Abstract
Background
Alcohol use is associated with health behaviors that impact cardiovascular outcomes in patients with hypertension, including avoiding salt, exercising, weight management, and not smoking. This study examined associations between varying levels of alcohol use and self-reported cardiovascular health behaviors among hypertensive Veterans Affairs (VA) outpatients.
Methods
Male outpatients with self-reported hypertension from seven VA sites who returned mailed questionnaires (n=11,927) were divided into five levels of alcohol use: non-drinking, low-level use, and mild, moderate, and severe alcohol misuse based on AUDIT-C scores (0, 1-3, 4-5, 6-7 and 8-12, respectively). For each category, adjusted logistic regression models estimated the prevalence of patients who self-reported avoiding salt, exercising, controlling weight, or not smoking, and the composite of all four.
Results
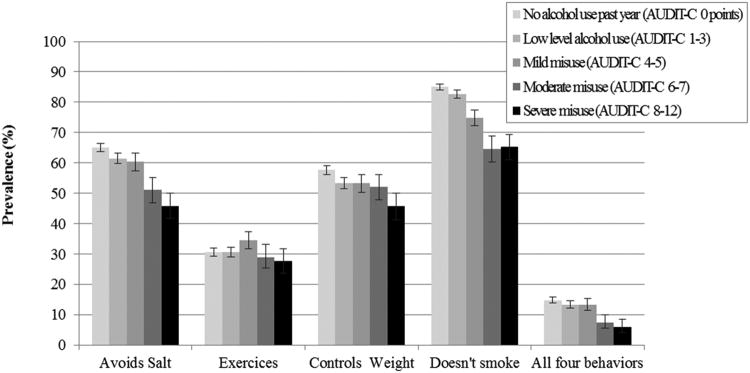
Increasing level of alcohol use was associated with decreasing prevalence of avoiding salt, controlling weight, not smoking, and the combination of all four behaviors (p-values all <0.001). A linear trend was not observed for exercise (p=0.83), which was most common among patients with mild alcohol misuse (p=0.01 relative to non-drinking).
Conclusions
Alcohol consumption is inversely associated with adherence to cardiovascular self-care behaviors among hypertensive VA outpatients. Clinicians should be especially aware of alcohol use level among hypertensive patients.
Keywords: alcohol, hypertension, self-care, cardiovascular
Introduction
One in three Americans has hypertension,1,2 which is a potentially modifiable risk factor for morbidity and mortality from coronary artery disease, stroke, peripheral vascular disease, and chronic kidney disease.3 Moreover, 54% of hypertensive individuals have uncontrolled hypertension,4 which accounts for nearly half of all deaths related to cardiovascular disease, the primary cause of death in the US.5 Hypertension can be managed in part by behavioral self-management. 6,7 Specifically, active patient involvement in following dietary recommendations, increasing physical activity, quitting smoking and/or adhering to medication regimens are cardiovascular health behaviors recommended by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7).7
Hypertension often co-occurs with alcohol misuse,8-10 which includes drinking above recommended limits and/or meeting diagnostic criteria for alcohol use disorders. 11 Alcohol misuse is likely to worsen hypertension,12 is associated with poorer adherence to antihypertensive medications,13 and has been associated with poorer diabetes self-care behaviors.14,15
While prior studies have assessed the prevalence of cardiovascular health behaviors among adults with hypertension,16,17 no previous study to our knowledge has described whether adherence to cardiovascular health behaviors differs by level of alcohol use. Because a dose-response association between levels of alcohol use and cardiovascular health behaviors would support a causal association, understanding whether such an association exists may influence clinician provision of brief alcohol interventions to hypertensive patients. This study describes the association between varying levels of alcohol use and four cardiovascular health behaviors among Veteran outpatients with self-reported hypertension.
