Abstract
Background
Vulnerable preterm infants experience repeated and prolonged pain/stress stimulation during a critical period in their development while in the neonatal intensive care unit (NICU). The contribution of cumulative pain/stressors to altered neurodevelopment remains unclear. The study purpose was to investigate the impact of early life painful/stressful experiences on neurobehavioral outcomes of preterm infants in the NICU.
Methods
A prospective exploratory study was conducted with fifty preterm infants (28 0/7 – 32 6/7 weeks gestational age) recruited at birth and followed for four weeks. Cumulative pain/stressors (NICU Infant Stressor Scale) were measured daily and neurodevelopmental outcomes (NICU Network Neurobehavioral Scale) were examined at 36-37 weeks post-menstrual age. Data analyses were conducted on the distribution of pain/stressors experienced over time and the linkages among pain/stressors and neurobehavioral outcomes.
Results
Preterm infants experienced a high degree of pain/stressors in the NICU, both in numbers of daily acute events (22.97±2.30 procedures) and cumulative times of chronic/stressful exposure (42.59±15.02 hours). Both acute and chronic pain/stress experienced during early life significantly contributed to the neurobehavioral outcomes, particularly in stress/abstinence (p < 0.05) and habituation responses (p < 0.01), meanwhile, direct breastfeeding and skin-to-skin holding were also significantly associated with habituation (p < 0.01 – 0.05).
Conclusion
Understanding mechanisms by which early life experience alters neurodevelopment will assist clinicians in developing targeted neuroprotective strategies and individualized interventions to improve infant developmental outcomes.
Keywords: Pain, Stress, Neurobehavioral Outcomes, Preterm Infants, Neonatal Intensive Care
Introduction
The United States ranks among the highest in the world for the number of preterm births, with approximately 10% of infants born before 37 weeks of gestation in 2014.1 Even though this rate was the lowest recorded for overall preterm births since 2007, the rates for very preterm (< 32 weeks of gestation), low birth weight (< 2500 grams) and very low birthweight (< 1,500 grams) births continue to be essentially unchanged and are still unacceptably high.1 Advances in neonatal care have contributed to an increase in survival, especially among these high-risk preterm infants.2 However, stressful early life experiences in the neonatal intensive care unit (NICU) have continued to be an inherent part of high-technology lifesaving care for these infants. Immature infants living outside the protective intrauterine environment are necessarily subjected to intensive care treatment which often involves numerous painful or stressful diagnostic and therapeutic procedures, uncomfortable interventions, compounded by infant isolation and parental separation. With substantial gains in survival from the NICU, there is increased focus on decreasing neurological morbidity and long-term adverse outcomes related to the immature neuro-immune systems and early life stress.3 The contribution of cumulative pain/stressors experienced in the NICU to altered neurobehavioral outcomes in preterm infants remains unclear and needs further investigation.
The course and length of the NICU experience has been found to be one of the most crucial factors influencing preterm infant neurodevelopmental and health outcomes; particularly because this is a modifiable factor that occurs during a critical period of neurodevelopment.4,5 Cumulative early life painful and stressful experiences, including repeated painful procedures, during critical neurodevelopmental windows is one of the major unsolved issues of neonatal intensive care. We know that early life stressors, especially in the fetal and neonatal period are associated with substantial long-term neurological morbidity and may even contribute to chronic metabolic conditions, such as diabetes and obesity.6 In one recent meta-analysis, it was reported that 39.4% of NICU survivors had at least one neurodevelopmental deficit.3 Furthermore, the estimated cost of prematurity and its neurodevelopmental consequences is at least $26.2 billion per year, not including the added emotional and time burden for families and society.7
The origins of altered neurobehavioral development induced by cumulative infant pain/stress are often insidious and the mechanisms remain largely unclear. Few studies have been conducted to measure the association of NICU pain/stress with neurobehavioral status in early life. Even though their brains are still in a critical period of development it is evident that preterm infants possess both anatomical and neurochemical capabilities of pain perception. Knowing that their tactile perception threshold is lower and that their descending inhibitory pathways are immature, they are even more sensitive to repeated and prolonged pain and stress stimulation during this vulnerable period.8 A recent study showed that greater numbers of painful procedures were directly correlated to subsequent decreases in head growth and brain function in very preterm infants; and suggested that repeated pain during a vulnerable period may activate a cascade of stress signaling that affects later growth and development.9 Quantification of cumulative infant stress has been challenging but a validated instrument, the NICU Infant Stressor Scale (NISS) has been successfully utilized to provide a cumulative measure of infant's exposure to both acute stressful procedures (numbers) and chronic stressful exposure (hours).10
Despite advances in care of preterm infants, it remains extremely difficult to predict adverse neurodevelopmental outcomes.11 There has been a surge in the literature over the past few years, addressing the comprehensive components and complexities of infant neurobehavioral assessments, especially with the introduction of the Neonatal Intensive Care Unit Network Neurobehavioral Scale (NNNS). The NNNS was designed to measure the infant's bio-behavioral organizations as a valid biomarker for detecting at-risk infants, with the ability to predict neurodevelopment and has been successfully utilized in both research and clinical settings.12
We hypothesized that premature infants subjected to stressful early life experiences would develop an altered neurodevelopmental outcome at 36 - 37 weeks post-menstrual age (PMA). The purpose of the study was threefold: 1) To describe the cumulative pain/stress of preterm infants during the first 28 days of life in the NICU; 2) To describe neurobehavioral profiles of preterm infants at 36 - 37 weeks PMA; and 3) To investigate the relationships of the preterm infant's early life pain/stress experiences and the infant's neurobehavioral functioning.
Methods
Design
A prospective longitudinal study design was used to explore cumulative early life stressors in preterm infants during the first four weeks of NICU hospitalization and early neurobehavioral responses of these infants.
