Abstract
Objective
To compare the benefit of wireless contralateral routing of signal (CROS) technology to bone-anchored implant (BAI) technology in monaural listeners.
Study Design
Prospective, single-subject
Setting
Tertiary academic referral center
Patients
Adult English speaking subjects using either a CROS hearing aid or BAI as treatment for unilateral severe-profound hearing loss.
Interventions
Aided performance utilizing the subjects BAI or CROS hearing device.
Main Outcome Measures
Outcome measures included speech-in-noise perception using the QuickSIN™ speech-in-noise test and localization ability using narrow and broadband stimuli. Performance was measured in the unaided and aided condition and compared to normal hearing controls. Subjective outcomes measures included the Speech Spatial and Qualities hearing scale and the Glasgow Hearing Aid Benefit Profile.
Results
A significant improvement in speech-in-noise performance for monaural listeners (p<0.0001) was observed, but there was no improvement in localization ability of either CROS or BAI users. There was no significant difference between CROS and BAI subject groups for either outcome measure. BAI recipients demonstrate higher initial disability and handicap over CROS hearing aid users. No significant difference was observed between treatment groups for subjective measures of post-treatment residual disability or satisfaction.
Conclusions
Our data demonstrate that both CROS and BAI systems provide significant benefit for monaural listeners. There is no significant difference between CROS or BAI systems for objective measures of speech-in-noise performance. CROS and BAI hearing devices do not provide any localization benefit in the horizontal plane for monaural listeners and there is no significant difference between systems.
Keywords: Unilateral hearing loss, Single-sided deafness, Bone anchored implant, Bone anchored hearing aid, Contralateral routing of signal, Monaural listening
INTRODUCTION
Individuals with a severe-profound unilateral sensorineural hearing impairment, often termed “single-sided deafness”, largely lose the ability to localize auditory events within the horizontal plane and experience difficulty understanding speech, particularly in reverberant or noisy environments (1,2). These impairments occur due to the loss of auditory cues provided through binaural hearing. In binaural hearing, the ear closest to the sound source receives the signal earlier and at a higher intensity. The differences in these timing and level cues for a sound arriving to two ears are critical for processing of complex auditory signals such as speech perception in noise and localization of sound. Individuals with a severe-profound unilateral sensorineural hearing loss become monaural listeners, thereby losing access to these essential auditory cues. As a result, all sounds arrive to the non-impaired ear at the same time and level. This is due to the head-shadow effect where the head acts as a barrier to sound as it travels from one side to the other resulting in an attenuation of the sound (21).
Despite one normally functioning ear, monaural listeners are subject to significant hearing disability and handicap (3–5). Lifting the head-shadow can significantly improve listening in noise ability in monaural listeners (6–10). In order to accomplish this, the signal of interest must be routed from the impaired (deaf) ear to the normal cochlea for processing. Historically, this was achieved using contralateral routing of signal (CROS) hearing aids where a microphone is placed at the impaired ear, which then routes the acoustic signal to a hearing aid worn in the normally functioning ear. The CROS hearing aid was first introduced by Harford and Barry (11) in 1965. Poor acceptance of CROS hearing aids at this time are largely attributed to complaints of occlusion in the better ear, poor sound quality, and discomfort (12,13). Additional limitations included aesthetics, size, and poor battery life. Consequently, monaural listeners went largely untreated. The introduction of bone-anchored implants (BAI) (14) resulted in a resurgence in treatment for unilateral sensorineural hearing loss (SNHL). BAIs utilize a small titanium implant in the temporal bone on the impaired side that couples to an external processor. This can be accomplished either percutaneously or transcutaneously. The processor stimulates the implant, which sends the signal of interest to the contralateral (normal) cochlea by way of transcranial bone conduction. This mechanism of stimulation proved to be highly successful in monaural listeners, and several comparison studies of CROS and BAI devices emerged in the literature suggesting that the BAI system is superior to CROS technology for the treatment of unilateral SNHL(8,10,15,16). However, many of the acoustic limitations in previous CROS devices, which led to the earlier reports of limited benefit, have been overcome in new wireless CROS systems.