Methods
This cross-sectional study used data from the Ambulatory Care Quality Improvement Project (ACQUIP), a negative trial of a health services intervention.18 Patients were enrolled in ACQUIP between 3/1997 and 12/1999, and were eligible if they visited their primary care provider at one of seven VA General Medicine Clinics in the year prior to enrollment. Eligible patients were mailed the ACQUIP Health Checklist, a baseline health inventory survey. The Health Checklist assessed whether participants had ever been told by their doctor or nurse that they had any of 24 chronic conditions, including hypertension. The Health Checklist also included validated screening questionnaires for both alcohol and tobacco.19 All respondents who self-reported hypertension on the Health Checklist were mailed a hypertension questionnaire, which asked participants to report the frequency with which they practiced cardiovascular health behaviors.18 All data for this study was obtained from ACQUIP surveys.
Male ACQUIP participants were included in the present study if they: 1) responded to the Health Checklist (response rate 59%) and were alive 1 year later; 2) self-reported ever being told by their doctor or nurse that they had hypertension; and 3) returned the Hypertension Questionnaire with one to four health behavior questions completed (response rate 66%). Women were excluded because they were < 3% of ACQUIP participants and few reported high levels of alcohol use.
These secondary analyses were approved by the Institutional Review Boards at VA Puget Sound and the University of Washington.
Measures
Alcohol Use and Misuse
Alcohol use and misuse were measured by the Alcohol Use Disorders Identification Test – Consumption (AUDIT-C), a validated screening questionnaire for alcohol misuse.19 Increasing AUDIT-C scores reflect increased alcohol consumption, adverse consequences of drinking, and likelihood of alcohol use disorders.20,21 Patients were divided a priori into five groups based on AUDIT-C scores (0-12 points) used in prior research:15 no past year alcohol use (0 points), low-level alcohol use (1-3), and mild (4-5), moderate (6-7), and severe (8-12) misuse.13,22
Cardiovascular Health Behaviors
Four primary outcomes of cardiovascular health behaviors were derived based on patient report of avoiding salt, exercising, controlling weight, and not smoking.6,7 Patients were asked on the Hypertension Questionnaire how often they: “avoid salt in my diet,” “exercise,” and “control my weight” with five response options ranging from “all of the time” to “never.” Patients were considered engaged in each of these health behaviors if they responded “all or most of the time.” Not smoking was measured by self-report of no past-year smoking on the Health Checklist. A composite dichotomous measure was derived for patients reporting all four cardiovascular health behaviors.
Other Patient Characteristics
Demographic information was obtained from the ACQUIP Health Checklist and included age, race/ethnicity, education, marital status, and income level. Additional information on clinical characteristics included history of drug abuse (based on patient report of being told by a doctor or nurse that they had drug abuse), depression (assessed by a score a score >17 on the Mental Health Inventory (MHI-5)) 23 and seven self-reported chronic medical conditions (myocardial infarction, diabetes mellitus, stroke, cancer, congestive heart failure, chronic lung disease, and pneumonia). These medical conditions, selected from 24 patient self-reported conditions on the ACQUIP Health Checklist,24 were included consistent with the Seattle Index of Comorbidity,24,25 which has been shown to predict mortality and utilization in the VA system,24 but was not used in the present study due to its inclusion of smoking.
Analyses
Participant characteristics and the unadjusted prevalence of cardiovascular health behaviors were described and compared across alcohol use groups using Chi-square tests of independence in the sample of eligible patients with hypertension. Multivariate logistic regression models were used to estimate the adjusted prevalence of report of each cardiovascular health behavior across the five categories of alcohol use. Models were adjusted for all measured patient characteristics due to known associations between these characteristics and both alcohol use and cardiovascular health behaviors. Non-drinkers were used as the referent group, consistent with a previous study of the AUDIT-C and antihypertensive medication adherence.13 Wald tests26 were used to assess linear trends for each outcome across alcohol use levels. Results were considered statistically significant at α=0.05, and all analyses were performed using STATA Special Edition 9.2 (2005, Stata Corporation, College Station, TX).