Participants
Stable preterm infants were recruited through a convenience sampling approach at two NICU sites of the Connecticut Children's Medical Center, at Hartford (Level IV NICU) and Farmington (Level III NICU), CT, U.S.A. Infants admitted to the NICU and meeting the inclusion criteria were invited to participate. Inclusion criteria: Infants who were 28 0/7 - 32 6/7 weeks gestational age at birth, aged 0 - 3 days old and cared for in an incubator. The infant's mother and/or father had to be ≥18 years old to give consent. Exclusion criteria: Infants who had: 1) known congenital anomalies; 2) severe periventricular/intraventricular hemorrhage (≥ Grade III); 3) undergone minor or major surgery including procedures such as inguinal hernia repair, laparotomy, thoracotomy, diaphragmatic hernia repair, or intestinal resection; and 4) history of illicit drug exposure during the current pregnancy. The focus of exclusion criteria were to control for factors that could contribute to extraordinary pain/stress experiences or influence neurobehavioral outcomes. The calculation of sample size was based on the exploratory nature of the study design.
Outcome Measurements and Data Collection
The study protocol was approved by the Institutional Review Boards of the affiliated hospitals and university. Data collection occurred when the infant was admitted in the NICU after obtaining informed consent from his/her parents. Early life stressors were measured daily from NICU enrollment to 4 weeks of hospitalization and infants' neurobehavioral responses were measured when the infant reached 36 - 37 weeks of post-menstrual age.
Early Life Pain/Stress was measured daily by using the NISS,10 a well described checklist based instrument to quantify infant pain/stressors. This instrument was originally developed for the measurement of NICU pain/stressors in Australia.10 We tested and modified the instrument because some of the original items were not relevant to NICU care in the U.S.A. and many procedures were not covered by the original NISS. We first conducted a focus group study (unpublished data) and then, a national survey to validate the addition or deletion of items.13 The modified NISS as developed by our research team now consists of 47 acute or short-term procedures (e.g., heel stick and chest tube insertion) and 23 chronic, long-term or recurrent events (e.g., nasogastric tube in situ and indwelling chest tube).13 Research nurses were trained in recording these procedures as they occurred in a dedicated log and the documentation was also crosschecked by the investigators against the clinical record. The frequency of acute pain/stressors and the duration (hours/minutes) of chronic pain/stressors were recorded. Each procedure/event was assigned or weighted based on a pain/stress severity level from 2 to 5 (2 = a little; 3 = moderate; 4 = very; and 5 = extremely). The acute and chronic NISS scores were further calculated over the course of days and weeks, and total scores over 4 weeks were summarized for assessing cumulative pain/stress.
Parental Contacts provided to the infant were also measured daily by recordings in the NICU using a self-developed chart because no existent tool is currently available for data collection. The contact chart included maternal and paternal contacts with their infant, such as skin-to-skin contact, maternal direct breastfeeding, holding or cuddling, hand swaddling or touch, and talking, singing, or reading, as well as other interactions with the infant. Duration (minutes) of each type of contact was recorded daily by research nurses using chart review of the nursing notes in the NICU.
Neurobehavioral Response Data were collected when the infant reached 36 - 37 weeks PMA or prior to hospital discharge using the NNNS instrument administered by a trained and certified neonatal developmental specialist.12 The NNNS is designed to examine both neurologic integrity and behavioral functioning of the normal and at-risk infant at 34 - 48 weeks PMA. The validity and reliability of this instrument has been tested in preterm infants.14,15 The three main sections of the NNNS are (i) neurological items for tone and reflexes; (ii) behavioral items of state, sensory, and interactive processes; and (iii) stress/abstinence responses. The NNNS includes a total of 115 items which generates 13 summary subscales measuring - habituation, attention, need for handling, quality of movement, self-regulation, non-optimal reflexes, asymmetric reflexes, arousal, hypertonicity, hypotonicity, excitability, lethargy, and stress/abstinence.12 The NNNS examinations were conducted in the NICU environment, ideally with the infant initially asleep; typically as per the design of the test, the infant awoke during the course of the examination which usually lasted approximately 30 minutes. Parents were encouraged to attend the NNNS administration.
For the purpose of our study, two relevant NNNS subscales, stress/abstinence (NSTRESS) and habituation (NHABIT) were selected as primary measures for evaluating the relationship of early life pain/stress and neurobehavioral outcomes. The NSTRESS subscale measures signs of stress and includes 50 items divided into physiologic, autonomic, CNS, skin, visual, gastrointestinal, and state categories.12 Each sign of stress/abstinence is scored as present or absent during the exam. A higher NSTRESS score demonstrates a more stressful behavioral performance. Habituation is an important concept in infant neurodevelopment indicating a decrease in response to a repeated stimulus leading to cessation of a behavioural response that occurs when an initially novel stimulus is repeatedly presented.16 The NHABIT subscale assesses the infant's ability to “protect” his/her sleep by rapidly adapting to repeated auditory and visual stimuli after an initial response. A higher NHABIT score indicates a better (more rapid) habituation outcome in response to stimulation.
Additional variables
Demographics, severity of illness, feeding type, infection and antibiotics use, probiotics and other medication use were collected for analyzing confounding variables. Severity of illness may influence the infant's ability to respond to stress 17 and was measured by the Score for Neonatal Acute Physiology – Perinatal Extension-II.18 These data were obtained by the researcher and/or trained research assistants from the medical records.
Data Analysis
Exploratory data analysis was initially conducted with a focus on describing characteristics of each stressor variable's daily occurrence and its distribution over time, using graphical techniques and summary statistics (mean ± SD). A linear regression model was used to assess the relationship between the NSTRESS outcome and key summary NISS measurements (i.e., mean, minimum, and maximum of the NISS scores) while controlling for confounding clinical and demographic factors, including gender, birth GA, body weight, SNAPEII, and delivery mode. In the linear regression model a good fit was ensured by the finding that residuals were randomly scattered around the horizontal axis. The variance of the residuals was tested to be homogenous by the White test. The Shapiro-Wilk test for the normal distribution of residuals further confirmed the normality assumption. All assumptions required for linear regression were thus satisfied. The variables in the final model were selected using the stepwise selection regression method in SAS. No evidence of multicollinearity was found given that all the variance inflation factors (VIF) were ≤ 5.
A post-hoc power analysis was conducted using Power Analysis and Sample Size Software (PASS-13) based on the method of Cohen.19 Using the multiple linear regression outputs, a sample size of 40 (after deleting infants with missing variables) achieved 84% power to detect an R-Squared of 0.16 attributed to the four independent variables (i.e., acute NISS, chronic NISS, direct breastfeeding and skin-to-skin holding) using an F-Test with α = 0.05, adjusting for the other controlled variables (i.e., gender, birth GA, body weight, SNAPE II, and delivery mode) with an R-Squared of 0.59.