Due to the inability to interpret interaural timing and level cues, monaural listeners have consistently been shown to have poor localization in the horizontal plane (6–10). Interestingly, others have demonstrated that monaural listeners can in fact localize in the horizontal plane by using either spectral cues(17) or perceived level differences in the signal as it moves from the impaired ear to the normal hearing ear(18). It is possible that with the increased audibility provided with CROS and BAIs, some localization ability may be restored.
The present report compares the benefits of currently available wireless CROS technology to BAI technology in monaural listeners. We hypothesized that non-invasive wireless CROS technology is capable of providing similar benefit to the more invasive BAI system for unilateral severe-profound sensorineural hearing loss. In particular, we compared the speech perception in noise and localization abilities of monaural listeners using a BAI to monaural listeners using a CROS hearing aid.
MATERIALS AND METHODS
University of Miami Institutional Review Board approval was obtained for this study. Adult subjects (≥18 years) using either a CROS hearing aid or BAI as treatment for unilateral severe-profound sensorineural hearing loss were prospectively enrolled for study. All subjects had normal hearing in the non-impaired ear defined as < 25dB threshold of hearing averaged at 500, 1000, 2000, and 4000 Hz. For all subjects, the impaired ear was confirmed to be clinically unaidable as defined by severe-profound threshold responses with poor word recognition ability defined as < 40% on NU-6 speech perception tests(19). A control group of normal hearing subjects defined as ≤ 25dB threshold of hearing averaged at 500, 1000, 2000, and 4000Hz in both ears were enrolled for comparison to BAI and CROS study groups. In total, 24 normal hearing subjects, 13 CROS hearing aid subjects, and 14 BAI subjects were included for study. All BAI subjects used a percutaneous implant with mean device use of 66 months and CROS hearing aid users a mean device use of 34 months.
Procedures
This study was designed as a single-subject, repeated measures experiment in which each subject served as his/her own control. Experienced unilateral severe-profound sensorineural hearing loss subjects using either a BAI or CROS hearing aid and with normal hearing in the contralateral ear (<25dB) were studied in the aided and unaided (monaural) listening conditions using localization and measures of speech-in-noise perception. Level of impairment was compared to normal (n=24) hearing adults and between study groups.
The CROS hearing aid system wirelessly transmits full audio bandwidth (130 Hz–6.0 kHz) from the CROS transmitter to the hearing aid worn in the normal ear by way of omnidirectional microphone. All subjects used a Phonak Audeo V50® CROS open fit hearing aid system. Devices were fit using NAL1 prescriptive targets and gain prescribed according to better ear thresholds. During testing conditions, volume control was inactive to ensure prescriptive targets were maintained. All subjects underwent real-ear measures to ensure absence of occlusion in the normal ear and that transmission of the CROS signal approximates the real ear unaided response(20). Although exact fitting methods cannot be replicated across devices, gain for BAIs were prescribed according to better ear hearing thresholds. Twelve subjects were users of Cochlear Baha® processors and two subjects used an Oticon Medical processor. As with CROS subjects, the volume control was inactive and the omnidirectional mode was maintained for BAI subjects.
Localization
Stimuli were presented in a custom 4m×4m×2m sound booth with 19 loudspeakers setup at a radius of 1.3m and spatially separated by 10°, spanning +/− 90° (Figure 1). Stimuli were generated by a custom-designed MATLAB (Mathworks, Natick, MA) front-end for TDT RX8 realtime multichannel processor (Tucker Davis Technologies, Alachua, FL), and a series of Crown Audio CT-8150 8-channel amplifiers. Laboratory testing was calibrated as specified by ISO 8253-2:2009 by warble-tone RMS-intensity measurements. Stimuli generated were corrected for individual speaker calibration characteristics.
Figure 1.

