Abstract
Introduction
Diet-related disease is disproportionally concentrated in low-income communities where fruit and vegetable consumption is far below guidelines. To address financial barriers, Double Up Food Bucks (DUFB)—a statewide healthy food incentive—matches Supplemental Nutrition Assistance Program (SNAP) funds spent at farmers markets. However, incentive use is limited. This study examined the impact of a brief waiting room–based intervention about DUFB on program utilization and produce consumption.
Study design
Longitudinal, repeated measures, quasi-experimental trial.
Setting/participants
SNAP—enrolled adults at a health center in a low-income, racially and ethnically diverse area of Southeast Michigan.
Intervention
Participants received a brief explanation of DUFB, written program materials, a map highlighting market locations and hours, and an initial $10 market voucher. DUFB use and produce consumption were measured through four surveys over 5 months (August 2014–January 2015).
Main outcome measures
Outcome measures included DUFB use and fruit and vegetable consumption (analyses conducted in 2015–2016).
Results
A total of 302 eligible adults were identified, and 177 (59%) enrolled. One hundred twenty-seven (72%) completed all surveys. At baseline, 57% of participants reported shopping at a farmers market within the last year; 18% had previously used DUFB. By the end of the DUFB season, participants were significantly more likely to report DUFB use than at baseline (AOR=19.2, 95% CI=10.3, 35.5, p<0.001), with 69% of participants reporting use of DUFB at least once, and 34% reporting use of DUFB three or more times. Adjusted fruit and vegetable consumption increased from baseline by 0.65 servings/day (95% CI=0.37, 0.93, p<0.001) at 3 months, and remained 0.62 servings/day (95% CI=0.32, 0.92, p<0.001) higher than baseline 2 months post-DUFB season.
Conclusions
A brief clinic-based intervention was associated with a nearly fourfold increase in uptake of a SNAP incentive, as well as clinically significant increases in produce consumption. Results suggested sustained behavior change even once the financial incentive was no longer available. Providing information about healthy food incentives is a low-cost, easily implemented intervention that may increase produce consumption among low-income patients.
INTRODUCTION
Diet-related diseases—including diabetes, heart disease, hypertension, and obesity—are among the leading causes of morbidity and mortality in the U.S.1,2 This disease burden is disproportionately concentrated in low-income communities where access to healthy food is limited, and fruit and vegetable (FV) consumption is far below national dietary guidelines.3–5
The high cost of produce relative to calorie-dense, nutrient-poor foods represents a significant barrier to more healthful eating in low-income communities.6–9 In addition to federal programs such as the Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp Program), public and private organizations have developed initiatives to address affordability-related barriers to healthy eating.10–13 One particularly promising approach provides produce-specific financial incentives by matching SNAP funds spent at farmers markets and other participating venues. A growing body of literature suggests that SNAP incentive programs facilitate increased produce purchase and consumption.14–17
One such SNAP incentive program is Double Up Food Bucks (DUFB). Launched in 2009, DUFB is currently accepted at more than 140 farmers markets/farm stands and 22 grocery stores throughout Michigan. When a customer uses SNAP benefits on any SNAP-eligible purchases at a participating farmers market between June 1 and October 31, they receive a 1:1 incentive match, up to $20 per visit, in DUFB that can be redeemed for locally grown produce.18 During 2015, participating Michigan markets reported $1,561,577 in combined SNAP sales ($861,308) and distributed Double Up Food Bucks ($700,269)a (E Trumbull, Fair Food Network, personal communication, 2016). The first statewide SNAP incentive program implemented with uniform design and central administration, the DUFB model has now expanded to 19 states.18
Many SNAP-enrolled families, however, do not take advantage of SNAP incentive programs such as DUFB, in part owing to lack of program awareness and understanding.14,19,20 Little is known about how best to increase program uptake. Health centers serving low-income communities could be effective venues for outreach to eligible families. Prior studies have examined health center efforts to screen for food insecurity and provide referrals to community resources,21–25 as well as the impact of establishing a health center–affiliated farmers market on produce consumption among low-income diabetics.26 However, there are no published studies examining health center–based initiatives to increase uptake of SNAP incentive programs, or longer-term impacts of SNAP incentive programs on overall dietary patterns.
To address these knowledge gaps, a longitudinal, repeated-measures, quasi-experimental trial was conducted evaluating a brief waiting room–based informational intervention promoting DUFB in a primary care clinic serving a low-income community in Southeast Michigan. It was hypothesized that a significant proportion of the health center population would be SNAP enrolled, and that baseline rates of DUFB utilization would be low. It was further hypothesized that the intervention would increase program use and produce consumption. Specifically, the authors examined: (1) self-reported rates of DUFB use among SNAP-enrolled households; and (2) self-reported rates of FV consumption. All data were collected at baseline, over the final 3 months of the DUFB market season (August–October 2014), and 2 months following the conclusion of the DUFB season.