Despite additional attempts to reschedule the exam to begin when the infant was asleep, 18 out of 49 (36.7%) infants had missing NHABIT scores, which is inherent to the design of the NNNS scale, as has been reported in previous studies.20,21 To account for these missing data, we first conducted a logistic regression to compare the missing data group members with their non-missing counterparts. There was no significant difference between the two groups in terms of all the independent covariates we considered, e.g., medical conditions, gestational age, delivery mode, and early life pain/stress. Based on the above evaluation, we assumed that the pattern of missing data of NHABIT was missing at random (MAR), where the probability of missingness depends solely on the observed data. We used multiple imputation (MI) with expectation-maximization (EM) algorithm to resolve the missing data problem. To be more specific, we first imputed the missing entries of the incomplete dataset 40 times, which resulted in 40 complete datasets. We then analyzed each of the 40 completed datasets using linear regression. Finally, we combined the estimates (coefficients, standard errors and p-values) across all the 40 imputed datasets using Rubin's combination rules.22 Linear regression was then carried out within each of the imputed datasets. The estimates (coefficients, standard errors and p-values) were combined across all the imputed datasets using Rubin's combination rules.23 To combine R-squared of each imputed datasets, we first used transformation (square root of inverse hyperbolic tangent) to convert R-squared to asymptotic normal distribution. Rubin's combination rule was then implemented on the transformed R-squared. Finally, we used the inverse transformation to switch back to the original metric of R-squared. This MAR assumption cannot be strictly verified using the data since the information that is needed for such a test is missing.24 Instead, we carried out a sensitivity analysis using the pattern-mixture approach. The results from sensitivity analysis were consistent with the results under the MAR assumption, which confirmed that the assumption was reasonable. All the analyses were run in SAS version 9.4.
Results
Infant and Parental Characteristics
A total of 50 preterm infants were recruited and followed-up in the study (Table 1). The majority of the infants were female (53%), white (80%), non-Hispanic (65%), and delivered by cesarean-section (65%). Infants were born at 31 ± 2 weeks gestational age and with 1431 ± 465 g birth weight. Mothers of the preterm infants were 30 ± 7 years old and 63% were married. One patient was transferred to another hospital before 36 weeks PMA and therefore, missed the NNNS examination. In the regression models of NSTRESS and NHABIT, 40 infant were included in the analysis after deleting missing data.
Table 1. Demographic Characteristics and Health Conditions.
| Characteristics | N | Mean (SD) | Range |
|---|---|---|---|
| Birth Gestational Age (GA, wks) | 49 | 30.73 (1.84) | 26.14 – 33.43 |
| Birth Body Length (cm) | 50 | 40.07 (3.95) | 32.50 – 50.50 |
| Birth Head Circumference (cm) | 48 | 27.80 (2.26) | 24.00 – 34.50 |
| Birth Body Weight (kg) | 50 | 1.44 (0.44) | 0.70 – 2.64 |
| NNNS examination- Body Weight (kg) | 45 | 2.26 (0.35) | 1.57 – 3.10 |
| Body Weight Difference (kg) | 45 | 0.81 (0.49) | - 0.28 – 1.80 |
| SNAPEII | 44 | 10.14 (10.99) | 0 – 44 |
|
| |||
| N | Percentage (%) | ||
|
| |||
| Gender | 50 | ||
| Male | 24 | 48.00 | |
| Female | 26 | 52.00 | |
| Race | 48 | ||
| White | 36 | 75.00 | |
| African American | 9 | 18.75 | |
| White & African American | 2 | 4.17 | |
| Asian | 1 | 2.08 | |
| Ethnicity | 49 | ||
| Hispanic | 12 | 24.49 | |
| Non- Hispanic | 37 | 75.51 | |
| Delivery type | 50 | ||
| Vaginal | 16 | 32.00 | |
| C-section | 34 | 68.00 | |
| PROM | 50 | ||
| Yes | 22 | 44.00 | |
| No | 28 | 56.00 | |
Note: Last Body Weight = body weight was measured on the day of NNNS examination performed when the infant reached 36 - 37 weeks post-menstrual age; Body Weight Difference = NNNS examination- Body Weight – Birth Body Weight; SNAPPEII= Score for Neonatal Acute Physiology - Perinatal Extension-II; PROM = premature rupture of membrane.
Acute and Chronic Painful/Stressful Events in the NICU
As shown in Figure 1, the unweighted daily acute pain/stressor was calculated by adding up the number of acute procedures (frequency) that the infants experienced; and the chronic pain/stressor was calculated by adding up hours (duration) of daily exposure to ‘chronic’ events, as previously defined in the NISS instrument. It is possible that a particular infant may encounter several chronic procedures at the same time, and since a cumulative hour score was calculated, it is possible that in certain instances the daily duration of chronic events might be more than 24 hours. During the first 4 weeks of NICU hospitalization, infants on average experienced a total of 643.15 ± 64.53 acute procedures with a daily average: 22.97 ± 2.30 procedures. There were 1192.51 ± 420.45 hours of chronic events with a daily average: 42.59 ± 15.02 hours. Figure 2 further shows the average unweighted amount of weekly acute (2A) and chronic (2B) pain/stressors during the 1st, 2nd, 3rd, and 4th week of NICU hospitalization. There was no change in the daily acute NISS scores over time, but daily chronic NISS scores showed a decrease over the first four weeks of infant life in the NICU. Figure 3 shows the most common daily pain/stressors and their assigned intensity scores per each activity as described in the NISS scoring system. The frequency of daily common acute (3A) and hours of chronic (3B) painful/stressful procedures experienced by preterm infants during the study period are shown.
Figure 1.
