Abstract
Background
Adhesive capsulitis is a common cause of stiff shoulder and may result in pain and restriction of movement. The study aimed to investigate the role of hydrodilatation of the glenohumeral joint in the management of adhesive capsulitis.
Methods
Patients referred from the shoulder clinic underwent hydrodilatation under ultrasound guidance. Of 209 referred for hydrodilatation, 163 underwent the procedure and attended follow-up physiotherapy. Outcome measures were available for 118 patients (58 men and 60 women). Mean age of the study group was 52.6 years.
Results
There was a statistically significant improvement in both Oxford Shoulder Score (OSS) and Disability Arm Shoulder Hand Scores (Quick DASH) in the first 4 weeks after the procedure, which was maintained but not improved to the end of the study period. Patients presenting with pain, those who had a history of steroid injections and older patients all had worse functional scores at presentation. Diabetes (both Type I and II), previous physiotherapy, length of history and whether pain or stiffness, or both, were the predominant symptom did not have any statistical significance at presentation. These factors were not predictors of any statistically significant improvement in functional scores.
Conclusions
Hydrodilatation results in a significant improvement of symptoms in patients with adhesive capsulitis.
Keywords: adhesive capsulitis, arthrodistension, frozen shoulder, hydrodilatation, hydrodistension
Introduction
Stiff shoulder is a common presentation to the shoulder clinic; adhesive capsulitis, (commonly referred to as frozen shoulder), is the most common cause, affecting approximately 2–5%of the population.1,2 However, later studies surmise that the real incidence of capsular contracture is about 0.75% of the population as described by Bunker.3 The condition is characterized by a thickening and contracture of the capsule akin to Dupuytren’s contracture of the hand.3
Night pain with a reduced range of movement, particularly external rotation is one of the cardinal symptoms.4 Frozen shoulder may be idiopathic or secondary to preceding trauma. Although older studies suggested a significant female preponderance,5 more recent arthroscopic studies demonstrate a 1 : 1 male to female ratio and go on to suggest female preponderance if any is very small.3 There is a strong association with diabetes mellitus.6 The condition is usually self-limiting, typically lasting between 12 months and 36 months,7 with spontaneous resolution usually demonstrated, although some studies demonstrate up to 41% of patients had persisting symptoms associated with pain and functional loss.8,9
Three stages have been described in the past,4 although it is accepted that the course of the disease can be variable.3 Multiple treatment strategies have been suggested for the management of adhesive capsulitis, including manipulation under anaesthesia, surgical capsular release, physiotherapy regimens, intra-articular steroid injections, hydrodilatation of the glenohumeral joint (either using fluoroscopy10 or ultrasound11 guidance), or a combination of the above. Hydrodilation has been demonstrated to be more effective than physiotherapy12 and is also effective when compared with manipulation under anaesthesia.13 Arthroscopic capsular release14 is an effective method of improving symptoms but is more invasive and expensive. Recent evidence suggests steroid injection into the rotator interval may be of benefit in this group of individuals.15 Studies have suggested an improvement following hydrodilatation, usually with steroid in the injectate.16–24
Hydrodilatation distends the glenohumeral joint capsule with capsular rupture as the desired end-point. The present study illustrates our strategy for managing stiff shoulder.
Materials and Methods
Patient recruitment
Our stiff shoulder service is a multi-disciplinary team (MDT) approach between orthopaedics, physiotherapy and radiology. Ethical approval was deemed unnecessary by our institutional review board. The present study aimed to assess the efficacy of hydrodilatation of the glenohumeral joint combined with intra-articular steroid injection and followed by a prescribed course of physiotherapy.
An initial pilot study of 20 patients with primary stiff shoulder was performed. Successful clinical outcomes were noted. Our institution’s ‘New Procedures Committee’ approved the technique for clinical use as part of a prospective clinical study. Appropriate consent procedures were established.
In total, 209 patients with primary or secondary (but not postoperative), stiff shoulder were referred to the study from the shoulder clinics of the Newcastle upon Tyne teaching hospitals. The main diagnostic criterion observed was passive external rotation less than 30° along with decreased active and passive shoulder movements. These restrictions were either anatomical end point limitation or pain related limitation. Most of the patients in this group had a primary frozen shoulder, a few (six in all) had a history of trauma or being treated for previous conditions including impingement (one patient, treated conservatively), breast cancer (one patient) and lymphoma (one patient) and were therefore classed as possible secondary frozen shoulders. After the procedure, subjects were followed up in the shoulder clinics. Six patients who failed to improve with hydrodilatation were considered for other procedures where appropriate.
