Abstract
Background and Objectives:
No criteria define indications for laparoscopic splenectomy in trauma. This investigation compared characteristics of trauma patients and outcomes between laparoscopic and open splenectomies.
Methods:
Patients were identified retrospectively by using ICD-9 codes. Included patients were 18 or older, with a blunt splenic injury from January 1, 2011, through December 31, 2014, and required splenectomy. Excluded patients had penetrating trauma, successful nonoperative management, or successful embolization. Variables included demographics, presenting characteristics, injury severity scores, abdominal abbreviated injury scores, splenic injury grade, surgical indication and approach (open or laparoscopic), surgery length, intra-operative blood loss, transfusions, length of stay, complications, mortality, and discharge disposition.
Results:
Forty-one patients underwent open splenectomy, and 11 underwent laparoscopic splenectomy. The mean age was 48.7 years, and men comprised the sample majority (36/52). The groups were well matched for age, abdominal injury scores, and admission vital signs. The open group had a significantly lower level of consciousness and more acidosis compared with the laparoscopic group. Most laparoscopic splenectomies were performed after failed nonoperative management or embolization. The indications for open splenectomy were a positive focused assessment with sonography for trauma and computed tomography results. Laparoscopic patients had significantly longer times between presentation and surgery and longer operations, but had significantly less blood loss and fewer transfusions compared with the open group. There were no differences in mortality, length of stay, complications, or discharge dispositions.
Conclusion:
Laparoscopic splenectomy is useful in patients with blunt trauma in whom conservative management produced no improvement and who do not have other injuries to preclude laparoscopy.
Keywords: laparoscopic surgery, laparotomy, nonpenetrating wounds, splenectomy, trauma
INTRODUCTION
Splenic conservation is considered the gold standard for the management of splenic injuries in the hemodynamically stable patient. According to the Eastern Association for the Surgery of Trauma (EAST) 2013 splenic trauma practice management guidelines (PMGs), patients with diffuse peritonitis or hemodynamic instability after blunt abdominal trauma should be taken urgently for laparotomy. However, in the EAST PMGs, there are no criteria defining indications for laparoscopic treatment of splenic injuries, especially for high-grade injuries.1 Nonoperative management of blunt splenic injuries has been reported to fail in 11 to 38% of adults.2,3
Laparoscopy is an integral part of general surgery training and should have an increased role in managing the acutely injured patient.4–6 It is considered the standard approach for most nontraumatic or elective splenectomies.7 As with laparoscopic cholecystectomy8 and antireflux surgery,9 laparoscopic splenectomy offers important advantages over an open approach such as reduced blood loss, less postoperative pain, improved pulmonary function, quicker recovery, and earlier hospital discharge.7–10 For more than 20 years, laparoscopic splenectomies in trauma patients have been described mostly in case reports or case series.4–6,11–13 However, the laparoscopic approach requires further investigation, because its role in trauma remains poorly defined.
This study had two goals: (1) to examine trauma patients who underwent laparoscopic splenectomy and compare their characteristics and outcomes to those of patients who underwent open splenectomy and (2) to define characteristics of trauma patients who are candidates for the laparoscopic approach.
METHODS
This was a retrospective chart review at an American College of Surgeons–accredited Level I Trauma Center, approved by the Mercy Health Youngstown Institutional Review Board. Patients were identified via a medical records request, using the primary or secondary splenic injury diagnosis ICD-9 codes 865.00, 865.01, 865.02, 865.03, 865.04, and 865.09. The patients' abdominal Abbreviated Injury Score (AIS) and Injury Severity Scores (ISS) were obtained from the Trauma Registry. Patients were included if they were 18 years of age or older, sustained a blunt splenic injury from January 1, 2011, through December 31, 2014, and underwent a splenectomy. Patients with penetrating trauma, nontraumatic splenic injuries (splenomegaly, iatrogenic, or elective), successful nonoperative splenic injury management, or successful embolization were excluded.
Variables of interest in this study included demographics (age, gender, and mechanism of injury [MOI]), presenting characteristics: admission systolic blood pressure (SBP), heart rate (HR), base excess (BE), and Glasgow Coma Scale (GCS), ISS, abdominal AIS, splenic injury grade per the American Association for the Surgery of Trauma (AAST) organ injury scale10 indication for splenectomy, surgical approach (open or laparoscopic), time from hospital arrival to surgery (in days), intra-operative blood loss in milliliters, blood transfusions in total units transfused, length of operation in minutes, ventilator days, days in the intensive care unit (ICU) and in hospital, postoperative complications related to splenectomy, mortality, and discharge disposition.