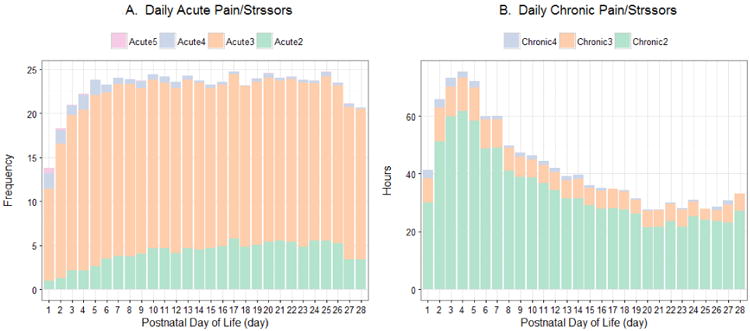
Unweighted daily mean pain/stressors during the first 28 postnatal days decomposed by pain/stress severity levels. 1A - Acute pain/stressors (frequency); 1B - Chronic pain/stressors (hours); Pain/stress severity levels: Acute2/Chronic2 = a little; Acute3/Chronic3 = moderate; Acute4/Chronic4 = very; and Acute5 = extremely painful/stressful.
Figure 2.
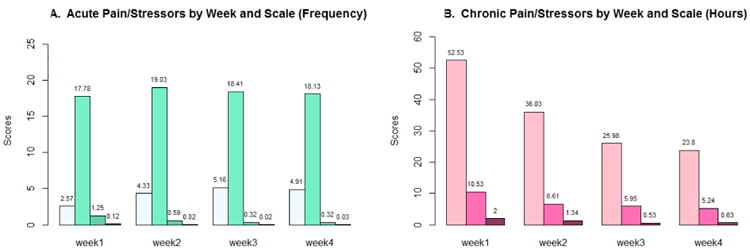
Unweighted weekly mean pain/stressors during the first four weeks decomposed by pain/stress severity levels. 2A - Average weekly mean (frequency) acute pain/stress experience; 2B - Average weekly mean (hours) chronic pain/stress experience. Pain/stress severity levels: Acute2/Chronic2 = a little; Acute3/Chronic3 = moderate; Acute4/Chronic4 = very; and Acute5 = extremely painful/stressful.
Figure 3.
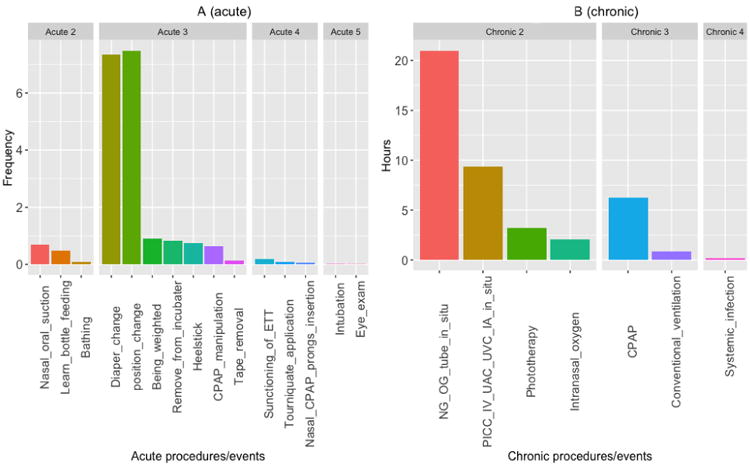
Common daily pain/stressors experienced during the first 28 postnatal days in the NICU. 3A - Acute procedures (frequency); 3B – Daily chronic events (hours); Pain/stress severity levels: Acute2/Chronic2 = a little; Acute3/Chronic3 = moderate; Acute4/Chronic4 = very; and Acute5 = extremely painful/stressful.
The mean daily weighted acute NISS score for each infant was 65.52 ± 5.50, which was computed as the weighted arithmetic mean of each acute event, with the corresponding severity level as the weight, ranging from 2 (a little) to 5 (extremely painful/stressful). The dominant component, Level 3 (moderate) pain/stressors involved, which accounted for the majority component of acute NISS scores included events such as heel stick, diaper change, or insertion of nasogastric tube (Fig. 3A). Similarly, each chronic event was assigned a pain severity level from 2 (a little) to 4 (very painful/stressful). The mean daily weighed chronic NISS score was 94.60 ± 33.34 for each infant, calculated as the weighted arithmetic mean of each chronic event, with the corresponding severity level as the weight. Here the dominant components were Level 2 chronic procedures such as intranasal oxygenation, presence of indwelling nasogastric tube, and presence of intravenous, umbilical arterial and umbilical venous catheter (Fig. 3B). Weighted acute and chronic NISS scores were used for the regression analysis mentioned below.
Parent Contact with infants in the NICU
Parent contact durations provided to the infant were measured daily in minutes. Skin-to-skin contacts (Kangaroo Care) were provided by mothers (13.35 ± 32.10 minutes) and fathers (1.44 ± 9.40 minutes) daily (t = 12.86, p < 0.001). Direct breastfeeding related infant contact time exclusively with their mothers (3.53 ± 13.41 minutes) was measured. Other forms of parent contacts included holding/cuddling (28.61 ± 50.89 minutes), hand swaddling/touching (14.15 ± 41.51 minutes) and talking/singing/reading (7.76 ± 33.04 minutes). Total daily parent contacts were 53.80 ± 68.07 minutes from mothers and 16.73 ± 38.19 minutes from fathers. Non-parent contact was 3.08 ± 13.71 minutes from others including grandparents, siblings and volunteers.
Neurobehavioral Outcomes
Neurobehavioral Outcomes in Preterm Infants
A summary score was generated for each of the 13 subscales of the NNNS (Table 2). As mentioned in the analysis, 18 out of 49 infants were coded as missing data because they were not in an appropriate state to administer the measurement.12 These infants started off asleep as the exam began, couldn't sustain a sleep state and the stimulus (either visual or auditory) woke up the infant or the infant continued to respond for an extended period (> 45 seconds after the stimulus), thus the remainder of habituation items could not be administered.