METHODS
Study Sample
Recruitment for the study took place in the waiting room of an academic outpatient family medicine and pediatrics practice serving a low-income, racially and ethnically diverse community in Ypsilanti, Michigan. Adults aged >18 years, currently SNAP enrolled, English or Spanish speaking, and self-identified as a primary food shopper for their household were eligible for participation. Eligibility was assessed through a baseline paper survey distributed to all adults present in the waiting room. Those who met eligibility criteria were invited to participate in the longitudinal study. Participants unable to complete a telephone survey in English or Spanish or to provide a working telephone number were excluded. All participants provided verbal informed consent for the initial eligibility screening survey. Eligible adults who agreed to participate in the longitudinal study provided written informed consent to receive three telephone surveys over a 5-month period. This study was approved by the University of Michigan Medical School IRB.
Recruitment took place during August 2014, which was 2 months into the DUFB season, to better assess a baseline rate of program use given standard program outreach. It was hypothesized that by August, participants would have had ample opportunity to learn about and use DUFB prior to enrollment, but would still have a full 3 months of potential DUFB use following the intervention.
Eligibility screening surveys were primarily self-administered, but research staff were available to assist participants preferring oral administration. Research staff distributed surveys daily for 4 weeks in staggered 6-hour time blocks. To capture as diverse a sample as possible, recruitment blocks included morning, afternoon, and evening clinic hours.
Several strategies were used to minimize loss to follow-up. Strategies included: (1) requesting multiple modes of contact, including a second phone number, address, and e-mail; (2) use of the same research assistant and outgoing phone number for each survey call; and (3) offering incentives for survey completion.
In the waiting room, study staff provided participants a brief verbal explanation of DUFB including program eligibility requirements, where and how to use the program, and rules and limitations. Participants were given print copies of branded DUFB promotional materials (Appendix Figure 1), a map of eight local farmers markets specifying locations and hours,b a list of frequently asked questions about DUFB (Appendix Figure 2), and a one-time $10 voucher redeemable for FV to use at their first farmers market visit as an additional financial incentive. Vouchers were not eligible for DUFB match.
Follow-up semi-structured telephone surveys were conducted at 1.5 months, 3 months (end of the DUFB season), and 5 months (2 months post–DUFB season), ending in January 2015. All study participants received a $10 Visa gift card for each completed telephone survey. Participants completing all surveys were entered into a raffle for a $50 gift card.
Measures
The primary outcome measure was use of DUFB. Baseline rates of DUFB use (ever) were assessed in the initial screening survey and verbally confirmed at the time of enrollment. Self-reported DUFB use (yes/no) and frequency within the prior month was assessed at 1.5-month and 3-month follow-up. At 5 months, a summary question was asked assessing DUFB use and frequency over the entire DUFB season. For those participants missing data for the 5-month summary question, missing values were replaced with reported DUFB use (yes/no) at 1.5 and 3 months, if available.
Participants’ FV intake was also examined at baseline, 1.5 months, 3 months, and 5 months, with a validated two-item FV instrument assessing the number of servings of fruits and of vegetables usually consumed each day.27,28
Baseline measures included participant sociodemographic characteristics, self-health assessment, food security status, federal food assistance received, and self and others in household with diet-related disease (Table 1).
Table 1.
Baseline Characteristics of SNAP-Enrolled Adults at Health Center
| Characteristics | Enrolled in study (n=177) | Eligible but not enrolled (n=125) | p-valuea,b |
|---|---|---|---|
| English-speaking, % (N) | 94.9 (168) | 98.4 (123) | 0.111 |
| Female, % (N) | 85.3 (151) | 88.4 (107) | 0.438 |
| Reason for visit, % (N) | 0.462 | ||
| Patient | 59.9 (106) | 59.3 (73) | |
| Parent of patient | 22.6 (40) | 26.8 (33) | |
| Family member of patient | 18.1 (32) | 12.2 (15) | |
| Age, mean (IQR) | 38 (29–46) | 35 (25–43) | 0.027 |
| Race/Ethnicity, % (N)c | 0.179 | ||
| Black, non-Hispanic | 59.9 (106) | 58.4 (73) | |
| White, non-Hispanic | 29.4 (52) | 34.4 (43) | |
| Hispanic | 9.0 (16) | 4.0 (5) | |
| Other | 9.0 (16) | 12.0 (15) | |
| Marital status, % (N)d | 0.792 | ||
