Abstract
Until the late 1980s, proximal interphalangeal (PIP) joint reconstruction had been almost exclusively performed by the use of monobloc silicone spacers and associated with acceptable to good clinical outcomes.
More recently, new materials such as metal-on-polyethylene and pyrocarbon implants were proposed, associated with good short-term and mid-term results.
Pyrocarbon is a biologically inert and biocompatible material with a low tendency to wear. PIP pyrolytic implants are characterised by a graphite core, visible on radiographs and covered by a radiolucent outer layer of pyrocarbon.
New surgical techniques and better patient selection with tailored rehabilitative protocols, associated with the knowledge arising from the long-term experience with pyrocarbon implants, has demonstrated noteworthy clinical outcomes over the years, as demonstrated by recent studies.
Cite this article: EFORT Open Rev 2017;2:21–27. DOI: 10.1302/2058-5241.2.160041
Keywords: Proximal interphalangeal joint, finger joints replacement, pyrocarbon, pyrolitic carbon implants, Rheumatoid arthritis, Osteoarthritis, hand, fingers
Introduction
Until the late 1980s, finger joint prosthetic reconstruction had been almost exclusively performed by using monobloc silicone spacers as developed by Swanson et al more than 20 years previously.1 Such implants are not fixed to bone and prosthetic stems are free to glide into the medullary canal during flexion and extension. The so-called ‘piston effect’ allows the distribution of forces over a broader section and permits the flexible hinge to find a better position with respect to the axis of rotation of the joint.1 Outcomes were reasonably good, particularly in the metacarpophalangeal (MP) joints of patients affected by rheumatoid arthritis (RA) and degenerative osteoarthritis (OA). The experience in the reconstruction of proximal interphalangeal (PIP) joints showed variable results and has been reported as less satisfactory.2 Silicone spacers did not offer enough lateral stability, therefore showing high rates of angular instability and secondary wear, leading to stem breakage at the junction with the central body of the spacer. Moreover, in such cases silastic debris may induce a synovial inflammatory reaction leading to the well-known ‘silicone-related synovitis’. Thus, the need for alternative biomaterials and prosthetic designs for PIP articular reconstruction led to the development of new devices. Metal-on-polyethylene implants, cementless or cemented prostheses, total or hemi-arthroplasties, as well as pyrocarbon PIP joint prostheses were proposed with satisfactory results.3-10 The latter are characterised by a biologically inert and biocompatible material with a low tendency to wear. Such implants consist of anatomic bicondylar semi-constrained press-fit components made of a graphite core, visible on radiographs, covered by a radiolucent outer layer of pyrocarbon. A minimal bone resection is required in respect of the anatomical centre of rotation of the joint; collateral ligaments must be preserved or reconstructed. Initial experiences with pyrocarbon implants showed encouraging outcomes.5-11 At mid- and long-term follow-up, among satisfactory reports, early failures or component rupture were recorded.12-19 Post-operative satisfaction and functional ability have been addressed as the clinical parameters associated with variable results, given the generally higher pre-operative patients’ expectations and the actual improvement of range of movement (ROM) after surgery.6-8,14,17,19,20 From the surgeons’ perspective, the significant percentage of additional procedures or revision surgery (reported as up to 25% and 15%, respectively) represent the concern regarding the use of such implants.2,6-8,16,17,20
Outcomes to date
PIP joint replacements have been performed for many decades with silicone implants with substantial acceptable to good outcomes.1 However, such types of surgery have been associated with less satisfactory results compared with MP joint replacement surgery due to several issues, often leading to early revisions. Specifically, the main causes of failure compared with MP joint arthroplasty were related to the more intense mechanical loads and angulatory forces acting on PIP joints during work and daily life activities, and the peculiar torque stress and strain at the bone/implant interfaces.20 Pyrocarbon was introduced in experimental studies in the 1970s and in clinical practice in orthopaedics, vertebral and hand surgery in the 1980s. After the first release of a small series,5-11 several mid to long-term follow-up studies related to PIP joint arthroplasties have been reported more recently.12-21 Despite a substantially good survivorship, clinical outcomes to date are variable and differently evaluated. The main points of debate are related to the surgical technique, radiological analysis, post-operative rehabilitation and assessment of clinical results.