Diagram of the experimental setup with 19 loudspeakers in the front hemifield with a radius of 1.3 meters. The subject is seated facing speaker 1 (0° front) and is provided with a feedback panel that mimics the arrangement of the speakers.
Localization stimuli included a narrowband 350-ms, 1/3 octave noise centered at 500Hz, a narrowband 350-ms, 1/3 octave noise centered at 4kHz, and a broadband 189-ms male-voiced ‘hey’, band-passed from 100–8000 Hz. Each stimuli was presented three times at 65 dB SPL roved by +/− 4dB for a total of 171 stimuli per subject in both the unaided and aided condition. The perceived locations of the sound sources were recorded utilizing a custom-designed, arduino-based 19-pushbutton feedback panel.
Speech-in-noise
Recorded commercially available QuickSIN™ (Etymotic Research, Elkgrove Village, IL, 2001) sentences were used for assessment of speech-in-noise perception. The QuickSIN™ uses low context sentences recorded in four-talker babble to estimate signal-to-noise ratio (SNR) loss. SNR loss is defined as the increase in SNR required by a listener to obtain 50% correct words in sentences compared to normal performance (21). The test was conducted in the sound field and subjects were evaluated in the speech poorer ear, noise better ear (90°/270° azimuth) configuration (22). A minimum of two lists were completed for each condition and averaged. All test protocols were repeated in the aided conditions (with CROS or BAI on) to characterize performance changes in this condition.
Subjective assessment
Speech Spatial and Qualities of Hearing (SSQ) Benefit questionnaire was used for subjective assessment of spatial perception. This questionnaire is designed to compare performance with a hearing device to performance before the hearing aid was fitted. The subjects reported on their perceived hearing ability compared to before receiving their hearing device using a visual analog scale ranging from −5 to +5 where −5 indicates much worse with the hearing device than without and +5 indicates much better. Midpoint of the scale (0) indicates no change in experience. Subjects rated their ability on 17 spatial items and 14 speech items using the same visual analog scale.
The Glasgow Hearing Aid Benefit Profile (GHABP) questionnaire was used for assessment of handicap, disability, use, benefit, and satisfaction. Subjects were given these questionnaires after a minimum of 6 months use with their hearing devices.
Statistical analyses were performed using Wilcoxon signed rank tests for nonparametric data and paired-sample. Student t tests were performed for normally distributed data. Statistical significance was set to p > 0.05. All analyses were performed using SAS JMP™ software (version 12.1; Cary, NC).
RESULTS
Twenty-seven subjects and 24 controls were included in the analysis. The subjects ranged in age from 24–77 years (52 ± 17 years) and the controls ranged in age from 24 – 49 years (mean, 34 years ± 8 years). There were 15 female controls, 9 male controls, 15 female subjects and 12 male subjects. Twelve right ears and 15 left ears were impaired. All subjects had acquired unilateral severe-profound sensorineural hearing loss with the exception of 1 CROS subject reporting congenital hearing loss. A wide range of etiology was reported including Meniere’s disease, sudden hearing loss, acoustic neuroma, aneurysm, meningitis, temporal bone fracture, autoimmune, viral infection, iatrogenic, and unknown causes.
Normal hearing controls were able to localize within the horizontal plane with a high degree of accuracy, with mean error of 6° (RMS, 13°) for voiced ‘hey’, 15° (RMS, 10°) for 1/3 octave 500 Hz and 13° (RMS 27°) for 1/3 octave 4000 Hz observed. These results were consistent with previously published reports for normal hearing individuals(23–25). In comparison, high error scores were observed for monaural listeners in the unaided condition with mean error of 66° (RMS, 44°) for voiced ‘hey’, 60° (RMS, 46°) for 1/3 octave 500 Hz, and 56° (RMS, 46°) for 1/3 octave 4000 Hz, demonstrating an inability to localize in the horizontal plane(26). There was no improvement in localization ability for voiced ‘hey’, 1/3 octave 500 Hz, or 1/3 octave 4000 Hz stimuli for any of the test subjects in the aided condition for BAI users (Figure 2) or CROS users (Figure 3). When BAI and CROS users were compared, there was no significant difference in performance for aided localization ability between groups (Figure 4).