Results
Among eligible men with hypertension (n=11,927), 47% reported no past-year alcohol use, 31% reported low-level use, and 11%, 5%, and 5% screened positive for mild, moderate, and severe alcohol misuse, respectively (Table 1). Differences in all patient characteristics were observed across alcohol use groups (Table 1). Patients who screened positive for alcohol misuse were younger and less likely to be White or married (compared with non-white or non-married, respectively), had less education and lower incomes, and had greater drug abuse and chronic lung disease but generally lower rates of other chronic disease.
Table 1. Characteristics of Study Sample across Alcohol Use and Misuse Groups* (n=11,927).
| No Alcohol Use AUDIT-C 0 points (n=5585; 46.8%) | Low-level Use AUDIT-C 1-3 points (n=3705; 31.0%) | Mild Misuse AUDIT-C 4-5 points (n=1353; 11.3%) | Moderate Misuse AUDIT-C 6-7 points (n=634; 5.3%) | Severe Misuse AUDIT-C 8-12 points (n=650; 5.4%) | Total (n=11927) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | p† | n | (%) | |
| Age, Mean (SD) | 65.5 | (10.3) | 64.4 | (11.0) | 64.4 | (10.5) | 61.1 | (10.5) | 57.8 | (10.1) | |||
| Age | <0.001 | ||||||||||||
| <50 | 505 | (9.0) | 425 | (11.5) | 145 | (10.7) | 104 | (16.4) | 161 | (24.8) | 1340 | (11.2) | |
| 50-59 | 931 | (16.7) | 689 | (18.6) | 250 | (18.5) | 146 | (23.0) | 196 | (30.2) | 2212 | (18.5) | |
| 60-69 | 1893 | (33.9) | 1211 | (32.7) | 454 | (33.6) | 236 | (37.2) | 201 | (30.9) | 3995 | (33.5) | |
| ≥70 | 2251 | (40.3) | 1374 | (37.1) | 503 | (37.2) | 146 | (23.0) | 91 | (14.0) | 4365 | (36.6) | |
| White | 4060 | (72.7) | 2689 | (72.6) | 993 | (73.4) | 437 | (68.9) | 434 | (66.8) | <0.001 | 8613 | (72.2) |
| Education | <0.001 | ||||||||||||
| Less than 12th grade | 1938 | (34.7) | 821 | (22.2) | 264 | (19.5) | 166 | (26.2) | 188 | (28.9) | 3377 | (28.3) | |
| HS graduate | 2930 | (52.5) | 2094 | (56.5) | 766 | (56.6) | 368 | (58.0) | 391 | (60.2) | 6549 | (54.9) | |
| College graduate | 580 | (10.4) | 689 | (18.6) | 292 | (21.6) | 79 | (12.5) | 53 | (8.2) | 1693 | (14.2) | |
| Married | 3631 | (65.0) | 2321 | (62.6) | 796 | (58.8) | 291 | (45.9) | 261 | (40.2) | <0.001 | 7300 | (61.2) |
| Income | <0.001 | ||||||||||||
| <$20,000 | 3581 | (64.1) | 1937 | (52.3) | 714 | (52.8) | 399 | (62.9) | 454 | (69.8) | 7085 | (59.4) | |
| $20,000-$39,999 | 1337 | (23.9) | 1058 | (28.6) | 378 | (27.9) | 142 | (22.4) | 119 | (18.3) | 3034 | (25.4) | |
| ≥$40,000 | 259 | (4.6) | 402 | (10.9) | 183 | (13.5) | 54 | (8.5) | 41 | (6.3) | 939 | (7.9) | |
| Drug abuse history | 100 | (1.8) | 53 | (1.4) | 29 | (2.1) | 27 | (4.3) | 67 | (10.3) | <0.001 | 276 | (2.3) |
| Depression (MHI-5≥17)§ | 1374 | (24.6) | 723 | (19.5) | 249 | (18.4) | 152 | (24.0) | 108 | (16.6) | <0.001 | 2744 | (23.0) |
| Comorbid conditions | |||||||||||||
| Myocardial Infarction | 1391 | (24.9) | 716 | (19.3) | 237 | (17.5) | 99 | (15.6) | 87 | (13.4) | <0.001 | 2530 | (21.2) |
| Diabetes Mellitus | 1727 | (30.9) | 935 | (25.2) | 239 | (17.7) | 104 | (16.4) | 96 | (14.8) | <0.001 | 3101 | (26.0) |