Surgical technique
PIP joint surgery may be performed by a dorsal, lateral or volar approach. A dorsal access is most frequently used, and either a longitudinal extensor tendon-splitting or a V-shaped tenotomy may be done preserving the central band insertion.22 A dorsal midline incision is made, through the extensor tendon from the P1 to the central slip insertion which is detached from the base of the middle phalanx and the soft-tissue is reflected by sharp dissection preserving collateral ligaments, the latter as a sleeve up to the anterior third attachment of the collateral ligament. Lifting a distally based extensor tendon flap of the common extensor allows a dislocation of the joint and leaves the central slip insertion intact at the base of the middle phalanx. In the first case, the central slip may be re-attached through bone sutures to the base of the middle phalanx. Alternatively, just a continuous suture is used to close the split in the extensor tendon without re-attachment of the central slip to bone.
The dorsal capsule is then elevated and the collateral ligaments protected. Bony resections are then performed and the medullary canals broached to allow the positioning of the components.
Some authors prefer a lateral or volar approach because tendon continuity is better preserved and an earlier rehabilitation may be performed.2,6-8,19,21,23
The lateral approach finds its main advantage in the preservation of extensor and flexor tendons. The skin incision is made longitudinally on the lateral aspect of the proximal phalanx and is then curved dorsally over the middle phalanx. The extensor apparatus is elevated after cutting the oblique and transverse fibres of the retinacular ligament; the tendon is then laterally dislocated preserving the bony insertion of its central band. The volar neurovascular structures are protected by the soft tissues. The ligament complex is elevated as a single triangular flap and proximally reflected, performing a V-shaped incision whose longitudinal branch corresponds to the dorsal margin of the collateral ligament, whereas the anterior-oblique branch separates the collateral and accessory collateral from the phalango-glenoidal ligament. The proximal insertion of the volar plate and the dorsal capsule are then partially released in order to laterally dislocate the joint, having the contralateral collateral ligament complex as a pivot point. Bone resections and medullary canal reaming are performed and the pyrocarbon components are implanted. The joint is reduced and the collateral ligament is resutured to the intact phalango-glenoidal component. The retinacular ligament is sutured to the lateral band in order to complete the anatomical reconstruction of the extensor apparatus (Figs 1 to 4).7
Fig. 1.
Proximal interphalangeal osteoarthritis of the ring finger in a 60-year-old patient. On the radiographs note the reduced joint space and major osteophytosis.
Fig. 4.
Radiograph at three-year follow-up. Note the dense bony line surrounding the prosthetic stems; the thin corticalisation process is to be considered as a typical sign of implant stability (the inner transparent line corresponds to the radiolucent pyrocarbon stem coating) (same case as in Fig. 1).
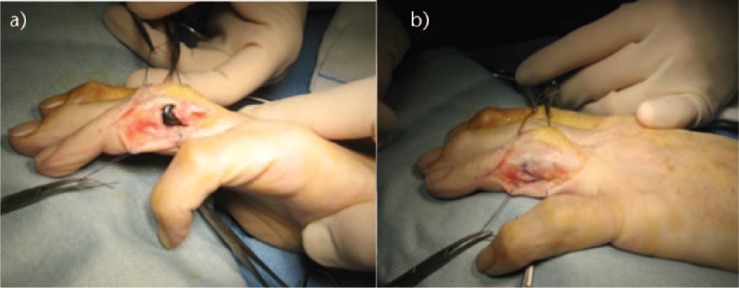
Fig. 2.
The pyrocarbon proximal interphalangeal components were implanted using a lateral surgical approach (see text). a) The ulnar collateral ligament was elevated and then b) re-sutured to the phalango-glenoidal fibres following the implant positioning (same case as in Fig. 1).
Fig. 3.

Range of flexion at three years (same case as in Fig. 1).
In the volar approach, the palmar skin is incised in a zigzag fashion (Bruner incision). The flexor tendon sheath is exposed, released at the A2 pulley and pulled distally, detaching the flexor tendon complex from P1 and P2 together with the volar plate. The volar insertion of the collateral ligament is also sectioned.12,24 The PIP joint is dislocated and the articular surfaces are resected from the palmar side. P1 condyles are removed by a 45º-angled cut; the resection is then completed by a vertical cut of the remaining dorsal rim. The P2 base is most commonly prepared by simply smoothing the articular surface and broaching the P2 medullary canal in order to obtain an even margin, which supports the distal component. The insertion of the extensor tendon central slip is preserved. At the end of the procedure, the flexor tendon sheath is brought back over the flexor tendon and resutured in its original anatomical position. The adequate sizing of the components and the axial alignment of the stems have to be carefully assessed during surgery in order to obtain a stable construct. Malalignment and inadequate cortical support of a component are considered causes of early failures and reactive pathological remodelling of the periprosthetic phalangeal bones, leading to implant subsidence.