The primary outcome measure was mortality. Secondary outcome measures were discharge disposition, days on mechanical ventilation, ICU and hospital length of stay (LOS). Discharge dispositions were grouped by implied level of function. Patients at home and in acute rehabilitation were considered mostly independent; those in skilled nursing facilities (SNF) and long-term acute care facilities (LTAC) were considered dependent on others; and those in hospice were grouped with those who did not survive because they were moribund. For ease of analysis, MOI was placed in 3 categories: vehicular (motor vehicle, motorcycle, and bicycle crashes), falls, and other (crushing, pedestrian, assault, and sports).
Data were entered into Excel 2013 (Microsoft Corporation, Redmond, Washington, USA) and transferred to SPSS Statistics 22.0 (IBM Corporation, Armonk, New York, USA) for analysis. Chi-square test, Mann-Whitney U test, and descriptive statistics were analyzed. Statistical significance was established with an α of 0.05 for all comparisons.
RESULTS
One hundred ninety-nine charts with an ICD-9 code for splenic injury were reviewed. One hundred forty-seven charts did not fit the inclusion and exclusion criteria. Fifty-two patients underwent splenectomy and were included. Forty-one patients underwent open splenectomy and 11 underwent laparoscopic splenectomy. The mean age was 48.7 years, with men accounting for 69.2% (36/52) of the sample. The most common mechanism of injury was motor vehicle crash (61.4%). Between the 2 groups, there was no significant difference in age, SBP, HR, abdominal AIS, and AAST splenic injury grade. However, the open group had a significantly lower presenting GCS and BE compared to the laparoscopic group. The ISS of the open group was numerically higher, approaching significance; but both groups were considered to have multiple injuries, with an ISS greater than 15. The average splenic injury grade was 3.72 in 43 patients who had organ grading. None of the surgeries in the laparoscopy group was converted to an open approach (Table 1).
Table 1.
Presenting Characteristics by Splenectomy Technique
| Laparoscopic (n = 11) | Open (n = 41) | Statistic | Significance | |
|---|---|---|---|---|
| Sex, n (%)* | P = .235 | |||
| Male | 6 (54.5) | 30 (73.2) | χ2 = 1.41 | |
| Female | 5 (45.5) | 11 (26.8) | ||
| MOI, n (%)* | P = .463 | |||
| Vehicular | 6 (54.5) | 28 (68.3) | χ2 = 1.54 | |
| Fall | 2 (18.2) | 8 (19.5) | ||
| Other | 3 (27.3) | 5 (12.2) |
| Means | ||||
|---|---|---|---|---|
| Age (years)** | 47.18 | 49.10 | U = 204.0 | P = .630 |
| Systolic BP (mm Hg)** | 121.73 | 108.02 | U = 185.5 | P = .370 |
| Heart rate (bpm)** | 90.36 | 96.15 | U = 185.5 | P = .370 |
| Base Excess (mmol/L)** | −2.78 | −5.47 | U = 102.0 | P = .021 |
| GCS** | 15.00 | 13.05 | U = 143.0 | P = .025 |
| ISS** | 21.64 | 28.60 | U = 142.0 | P = .073 |
| Abdominal AIS** | 3.36 | 3.75 | U = 159.5 | P = .139 |
| AAST Grading** | 3.44 | 3.79 | U = 123.5 | P = .385 |
Mechanism of Injury (MOI), Blood Pressure (BP), mmHg (millimeters of mercury); bpm (beats per minute); mmol/L (millimoles per liter); Glasgow Coma Scale (GCS), Injury Severity Score (ISS), Abbreviated Injury Score (AIS), American Association for the Surgery of Trauma (AAST).