| Stroke | 914 | (16.4) | 406 | (11.0) | 119 | (8.8) | 55 | (8.7) | 61 | (9.4) | <0.001 | 1555 | (13.0) |
| Cancer | 699 | (12.5) | 390 | (10.5) | 142 | (10.5) | 59 | (9.3) | 46 | (7.1) | <0.001 | 1336 | (11.2) |
| Congestive Heart Failure | 657 | (11.8) | 307 | (8.3) | 93 | (6.9) | 40 | (6.3) | 35 | (5.4) | <0.001 | 1132 | (9.5) |
| Chronic Lung Disease | 1254 | (22.5) | 661 | (17.8) | 261 | (19.3) | 132 | (20.8) | 166 | (25.5) | <0.001 | 2474 | (20.7) |
| Pneumonia | 871 | (15.6) | 457 | (12.3) | 140 | (10.3) | 74 | (11.7) | 72 | (11.1) | <0.001 | 1614 | (13.5) |
Note.
Ascertainment of characteristics was not available for all patients. Therefore, the Ns differ across characteristics.
Based on Chi-square test
Mental Health Inventory – 5 (MHI-5) ≥ 17 – positive depression screen 23
Unadjusted prevalences of each cardiovascular health behavior outcome, overall and across alcohol use groups, are presented in Table 2. A majority of patients reported not smoking (78%), avoiding salt (62%), and controlling their weight (55%) while only one-third of patients reported exercise (33%); less than one-sixth (15%) reported all four behaviors. Significant differences in all cardiovascular health behaviors were observed across alcohol use groups with the unadjusted prevalence of each cardiovascular health behavior generally decreasing with each increase in level of alcohol use, with the exception of exercise, in which the unadjusted prevalence was highest in patients with low level alcohol use and mild alcohol misuse (Table 2).
Table 2. Unadjusted Prevalence of Each Outcome: Overall and across Alcohol Use and Misuse Groups* (n=11,927).
| No Alcohol Use AUDIT-C 0 points (n=5585; 46.8%) | Low-level Use AUDIT-C 1-3 points (n=3705; 31.0%) | Mild Misuse AUDIT-C 4-5 points (n=1353; 11.3%) | Moderate Misuse AUDIT-C 6-7 points (n=634; 5.3%) | Severe Misuse AUDIT-C 8-12 points (n=650; 5.4%) | Total (n=11927) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | p† | n | (%) | |
| Avoids Salt | 3633 | (65.4) | 2288 | (62.0) | 809 | (60.2) | 322 | (51.0) | 284 | (43.8) | <0.001 | 7336 | (61.8) |
| Exercises | 1738 | (31.9) | 1233 | (34.0) | 513 | (38.9) | 182 | (29.3) | 148 | (23.5) | <0.001 | 3814 | (32.7) |
| Controls Weight | 3250 | (59.1) | 1981 | (54.2) | 717 | (53.8) | 309 | (49.5) | 259 | (40.3) | <0.001 | 6516 | (55.4) |
| Does not Smoke | 4593 | (82.9) | 3004 | (81.6) | 996 | (74.1) | 363 | (57.4) | 320 | (49.7) | <0.001 | 9276 | (78.3) |
| Composite: All 4 Health Behaviors | 936 | (16.8) | 606 | (16.4) | 230 | (17.0) | 53 | (8.4) | 33 | (5.1) | <0.001 | 1858 | (15.6) |
The adjusted prevalences of each cardiovascular health behavior, and the composite of all four, are presented in Figure 1 across alcohol use levels. Increasing level of alcohol use was associated with decreasing prevalence of avoiding salt, controlling weight, not smoking, and reporting all four cardiovascular health behaviors (p-values for linear trend all <0.001). A linear trend was not observed for exercise (p=0.83), which, in adjusted results, was most common among patients with mild alcohol misuse (p=0.01 relative to non-drinking).