Radiograph findings
Radiograph findings following a pyrocarbon arthroplasty show peculiar aspects which are useful to follow the evolution and survivorship of such implants. In fact, the development of a bone apposition process surrounding the bone-pyrocarbon interface, as a symmetrical rim of lucency, may be observed on sequential radiographs up to two years after surgery.2,6-8,13,17,18 It consists of a high-density bony line surrounding the implant stem and sealing the medullary canal at the level of the tip of the stem.7,18,19 This process generally intensifies as post-operative mobility is allowed. No further process of bone remodelling is reported once the dense bony line around stems become evident on radiographs. This is considered as consistent with implant stabilisation.13,17,21,25 Note that findings related to every type of implant, such as tilting, migration and loosening, are also evaluated in the radiological follow-up of such implants.8 These aspects do not show any characteristic feature related to the material or the shape of pyrocarbon PIP implants.
Rehabilitation
Rehabilitation protocols are strictly correlated with the surgical approach. In cases with a dorsal approach, mobilisation is not started before the fourth post-operative day. A dynamic PIP joint extension splint is usually worn during the day and gradually adjusted to allow 60° of flexion within four weeks post-operatively. Splinting is then maintained up to six weeks. On the other hand, a lateral or volar approach allows an earlier and less restricted mobilisation, also because the extensor tendons are preserved during surgery. Active joint mobility is permitted wearing a digital dorsal custom-made static splint that limits PIP joint extension to 5° and prevents any lateral deviation but does not prevent DIP flexion and extension. Complete PIP extension is to be avoided for the first two weeks in order to allow the healing of the articular ligament complex. A palmar static splint is worn at night, keeping MP and PIP joints flexed in a resting position. Four weeks after surgery, activities of daily living are permitted, wearing a protective ‘buddy-taping’ to the adjacent finger for two months. If necessary, an oval eight splint can also be used to prevent PIP joint hyperextension. The supervision of an experienced hand physiotherapist is highly recommended for the first three months after surgery.
Assessment of results
Clinical outcomes
As mentioned, several studies have been published recently with consistent numbers of patients and extended follow-up periods.2,9,16,17,19 However, no uniformity may be found in the assessment of clinical outcomes. The following parameters are evaluated: patient overall satisfaction, pain relief, grip and key-pinch strength, ROM, quick-DASH and Michigan Hand Outcomes Questionnaire score. These data are summarised in Table 1. Osteoarthritis, post-traumatic arthritis and in some series RA and psoriatic arthritis have been the main causes of disease of PIP joints. Considering degenerative and inflammatory conditions together may also represent a limit of such series, particularly since complications are reported with a significant higher frequency in patients affected by an inflammatory joint disease.2,9 The majority of the series include multidigital arthroplasties. The overall patient satisfaction and relief from pain have been mostly reported as good. Most authors are continuing to use pyrocarbon implants in such type of surgery,2,6-8,10,13,14,16,17 while few showed no intention of continuing to use such devices.7,14,18
Table 1.