Chi-square
Mann-Whitney U test
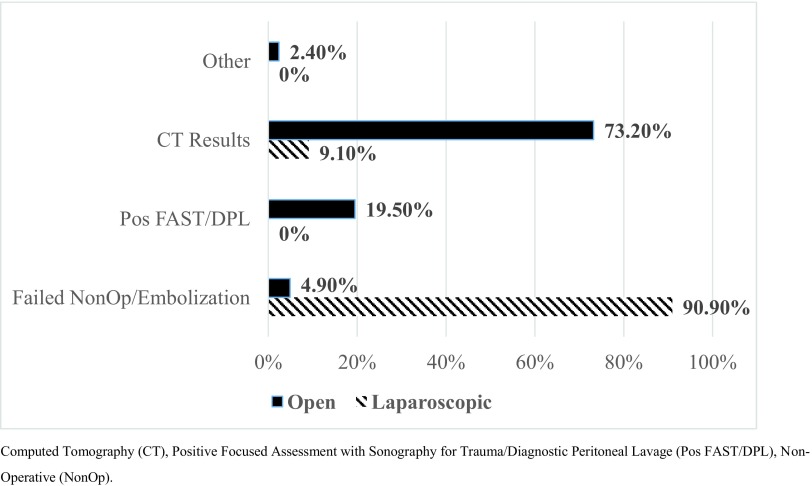
The indications for surgery in both groups are detailed in Figure 1. Most laparoscopic splenectomies were performed after nonoperative management or embolization were unsuccessful. The most common indications for open splenectomy were a positive focused assessment with sonography for trauma (FAST) or diagnostic peritoneal lavage (DPL) and positive computed tomography results (blush, rupture, and high organ injury grade).
Figure 1.
Surgical indication comparison.
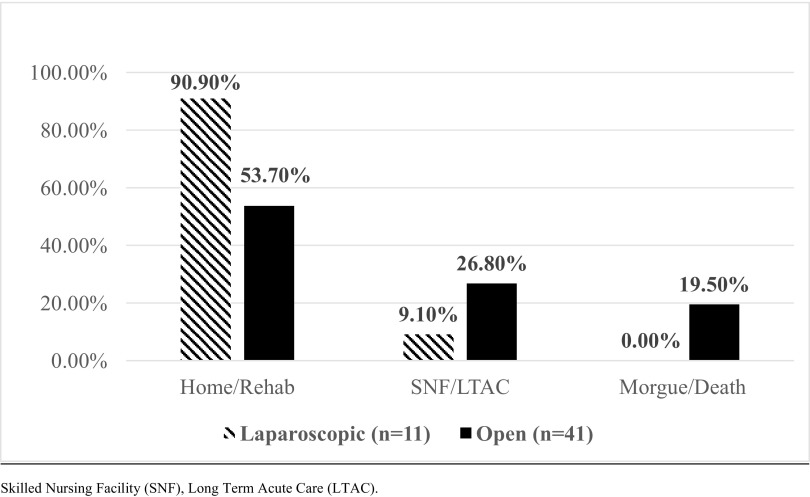
Patients with laparoscopic splenectomy patients (mean = 3.18 days) had a longer time from hospital arrival to surgery versus those who had open surgery (mean = 0.27 d, range, 0–5 days) (mean rank, 22.38 and 41.86, respectively; P < .001). Most open patients (87.8%, n = 36) had surgery on the day of presentation. During surgery, the laparoscopic group had significantly less blood loss, required fewer blood transfusions, but had longer operating times. Patients with laparoscopy also had significantly fewer days on the ventilator. The difference in ICU and hospital days did not reach statistical significance; however, with 5.6 fewer ICU days and 1.9 fewer hospital days the laparoscopic technique was favored over open (Table 2). There was no difference in mortality (19.5%, n = 8 of open, 0%, n = 0 of laparoscopic; P = .111) or complications (24.4%, n = 10 of open, 9.1%, n = 1 of laparoscopic; P = .270) between the groups (Table 2). There was a trend that favored discharge of patients who had laparoscopic surgery to home or acute rehabilitation over SNF or LTAC (P = .071; Figure 2).
Table 2.
Comparison of Splenectomy Outcomes by Operative Technique
| Laparoscopic (n = 11) | Open (n = 41) | Statistic | Significance | |
|---|---|---|---|---|
| Mortality, n (%)* | 0 (0%) | 8 (19.5%) | χ2 = 2.54 | p = 0.111 |
| Complications, n (%)* | 1 (9.1%) | 1 (9.1%) | χ2 = 1.22 | p = 0.270 |
| Means | ||||
|---|---|---|---|---|
| Blood Loss (mL**) | 273.18 | 2297.23 | U = 34.0 | P < .001 |
| Transfusion (units)** | 2.64 | 11.22 | U = 110.5 | P = .010 |
| OR Time (min)** | 171.18 | 127.30 | U = 67.5 | P < .001 |
| Ventilator Days** | 0.09 | 6.61 | U = 92.0 | P = .001 |
| ICU Days** | 2.91 | 8.46 | U = 162.0 | P = .152 |
| Hospital Days** | 9.64 | 11.54 | U = 203.5 | P = .622 |
Milliliters (mL), minutes (min), Operation Room (OR), Intensive Care Unit (ICU).