Table 2. NICU Network Neurobehavioral Scale (NNNS) Summary Scores.
| NNNS items | N | Mean (SD) | Range |
|---|---|---|---|
| Attention | 46 | 4.42 (1.11) | 2.29 - 6.67 |
| Arousal | 49 | 3.32 (0.58) | 2.29 - 5.14 |
| Regulation | 47 | 4.81 (0.80) | 3.23 - 6.31 |
| Habituation | 31 | 6.28 (1.52) | 3.00 - 8.50 |
| Handling | 49 | 0.55 (0.20) | 0.25 - 1.00 |
| Quality of Movement | 49 | 4.08 (0.69) | 2.83 - 5.67 |
| Excitability | 49 | 3.37 (1.99) | 0.00 - 8.00 |
| Lethargy | 49 | 6.24 (2.60) | 2.00 - 13.00 |
| Non-Optimal reflexes | 49 | 5.41 (1.78) | 2.00 - 11.00 |
| Asymmetrical reflexes | 49 | 0.22 (0.62) | 0.00 - 3.00 |
| Hypertonicity | 49 | 0.04 (0.20) | 0.00 - 1.00 |
| Hypotonicity | 49 | 0.55 (0.89) | 0.00 - 4.00 |
| Stress/Abstinence | 49 | 0.18 (0.10) | 0.00 - 0.39 |
Note: The NNNS examination generated 13 summary scores of the subscales.
Impact of Pain/Stress on Neurobehavioral Outcomes
In the linear regression model with NSTRESS as the outcome measure (Table 3), after deleting infants with missing covariates, the effective sample size was 40 infants. Fifty-nine percent of the variance of NSTRESS was explained by the model, F (9, 30) = 4.89, p < 0.001. The daily weighted acute NISS score had a significant association with NSTRESS, p = 0.03, and the parameter estimate of acute NISS was positive, indicating that NSTRESS scores would be higher and therefore worse if the infant experienced more daily acute pain/stressors. The daily chronic pain/stressors also had a significant positive association with NSTRESS, p = 0.05, i.e., the NSTRESS scores would be significantly increased (worse) if the infant experienced more daily chronic pain/stressors.
Table 3. Results of Linear Regression Model of NNNS Subscales.
| Stress/Abstinence (NSTRESS) N = 40 | Habituation (NHABIT) N = 40 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Parameter | Estimate | F-value | p-value | Estimate | T-value | p-value | |
| Gender | female | -0.0134 | 0.39 | 0.54 | 0.4027 | 0.86 | 0.39 |
| male | 0.0000 | 0.0000 | |||||
| Birth Gestational Age | -0.0090 | 0.82 | 0.37 | -0.2275 | -1.22 | 0.22 | |
| Last Body Weight | 0.0462 | 1.47 | 0.23 | -0.6975 | -1.10 | 0.27 | |
| SNAPEII | -0.0003 | 0.03 | 0.85 | -0.0059 | -0.22 | 0.82 | |
| Delivery | C-section | 0.0369 | 1.10 | 0.30 | -0.4879 | -0.79 | 0.43 |
| vaginal | 0.0000 | 0.0000 | |||||
| Daily Acute NISS Score | 0.0035 | 5.30 | 0.03* | -0.0889 | -2.94 | <0.01** | |
| Daily Chronic NISS Score | 0.0005 | 4.13 | 0.05 | -0.0186 | -2.48 | 0.02* | |
| Daily Breastfeeding | -0.0003 | 0.03 | 0.85 | 0.0647 | 2.27 | 0.02* | |
| Daily Skin-to-Skin Holding | 0.0008 | 1.27 | 0.27 | 0.0670 | 4.81 | <0.01** | |
|
| |||||||
| R-Squared | 0.59 | R-Squared | 0.78 | ||||
Note:
p<0.05,
p<0.01;
Daily Acute NISS score = the daily weighted average of each severity level acute pain/stressors; Daily Chronic NISS score = the daily weighted average of each severity level chronic pain/stressors.
After multiple imputation, the effect sample size of NHABIT was 40 infants (Table 3). Seventy-eight percent of the variance of NHABIT was explained by the model. Both daily weighted acute (p < 0.01) and chronic (p = 0.01) NISS scores had significantly negative associations with infants' habituation performance. Daily mean duration of direct breastfeeding (p < 0.05) and skin-to-skin holding (p < 0.01) were significantly associated with better habituation scores in preterm infants.
Discussion
Although survival rates of extremely premature infants have steadily improved, the incidence of later developmental disabilities for these infants remains high 25 and concerns have been raised about the effects of stressful early life experiences on immature neuro-immune systems and long-term health outcomes.5 However, the impact of cumulative early life stressors altering neurodevelopment has remained unclear. Even though there have been earlier studies relating early life stress to neurodevelopmental outcomes, to the best of our knowledge, this is the first study innovatively taken together stressful events and protective experiences of preterm infants during the NICU stay to examine neurobehavioral outcomes. We found that both acute and chronic pain/stress significantly contributed to the neurobehavioral outcomes, meanwhile, direct breastfeeding and skin-to-skin holding were also significantly associated with infant habituation, but in the opposite direction.
Stressful early life experiences in the NICU are inherent to high-technology lifesaving care of preterm infants. Repeated skin breaches such as heel sticks and intravenous line placements, other even more painful procedures as well as stressful daily care-handling and treatment events are some of the major stressors to which neonates are routinely subjected to in the NICU. Results of our study showed that preterm infants experienced a total of 643 acute procedures (23 daily) and 1193 hours of chronic events (43 hours daily) cumulatively (chronic stressors accruing simultaneously) during their first 4 weeks of NICU hospitalization. The findings are consistent with previous studies, showing that infants can experience an average of 10 – 18 painful procedures per day, and very preterm infants may have hundreds of painful procedures during their NICU stay.26-30 Recent multicenter studies in France also showed that a newborn experienced a mean number of 16 heelsticks and 4 venipunctures during a mean of 8 days NICU hospitalization without routine analgesic use.31,32 The frequency of acute pain/stressors found in our study was higher than many previous studies; this may be due to different measurement tools being used in studies as well as the increased severity of illness and younger gestation of the infants participating in our study. The modified NISS instrument used in the study, included elements such as diaper change, position change, mouth care, bathing, and weighing (Fig. 3A), which were not identified as painful/stressful procedures in previous studies. When each procedure or event was weighted by severity levels, the level 3 (moderate stress) acute procedures and level 2 (a little stressful) chronic events were the most frequent component of the cumulative pain/stressors. Even though these procedures are common practice in the NICU and are not usually categorized as ‘harmful’ in preterm infants, their ability to induce a stress response and be responsible for cumulative ‘harm’ needs to be considered and evaluated in future studies. The way we examined these stressors is different than in previous research and needs to be further examined. We believe our scoring better takes into account the number of different events that are occurring and being endured by the vulnerable preterm infants. Meanwhile, in consideration of the chart review data collection procedure, these data could be also underestimated, then, the rates of pain/stress could be higher than observed in the present study. We expect to further refine our modified NISS instrument based on these findings and in other studies we are conducting.