Patients were recruited from 2011 to 2014. Four patients with a proven full thickness rotator cuff tear were excluded because hydrodilatation is not effective in this group.
Technique
All procedures were carried out by one of two consultant musculoskeletal radiologists, with the first author performing (RS) all of the procedures in the initial pilot study.
Patients were requested to bring a family member/friend as an escort after the procedure and were also recommended not to drive postprocedure. If any patient was on anticoagulant usual departmental policy for interventional procedures was followed.
Radiographs of the shoulder were assessed to exclude osteoarthritis of the shoulder. History obtained included duration of symptoms, history of diabetes, previous steroid injections, physiotherapy, any co-existing medical condition, whether symptoms were worsening or plateaued prior to procedure, and whether pain or stiffness, or both, were the predominant symptom.
Oxford Shoulder Score (OSS) and Disabilities of the arm, shoulder and hand (Quick DASH) scores were also obtained immediately prior to the procedure. A diagnostic ultrasound of the shoulder was performed with a 9-MHz curvilinear or 12.5-MHz linear array ultrasound transducer (IU22 or Epiq 5; Philips, Eindhoven, The Netherlands) to confirm cuff integrity and exclude other causes of shoulder pain relating to the cuff, long head of biceps tendon, subacromial bursa or acromioclavicular joint. In the absence of contra-indications the patient was consented, including a discussion of potential complications.
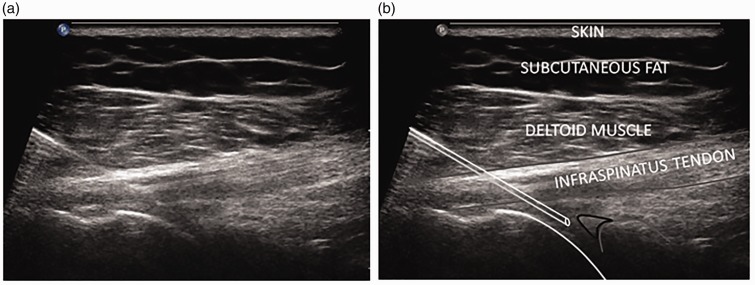
The procedure was performed in the lateral position lying on the un-affected side. The probe was placed transversely across the posterior aspect of the glenohumeral joint such that the glenoid labrum was in the middle of the screen (Figs. 1a and b). An appropriate site of puncture was marked. Using aseptic technique, 1% lidocaine was infiltrated into the skin and subcutaneous tissues. Under ultrasound guidance a 21-G needle was placed into the glenohumeral joint via a postero-oblique approach.
Figure 1.
(a) Ultrasound image showing needle tip position into the glenohumeral joint with (b) corresponding image on the right annotating various structures (humeral head outlined, glenoid outline in grey and posterior labrum in black).
Approximately 8 ml to 10 ml of lignocaine 1% was then injected into the joint followed by a mixed injectate of 80 mg of triamcinolone, 15 ml of 0.25% bupivacaine and 40 ml to 60 ml of normal saline with phasic distension to the point of rupture. If capsular rupture had not been achieved after instillation of 60 ml of normal saline, the procedure was terminated. Initial injection leads to fluid flowing into the lower third of the joint and into the inferior capsular recess. It is only when the inferior capsular recess is filled that distention starts appearing at the level of the superior capsule, with elevation of the superior capsule and with it the supraspinatus tendon, and concurrently extends into the rotator interval. Capsular rupture typically occurs at the rotator interval with fluid extending into the pericapsular soft tissues at this level. The shoulder joint has 2 areas of inherent weakness; first, the inferior capsule and, second, the rotator interval. When fluid is injected, pressure, which is force per unit area, builds up maximally at the rotator interval because of the smaller area compared to the inferior capsule, which has a much wider area. This would explain the rupture preferentially occurring at the rotator interval.
Five simple exercises aimed at increasing shoulder joint ranges of movement (flexion, abduction and rotations) were demonstrated to the patient. These were to be performed 25 times each, three times a day. Physiotherapy started the day after the procedure and continued for at least 3 months or as required and advised by the physiotherapist.
Patients completed the Quick DASH (QDASH) and the OSS scores at 4 weeks, 3 months, 6 months and 12 months postprocedure.