Chi-square
Mann-Whitney U test
Figure 2.
Discharge disposition of patients with laparoscopic versus open splenectomy (P = .071).
DISCUSSION
Laparoscopic partial and total splenectomies in trauma patients were initially described as case reports in 1995 and 2003.4,13 Huscher et al5 reported 11 patients undergoing laparoscopic splenectomy for blunt trauma in 2006 and concluded that the approach is feasible and safe. Carobbi et al6 described another series of 10 patients undergoing laparoscopic splenectomy in 2009 with “fast hemostatic technique.” Ransom and Kavic11 described performing laparoscopic splenectomy in 11 patients in whom splenic embolization failed. These 3 papers clearly demonstrated the feasibility of using laparoscopic splenectomy in trauma.
In this study, we sought to compare laparoscopic with open splenectomy in high-grade splenic injuries. According to the AAST criteria, our overall splenic grade approached IV.14 Ermolov et al12 reported a large study in 2015, comparing 23 laparoscopic splenectomies and 19 open splenectomies for grade III lacerations. The results showed longer operating times in the laparoscopic group, but no difference in complications or mortality, which is similar to the current investigation. A study with a smaller sample reviewed 11 hemodynamically stable, emergent laparoscopic splenectomies in grade III injuries.5 The results demonstrated low morbidity and no deaths, suggesting that, in this population, laparoscopic splenectomy may be a safe alternative compared with open laparotomy.
The results of the current investigation showed less blood loss and longer operating room times with the laparoscopy group. The longer operating times could be associated with the setup of the laparoscopic equipment, as well as technique-related difficulties: intra-abdominal blood obstructing visualization and morselizing the spleen. Although there were no conversions to open surgery, laparoscopic splenectomy remains technically demanding. The first author, along with another trauma surgeon, skilled in advanced laparoscopy, performed all 11 laparoscopic splenectomies in this sample. The other trauma surgeons at the institution perform only open splenectomies. Laparoscopic surgery should not be performed in any hemodynamically unstable patient, because pneumoperitoneum affects cardiac output.
Most laparoscopic splenectomies were performed later than the open procedures without a significant difference in vital signs. Patients who present with hemodynamic instability or become unstable during the initial evaluation and have a positive FAST/DPL undergo an emergent open exploration, whereas the hemodynamically stable patient, free of peritonitis, is treated with nonoperative management. Patients with spleen injuries in whom nonoperative management or embolization has not been successful appear to be good candidates for laparoscopic splenectomies.
Both groups of patients were severely injured (ISS > 15). The greater ISS in the open group approached significance (P = .07), suggesting that the patients in the open group had greater body injury than those in the laparoscopic group. ISS is the sum of the 3 highest AIS scores, squared. In addition, the AIS of both the laparoscopic and open groups were statistically similar (3.36 vs 3.76) which suggests that the intra-abdominal injuries were not different. Based on the ISS of both groups, the open and laparoscopic groups were critically ill, with significant injury burden—another confounding variable, as these were not isolated splenic injuries.
From the current analysis, characteristics of successful laparoscopic splenectomy in the setting of polytrauma include a normal SBP, grade III or IV splenic injury, and BE higher than −3.0. No grade V shattered spleens were removed laparoscopically. A surgeon's technical skill is another factor that influences the decision to proceed with laparoscopy.
One limitation of this study is the small sample size, which likely contributed to the lack of statistical significance in mortality between the 2 groups, because laparoscopic splenectomy for trauma is not performed frequently. Zafar and colleagues10 reviewed the National Trauma Data Bank between 2007 and 2010 and noted 4,755 diagnostic laparoscopies at 467 centers and splenectomy occurring in only 48 patients. These data average to 16 laparoscopic trauma splenectomies per year across all trauma centers. The current study's facility had 52 splenic injuries requiring surgical intervention with 11 undergoing laparoscopic approach in the same time frame, which appears higher than the national rate.