| Single, never married | 55.4 (98) | 53.6 (67) | |
| Married/Partnered | 20.9 (37) | 24.0 (30) | |
| Divorced/Separated/Widowed | 22.6 (40) | 20.8 (26) | |
| Education, % (N)d | 0.307 | ||
| <HS degree | 13.2 (23) | 15.5 (19) | |
| HS grad/GED | 38.5 (67) | 41.5 (51) | |
| Some college/Technical school | 37.4 (65) | 27.6 (34) | |
| College grad or higher | 10.9 (19) | 15.5 (19) | |
| Household size, mean (SD) | 3.16 (1.76) | 3.42 (1.82) | 0.211 |
| At least 1 child <18 in household, % (N) | 63.3 (112) | 71.2 (89) | 0.151 |
| Employment status, % (N)d | 0.739 | ||
| Employed | 35.0 (62) | 39.2 (49) | |
| Unemployed, in school, retired | 40.1 (71) | 40.8 (51) | |
| Disabled | 22.0 (39) | 19.2 (24) | |
| Annual household income, % (N)d | 0.015 | ||
| <$15,000 | 69.4 (123) | 52.8 (66) | |
| $15,000–$24,999 | 16.4 (29) | 20.0 (25) | |
| ≥$25,000 | 4.52 (8) | 7.2 (9) | |
| Food assistance in addition to SNAP, % (N) | 0.231 | ||
| WIC | 29.4 (52) | 36.0 (45) | |
| Other | 2.3 (4) | 3.2 (4) | |
| Worried about having enough money to buy food in the past year, % (N)d | 0.006 | ||
| Always or usually | 38.4 (68) | 24.8 (31) | |
| Sometimes | 41.2 (73) | 42.4 (53) | |
| Rarely or never | 18.6 (33) | 32.8 (41) | |
| Daily servings of FV, mean (SD) | 3.63 (1.78) | 3.38 (1.72) | 0.231 |
| Self-health assessment poor or fair, % (N) | 32.8 (58) | 30.7 (38) | 0.697 |
| Shopped at a FM in the last year, % (N) | 56.6 (99) | 45.1 (56) | 0.052 |
| Previously used DUFB, % (N) | 18.2 (32) | 7.3 (9) | 0.023 |
| ≥1 Household member with following health conditions (self-report), % (N)c | |||
| Diabetes | 25.4 (45) | 12.8 (16) | 0.007 |
| Hypertension | 40.7 (72) | 28.8 (36) | 0.034 |
| High cholesterol | 18.6 (33) | 8.8 (11) | 0.017 |
| Obesity | 45.2 (80) | 33.6 (42) | 0.043 |
t-test for continuous variables, chi-squared test for categorical variables.
Boldface indicates statistical significance (p>0.05).
Totals sum to >100% due to option to check more than one category.
Totals do not sum to 100% due to missing data.
DUFB, Double Up Food Bucks; SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; HS, High School; GED, General Education Development
Statistical Analysis
A goal was set of recruiting 150 participants for the longitudinal portion of the study. Sample size was calculated to detect at least a 15% pre/post change in rates of DUFB use (0.9 power, a=0.05), with oversampling to accommodate 25% attrition at each survey wave. Although the study was not prospectively powered to detect a clinically meaningful change in FV consumption—defined as 0.5 servings/day, as this is both clinically significant and consistent with other studies14,26,28—the final sample was larger than anticipated, thereby improving power to detect change in this outcome.
Standard descriptive statistics were calculated for all variables. Independent samples t-tests and chi-square tests were used to assess differences in continuous and categorical characteristics, respectively, between study participants and non-participants. Multivariable clustered logistic regression models were used to estimate DUFB use (dependent variable), with a two-level factor time (baseline, 5 months) as the primary independent variable. Clustering within subject was accounted for via a generalized estimating equations approach. A Poisson regression model was used to estimate predicted mean number of times participants who were DUFB naïve at baseline used DUFB by the end of the season, assuming a mean value for all covariates. A multivariable linear mixed model was used to estimate FV consumption (dependent variable), with a four-level categorical variable denoting time (baseline and three follow-up waves) as the primary factor. A random subject intercept was used to account for clustering within individual participants. Models employed all-case analyses, and were analyzed unadjusted as well as adjusted for the baseline covariates: FV consumption, farmers market use within the last year, DUFB use, gender, age, race/ethnicity, children aged <18 years in the household, at least one person in the household with diet-related disease, and employment status. Sensitivity analyses were conducted for each model using complete-case analyses, and were not found to substantively differ from models using all-case analyses.
Interaction analyses were conducted (by including a multiplicative term in the linear mixed model) to assess if the association between receipt of the intervention and change in FV consumption was modified by baseline FV consumption. Finally, multiple linear regression models were used to assess the association between change from baseline FV consumption at 3 and 5 months and the number of times participants reported using DUFB, controlling for baseline DUFB use. Stata, version 13.1 was used for all analyses, which were conducted in 2015–2016.