Comparison of the clinical outcomes reported in a series of recent studies on proximal interphalangeal pyrolytic carbon implants
| Patient satisfaction | Pain (pre-op) | Pain (post-op) | Grip* (pre-op) | Grip* (post-op) | Pinch* | ROM† (pre-op) | ROM† (post-op) | DASH (pre-op) | DASH (post-op) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Bravo (2007) 5 | 77% | 6 (VAS) | 1 (VAS) | 19 (3-36) | 24 (4-41) | 4.4 (2-10) | 40° (0°-60°) | 47° (10°-0°) | ||
| Meier (2007)6 | 50% | 0-3 (VAS) | 50° | |||||||
| Sweets (2011)8 | 3.4 (Likert scale) | 3 (VAS) | 57° (15°-95°) |
31° (0°-100°) | ||||||
| McGuire (2011)16 | 4.2 (Likert scale) | Excellent pain relief |
30° | 66° | ||||||
| Ceruso (2011)7 | 9.2 (1-10 scale) | 7.3 (VAS) | 0.8 (VAS) | 25 | 6.9 | 14.5° AROM | 50° AROM | 43 | 16 | |
| Watts (2012)9 | 2 (PEMq) | 0 (VAS) | 96% of other side | 25° (0°-85°) |
30° (0°-90°) |
22 (10-48) |
||||
| Ono (2012)13 | 11±7 | 12.4±13.5 | 4.8 | 43°±6 | 51°±24 | |||||
| Heers (2012)15 | 100% | 0-5 (VAS) | 46° | 58° | ||||||
| Daecke (2012)26 | 8.1±1.8 (VAS max) |
2.7±2.9 | 20.3 | 26.0 | 61°± 23 (max) | 68 | 48 | |||
| Mashhadi (201210) | 100% | 0.9 (VAS) | 15 | 7.7 | 36° AROM 37° PROM |
46° AROM 58° PROM |
||||
| Hutt (2012)14 | 4.2 rest 8.6 act. |
0 rest. 0 act. |
40° | 45° (0°-90°) | ||||||
| Tägil (2013)17 | 5.9 (COPM°) | 4 rest 6 act. |
0 rest 1 act. |
19 | 25 | 53° | 54° | 40 | 25 | |
| Reissner (2014)21 | 7.6 (VAS) | 0.7 (VAS) | 21 | 17 | 36° | 29° | 21 | |||
| Pettersson (2015)19 | 5 (COPM°) | 3 (VAS) | 0.6 (VAS) | 16 | 20 | - | 39° | 41° | 42 | 31 |
expressed in kg
Canadian Occupational Performance Measure (COPM)
Radiological outcomes
Radiological findings have been evaluated according to different scoring systems: Sweet and Stern Grading system,8 Nelson Hospital scoring system14 and Herren systems have been used.12 Radiolucent lines, subsidence and settling of the implant have been evaluated periodically, corresponding to specific radiological patterns such as the following: no variations, early changes followed by unmodified radiograph findings on further controls (implant settlement in a stable position) (Fig. 5),13,16 implant tilting, and subsidence and/or loosening (Fig. 6).8 It should be noted that radiographic changes were observed during the first 18 to 24 months post-operatively.6-8,17,21 Furthermore, a certain degree of implant settlement or tilting were not always related to symptomatic conditions.9,16
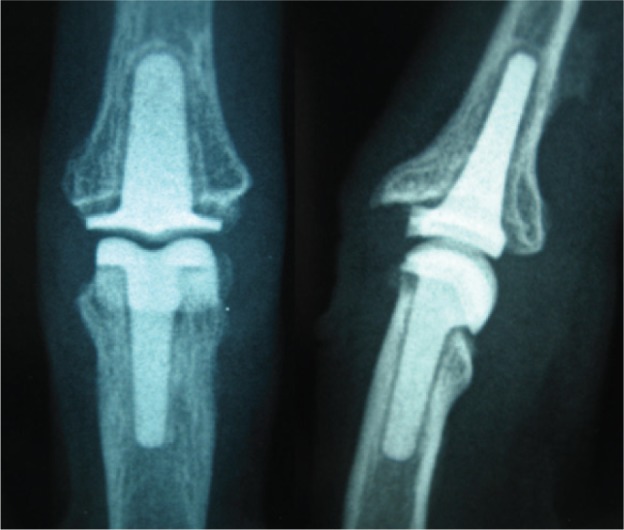
Fig. 5.
Radiographs of a 58-year-old patient at a) one year and b) eight years follow-up: the implant is stable and no change of its position are observed. b) Note the symmetric radiolucency surrounding the distal stem with a sclerotic rim on the long-term control radiographs.