Maternal-infant separation is another crucial stressor in the NICU. Maternal and paternal contact with preterm infants in early life is the cornerstone of normal infant growth and development. Our study showed that infants received skin-to-skin contact by their mothers (13 minutes daily on average) and fathers (1 minute daily on average), direct breastfeeding from their mothers (4 minutes daily on average). The amount of skin-to-skin contact provided from both mother and father seemed insufficient to meet preterm infants' needs 33 and direct breastfeeding contact was also poor for the these infants.34 These low daily averages could be related to the fact that our data were collected during the first four weeks of life when these very preterm infants are very immature and less stable and may not be ready for these interventions. It also needs to be noted that the data collected for this variable was from chart review and parent interaction may have been under documented. Literatures including our previous studies show that skin-to-skin contact and other contacts, such as direct breastfeeding and swaddling have significant effects on reducing infant pain and stress in early life.35,36 When infants undergo painful procedures, skin-to-skin position can act as a pain/stress treatment through multisensory stimulation input, activation of the neuro-chemical system, and modulation of the stress regulation system involved in painful experience, which supports infants' neurodevelopment.
There is a lack of published norms of NNNS for very preterm infants (born at 28 – 32 weeks GA). The NNNS summary scores (Table 2) of the current study were similar to previous studies,15,37,38 in that the NNNS subscales of handling, excitability, lethargy, non-optimal reflexes, hypotonicity and stress/abstinence were higher. The subscales of attention, habituation, arousal, regulation, quality of movement, asymmetrical reflexes and hypertonicity were lower in very preterm infants, compared to infants born full term.39-41 These findings indicate that infants born prematurely demonstrate a different level of developmental competence during the neurobehavioral assessment at 36 – 37 weeks PMA compared to term infants.
The NNNS was created based on the notion that all human experiences have psychosocial as well as biological or organic context which dynamically influence each other in connection with the environment.40 The NNNS considers the infant to be an active participant throughout the assessment, and is in part responsible for generating responses to stimuli as well as the environment. This represents the challenge that preterm infants have to sustain deep sleep in often random and continuous sensory rich environment of the NICU. Infants must be asleep at the start of the NNNS test for obtaining the habituation data. In our study, there were only 31 effective observations/infants for the habituation (NHABIT) measurement after deleting missing values because many infants consistently were not in an appropriate state. An effort was made to begin the exam with the infant asleep, and when not possible on initial exam attempt was made to evaluate this response on the following day. Thus the valid data of NHABIT may have been better than previously reported in the literature and many studies omitted reporting on habituation.15,39 The infant's ability to protect their sleep is imperative to their developmental trajectory. The habituation package utilizes response decrement items that indicate an infant's ability to habituate; which means the infant moves from broad, generalized responses such as startles to little or no response over repeated presentations of a specific stimuli which provides an indicator of neural processing.42 The response decrement items also assess for the possibility that the infant may habituate differently to light, sound, or tactile stimuli. The infant's inability to habituate may be an indication of an immature or stressed nervous system.42 Abnormal habituation has been described in many conditions where there is abnormal central nervous system function such as hyperkinetic children, Down's Syndrome, brain damage and unconsciousness.43
Preterm infants possess both anatomical and neurochemical capabilities of pain perception.44 Moreover, their tactile threshold is lower, and descending inhibitory pathways are immature, thereby making them more sensitive to cumulative pain/stressors. Greater numbers of painful procedures have been found to directly predict decreased head growth and brain function in preterm infants indicating that pain/stress during this vulnerable period may activate a downstream cascade of stress signaling that affects later growth.9 Continual adaptation to repeated and cumulative pain/stressors appears to induce functional changes in neurobehavioral pain/stress processing systems.45 However, the mechanisms underlying the consequences of neonatal noxious insults on neurodevelopment are still largely. A recent study identified a significant negative correlation between the amount of skin-breaking procedures and the neuroendocrine marker 17-hydroxyprogesterone (17-OHP values), suggesting that exposures of recurrent pain/stressor may be a more important predicator than birthweight, gestational age, or chronological age in contributing the variance of 17-OHP levels at 37 weeks PMA.29 In the regression analyses of our study, both weighted acute and chronic NISS scores were significantly associated with neurobehavioral outcomes, the NSTRESS and NHABIT, indicating the more painful/stressful procedures experienced in early life, the more stress signs showed and worse habituation behavior demonstrated in preterm infants. The effects of cumulative pain/stressors on neonatal neurodevelopment are still poorly studied. Gorzilio and colleagues found that acute stressful events are predictors for worse development of motor, alertness, and orientation in preterm infants.46 Montirosso and colleagues also reported that preterm infants from NICUs with better pain management also have higher scores of attention and arousal, and lower scores of lethargy and non-optimal reflexes on the NNNS than infants from NICUs with inadequate pain management.15
A large number of animal and human studies show that deprivation of maternal care, another crucial stressor in the NICU, results in altered neuronal, hormonal, genetic, and bio-behavioral outcomes over the sensitive developmental period.44 Maternal-infant contact, such as kangaroo care can dampen stress response to neonatal pain and promote positive neurodevelopment.47 Our study provides evidence that increased daily Kangaroo Care and direct breastfeeding provided to infants, is associated with better habituation responses at 36 – 37 weeks PMA. Similar findings reported in a recent study support our results that the frequency of Kangaroo Care was associated with better neurobehavioral performance (NNNS) in preterm infants, including higher scores on attention, quality of movements, and lower scores on asymmetry and NSTRESS.37 More parental presence and holding in the NICU were also found to be associated to better early neurobehavior (NNNS scores), including quality of movement, arousal, excitability, and stress responses.48
Generalization of findings may be limited by the exploratory attribute of the study design and the small sample size. Another limitation is that the data collection of pain/stressors and contact measurement were primarily based on chart review. Even though the NISS is a well-developed instrument, the weighted NISS score is still considered as an indirect measurement of stress because the stressful level of each events in the NICU is perceived by the health professionals. Potential biases caused by these limitations need to be considered and fully powered studies are demanded.49 As we become more successful in increasing survival of preterm infants, we need to become more cognizant of the continuing exposure of these vulnerable infants to a wide range of pain/stressors during their stay in the NICU and the cumulative effects of these early life stressors on neurodevelopment. To ameliorate these negative consequences, changing the NICU environmental conditions, reducing stressful/painful events and enhancing the protective mechanisms are imperative. Our research contributes to the knowledge of the impact of early life experience on the prediction of neurobehavioral outcomes in preterm infants. These findings will provide neonatal clinicians and scientists enhanced capability in developing patient-oriented interventions, e.g., systematic monitoring of pain/stressor and providing early neuroprotective interventions for preterm high-risk infants.