Figure 2.

Localization performance RMS error for BAI subjects for the 500Hz 1./3 octave (A), 4kHz 1/3 octave noise (B), and voiced ‘hey’ (C) respectively are shown. Unaided and Aided responses are plotted against normative data.
Figure 3.
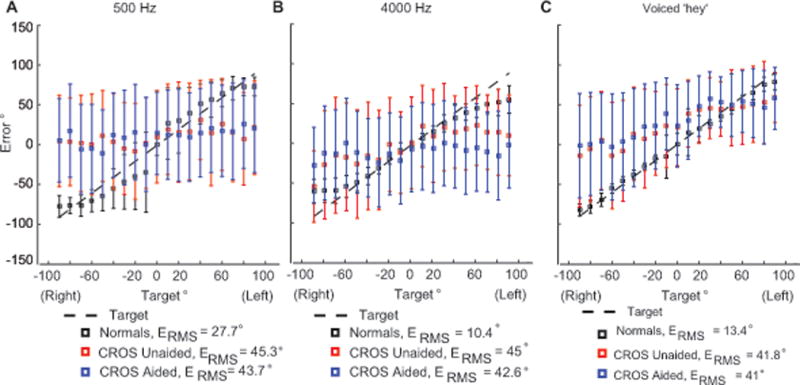
Localization performance RMS error for CROS subjects for the 500Hz 1 ./3 octave (A), 4kHz 1/3 octave noise (B), and voiced ‘hey’ (C) are shown respectively. Unaided and Aided responses are plotted against normative data.
Figure 4.

Localization performance RMS error for BAI versus CROS subjects for the 500Hz 1./3 octave (A), 4kHz 1/3 octave noise (B), and voiced ‘hey’ (C), are shown respectively. Aided responses are plotted against normative data.
When speech was directed at the poorer ear and noise directed at the better ear (90/270) a significant improvement in signal-to-noise ratio loss from the unaided to aided condition for monaural listeners was observed (p<0.0001, Figure 5a). Both BAI and CROS subject groups significantly improved on tasks of speech perception in noise from the unaided to aided condition (p<0.0001) and there was no significant difference between BAI and CROS subject groups for unaided or aided performance (Figure 5b).
Figure 5.

Speech in noise performance by individual (A) and subject group (B) are represented in SNR loss where the smaller the dB value indicates improved performance. Results demonstrate significant improvement from the unaided to aided condition for both BAI and CROS subject groups (p < 0.0001), however no significant difference is observed for aided performance between BAI and CROS subject groups (p > 0.05).
For subjective assessment of spatial perception BAI users reported significant improvement in spatial perception from the unaided to the aided condition (p < 0.0001), while CROS users did not report improved spatial perception (p = 0.07). Despite this, no significant difference was observed between CROS or BAI users for the spatial domain overall with the exception of CROS users reporting a decrease in ability to tell the distance of the speaker (spatial domain question 15, p = 0.01). Subjects were also asked to rate their ability on 14 speech items using the same visual analog scale. Both BAI (p < 0.001) and CROS (p = 0.0004) groups reported significant benefit in the aided condition for the speech domain; however, no significant difference was observed between CROS or BAI users.
The GHABP was used to subjectively measure initial disability, handicap, use, benefit, residual disability, and satisfaction for each subject group. There was a significant improvement in selfreported disability for monaural listeners (p < 0.0001). BAI users demonstrated a significantly higher initial disability (p = 0.01) and handicap (p = 0.01) than CROS users although no significant difference between BAI and CROS users was observed for use, benefit, residual disability and satisfaction (Figure 6).
Figure 6.