RESULTS
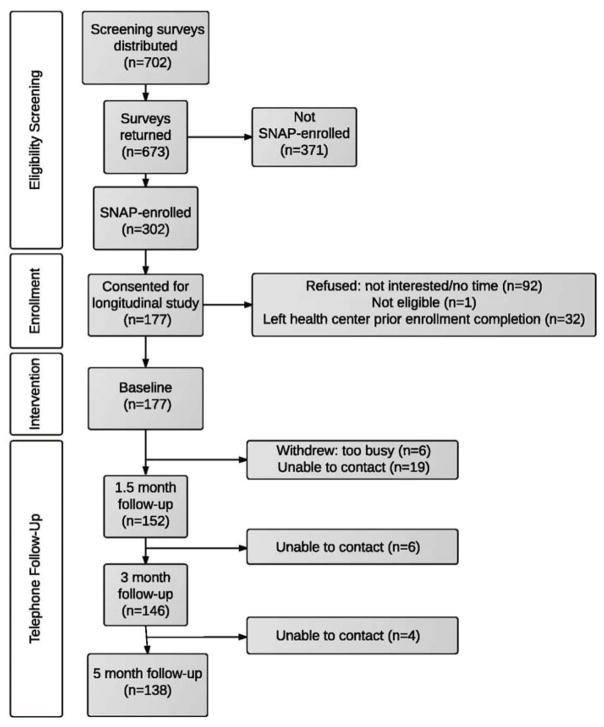
Of 702 adults, 673 (96%) who received baseline surveys completed them, and almost half reported current SNAP enrollment. Of the 302 SNAP-enrolled participants, 177 (59%) enrolled in the study (Figure 1). One hundred forty-nine (84%) completed at least three surveys, and 127 (72%) completed all four surveys.
Figure 1.
Study flow diagram.
SNAP, Supplemental Nutrition Assistance Program
Participants largely identified as African American/black (60%), female (85%), and having an annual household income <$15,000 (69%). Mean baseline FV consumption was 3.63 (SD=1.78) servings/day, consistent with reported rates for similar low-income populations.27,28 Almost half of participants reported at least one household member with hypertension (41%) and/or obesity (45%), and one quarter reported at least one household member with diabetes (Table 1). Differences between eligible adults who enrolled versus those who did not enroll are noted in Table 1.
At baseline, 56% of participants reported shopping at a farmers market within the last year, consistent with baseline rates of farmers market use in several other low-income communities.20,26,29 Only 18% of study participants, however, reported prior DUFB use (Table 1). By the end of the DUFB season, participants were significantly more likely to report DUFB use than at baseline in both unadjusted (OR=9.2, 95% CI=6.1, 13.8) and adjusted (AOR=19.2, 95% CI=10.3, 35.5, p<0.001) (Appendix Table 1) models, with 69% of participants reporting use of DUFB at least once and 34% reporting use of DUFB three or more times. Among the 82% of participants reporting no prior DUFB use at baseline, 61% reported using DUFB at least once by the end of the season, and 27% reported using DUFB three or more times, with an adjusted predicted mean of 1.7 visits by the end of the season (95% CI=1.5, 2.0, p<0.001). Breakdown of DUFB use by follow-up period is presented in Appendix Table 2.
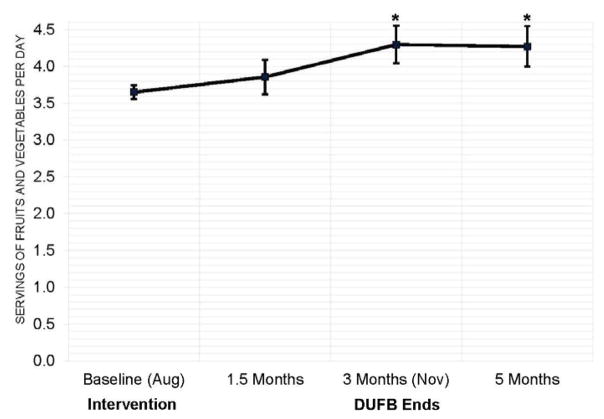
In the unadjusted model, FV consumption in the study sample increased from baseline by 0.66 servings/day (95% CI=0.38, 0.93, p<0.001) at 3 months and remained increased at 5 months (0.63 servings/day higher than baseline, 95% CI=0.34, 0.92, p<0.001). After adjusting for covariates, FV consumption remained increased at 3 and 5 months (0.65 servings/day, 95% CI=0.37, 0.93, p<0.001 and 0.62 servings/day, 95% CI=0.32, 0.92, p<0.001, respectively) (Figure 2, Appendix Table 3).
Figure 2.
Adjusted change in fruit and vegetable consumption.
Notes: Multivariable linear mixed model (n=168), adjusted for gender, age, children <18 in household, race/ethnicity, baseline fruit and vegetable consumption, baseline farmers market use in the past year, baseline DUFB use, ≥1 household-members with diet-related disease, and employment status.
* difference from baseline, p<0.001
DUFB, Double Up Food Bucks
There was a significant interaction between change in FV consumption and baseline consumption (p<0.001). Participants with baseline FV consumption of zero to three servings/day had a 0.89 servings/day increase at 1.5 months (95% CI=0.56, 1.21, p<0.001), 1.33 servings/day increase at 3 months (95% CI=0.964, 1.70, p<0.001), and 1.25 servings/day increase at 5 months (95% CI=0.86, 1.63). Among those participants with a baseline FV consumption of ≥4 servings/day, there was a 0.48 serving/day decrease in consumption at 1.5 months (95% CI= −0.84, −0.12, p=0.010); but no significant change at 3 or 5 months (Appendix Table 4).