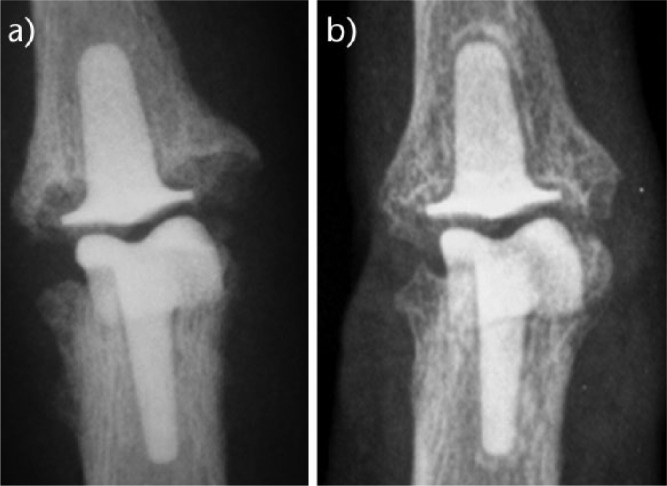
Fig. 6.

Radiological signs of subsidence of the P2 component two years after surgery, due to inadequate sizing of the implant.
Additional procedures and implant revisions are summarised in Table 2. Implant failures requiring either conversion to a Swanson spacer or PIP joint fusion were in the range of 0% to 16%. A single component substitution was rarely reported (0.5%).7,16
Table 2.
Summary of the complications and additional procedures reported in a series of recent studies on proximal interphalangeal pyrolytic implants
| Cases (n) | Additional surgery | Revision arthroplasty (total failures) | |
|---|---|---|---|
| Meier (2007)6 | 24 implants | 3 arthrodesis | 1 infection 2 dislocations Asymptomatic squeaking (87%) |
| Sweets (2011)8 | 31 implants | 1 excision of exostosis | 4 arthrodeses 1 silicone implant |
| McGuire (2011)16 | 57 implants | 6 arthrolyses/tenolyses 7 FDS tenodeses |
5 (9%) revisions 4 Silicone implants 1 larger proximal component |
| Ceruso (2011)7 | 40 implants | 6 tenolyses | 1 arthrodesis 3 silicone implants 1 larger proximal component |
| Pritsch and Rizzo (2011)2 | 203 on pyrocarbon (on 294 total implants) |
50 (24.6%) 25 arthrolyses/tenolyses 9 ligament/joint stabilisation 8 FDS hemitenodeses 4 bone spur removals 1 exposed implant 1 triggering 2 extensor tendon repair |
29 revisions (14.2% ) 18 revision 12 larger 4 SRA (+/- cement) 2 silicone 7 arthrodeses 4 amputation |
| Watts (2012)9 | 97 implants | 22 (23%) 9 arthrolyses/tenolyses 3 percutaneous accessory collateral release 4 FDS tenodeses 1 central slip advancement 1 collateral ligament reconstruction 1 retained suture |
13 (13%) revision 4 arthrodeses 9 silicone implants |
| Ono (2012)13 | 21 implants | None | None |
| Heers (2012)15 | 13 implants | 2 tenolyses | None |
| Daecke (2012)26 | 18 implants | 7 revision (39%) Aseptic loosening, restricted ROM or dislocation |
|
| Mashhadi (2012)10 | 24 implants | 3 arthrolyses/tenolyses | None |
| Hutt (2012)14 | 15 implants | 2 tenolyses | 1 amputation |
| Tägil (2013)17 | 89 implants | 4 arthrolyses/tenolyses 2 Littler tenoplasty |
4 arthrodeses (1 after silicone implant) 2 smaller components |
| Reissner (2014)21 | 15 implants | None | None |
| Pettersson (2015)19 | 42 implants | None | 3 arthrodeses 1 conversion to silicone implant |
Complications
Complications in PIP surgery with pyrolytic carbon implants have been reported in the literature with rates in the range of 0% to almost 25%. On the other hand, revision surgery was necessary from 0% to 39% of the series.6-10,13,15-17,19,21,26 One of the most common post-operative clinical settings not requiring revision is squeaking. In such conditions, an articular ‘noise’ may be heard through the ROM of the finger, which in most cases spontaneously resolves over time. In several cases, the squeaking may be related to malalignment of the components.6 Other complications needing further surgery or even revision with silicone implants may occur or, in the most severe cases, a joint fusion. Less common problems are the need for surgery of extensor tendons in cases of dorsal approaches (surgical repair, tenolysis, advancement or tenodesis), incomplete osteophyte removal, dislocation, swan-neck deformity and infection.