Highlights.
Preterm infants experienced a high degree of pain/stress in the NICU, both in numbers of daily acute events and cumulative times of chronic/stressful exposure
Both acute and chronic pain/stress experienced in early life significantly contributed to the neurobehavioral outcomes.
Systematic monitoring of pain/stressor and providing early neuroprotective interventions for preterm high-risk infants are needed.
Acknowledgments
The authors thank the medical and nursing staff in the NICUs of Connecticut Children's Medical Center at Hartford and Farmington, CT for their support and assistance as well as the participants in our study. We thank Victoria Vazquez, Carrie-Ellen Briere for their assistance in recruiting subjects, collecting clinical data, managing stool sample collection and storage, and data management.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hamilton BEPD, Martin JA, Osterman MMHS, Curtain SMA, Mathews TJMS. Births: Final Data for 2014. Natl Vital Stat Rep. 2015;64:1–64. [PubMed] [Google Scholar]
- 2.Stoll BJ, Hansen NI, Bell EF, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. Jama. 2015;314:1039–51. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;379:445–52. doi: 10.1016/S0140-6736(11)61577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kugelman A, Colin AA. Late preterm infants: near term but still in a critical developmental time period. Pediatrics. 2013;132:741–51. doi: 10.1542/peds.2013-1131. [DOI] [PubMed] [Google Scholar]
- 5.Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. 2016;40:542–8. doi: 10.1053/j.semperi.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Smith GC, Gutovich J, Smyser C, et al. Neonatal intensive care unit stress is associated with brain development in preterm infants. Annals of neurology. 2011;70:541–9. doi: 10.1002/ana.22545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morken NH. Preterm birth: new data on a global health priority. Lancet. 2012;379:2128–30. doi: 10.1016/S0140-6736(12)60857-5. [DOI] [PubMed] [Google Scholar]
- 8.Valeri BO, Holsti L, Linhares MB. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31:355–62. doi: 10.1097/AJP.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 9.Vinall J, Miller SP, Chau V, Brummelte S, Synnes AR, Grunau RE. Neonatal pain in relation to postnatal growth in infants born very preterm. Pain. 2012;153:1374–81. doi: 10.1016/j.pain.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Newnham CA, Inder TE, Milgrom J. Measuring preterm cumulative stressors within the NICU: the Neonatal Infant Stressor Scale. Early Hum Dev. 2009;85:549–55. doi: 10.1016/j.earlhumdev.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Noble Y, Boyd R. Neonatal assessments for the preterm infant up to 4 months corrected age: a systematic review. Dev Med Child Neurol. 2012;54:129–39. doi: 10.1111/j.1469-8749.2010.03903.x. [DOI] [PubMed] [Google Scholar]
- 12.Lester BM, Tronick EZ, Brazelton TB. The Neonatal Intensive Care Unit Network Neurobehavioral Scale procedures. Pediatrics. 2004;113:641–67. [PubMed] [Google Scholar]
- 13.Xu W, Walsh S, Cong XS. Development of Accumulated Pain/Stressor Scale (APSS) in NICUs: A National Survey. Pain Manag Nurs. 2016;17:354–62. doi: 10.1016/j.pmn.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pineda RG, Tjoeng TH, Vavasseur C, Kidokoro H, Neil JJ, Inder T. Patterns of altered neurobehavior in preterm infants within the neonatal intensive care unit. J Pediatr. 2013;162:470–6 e1. doi: 10.1016/j.jpeds.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montirosso R, Del Prete A, Bellu R, Tronick E, Borgatti R. Level of NICU quality of developmental care and neurobehavioral performance in very preterm infants. Pediatrics. 2012;129:e1129–37. doi: 10.1542/peds.2011-0813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson RF, Clansman DL. Neural and behavioural mechanisms of habituation and sensitisation. In: Tighe TJ, Leaton RN, editors. Habituation. Hillsdale, NJ: Lawrence Erlbaum Associates; 1976. p. 49. [Google Scholar]
- 17.Morison SJ, Holsti L, Grunau RE, et al. Are there developmentally distinct motor indicators of pain in preterm infants? Early Hum Dev. 2003;72:131–46. doi: 10.1016/s0378-3782(03)00044-6. [DOI] [PubMed] [Google Scholar]
- 18.Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100. doi: 10.1067/mpd.2001.109608. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 20.Aubuchon-Endsley N, Morales M, Giudice C, et al. Maternal pre-pregnancy obesity and gestational weight gain influence neonatal neurobehaviour. Matern Child Nutr. 2016 doi: 10.1111/mcn.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eeles AL, Olsen JE, Walsh JM, et al. Reliability of Neurobehavioral Assessments from Birth to Term Equivalent Age in Preterm and Term Born Infants. Physical & occupational therapy in pediatrics. 2016:1–11. doi: 10.3109/01942638.2015.1135845. [DOI] [PubMed] [Google Scholar]
- 22.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention science : the official journal of the Society for Prevention Research. 2007;8:206–13. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- 23.Chen Q, Ibrahim JG, Chen MH, Senchaudhuri P. Theory and Inference for Regression Models with Missing Responses and Covariates. Journal of multivariate analysis. 2008;99:1302–31. doi: 10.1016/j.jmva.2007.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuan Y. Sensitivity Analysis in Multiple Imputation for Missing Data. Proceedings of the SAS Global Forum 2014 Conference. 2014 [ http://supportsascom/resources/papers/proceedings14/SAS270-2014pdf]
- 25.Schmidhauser J, Caflisch J, Rousson V, Bucher HU, Largo RH, Latal B. Impaired motor performance and movement quality in very-low-birthweight children at 6 years of age. Dev Med Child Neurol. 2006;48:718–22. doi: 10.1017/S001216220600154X. [DOI] [PubMed] [Google Scholar]