Results of the GHABP for BAI and CROS users are displayed on a 100 point scale demonstrating significant increase in initial disability and handicap for BAI users over CROS users (p = 0.01). No significant difference between groups is observed for the post treatment use, benefit, residual disability, and satisfaction domains (p > 0.05).
DISCUSSION
Early reports of benefit in monaural listeners with CROS hearing devices suggested that lifting of the head-shadow resulted in significant benefit to this population (13). However, this treatment was plagued by acoustic limitations that resulted in complaints of poor sound quality and discomfort with device use (12,13) ultimately leading to a lack of acceptance for CROS as a treatment solution by individuals with unilateral severe-profound sensorineural hearing loss. The introduction of implantable bone conduction solutions overcame much of the acoustic limitations of CROS hearing aids. BAIs eliminated the occlusion of the normal hearing ear that occurred from having to wear a hearing aid in both ears. CROS hearing aids were subject to timing delays that occurred when the signal was routed from the microphone to the transmitter worn in the better hearing ear. This resulted in complaints of poor sound quality, specifically an “echo”. Because BAIs rely on bone conduction to transcranially transmit the acoustic signal, timing delays are indiscernible resulting in a clear and more natural signal. Other benefits included the aesthetic appeal of being able to hide the BAI processor under the hair. Several comparison studies have demonstrated these benefits of BAI over CROS hearing aids in monaural listeners (8,10,15,16). As a result, BAIs emerged as the optimal solution for remediation of hearing loss in monaural listeners. In recent years, several technological improvements have been made to the CROS hearing aid system, overcoming much of the early physical, aesthetic, and acoustical limitations of these devices. In early CROS systems the acoustic signal was transferred either by a wire connecting the microphone to the receiver worn on the normal hearing ear, or wirelessly by an amplitude or frequency modulated signal. This required devices to be large enough to house the internal components required to route the signal around the head, often resulting in an aversion to the aesthetics and comfort of CROS hearing aids. Additionally these early systems were subject to interference from electromagnetic fields such as security systems or fluorescent lighting, resulting in intermittent function or distortion. Current CROS technology allows for wireless HiBAN (Hearing instrument Body Area Network, Phonak, LLC) signal transmission, which significantly reduced signal transmission time from earlier technology. The result is a clear signal without any perceivable delay or audible “echo”. These changes also allowed for smaller more discrete housing resulting in improved aesthetics. Technological advances have allowed for use of an open fit earpiece, whereas early CROS systems required occlusion of the ear. This results in minimal alteration to ear canal resonance and allows for natural sound transmission into the normal ear, thereby overcoming the occlusion effect experienced with earlier CROS hearing aids.
Mean degree of error for horizontal localization studies indicates monaural listeners performed at chance in both the unaided and aided condition for voiced ‘hey’, 1/3 octave 500 Hz, or 1/3 octave 4000 Hz stimuli(26). Close review of the results (Figures 2–4) demonstrate more than 50° mean error for monaural listeners regardless of condition or device. Monaural listeners deviate significantly from normal performance, which approximates 6° mean error for the broadband signal, voiced ‘hey’. These results are consistent with previous reports(8,10,15,16) and demonstrate that despite the considerable advancements in treatment solutions for monaural listeners, localization ability remains impaired. These results are expected as both BAI and CROS systems rely on monaural processing of a bilaterally presented signal. Neither the BAI nor the CROS system restore binaural hearing, preventing access to critical timing and level cues. Despite this, some have reported that monaural listeners do localize in the horizontal plane(18). This is attributed to the head shadow effect and the resulting sound level differences that occur for sounds arriving at the impaired ear versus the normal hearing ear(18). Others have shown that some monaural listeners are able to use spectral cues to improve horizontal localization ability, although large inter-subject variability is observed(17). In our clinical experience we have observed that some monaural listeners will anecdotally report perceived localization ability. The subjective data obtained by the SSQ supported this with BAI users reporting a significant improvement in spatial perception. It is possible that subjects are gaining some ability to lateralize acoustic signals in the horizontal plane, perhaps by perceived changes in level differences from the aided to unaided condition. However, neither BAI nor CROS users demonstrated improved lateralization in aided condition for objective measures of localization ability. Further, monaural spectral cues would not impact changes from the unaided to aided condition. While there was no overall statistical difference in spatial perception between BAI or CROS subject groups on the SSQ, it is unclear why BAI users reported significant improvement from the unaided condition while CROS users did not. It is possible that bone conducted stimuli resulted in changes for better ear performance that are misinterpreted by the user as a change in localization ability. Review of better ear localization ability revealed it was not negatively affected in aided condition for either group. Of interest, BAI users demonstrated a higher initial disability and handicap index suggesting that perhaps those who are more debilitated by their hearing loss are more likely to seek an invasive treatment solution for their hearing. It is possible that the difference in subjective report in these two groups may be a function of this increased disability and handicap observed in BAI users.