Conclusions
PIP joint prosthetic replacement has characteristic aspects related to the functional substantial independency of each of the joints. This exposes each single PIP to lateral, dorso-volar and torque stresses in any activity of daily life that a hand performs continuously. Moreover, it is generally associated with less good outcomes and higher rates of complications and revisions with respect to other more proximal joint arthroplasties of the hand. Soft tissue management is more technically demanding, requiring joint reconstruction which is the main feature of such surgery. Technical difficulties are presented by the small dimensions and the thin cortices of the phalanges, which make canal reaming particularly difficult, and the scarce bony vascularisation related to the absence of muscular coverage can lead to problems of healing. Pyrocarbon implants have to be considered reasonable options in PIP joint reconstructions given their specific characteristics, such as the bicondylar semi-constrained anatomical design, the need for limited bone resections, a press-fit fixation, the high biocompatibility and the low tendency to wear.
Degenerative OA and post-traumatic conditions may be considered the best indication for such implants as several series in the literature have shown, but silicone implants or fusion still represent the ‘gold standard’ for the treatment of the PIP joint in inflammatory arthritis. On the other hand, the surgical technique is of paramount importance and the knowledge of the different approaches is useful to better address the specific PIP joint deformities. The preservation of the extensor apparatus, feasible either by a lateral or a volar approach, is another key factor in order to obtain anatomical reconstruction and more rapid post-operative rehabilitation protocols. After surgery, the use of custom-made splints and close supervision by a hand physiotherapist are strongly recommended. Intra-operatively, two main goals should be achieved: the adequate sizing of the components and the axial alignment of the stems. PIP joint stability and a functional ROM should in any case be obtained at the end of the procedure.
Footnotes
ICMJE Conflict of interest statement: None
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. 5. The author or authors choose not to respond to the above statements.
References
- 1. Swanson AB, Swanson GG, De Heer DH. Small Joint implant arthroplasty: 38 years of research and experience. In: Simmen BR, Allieu Y, Lluch A, Stanley J, eds. Hand arthroplasty.London: Martin Dunitz; 2000:69-81. [Google Scholar]
- 2. Pritsch T, Rizzo M. Reoperations following proximal interphalangeal joint nonconstrained arthroplasties. J Hand Surg Am 2011;36:1460-1466. [DOI] [PubMed] [Google Scholar]
- 3. Uchiyama S, Cooney WP, III, Linscheid RL, Niebur G, An KN. Kinematics of the proximal interphalangeal joint of the finger after surface replacement. J Hand Surg Am 2000;25:305-312. [DOI] [PubMed] [Google Scholar]
- 4. Ampofo C, Aerni M. Experience with the SRTM-PIP prosthesis as joint replacement: a retrospective overview with a follow-up of 2.4 years. Handchir Mikrochir Plast Chir 2011;43:167-174. [DOI] [PubMed] [Google Scholar]
- 5. Bravo CJ, Rizzo M, Hormel KB, Beckenbaugh RD. Pyrolytic carbon proximal interphalangeal joint arthroplasty: results with minimum two-year follow-up evaluation. J Hand Surg Am 2007;32:1-11. [DOI] [PubMed] [Google Scholar]
- 6. Meier R, Schulz M, Krimmer H, Stütz N, Lanz U. Proximal interphalangeal joint replacement with pyrolytic carbon prostheses. Oper Orthop Traumatol 2007;19:1-15. [DOI] [PubMed] [Google Scholar]
- 7. Ceruso M, Pfanner S, Guidi G. PIP joint replacement with a Pyrolitic Carbon Implant. In: Røkkum M, ed. Wrist and Hand Joint replacement. FESSH Instructional Course Book; 2011:236-243. [Google Scholar]
- 8. Sweets TM, Stern PJ. Pyrolytic carbon resurfacing arthroplasty for osteoarthritis of the proximal interphalangeal joint of the finger. J Bone Joint Surg [Am] 2011;93-A:1417-1425. [DOI] [PubMed] [Google Scholar]