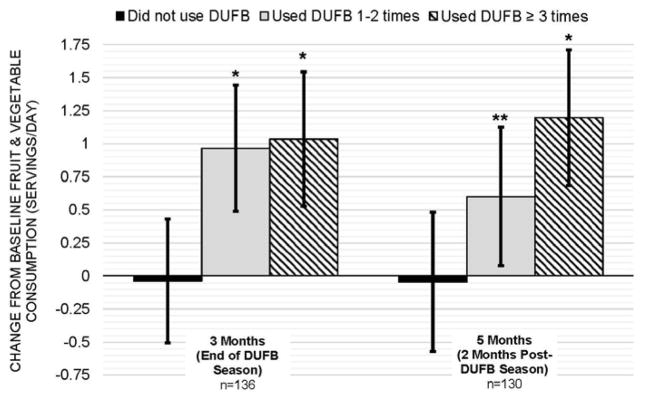
Self-reported frequency of DUFB use over the course of the study was also significantly associated with change from baseline FV consumption over time (p=0.002). Among participants who used DUFB three or more times, FV consumption increased by 1.04 servings/day from baseline at 3 months (95% CI=0.52, 1.55, p<0.001) and remained elevated at 5 months (1.16 servings/day above baseline, 95% CI=0.62, 1.69, p<0.001). There were similar increases at 3 months among those participants reporting DUFB use one to two times, although the magnitude of increase diminished at 5 months. FV consumption was unchanged among participants who did not use DUFB (Figure 3).
Figure 3.
Adjusted change in fruit and vegetable consumption, by DUFB use.
Notes: Multivariable linear regression, adjusted for gender, age, children <18 in household, race/ethnicity, baseline fruit and vegetable consumption, baseline farmers market use in the past year, baseline DUFB use, ≥1 household-members with diet-related disease, and employment status.
* difference from baseline, p<0.001; **difference from baseline, p=0.039
DUFB, Double Up Food Bucks
DISCUSSION
A brief waiting room intervention in an urban primary care center was associated with an almost fourfold increase in reported use of DUFB over a 3-month period. In addition, the intervention was associated with a statistically and clinically significant increase of approximately two-thirds of a serving/day of FVs. A dose–response relationship was observed between produce consumption and frequency of DUFB use, although there appeared to be a ceiling effect with the greatest increases in consumption among those with lowest (0–3 servings/day) baseline consumption. Increased consumption across the study population was largely maintained 2 months after the DUFB season ended, suggesting sustained behavior change even when the financial incentive was no longer available.
This study builds on prior studies in several ways. Most prior studies have examined the impact of SNAP incentive use among individuals already shopping at a farmers market.15,16,34 However, these individuals may not be representative of the broader SNAP-enrolled population. The U.S. Department of Agriculture Healthy Incentive Pilot Study is the only prior investigation of an incentive program in a broad SNAP-enrolled population. In this study, a random subsample of 7,500 SNAP households in one county of Massachusetts received a $0.30 incentive for every dollar of SNAP benefits spent on targeted FVs at participating retailers.14 Although the study presented here was much smaller in scale, in contrast to the Healthy Incentive Pilot, it assessed the impact of an intervention on use of an existing SNAP incentive program, rather than evaluating a newly created program.
The intervention presented here was associated with increases in FV consumption similar to those found in the Healthy Incentive Pilot and other behavioral interventions targeting increased FV consumption.14,31,32 This study also had higher retention rates compared with several prior longitudinal incentive interventions,30,33–35 which may augment generalizability and help mitigate potential selection bias.
The authors believe the intervention was likely successful for several reasons. First, situating the intervention in a health center framed information and messaging about the program in a health-oriented setting. Second, this approach may have conveyed implicit endorsement of the incentive program by the health center and providers. Finally, by recruiting participants and delivering the intervention in the clinic waiting room, the intervention was able to capitalize on a time when patients and family members were typically unengaged and available for interaction with study staff.
Providing brief waiting room information to eligible adults about healthy food incentive programs is a low-cost, easily implemented intervention that may increase produce purchase and consumption for a substantial portion of patients. There are currently incentive programs in at least 40 states and the District of Columbia.18,36 With $31.5 million in federal funding awarded in 2015 for the expansion and evaluation of SNAP incentive programs through the U.S. Department of Agriculture Food Insecurity Nutrition Incentive Grant Program, and $100 million in funding committed by Fiscal Year 2018,37 there are now plans for incentive programs in almost every state.18,36 With this geographic spread, interventions to increase incentive use will become only more relevant.