- 26.Carbajal R, Rousset A, Danan C, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. Jama. 2008;300:60–70. doi: 10.1001/jama.300.1.60. [DOI] [PubMed] [Google Scholar]
- 27.Kothari SY, Dongara AR, Nimbalkar SM, Phatak AG, Nimbalkar AS. Missed Opportunities for Sedation and Pain Management at a Level III Neonatal Intensive Care Unit, India. Frontiers in pediatrics. 2016;4:7. doi: 10.3389/fped.2016.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cruz MD, Fernandes AM, Oliveira CR. Epidemiology of painful procedures performed in neonates: A systematic review of observational studies. European journal of pain (London, England) 2016;20:489–98. doi: 10.1002/ejp.757. [DOI] [PubMed] [Google Scholar]
- 29.Rohan AJ. Pain-associated stressor exposure and neuroendocrine values for premature infants in neonatal intensive care. Dev Psychobiol. 2016;58:60–70. doi: 10.1002/dev.21346. [DOI] [PubMed] [Google Scholar]
- 30.Victoria NC, Murphy AZ. The long-term impact of early life pain on adult responses to anxiety and stress: Historical perspectives and empirical evidence. Experimental neurology. 2016;275 Pt 2:261–73. doi: 10.1016/j.expneurol.2015.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Courtois E, Droutman S, Magny JF, et al. Epidemiology and neonatal pain management of heelsticks in intensive care units: EPIPPAIN 2, a prospective observational study. Int J Nurs Stud. 2016;59:79–88. doi: 10.1016/j.ijnurstu.2016.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Courtois E, Cimerman P, Dubuche V, et al. The burden of venipuncture pain in neonatal intensive care units: EPIPPAIN 2, a prospective observational study. Int J Nurs Stud. 2016;57:48–59. doi: 10.1016/j.ijnurstu.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 33.Ludington-Hoe SM. Thirty years of Kangaroo Care science and practice. Neonatal Netw. 2011;30:357–62. doi: 10.1891/0730-0832.30.5.357. [DOI] [PubMed] [Google Scholar]
- 34.Pineda R. Direct breast-feeding in the neonatal intensive care unit: is it important? J Perinatol. 2011;31:540–5. doi: 10.1038/jp.2010.205. [DOI] [PubMed] [Google Scholar]
- 35.Cong X, Cusson RM, Walsh S, Hussain N, Ludington-Hoe SM, Zhang D. Effects of skin-to-skin contact on autonomic pain responses in preterm infants. J Pain. 2012;13:636–45. doi: 10.1016/j.jpain.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Johnston C, Campbell-Yeo M, Disher T, et al. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst Rev. 2017;2:CD008435. doi: 10.1002/14651858.CD008435.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silva MG, Barros MC, Pessoa UM, Guinsburg R. Kangaroo-mother care method and neurobehavior of preterm infants. Early Hum Dev. 2016;95:55–9. doi: 10.1016/j.earlhumdev.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Sullivan MC, Miller RJ, Fontaine LA, Lester B. Refining Neurobehavioral Assessment of the High-Risk Infant Using the NICU Network Neurobehavioral Scale. J Obstet Gynecol Neonatal Nurs. 2012;41:17–23. doi: 10.1111/j.1552-6909.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- 39.Spittle AJ, Walsh J, Olsen JE, et al. Neurobehaviour and neurological development in the first month after birth for infants born between 32-42 weeks' gestation. Early Hum Dev. 2016;96:7–14. doi: 10.1016/j.earlhumdev.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 40.Lester BM, Tronick EZ. History and description of the Neonatal Intensive Care Unit Network Neurobehavioral Scale. Pediatrics. 2004;113:634–40. [PubMed] [Google Scholar]
- 41.Tronick E, Lester BM. Grandchild of the NBAS: the NICU network neurobehavioral scale (NNNS): a review of the research using the NNNS. Journal of child and adolescent psychiatric nursing : official publication of the Association of Child and Adolescent Psychiatric Nurses, Inc. 2013;26:193–203. doi: 10.1111/jcap.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boukydis CF, Bigsby R, Lester BM. Clinical use of the Neonatal Intensive Care Unit Network Neurobehavioral Scale. Pediatrics. 2004;113:679–89. [PubMed] [Google Scholar]
- 43.Leader LR, Baillie P, Martin B, Vermeulen E. The assessment and significance of habituation to a repeated stimulus by the human fetus. Early Hum Dev. 1982;7:211–9. doi: 10.1016/0378-3782(82)90084-6. [DOI] [PubMed] [Google Scholar]
- 44.Anand KJ, Hall RW. Love, pain, and intensive care. Pediatrics. 2008;121:825–7. doi: 10.1542/peds.2007-3828. [DOI] [PubMed] [Google Scholar]
- 45.Slater R, Worley A, Fabrizi L, et al. Evoked potentials generated by noxious stimulation in the human infant brain. European journal of pain (London, England) 2010;14:321–6. doi: 10.1016/j.ejpain.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 46.Gorzilio DM, Garrido E, Gaspardo CM, Martinez FE, Linhares MB. Neurobehavioral development prior to term-age of preterm infants and acute stressful events during neonatal hospitalization. Early Hum Dev. 2015;91:769–75. doi: 10.1016/j.earlhumdev.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 47.Mooney-Leber SM, Brummelte S. Neonatal pain and reduced maternal care: Early-life stressors interacting to impact brain and behavioral development. Neuroscience. 2017;342:21–36. doi: 10.1016/j.neuroscience.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Reynolds LC, Duncan MM, Smith GC, et al. Parental presence and holding in the neonatal intensive care unit and associations with early neurobehavior. J Perinatol. 2013;33:636–41. doi: 10.1038/jp.2013.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MEDICINE COFANaSOAAP. Prevention and Management of Procedural Pain in the Neonate: An Update. Pediatrics. 2016;137:e20154271. doi: 10.1542/peds.2015-4271. [DOI] [PubMed] [Google Scholar]