We have demonstrated that pre-operative assessment of speech perception in noise ability serves as a good predictor of post-operative outcomes with BAIs (27). Others have used tests of speech perception in noise as the primary measure for benefit in both CROS and BAI devices (8,10,15,16). These studies also showed that performance for the speech poorer ear, noise better ear (90°/270° azimuth) condition demonstrated the greatest degree of impairment in the unaided condition as well as the greatest degree of improvement in the aided condition. Given these findings, clinical assessment of both BAI and CROS hearing devices using this protocol provides an accurate reflection of performance changes and estimation of benefit in this population. The results of this study found that both BAI and CROS devices provide significant benefit for listening in noise ability and no significant difference is seen between devices. It is possible that differences in microphone placement for the two devices may result in variations in outcomes, but our results did not support this. For our study groups, subjects performed almost equal with average unaided performance at 9.6 dB signal-to-noise ratio loss for BAI users and 8.8 dB signal-to-noise ratio loss for CROS users. Likewise, aided performance averaged at 1.4 dB signal-to-noise ratio loss for BAI users and 1.1 dB for CROS users. This represents roughly a 9dB improvement in signal to noise ratio for both groups. More importantly it demonstrates a shift from a moderate SNR loss to normal performance where values less than 3dB on the QuickSIN™ is consistent with published norms for normal hearing listeners(21).
These findings clearly demonstrate that monaural listeners receive significant objective benefit as measured by behavioral tests of speech perception in noise for both BAI and CROS devices. In fact, individuals with severe-to profound unilateral hearing loss were equally satisfied with treatment regardless of the modality. Our findings demonstrate that new wireless CROS technology has resolved many of the previous limitations that led to reduction in behavioral and subjective outcomes in monaural listeners. Subjective assessment reveals a high satisfaction and use rate among CROS hearing aid users as well as a significant reduction in disability and handicap. Despite the homogeneous nature of our group data, as with other studies in monaural listeners (22,27), we observed a high degree of inter-subject variability among our subjects. A limitation of this study is that unlike the CROS subjects, the BAI subjects did not all use the same processor. Processors varied both in make and model (Figure 5a). While the variability may be attributed to differences in the processor such as microphone characteristics, prescriptive methods for gain and compression, etc., our previous work has confirmed that this inter-subject variability exists in monaural listeners prior to treatment(22,27) and suggests that variations in performance are individual specific. Specifically, the degree of benefit associated with lifting the head-shadow does not vary within the same subject, is largely independent of device features, and is characterized by each individual’s auditory processing capabilities. We have demonstrated that the current protocol (22) is a good predictor of performance in monaural listeners using BAIs, and combined with the presented subjective assessment tools this protocol provides the ability to predict post-treatment benefit(27). This study supports that this protocol can also be successfully applied to CROS users for assessment of benefit and validation of performance. Without any observable aided benefit, assessment of localization ability does not provide a clinical utility in assessment of benefit for these treatment options. Behavioral assessment of performance on tasks of speech-in-noise performance combined with subjective assessment provides clinically applicable individualized pre-treatment predictors regarding invasive versus non-invasive device selection.