Results
In total, 209 patients were referred for hydrodilatation during the study period. On presentation for the procedure, 19 had improved and declined treatment, 11 patients did not attend the procedure and seven did not attend their initial physiotherapy appointment. Nine procedures were abandoned for various reasons, (Table 1). Six patients had subsequent procedures following failed hydrodilatation (Table 2).
Table 1.
Indication for abandoning/not performing a procedure.
| Indication | Number of patients |
|---|---|
| Extremely tight capsule | 1 |
| Breast carcinoma and radiotherapy | 1 |
| Cuff tear | 4 |
| Syncope prior to procedure | 1 |
| Cerebral bleed prior to procedure | 1 |
| Withdrawn consent | 1 |
Table 2.
Post hydrodilatation surgery.
| Surgery | Number of patients |
|---|---|
| Arthroscopic capsular release | 2 |
| Manipulation under anesthesia | 2 |
| Subacromial decompression and capsular release | 1 |
| Cervical decompression for disc prolapse | 1 |
In total, 163 patients underwent hydrodilatation, with adequate postprocedure rehabilitation and data scores (at least two sets) available in 118. Of the 46 who did not have hydrodilatation and excluding the 19 who had improved and declined treatment, two had surgery for cuff repair, seven had physiotherapy only and another 18 were lost to follow-up.
Mean age was 52.6 years (range 28 years to 73 years) (Table 3), 60 were female and 58 were male, and 26 suffered from diabetes mellitus.
Table 3.
Age distribution of the study group.
| Age group (years) | Number of patients |
|---|---|
| <20 | 0 |
| 21–30 | 2 |
| 31–40 | 2 |
| 41–50 | 31 |
| 51–60 | 59 |
| 61–70 | 21 |
| 71–80 | 3 |
Regression analysis of the pre-procedure OSS and QDASH scores (Table 4) demonstrated that older patients, those who had undergone steroid injection(s) and those who considered themselves to be in the worsening phase rather than in the plateau phase were functionally worse at the time of presentation. No statistical difference in pre-procedure scores was noted between the diabetics and nondiabetics. Patients who had received prior physiotherapy did not have a statistically different score from those who had not; the duration of symptoms pre-procedure did not correlate with the scores at time of hydrodilatation.
Table 4.
Regression analysis of pre-procedure scores.
| Estimate |
SE |
t
|
p
|
|||||
|---|---|---|---|---|---|---|---|---|
| OSS | QDASH | OSS | QDASH | OSS | QDASH | OSS | QDASH | |
| Constant | 38.66 | 16.46 | 6.57 | 12.68 | 5.89 | 1.30 | 0.00 | 0.20 |
| Diabetes (y = 1) | 1.77 | −1.48 | 2.38 | 4.59 | 0.74 | −0.32 | 0.46 | 0.75 |
| Physio (y = 1) | −1.33 | 2.37 | 2.41 | 4.65 | −0.55 | 0.51 | 0.58 | 0.61 |
| Pain/stiffness/both (p = 1) | 0.42 | −3.83 | 1.74 | 3.34 | 0.24 | −1.15 | 0.81 | 0.25 |
| Plateau/worse (w = 1) | −5.74 | 13.50 | 2.30 | 4.43 | −2.50 | 3.05 | 0.01 | 0.00 |
| Steroid > 0 | −4.41 | 9.26 | 2.16 | 4.17 | −2.04 | 2.22 | 0.04 | 0.03 |
| Age (years) | −0.22 | 0.50 | 0.11 | 0.22 | −1.97 | 2.30 | 0.05 | 0.02 |
| Symptom duration (months) | −0.02 | 0.05 | 0.07 | 0.13 | −0.31 | 0.39 | 0.76 | 0.70 |
| Adjusted r2 | 0.10 | 0.14 | ||||||
OSS, Oxford Shoulder Score; QDASH, Quick Disability Arm Shoulder Hand Scores.
A significant improvement in functional scores was demonstrated at 4 weeks postprocedure, with the OSS score increasing by 14.99 (p = 0.00) and the QDASH reducing by 26.82 (p = 0.00).
No statistical difference was observed in either score between four weeks and subsequent follow-up, (Table 5).
Table 5.