Figure 1.
Proportion of patients self-reporting engagement in cardiovascular health behaviors across alcohol use and misuse groups. (n=11,927)
Note. Wald tests for linear trend were significant (p<0.001) for all outcomes except exercises, which was not (p=0.83).
Discussion
This study indicates that self-report of three of the four cardiovascular health behaviors—avoiding salt, controlling weight and not smoking—decreased as alcohol use increased among male VA outpatients with hypertension. The proportion of patients who reported avoiding salt, controlling weight, and not smoking were 12% to 20% lower in those with the highest alcohol use compared with those who reported no alcohol use. Although increasing alcohol use is associated with decreased self-care in patients with diabetes,14,15 and decreased medication adherence in patients with hypertension,13 no previous study to our knowledge has described the association between increasing alcohol use and cardiovascular health behaviors in patients with hypertension.
Results of this study have several implications for clinicians. Some previous studies have shown significantly greater declines in blood pressure among patients who receive brief alcohol intervention,27-29 while others have not.30 This study shows that increasing levels of alcohol use and misuse are associated with poorer hypertension self-care. Brief alcohol counseling interventions have efficacy for reducing drinking in primary care patients with alcohol misuse,31,32 and prior studies have shown that hypertensive patients benefit from brief alcohol interventions.33,34 If the association between alcohol use and other self-care behaviors is causal (e.g. intoxication leads to poorer adherence), brief alcohol interventions may improve adherence to other recommended cardiovascular health behaviors independent of direct effects of lower alcohol consumption on blood pressure.35,36 Further research is needed to evaluate this.
Several limitations of this study should be noted. First, study data were collected between 1997 and 1999. While associations between alcohol use and cardiovascular health behaviors may have changed over time, we are not aware of any study that describes these changes. However, future research could replicate these findings given that healthcare systems are increasingly implementing the AUDIT-C into routine practice. Another limitation is the use of self-reported measures, which could introduce both social desirability and recall bias. In particular, social desirability bias is likely present in measures of alcohol use. Additionally, due to the past-year time frame of the AUDIT-C questionnaire, the non-drinkers captured both lifetime abstainers and former drinkers, including patients who may have stopped drinking due to chronic medical conditions. Inclusion of these patients in the reference group may have biased results to the null. Generalizability of findings is limited to men, and potentially to VA populations, although the age distribution of hypertensive patients in this study was consistent with other populations37 with a majority of patients over sixty years of age. Generalizability may also be limited by response bias.38 Finally, this cross-sectional study cannot address causality between alcohol use and cardiovascular health behaviors.
Despite these limitations, this is the first study to our knowledge to assess the association between increasing levels of alcohol use and self-report of cardiovascular health behaviors in outpatients with hypertension. Results should encourage clinicians to routinely screen for alcohol misuse in hypertensive patients and, when patients screen positive, address other cardiovascular self-care behaviors in addition to offering brief alcohol interventions.
Acknowledgments
Funding: This work was funded by VA HSR&D IIR Grant #IAC 05-206-1 and conducted with support from VA Health Services Research and Development and VA Center of Excellence for Substance Abuse Treatment and Education. The VA Ambulatory Care Quality Improvement Project (ACQUIP) was funded by VA HSR&D Grants #SDR96-002 and IIR99-376. Dr. Williams is supported by a Career Development Award from VA Health Services Research & Development (CDA 12-276) and is an investigator with the Implementation Research Institute (IRI) at the George Warren Brown School of Social Work at Washington University in St. Louis. IRI is supported through an award from the National Institute of Mental Health (R25 MH080916-01A2) and the Department of Veterans Affairs, Health Services Research & Development Service, Quality Enhancement Research Initiative (QUERI). Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the University of Washington, or Group Health Research Institute.