Given recent renewed recognition of the importance of identifying and addressing food insecurity and other material hardship among low-income patients, several professional societies and national guidelines have called for the incorporation of food insecurity screening into clinical care. 38–40 Several recent studies have described promising clinical–community partnerships to address food insecurity.21,23–25 Interventions such as the one presented here that educate and connect eligible low-income patients to existing resources can serve as a valuable component of clinic to community integration.
Several areas for future research include exploration of the mechanisms through which the intervention was associated with increased DUFB use, and the relative importance of each of the constituent parts (e.g., information, $10 voucher, clinic-based setting). A better understanding of how specific aspects of the intervention may have facilitated increased consumption can help focus future clinic-based initiatives. Additionally, more rigorous evaluation incorporating a comparison group is merited to confirm reproducibility of results. Research is also warranted to better understand barriers to SNAP incentive use, and how communities can best address these barriers in order to maximize program impact.
Limitations
This study has several limitations. First, the study took place at a single health center, potentially limiting generalizability. The health center does, however, serve a low-income, racially and ethnically diverse population, and indicators measured such as baseline FV consumption were consistent with rates reported in the literature for similarly diverse low-income communities. Second, although a strength of the study was the ability to collect descriptive data on both participants and eligible non-participants, findings may be susceptible to selection bias because those more familiar with or interested in going to farmers markets or using DUFB may have been more likely to participate in the study. Relative to non-participants, participants were also more likely to be poorer, slightly older, more food insecure, and report a higher rate of diet-related disease.
Third, absent a control group, a causal relationship cannot be established between the intervention and either use of DUFB or increases in produce consumption. There may have been confounding factors influencing DUFB use that could not be measured, and those participants who used DUFB may have been predisposed to increase their FV consumption for reasons other than the intervention. Increases in FV consumption may also have been influenced by purchases made at non-farmers market venues. Although baseline rates of DUFB (18%) were measured at the height of the farmers market season, it is possible that some participants would have used the program even without the intervention. Conversely, because there were only 3 months remaining in the DUFB season at the time of recruitment, the potential season-long impact of the intervention may have been underestimated. There may have also been a seasonal component to participants’ increased FV consumption, although increases in reported consumption were maintained at the January follow-up. Additionally, in analyses examining consumption by frequency of DUFB use, there was no change in consumption over time among DUFB non-users, indicating that consumption was not simply higher for all participants during periods when more FVs were in season.
Fourth, measures of DUFB and FV consumption were based on self-report, which may limit the validity and reliability of results, and is subject to recall bias. However, the study employed repeated measures using an instrument for FV consumption validated in a low-income population.27,28 Furthermore, as the study used repeated measures, the findings should be robust to within-person changes.
Finally, use of follow-up phone calls over 5 months to ascertain information on DUFB use and produce consumption may have prompted some participants to increase the behaviors being studied. Additionally, reported increases in DUFB use may have been affected by learned response or social acceptability bias. To the extent there was a “Hawthorne effect,” this intervention might have been less effective if not paired with recurring assessments.
CONCLUSIONS
A brief waiting room–based intervention was associated with increased use of a SNAP incentive program and participant FV consumption over a 5-month period. This study highlights opportunities for clinics to support healthy behavior change by promoting linkages with relevant community resources. If taken to scale, bridging historical silos between clinical care and community-based social services may pay dividends in improved population health.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the patients, staff, and providers of the Ypsilanti Health Center, Washtenaw County Farmers Markets, Elisa Trumbull of Fair Food Network, and Rachel Chadderdon Bair of Kalamazoo Valley Community College (formerly of Fair Food Network). We also thank Hwajung Choi for her statistical assistance, and Jason Buxbaum for his thoughtful review of the manuscript. We gratefully acknowledge the support of our research assistants Steven Merritt, Kirke Elsass, Jessica Landgraf, Robyn Power, Jessica Haeffner, and Jamarie Geller.
This study was supported by grants from the Robert Wood Johnson Foundation Clinical Scholars® and the W.K. Kellogg Foundation. Study sponsors had no role in study design; collection, analysis, or interpretation of data; writing the report; or the decision to submit the report for publication. This study was approved by the University of Michigan Medical School IRB, HUM00076630.
Footnotes
Of these transactions, $68,341 in SNAP and $57,999 in DUFB were from eight farmers markets in Washtenaw County, all of which are 1–25 miles from the health center where the intervention was delivered.
Two markets furthest away from the health center (20 and 25 miles, respectively) were listed but not visually depicted on the map.
AJC is responsible for study conception, study design, data collection, data analysis, data interpretation, and manuscript preparation and revision; had access to all of the data in the study; and takes responsibility for the integrity of the data and the accuracy of the data analysis. OBH and SMZ contributed to conception of the study; CRR, ECM, and SMZ contributed to the design of the study; ECM contributed to data collection; CRR, AS, and SMZ contributed to data analysis; CRR, MH, AS, ECM, MMD, and SMZ contributed to data interpretation; CRR, MH, ECM, MMD, and SMZ contributed to manuscript preparation and revision; and AS, and OBH, provided assistance with manuscript revision. (MMD was faculty at the University of Michigan during the period this study was conducted.)