Test of mean difference of OSS and QDASH score.
| Mean |
t
|
d.f. |
p
|
|||||
|---|---|---|---|---|---|---|---|---|
| OSS | QDASH | OSS | QDASH | OSS | QDASH | OSS | QDASH | |
| Between procedure and 4 weeks | 14.99 | −26.82 | 15.75 | −15.20 | 79 | 80 | 0.00 | 0.00 |
| Between 4 weeks and 3 months | 1.02 | −3.34 | 1.36 | −2.28 | 52 | 53 | 0.18 | 0.03 |
| Between 3 and 6 months | −0.54 | 1.91 | −0.56 | 0.95 | 34 | 34 | 0.58 | 0.35 |
| Between 6 months and 1 year | 0.79 | −4.97 | 0.44 | −1.46 | 42 | 42 | 0.66 | 0.15 |
The use of italics demonstrates that the only significant consistent improvement occurs between the procedure and 4 weeks when using both OSS and QDASH scores. OSS, Oxford Shoulder Score; QDASH, Quick Disability Arm Shoulder Hand Scores.
There has been a reduction in datasets available especially in the latter stages of patient follow-up with the largest set of scores (d.f.) being available for the time period from procedure to 4 weeks [i.e. 79 (OSS) and 80 (QDASH)], which reduced for subsequent periods.
Regression analysis of the functional scores between the procedure and 4 weeks (Table 6), demonstrated significant (p = 0.04) improvement in the QDASH scores of younger patients versus older patients, with a similar but not as significant (p = 0.07) trend with the OSS scores. The other patient factors did not correlate with postprocedure scores.
Table 6.
Regression results on the difference of OSS and QDASH scores between the procedure and 4 weeks against various patient factors.
| Estimate |
SE |
t
|
p
|
|||||
|---|---|---|---|---|---|---|---|---|
| OSS | QDASH | OSS | QDASH | OSS | QDASH | OSS | QDASH | |
| Constant | 4.31 | 0.10 | 7.44 | 13.90 | 0.58 | 0.01 | 0.56 | 0.99 |
| Diabetic | −2.99 | 1.85 | 2.71 | 5.05 | −1.10 | 0.37 | 0.27 | 0.72 |
| Prior physiotherapy | −0.01 | −1.73 | 2.74 | 5.11 | 0.00 | −0.34 | 1.00 | 0.74 |
| Type of symptoms (pain/stiffness/both) | 0.19 | 3.73 | 2.02 | 3.73 | 0.10 | 1.00 | 0.92 | 0.32 |
| Stage of disease (plateau/worse) | 4.07 | −7.82 | 2.65 | 4.95 | 1.53 | −1.58 | 0.13 | 0.12 |
| Prior steroid injections | −1.10 | 2.99 | 2.41 | 4.49 | −0.46 | 0.67 | 0.65 | 0.51 |
| Age (years) | 0.24 | −0.51 | 0.13 | 0.24 | 1.87 | −2.11 | 0.07 | 0.04 |
| Symptom duration (months) | −0.11 | −0.14 | 0.14 | 0.26 | −0.76 | −0.53 | 0.45 | 0.60 |
| Adjusted R2 | 0.01 | 0.01 | ||||||
OSS, Oxford Shoulder Score; QDASH, Quick Disability Arm Shoulder Hand Scores.
Discussion
Stiff shoulder, with or without pain, is a common presenting symptom.25 It represents a socio-economic burden leading to significant work absence.26
Incidence of stiff shoulder in General Practice is approximately 2.4 per 1000 head of population per year.27 Referral to secondary care varies but UK data suggest that only 22% patients were referred during the three years from initial presentation.28
Many strategies have been described to reduce the level of pain or the duration of symptoms. We feel that the management of these patients within the current National Health Service primary care and secondary/tertiary musculoskeletal services is often fragmented. We consider that a composite MDT approach improves and hastens the treatment of the condition.
Glenohumeral osteoarthritis can mimic frozen shoulder. All stiff shoulders should therefore be X-rayed.
Referral from primary care to specialist clinics is often delayed (Table 7).
Table 7.
Referral delays for hydrodilatation.
| Duration of symptoms to hydrodilatation | Number of patients |
|---|---|
| 0–6 months | 18 |
| 7–12 months | 63 |
| 13–24 months | 28 |
| >24 months | 9 |
Regression analysis of scores at presentation suggest patients in the worsening stage were, on average, 13.5 points worse off on Quick DASH and 5.74 points worse off on OSS compared to the plateau stage. Patients who had at least one prior steroid injection had QDASH scores and OSS scores that were worse off by 9.26 points and 4.41 points, respectively. The scores also reveal that, for every additional year of age, the QDASH and OSS scores were worse by a factor of 0.5 and 0.22, respectively.