Future directions for research include conducting a meta-analysis of the published literature to obtain a larger sample size. A well designed, ethically sound randomized, multicenter trial in hemodynamically stable patients in whom nonoperative or embolization has failed is warranted. A larger sample size would allow better identification of characteristics of those patients who are ideal for laparoscopic splenectomy.
CONCLUSION
Laparoscopic splenectomy for blunt trauma appears beneficial compared to open splenectomy, even in the patient with a high injury grade. It appears safe and effective in hemodynamically stable patients in whom initial nonoperative management or embolization fails. There may be other factors that influence the decision to proceed laparoscopically; therefore, more research is needed.
Contributor Information
Gregory S. Huang, Trauma and Critical Care Services, St Elizabeth Youngstown Hospital, Youngstown, Ohio, USA..
Elisha A. Chance, Trauma and Critical Care Services, St Elizabeth Youngstown Hospital, Youngstown, Ohio, USA..
Barbara M. Hileman, Trauma and Critical Care Services, St Elizabeth Youngstown Hospital, Youngstown, Ohio, USA..
Eric S. Emerick, Department of Sociology, Anthropology, and Gerontology, Youngstown State University, Youngstown, Ohio, USA..
Emily A. Gianetti, Department of Medical Education, Northeast Ohio Medical University, Rootstown, Ohio, USA..
References:
- 1. Stassen NA, Bhullar I, Cheng JD, et al. Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S294–S300. [DOI] [PubMed] [Google Scholar]
- 2. Velmahos GC, Zacharias N, Emhoff TA, et al. Management of the most severely injured spleen: a multicenter study of the Research Consortium of New England Centers for Trauma (ReCONECT). Arch Surg. 2010; May 145:456–460. [DOI] [PubMed] [Google Scholar]
- 3. Harbrecht BG, Ko SH, Watson GA, Forsythe RM, Rosengart MR, Peitzman AB. Angiography for blunt splenic trauma does not improve the success rate of nonoperative management. J Trauma. 2007;63:44–49. [DOI] [PubMed] [Google Scholar]
- 4. Poulin EC, Thibault C, DesCôteaux JG, Côté G. Partial laparoscopic splenectomy for trauma: technique and case report. Surg Laparosc Endosc. 1995;5:306–310. [PubMed] [Google Scholar]
- 5. Huscher CG, Mingoli A, Sgarzini G, Brachini G, Ponzano C, Di Paola M. Laparoscopic treatment of blunt splenic injuries: initial experience with 11 patients. Surg Endosc. 2006;20:1423–1426. [DOI] [PubMed] [Google Scholar]
- 6. Carobbi A, Romangnani F, Antonelli G, Bianchini M. Laparoscopic splenectomy for severe blunt trauma: initial experience of ten consecutive cases with a fast hemostatic technique. Surg Endosc. 2010;24:1325–1330. [DOI] [PubMed] [Google Scholar]
- 7. Habermalz B, Sauerland S, Decker G, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2008;22:821–848. [DOI] [PubMed] [Google Scholar]
- 8. Schulze S, Thorup J. Pulmonary function, pain, and fatigue after laparoscopic cholecystectomy. Eur J Surg. 1993;159:361–364. [PubMed] [Google Scholar]
- 9. Hinder R, Filipi CJ, Wetscher G, Neary P, de Meester TR, Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994;220:472–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zafar S, Onwugbufor M, Hughes K, et al. Laparoscopic surgery for trauma: the realm of therapeutic management. Am J Surg. 2015;209:627–632. [DOI] [PubMed] [Google Scholar]
- 11. Ransom KJ, Kavic MS. Laparoscopic splenectomy for blunt trauma: a safe operation following embolization. Surg Endosc. 2009;23:352–355. [DOI] [PubMed] [Google Scholar]
- 12. Ermolov AS, Tlibekova MA, Yartsev PA, et al. Laparoscopic splenectomy in patients with spleen injuries. Surg Laparosc Endosc Percutan Tech. 2015;25:483–486. [DOI] [PubMed] [Google Scholar]
- 13. Basso N, Silecchia G, Raparelli L, Pizzuto G, Picconi T. Laparoscopic splenectomy for ruptured spleen: lesson learned from a case. J Laparosc Adv Surg Tech. 2003;13:109–112. [DOI] [PubMed] [Google Scholar]
- 14. Moore EE, Cogbill TH, Jurkovich GJ, et al. Organ injury scaling, V: spleen and liver (1994 revision). J Trauma. 1995;38:323–324. [DOI] [PubMed] [Google Scholar]