DOI] [PubMed] [Google Scholar]
- 30. Nagy MT, Walker CR, Sirikonda SP. Second-generation ceramic first metatarsophalangeal joint replacement for hallux rigidus. Foot Ankle Int 2014;35:690-698. [DOI] [PubMed] [Google Scholar]
- 31. Dawson-Bowling S, Adimonye A, Cohen A, et al. MOJE ceramic metatarsophalangeal arthroplasty: disappointing clinical results at two to eight years. Foot Ankle Int 2012;33:560-564. [DOI] [PubMed] [Google Scholar]
- 32. Townley CO, Taranow WS. A metallic hemiarthroplasty resurfacing prosthesis for the hallux metatarsophalangeal joint. Foot Ankle Int 1994;15:575-580. [DOI] [PubMed] [Google Scholar]
- 33. Konkel KF, Menger AG. Mid-term results of titanium hemi-great toe implants. Foot Ankle Int 2006;27:922-929. [DOI] [PubMed] [Google Scholar]
- 34. Raikin SM, Ahmad J, Pour AE, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg [Am] 2007;89-A:1979-1985. [DOI] [PubMed] [Google Scholar]
- 35. Baumhauer JF, Singh D, Glazebrook M, et al. ; for and on behalf of the CARTIVA Motion Study Group. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int 2016;37:457-469. [DOI] [PubMed] [Google Scholar]
- 36. Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int 2003;24:332-337. [DOI] [PubMed] [Google Scholar]
- 37. Hyer CF, Glover JP, Berlet GC, Lee TH. Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg 2008;47:13-18. [DOI] [PubMed] [Google Scholar]
- 38. Lewis JT, Hanselman AE, Lalli TA, Daigre JL, Santrock RD. Effect of dorsal plate positioning on dorsiflexion angle in arthrodesis of the first metatarsophalangeal joint: a cadaveric study. Foot Ankle Int 2014;35:802-808. [DOI] [PubMed] [Google Scholar]
- 39. Leaseburg JT, DeOrio JK, Shapiro SA. Radiographic correlation of hallux MP fusion position and plate angle. Foot Ankle Int 2009;30:873-876. [DOI] [PubMed] [Google Scholar]
- 40. Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int 2006;27:869-876. [DOI] [PubMed] [Google Scholar]
- 41. Doty J, Coughlin M, Hirose C, Kemp T. Hallux metatarsophalangeal joint arthrodesis with a hybrid locking plate and a plantar neutralization screw: a prospective study. Foot Ankle Int 2013;34:1535-1540. [DOI] [PubMed] [Google Scholar]
- 42. Bennett GL, Sabetta J. First metatarsalphalangeal joint arthrodesis: evaluation of plate and screw fixation. Foot Ankle Int 2009;30:752-757. [DOI] [PubMed] [Google Scholar]
- 43. Brodsky JW, Passmore RN, Pollo FE, Shabat S. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot Ankle Int 2005;26:140-146. [DOI] [PubMed] [Google Scholar]
- 44. DeFrino PF, Brodsky JW, Pollo FE, Crenshaw SJ, Beischer AD. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int 2002;23:496-502. [DOI] [PubMed] [Google Scholar]
- 45. Brodsky JW, Baum BS, Pollo FE, Mehta H. Prospective gait analysis in patients with first metatarsophalangeal joint arthrodesis for hallux rigidus. Foot Ankle Int 2007;28:162-165. [DOI] [PubMed] [Google Scholar]