Footnotes
A portion of this work was presented at the 2007 Association for Medical Education and Research in Substance Abuse Annual Meeting in Washington, DC as an invited presentation.
The authors declare that they have no competing interests
Author Contributions: KB, EW, and CB contributed to the study design and execution. HS and EW conducted data analyses. All authors interpreted the data. SR and MF co-wrote iterative drafts of the manuscript. All authors read, contributed to and approved the final manuscript.
References
- 1.National Center for Health Statistics. Deaths-Leading Causes. [accessed May 17, 2007];2007 http://www.cdc.gov/nchs/fastats/lcod.htm.
- 2.MMWR. Vital Signs: Prevalence, Treatment, and Control of Hypertension --- United States, 1999--2002 and 2005--2008. Morb Mortal Wkly Rep. 2011 Feb 4;60(04):103–108. [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much: A Clinicians Guide. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. NIH Publication No. 07–3769. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vital Signs: Prevalence, Treatment, and Control of Hypertension --- United States, 1999--2002 and 2005--2008. Morb Mortal Wkly Rep. 2011 Feb 24;60(4):103–108. [PubMed] [Google Scholar]
- 5.Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung HC. Deaths: Preliminary Data for 2009. National Vital Statistics Reports. 2011 Mar 16;59(4) 2011. [PubMed] [Google Scholar]
- 6.Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24(2) doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services, National Institutes of Health, National Heart Lung and Blood Institute. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. 2004 Aug; 2004. [PubMed] [Google Scholar]
- 8.Stranges S, Wu T, Dorn JM, et al. Relationship of alcohol drinking pattern to risk of hypertension: a population-based study. Hypertension. 2004 Dec;44(6):813–819. doi: 10.1161/01.HYP.0000146537.03103.f2. [DOI] [PubMed] [Google Scholar]
- 9.Klatsky AL. Alcohol-associated hypertension: when one drinks makes a difference. Hypertension. 2004 Dec;44(6):805–806. doi: 10.1161/01.HYP.0000146538.26193.60. [DOI] [PubMed] [Google Scholar]
- 10.Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012 Nov;14(11):792–798. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005 Feb 10;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 12.Klatsky AL, Gunderson E. Alcohol and hypertension: a review. J American Soc Hypertension : JASH. 2008 Sep-Oct;2(5):307–317. doi: 10.1016/j.jash.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008 Dec 2;149(11):795–804. doi: 10.7326/0003-4819-149-11-200812020-00004. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed AT, Karter AJ, Liu J. Alcohol consumption is inversely associated with adherence to diabetes self-care behaviours. Diabet Med. 2006;23(7):795–802. doi: 10.1111/j.1464-5491.2006.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas RM, Francis GPA, Williams EC, et al. Association between alcohol screening scores and diabetic self-care behaviors. Fam Med. 2012;44(8):555–563. [PubMed] [Google Scholar]
- 16.Barrett DH, Anda RF, Croft JB, Serdula MK, Lane MJ. The association between alcohol use and health behaviors related to the risk of cardiovascular disease: the South Carolina Cardiovascular Disease Prevention Project. J Stud Alcohol. 1995 Jan;56(1):9–15. doi: 10.15288/jsa.1995.56.9. [DOI] [PubMed] [Google Scholar]
- 17.Kim MT, Dennison CR, Hill MN, Bone LR, Levine DM. Relationship of alcohol and illicit drug use with high blood pressure care and control among urban hypertensive Black men. Ethn Dis. 2000 Spring-Summer;10(2):175–183. [PubMed] [Google Scholar]