- 9. Watts AC, Hearnden AJ, Trail IA, et al. Pyrocarbon proximal interphalangeal joint arthroplasty: minimum two-year follow-up. J Hand Surg Am 2012;37:882-888. [DOI] [PubMed] [Google Scholar]
- 10. Mashhadi SA, Chandrasekharan L, Pickford MA. Pyrolytic carbon arthroplasty for the proximal interphalangeal joint: results after minimum 3 years of follow-up. J Hand Surg Eur Vol 2012;37:501-505. [DOI] [PubMed] [Google Scholar]
- 11. Tuttle HG, Stern PJ. Pyrolytic carbon proximal interphalangeal joint resurfacing arthroplasty. J Hand Surg Am 2006;31:930-939. [DOI] [PubMed] [Google Scholar]
- 12. Herren DB, Schindele S, Goldhahn J, Simmen BR. Problematic bone fixation with pyrocarbon implants in proximal interphalangeal joint replacement: short-term results. J Hand Surg Br 2006;31:643-651. [DOI] [PubMed] [Google Scholar]
- 13. Ono S, Shauver MJ, Chang KW, Chung KC. Outcomes of pyrolytic carbon arthroplasty for the proximal interphalangeal joint at 44 months’ mean follow-up. Plast Reconstr Surg 2012;129:1139-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hutt JR, Gilleard O, Hacker A, Citron N. Medium-term outcomes of pyrocarbon arthroplasty of the proximal interphalangeal joint. J Hand Surg Eur Vol 2012;37:497-500. [DOI] [PubMed] [Google Scholar]
- 15. Heers G, Springorum HR, Baier C, et al. Proximal interphalangeal joint replacement with an unconstrained pyrocarbon prosthesis (Ascension(R)): a long-term follow-up. J Hand Surg Eur Vol 2013;38:680-685. [DOI] [PubMed] [Google Scholar]
- 16. McGuire DT, White CD, Carter SL, Solomons MW. Pyrocarbon proximal interphalangeal joint arthroplasty: outcomes of a cohort study. J Hand Surg Eur Vol 2012;37:490-496. [DOI] [PubMed] [Google Scholar]
- 17. Tägil M, Geijer M, Abramo A, Kopylov P. Ten years’ experience with a pyrocarbon prosthesis replacing the proximal interphalangeal joint. A prospective clinical and radiographic follow-up. J Hand Surg Eur Vol 2014;39:587-595. [DOI] [PubMed] [Google Scholar]
- 18. Paulos RG, Sousa E, Silva R, Le Viet D, Le Viet D. Fracture of a pyrolytic carbon proximal interphalangeal prosthesis: clinical case. Chir Main 2014;33:55-58. [DOI] [PubMed] [Google Scholar]
- 19. Pettersson K, Amilon A, Rizzo M. Pyrolytic carbon hemiarthroplasty in the management of proximal interphalangeal joint arthritis. J Hand Surg Am 2015;40:462-468. [DOI] [PubMed] [Google Scholar]
- 20. Shin AS, Amadio PC. Stiff finger joints (Chapter 11). In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW. (eds). Green’s Operative Hand Surgery. Volume 1. Elsevier-Churchill Livingstone, 2005:417-460. [Google Scholar]
- 21. Reissner L, Schindele S, Hensler S, Marks M, Herren DB. Ten year follow-up of pyrocarbon implants for proximal interphalangeal joint replacement. J Hand Surg Eur Vol 2014;39:582-586. [DOI] [PubMed] [Google Scholar]
- 22. Chamay A. A distally based dorsal and triangular tendinous flap for direct access to the proximal interphalangeal joint. Ann Chir Main 1988;7:179-183. [DOI] [PubMed] [Google Scholar]
- 23. Merle M, Villani F, Lallemand B, Vaienti L. Proximal interphalangeal joint arthroplasty with silicone implants (NeuFlex) by a lateral approach: a series of 51 cases. J Hand Surg Eur Vol 2012;37:50-55. [DOI] [PubMed] [Google Scholar]
- 24. Simmen BR. Der palamre Zugang zur Arthroplastik des proximalen Interphalangeal-Finger-Gelenkes. Operative techniken Ortopadie und Traumatologie 1993;5:112-123. [Google Scholar]
- 25. Petscavage JM, Ha AS, Chew FS. Arthroplasty of the hand: radiographic outcomes of pyrolytic carbon proximal interphalangeal and metacarpophalangeal joint replacements. AJR Am J Roentgenol 2011;197:1177-1181. [DOI] [PubMed] [Google Scholar]
- 26. Daecke W, Kaszap B, Martini AK, et al. A prospective, randomized comparison of 3 types of proximal interphalangeal joint arthroplasty. J Hand Surg Am 2012;37:1770-1779. [DOI] [PubMed] [Google Scholar]