We have used ultrasound guidance in the present study because it allows confirmation of cuff integrity (allowing sufficient pressure for capsular rupture if achievable) and exclusion of alternate local pathologies.
The results of the present study demonstrate a statistically significant improvement in shoulder function and symptoms within 4 weeks of the procedure. This improvement was maintained to the end of the study period.
Given the initial results we observed for the patients with primary stiff shoulders, we subsequently performed the procedure in the later part of the study on some patients with secondary stiff shoulders. However, we do not have adequate data and consider this aspect to be part of a future study.
We consider that it is vitally important to start exercising on the day of hydrodilatation and to have a physiotherapy appointment the day after. However, we aim to assess the role of physiotherapy in a future study.
Age does not appear to be a significant predictor of response to hydrodilatation. The results demonstrated (Table 6) that, although there was some statistical significance on QDASH scores (p = 0.04), this was not mirrored in the OSS scores (p = 0.07). However, there may be an underlying trend.
There is a higher incidence of adhesive capsulitis in the diabetic population.6 The present study included 22% patients who were diabetics. There was no difference in outcome between the diabetics to the nondiabetics in our study group, which is in accordance with a previous study by Clement et al.29
There was also no statistical significance to the functional outcome in hydrodilatation patients who had previous physiotherapy, regardless of whether they recorded pain or stiffness, or both, as the predominant symptom and whether patients felt they were in the plateau or worsening stage.
Six patients required surgery posthydrodilatation. These patients are regarded as ‘failure of the procedure’. Three patients underwent an arthroscopic capsular release, two had manipulation under anaesthetic and one went on to have cervical spinal surgery. No common factors were demonstrated in this small sub-group of patients. All three participating surgeons saw a large reduction in the number of ‘stiff shoulder ‘procedures performed during the study period.
The procedure was well tolerated by all patients. Our patient group experienced few adverse events/complications of the procedure. One patient developed transient suprascapular nerve palsy because of leakage of anaesthetic into the supraglenoid notch region. Patients often feel some discomfort and sometimes feel dizzy in the first few minutes of/after the procedure. We advised our patients to be accompanied for the procedure and not to drive for the rest of the day.
Table 8 demonstrates the reduction in surgical procedures (manipulation under anaesthesia or arthroscopic capsular release) for stiff shoulder in the 4 years after the start of the study period. This represents a 78.5% reduction in surgical treatment. It also demonstrates the total number of patient appointments excluding non attendances in the time period between 2007 and 2014. Although the exact numbers of patients with a diagnosis of stiff shoulder were not available on our coding systems, the drop in surgical rates has occurred in the background of a significantly increased number of patient appointments to the upper limb clinic.
Table 8.
Surgical rates and total number of outpatient appointments in shoulder clinic pre/post study.
| Before onset of hydrodilatation service | Numbers operated for frozen shoulder (MUA or arthroscopic release) | Total number of patients seen in upper limb clinic | After start of hydrodilatation service | Numbers operated for frozen shoulder (MUA or arthroscopic release) | Total number of patients seen in upper limb clinic |
|---|---|---|---|---|---|
| 2007 | 14 | 2353 | 2011 | 3 | 3964 |
| 2008 | 18 | 2388 | 2012 | 2 | 4146 |
| 2009 | 10 | 1996 | 2013 | 3 | 4353 |
| 2010 | 14 | 3193 | 2014 | 4 | 4246 |
| Total | 56 | 9930 | Total | 12 | 16709 |
MUA, manipulation under anaesthesia.
The procedure takes 1 hour to perform in our ultrasound department, with the patient free to leave once the procedure is completed. This compares favourably to surgical procedures.