- 18.Fihn SD, McDonell MB, Diehr P, et al. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004 Feb 15;116(4):241–248. doi: 10.1016/j.amjmed.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 19.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998 Sep 14;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 20.Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013 Aug;37(8):1380–1390. doi: 10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- 21.Rubinsky AD, Kivlahan DR, Volk RJ, Maynard C, Bradley KA. Estimating risk of alcohol dependence using alcohol screening scores. Drug AlcDepend. 2010 Apr 1;108(1-2):29–36. doi: 10.1016/j.drugalcdep.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greene CC, Bradley KA, Bryson CL, et al. The association between alcohol consumption and risk of COPD exacerbation in a veteran population. Chest. 2008 Oct;134(4):761–767. doi: 10.1378/chest.07-3081. [DOI] [PubMed] [Google Scholar]
- 23.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991 Feb;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Fan VS, Au D, Heagerty P, Deyo RA, McDonell MB, Fihn SD. Validation of case-mix measures derived from self-reports of diagnoses and health. J Clin Epidemiol. 2002 Apr;55(4):371–380. doi: 10.1016/s0895-4356(01)00493-0. [DOI] [PubMed] [Google Scholar]
- 25.Fan VS, Maciejewski ML, Liu CF, McDonell MB, Fihn SD. Comparison of risk adjustment measures based on self-report, administrative data, and pharmacy records to predict clinical outcomes. Health Serv Outcomes Res Method. 2006;6:21–36. [Google Scholar]
- 26.Wald A. Tests of statistical hypotheses concerning several parameters when the number of observations is large. TransAmerican MathSoc. 1943;54(3):426–482. [Google Scholar]
- 27.Rose HL, Miller PM, Nemeth LS, et al. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Addiction. 2008 Aug;103(8):1271–1280. doi: 10.1111/j.1360-0443.2008.02199.x. [DOI] [PubMed] [Google Scholar]
- 28.Maheswaran R, Beevers M, Beevers DG. Effectiveness of advice to reduce alcohol consumption in hypertensive patients. Hypertension. 1992;19:79–84. doi: 10.1161/01.hyp.19.1.79. [DOI] [PubMed] [Google Scholar]
- 29.Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–668. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cushman WC, Cutler JA, Hanna E, et al. Prevention and Treatment of Hypertension Study (PATHS): effects of an alcohol treatment program on blood pressure. ArchIntern Med. 1998 Jun 8;158(11):1197–1207. doi: 10.1001/archinte.158.11.1197. [DOI] [PubMed] [Google Scholar]
- 31.Moyer VA. Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013 May 14; doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- 32.Jonas DE, Garbutt JC, Amick HR, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2012 Nov 6;157(9):645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- 33.Miller PM, Anton RF, Egan BM, Basile J, Nguyen SA. Excessive Alcohol Consumption and Hypertension: Clinical Implications of Current Research. J Clin Hypertension. 2005;7(6):346–351. doi: 10.1111/j.1524-6175.2004.04463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fleming M, Brown R, Brown D. The efficacy of a brief alcohol intervention combined with %CDT feedback in patients being treated for type 2 diabetes and/or hypertension. J Stud Alcohol. 2004 Sep;65(5):631–637. doi: 10.15288/jsa.2004.65.631. [DOI] [PubMed] [Google Scholar]
- 35.McFadden CB, Brensinger CM, Berlin JA, Townsend RR. Systematic review of the effect of daily alcohol intake on blood pressure. Am J Hypertens. 2005 Feb;18(2 Pt 1):276–286. doi: 10.1016/j.amjhyper.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 36.Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of Alcohol Reduction on Blood Pressure: A Meta-Analysis of Randomized Controlled Trials. Hypertension. 2001;38:1112–1117. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 37.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003 Jul 9;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 38.Bradley KA, Bush KR, McDonell MB, Malone T, Fihn SD. Screening for problem drinking: comparison of CAGE and AUDIT. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. J Gen Intern Med. 1998 Jun;13(6):379–388. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]