This study was registered at clinicaltrials.gov (NCT02558660).
Preliminary results were presented as a work-in-progress poster at the Society of Teachers of Family Medicine Annual Meeting in April 2015 and the Academy Health Annual Research Meeting in June 2015, as well as an oral presentation at the North American Primary Care Research Group Annual Meeting in October 2015.
CRR serves as an Associate Editor and AS serves as a Statistics Editor for the American Journal of Preventive Medicine. Neither had any involvement in the peer review and decision-making process for this paper.
OBH is president and CEO of Fair Food Network, which administers the Double Up Food Bucks program. No other financial disclosures were reported by the authors of this paper.
References
- 1.Murphy SL, Kochanek KD, Xu JQ, Arias E. Mortality in the United States, 2014. Hyattsville, MD: National Center for Health Statistics; 2015. [Google Scholar]
- 2.Murray CJ, Atkinson C, Bhalla K, et al. The state of U.S. health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. http://dx.doi.org/10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among U.S. adults: A 2012 update. Prev Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. http://dx.doi.org/10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department of Agriculture. Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: USDA; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. doi: 10.1001/jamainternmed.2014.3422. http://dx.doi.org/10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. doi: 10.1093/nutrit/nuv027. http://dx.doi.org/10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107(12):2071–2076. doi: 10.1016/j.jada.2007.09.009. http://dx.doi.org/10.1016/j.jada.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Drewnowski A. The cost of U.S. foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181–1188. doi: 10.3945/ajcn.2010.29300. http://dx.doi.org/10.3945/ajcn.2010.29300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;(87):1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 10.Bleich SN, Jones-Smith J, Wolfson JA, Zhu X, Story M. The complex relationship between diet and health. Health Aff (Millwood) 2015;34(11):1813–1820. doi: 10.1377/hlthaff.2015.0606. http://dx.doi.org/10.1377/hlthaff.2015.0606. [DOI] [PubMed] [Google Scholar]
- 11.Block JP, Subramanian SV. Moving beyond “food deserts”: Reorienting United States policies to reduce disparities in diet quality. PLoS Med. 2015;12(12):e1001914. doi: 10.1371/journal.pmed.1001914. http://dx.doi.org/10.1371/journal.pmed.1001914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon E, Dawkins-Lyn N, Hogan-Yarbro R, et al. Approaches for promoting healthy food purchases by SNAP participants. U.S. Department of Agriculture, Food and Nutrition Service; 2014. [Google Scholar]
- 13.King M, Dixit-Joshi S, MacAllum K, Steketee M, Leard S. Famers market incentive provider study. U.S. Department of Agriculture, Food and Nutrition Service; 2014. [Google Scholar]
- 14.Bartlett S, Klerman J, Wilde P, et al. Evaluation of the Healthy Incentives Pilot (HIP) final report. U.S. Department of Agriculture, Food and Nutrition Service; 2014. [Google Scholar]
- 15.Young CR, Aquilante JL, Solomon S, et al. Improving fruit and vegetable consumption among low-income customers at farmers markets: Philly Food Bucks, Philadelphia, Pennsylvania, 2011. Prev Chronic Dis. 2013;10:E166. doi: 10.5888/pcd10.120356. http://dx.doi.org/10.5888/pcd10.120356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savoie-Roskos M, Durward C, Jeweks M, LeBlanc H. Reducing food insecurity and improving fruit and vegetable intake among farmers’ market incentive program participants. J Nutr Educ Behav. 2016;48(1):70–76. doi: 10.1016/j.jneb.2015.10.003. http://dx.doi.org/10.1016/j.jneb.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Phipps EJ, Braitman LE, Stites SD, et al. Impact of a rewards-based incentive program on promoting fruit and vegetable purchases. Am J Public Health. 2015;105(1):166–172. doi: 10.2105/AJPH.2013.301752. http://dx.doi.org/10.2105/ajph.2013.301752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fair Food Network. [Accessed December 30, 2015];Double Up National Network. 2015 www.doubleupfoodbucks.org/national-network.