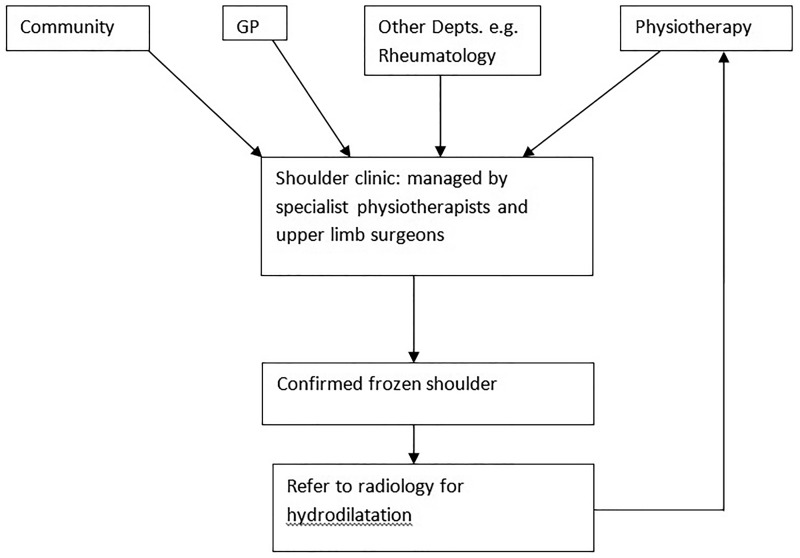
Our current management follows the algorithm shown in Fig. 2.
Figure 2.
Flow pattern for management of frozen shoulder. GP, general practitioner; Depts., departments.
A review in 2012 concluded that there was limited clinical evidence on the effectiveness of treatments for primary frozen shoulder and that the studies that have been published in this area have all suffered from small participant numbers.30 The present study demonstrates, with statistical significance, the effectiveness of hydrodilatation in a large cohort. At our institution, the estimated cost of a surgical release is £1015, whereas, for hydrodilatation, the cost is £282 in accordance with currently priced coding guidelines. This represents a saving to the trust of £733 per case.
We also acknowledge that, in 2011, the first author (RS) was the only consultant providing this service. Waiting times were almost at 3 months and this might have resulted in a proportion of the 19 patients who improved with conservative treatment declining hydrodilatation. However, by early 2012, after the first author had trained other colleagues, this waiting time had been reduced significantly to 4 weeks and take up had significantly improved.
We also propose to follow-up the present study with further follow-up studies, including studies considering steroid injection only versus hydrodilatation and hydrodilatation with and without physiotherapy input. These can be blinded and randomized to increase efficacy.
Conclusions
We have demonstrated that hydrodilatation under ultrasound guidance followed by physiotherapy is an effective management option for the stiff shoulder.
We have found that the MDT approach to the stiff shoulder has improved our management of this group of patients and markedly reduced our requirement for surgical procedures. The major aim of the present study has been to assess outcome measures following hydrodilatation. The dataset needs to be improved with larger numbers, although we consider and hope that this is at least a starting point. Anecdotally, we find a lack of follow-up with respect to assessing outcome measures, in many centres that are offering hydrodilatation.
We propose that the establishment of a ‘stiff shoulder clinic’, run by specialist physiotherapists within the consultant led shoulder clinic with rapid access to hydrodilatation, would be an effective method for managing stiff shoulder. In our unit, this has become the initial method of management of primary frozen shoulder. The reduction in surgical procedures will lead to considerable financial savings for the NHS and, at the same time, create a non-operative pathway for the management of this condition.
Article focus
A combined service for managing the stiff shoulder using orthopaedics, physiotherapy and radiology was analysed using patient scoring systems.
Key message
Hydrodilatation under ultrasound guidance is an effective treatment for the stiff shoulder.
Strengths and limitations
Hydrodilatation is a minimally invasive procedure for the management of the non-arthritic stiff shoulder.
The procedure is well tolerated.
The multi-disciplinary team (MDT), of orthopaedic surgeons, physiotherapists and radiologists functioned well in our institution.
Loss to follow-up limited the size of our trial cohort.
Acknowledgements
We thank Helen Watson (Specialist Physiotherapist; Newcastle Hospitals NHS Trust).
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The paper has not been presented at any society or meeting.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Written consent was obtained from every patient. Ethical approval was deemed not necessary by our Institutional Ethics committee.
References
- 1.Anton HA. Frozen shoulder. Can Fam Phys 1993; 39: 1773–1777. [PMC free article] [PubMed] [Google Scholar]
- 2.Lundberg B. The frozen shoulder. Acta Orthop Scand 1969; 119(Suppl): 5–59. [PubMed] [Google Scholar]
- 3.Bunker T. Time for a new name for frozen shoulder – contracture of the shoulder. Shoulder Elbow 2009; 1: 4–9. [Google Scholar]
- 4.Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ 2005; 331: 1453–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rizk TE, Pinals RS. Frozen shoulder. Semin Arthritis Rheum 1982; 11: 440–452. [DOI] [PubMed] [Google Scholar]
- 6.Bridgman JF. Periarthritis of the shoulder and diabetes mellitus. Ann Rheum Dis 1972; 31: 69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol 1975; 4: 193–196. [DOI] [PubMed] [Google Scholar]
- 8.Hand CA. Long term follow up of outcome of patients with frozen shoulder. Annual Scientific Meeting BESS 2005, Cambridge, 2005.50.
- 9.Hand C, Clipsman K, Rees J, et al. The long term outcome of frozen shoulder. J Shoulder Elbow Surg 2008; 17: 231–236. [DOI] [PubMed] [Google Scholar]
- 10.Andren L, Lundberg BJ. Treatment of rigid shoulders by joint distension during arthrography. Acta Orthop Scand 1965; 36: 45–53. [DOI] [PubMed] [Google Scholar]
- 11.Zwar RB, Read JW, Noakes JB. Sonographically guided glenohumeral joint injection. AJR Am J Roentgenol 2004; 183: 48–50. [DOI] [PubMed] [Google Scholar]
- 12.Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003; 1: CD004016–CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quraishi NA, Johnston P, Bayer J, et al. Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br 2007; 89: 1197–1200. [DOI] [PubMed] [Google Scholar]
- 14.Smith CD, Hamer P, Bunker TD. Arthroscopic capsular release for idiopathic frozen shoulder with intra-articular injection and a controlled manipulation. J Shoulder Elbow Surg 2000; 9: 23–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoong P, Duffy S, McKean D, et al. Targeted ultrasound-guided hydrodilatation via the rotator cuff interval for adhesive capsulitis. Skeletal Radiol 2015; 44: 703–708. [DOI] [PubMed] [Google Scholar]
- 16.Granville-Chapman J, et al. Long-term results of hydrodistension for frozen shoulder. Shoulder Elbow 2015; 7: 309–332. [Google Scholar]
- 17.Ekelund A, Rydell N. Combination treatment for adhesive capsulitis of the shoulder. Clin Orthop Relat Res 1992; 282: 105–109. [PubMed] [Google Scholar]
- 18.Fareed DO, Gallivan WR., Jr Office management of frozen shoulder syndrome: treatment with hydraulic distension under local anesthesia. Clin Orthop Relat Res 1989; 242: 177–183. [PubMed] [Google Scholar]
- 19.Gavant M, Rizk T, Gold R, et al. Distension arthrography in the treatment of adhesive capsulitis of the shoulder. J Vasc Intervent Radiol 1994; 5: 305–308. [DOI] [PubMed] [Google Scholar]
- 20.Loyd JA, Loyd HM. Adhesive capsulitis of the shoulder: arthrographic diagnosis and treatment. South Med J 1983; 76: 879–883. [DOI] [PubMed] [Google Scholar]
- 21.Older MWJ. Distension arthrography of the shoulder joint. In: Bayley I, Kessel L. (eds). Shoulder surgery, Berlin: Springer, 1982, pp. 123–127. [Google Scholar]
- 22.Mulcahy KA, Baxter AD, Oni OOA, et al. The value of shoulder distension arthrography with intraarticular injection of steroid and local anaesthetic: a follow-up study. Br J Rheumatol 1994; 67: 263–266. [DOI] [PubMed] [Google Scholar]
- 23.Royen B, Pavlov P. Treatment of frozen shoulder by distension and manipulation under local anaesthesia. Int Orthop 1996; 20: 207–210. [DOI] [PubMed] [Google Scholar]
- 24.Hsu SYC, Chan KM. Arthroscopic distension in the management of frozen shoulder. Int Orthop 1991; 15: 79–83. [DOI] [PubMed] [Google Scholar]
- 25.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community:the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Am Rheum Dis 1998; 557: 649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Windt D, Thomas E, Pope DP, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Env Med 2000; 57: 433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Windt DA, Koes BW, de Jong BA, et al. Shoulder disorders in general practice: incidence, patient characteristics and management. Ann Rheum Dis 1995; 54: 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006; 45: 215–221. [DOI] [PubMed] [Google Scholar]
- 29.Clement RG, et al. Frozen shoulder: long-term outcome following arthrographic distension. Acta Orthop Belg 2013; 79: 368–374. [PubMed] [Google Scholar]
- 30.Maund E, Craig D, Suekarran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess 2012; 16: 1–264. [DOI] [PMC free article] [PubMed] [Google Scholar]