- 19.Karakus M, MacAllum K, Milfort R, Hao H. Nutrition assistance in farmers markets: Understanding the shopping patterns of SNAP participants. U.S. Department of Agriculture, Food and Nutrition Service; Oct, 2014. [Google Scholar]
- 20.Olsho LE, Payne GH, Walker DK, Baronberg S, Jernigan J, Abrami A. Impacts of a farmers’ market incentive programme on fruit and vegetable access, purchase and consumption. Public Health Nutr. 2015;18(15):2712–2721. doi: 10.1017/S1368980015001056. http://dx.doi.org/10.1017/s1368980015001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beck AF, Henize AW, Kahn RS, Reiber KL, Young JJ, Klein MD. Forging a pediatric primary care-community partnership to support food-insecure families. Pediatrics. 2014;134(2):e564–571. doi: 10.1542/peds.2013-3845. http://dx.doi.org/10.1542/peds.2013-3845. [DOI] [PubMed] [Google Scholar]
- 22.Garg A, Sandel M, Dworkin PH, Kahn RS, Zuckerman B. From medical home to health neighborhood: transforming the medical home into a community-based health neighborhood. J Pediatr. 2012;160(4):535–536. e531. doi: 10.1016/j.jpeds.2012.01.001. http://dx.doi.org/10.1016/j.jpeds.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Beck AF, Henize A, Kahn R, Reiber K, Klein M. Curtailing food insecurity with clinical-community collaboration. [Accessed May 15, 2016];Health Affairs Blog. 2015 http://healthaffairs.org/blog/2015/07/09/curtailing-food-insecurity-with-clinical-community-collaboration/
- 24.Stenmark S, Solomon L, Allen-Davis J, Brozena C. Linking the clinical experience to community resources to address hunger in Colorado. [Accessed May 15, 2016];Health Affairs Blog. 2015 http://healthaffairs.org/blog/2015/07/13/linking-the-clinical-experience-to-community-resources-to-address-hunger-in-colorado/
- 25.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: A cluster RCT. Pediatrics. 2015;135(2):e296–304. doi: 10.1542/peds.2014-2888. http://dx.doi.org/10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freedman DA, Choi SK, Hurley T, Anadu E, Hebert JR. A farmers’ market at a federally qualified health center improves fruit and vegetable intake among low-income diabetics. Prev Med. 2013;56(5):288–292. doi: 10.1016/j.ypmed.2013.01.018. http://dx.doi.org/10.1016/j.ypmed.2013.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Resnicow K, Odom E, Wang T, et al. Validation of three food frequency questionnaires and 24-hour recalls with serum carotenoid levels in a sample of African-American adults. Am J Epidemiol. 2000;152(11):1072–1080. doi: 10.1093/aje/152.11.1072. http://dx.doi.org/10.1093/aje/152.11.1072. [DOI] [PubMed] [Google Scholar]
- 28.Allicock M, Johnson LS, Leone L, et al. Promoting fruit and vegetable consumption among members of black churches, Michigan and North Carolina, 2008–2010. Prev Chronic Dis. 2013;10:e33. doi: 10.5888/pcd10.120161. http://dx.doi.org/10.5888/pcd10.120161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leone LA, Beth D, Ickes SB, et al. Attitudes toward fruit and vegetable consumption and farmers’ market usage among low-income North Carolinians. J Hunger Environ Nutr. 2012;7(1):64–76. doi: 10.1080/19320248.2012.651386. http://dx.doi.org/10.1080/19320248.2012.651386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dimitri C, Oberholtzer L, Zive M, Sandolo C. Enhancing food security of low-income consumers: An investigation of financial incentives for use at farmers markets. Food Policy. 2015;52:64–70. http://dx.doi.org/10.1016/j.foodpol.2014.06.002. [Google Scholar]
- 31.Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Prev Med. 2002;35(1):25–41. doi: 10.1006/pmed.2002.1028. http://dx.doi.org/10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- 32.Resnicow K, Jackson A, Blissett D, et al. Results of the healthy body healthy spirit trial. Health Psychol. 2005;24(4):339–348. doi: 10.1037/0278-6133.24.4.339. http://dx.doi.org/10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- 33.Lindsay S, Lambert J, Penn T, et al. Monetary matched incentives to encourage the purchase of fresh fruits and vegetables at farmers markets in underserved communities. Prev Chronic Dis. 2013;10:E188. doi: 10.5888/pcd10.130124. http://dx.doi.org/10.5888/pcd10.130124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anliker JA, Winne M, Drake LT. An evaluation of the Connecticut farmers’ market coupon program. J Nutr Educ. 1992;24(4):185–191. http://dx.doi.org/10.1016/s0022-3182(12)81152-6. [Google Scholar]
- 35.Kunkel ME, Luccia B, Moore AC. Evaluation of the South Carolina seniors farmers’ market nutrition education program. J Am Diet Assoc. 2003;103(7):880–883. doi: 10.1016/s0002-8223(03)00379-1. http://dx.doi.org/10.1053/jada.2003.50164. [DOI] [PubMed] [Google Scholar]
- 36.Wholesome Wave. [Accessed December 30, 2015];Our initiatives. 2014 www.wholesomewave.org/our-initiatives/
- 37.Agricultural Act of 2014. Pub.L. 113–79.
- 38.American Academy of Pediatrics. Promoting food security for all children. Pediatrics. 2015;136(5):e1431–1438. doi: 10.1542/peds.2015-3301. http://dx.doi.org/10.1542/peds.2015-3301. [DOI] [PubMed] [Google Scholar]
- 39.Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 40.American Academy of Family Physicians. [Accessed January 2, 2016];Social determinants of health policy. 2013 www.aafp.org/about/policies/all/social-determinants.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.