Results from 13 CROS and 14 BAI subjects suggests that: 1) BAI and CROS do not provide any localization benefit in the horizontal plane for monaural listeners (Figure 2), and 2) there is no significant difference between systems (Figure 2). The study groups did not show improved lateralization in aided condition and better ear performance was not negatively affected in aided condition. Preliminary data for SIN performance for the speech poorer ear, noise better ear (90°/270° azimuth) demonstrated significant improvement on SIN tasks from unaided to aided condition (p < 0.0001) for both BAI and CROS groups, however no significant difference observed for aided performance between groups.
A limitation of the present study is the inter-subject design. Our lab is currently in the process of conducting an intra-subject comparison of CROS versus BAI outcomes that we anticipate to present to this audience in the future. This additional work allows each subject to serve as his or her own control, thereby reducing the potential impact by the inter-subject variability observed in monaural listeners.
Conclusions
Our data demonstrate that monaural listeners receive significant improvements in speech-in-noise ability for both BAI and CROS hearing aid systems. However, there is no significant difference between BAI and CROS systems for objective measures of speech-in-noise performance. Monaural listeners perform at chance for localization ability. BAI and CROS hearing devices do not provide any localization benefit in the horizontal plane for monaural listeners and there is no significant difference between BAI and CROS on tests of speech in noise and localization ability. Subjective outcomes suggest some patients do perceive improved spatial perception with the BAI and CROS hearing devices despite objective results but there is no significant difference in BAI vs CROS for subjective outcomes.
Footnotes
Presented at Association for Research in Otolaryngology, 2015 Baltimore, MD
References
- 1.Giolas TG, Wark DJ. Communication problems associated with unilateral hearing loss. The Journal of speech and hearing disorders. 1967;32:336–43. doi: 10.1044/jshd.3204.336. [DOI] [PubMed] [Google Scholar]
- 2.Sargent EW, Herrmann B, Hollenbeak CS, et al. The minimum speech test battery in profound unilateral hearing loss. Otology and Neurotology. 2001;22:480–6. doi: 10.1097/00129492-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Silverman CA, Silman S, Emmer MB, et al. Auditory deprivation in adults with asymmetric, sensorineural hearing impairment. Journal of the American Academy of Audiology. 2006;17:747–62. doi: 10.3766/jaaa.17.10.6. [DOI] [PubMed] [Google Scholar]
- 4.Sano H, Okamoto M, Ohhashi K, et al. Quality of life reported by patients with idiopathic sudden sensorineural hearing loss. Otology and Neurotology. 2013;34:36–40. doi: 10.1097/MAO.0b013e318278540e. [DOI] [PubMed] [Google Scholar]
- 5.Augustine AM CS, Thenmozhi K, Rupa V. Assessment of auditory and psychosocial handicap associated with unilateral hearing loss among Indian patients. Indian J Otolaryngol Head Neck Surg. 2013;65:120–5. doi: 10.1007/s12070-012-0586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hol MK, Bosman AJ, Snik AF, et al. Bone-anchored hearing aid in unilateral inner ear deafness: a study of 20 patients. Audiology & neuro-otology. 2004;9:274–81. doi: 10.1159/000080227. [DOI] [PubMed] [Google Scholar]
- 7.Hol MK, Kunst SJ, Snik AF, et al. Bone-anchored hearing aids in patients with acquired and congenital unilateral inner ear deafness (Baha CROS): clinical evaluation of 56 cases. The Annals of otology, rhinology, and laryngology. 2010;119:447–54. doi: 10.1177/000348941011900704. [DOI] [PubMed] [Google Scholar]
- 8.Lin LM, Bowditch S, Anderson MJ, et al. Amplification in the rehabilitation of unilateral deafness: speech in noise and directional hearing effects with bone-anchored hearing and contralateral routing of signal amplification. Otology and Neurotology. 2006;27:172–82. doi: 10.1097/01.mao.0000196421.30275.73. [DOI] [PubMed] [Google Scholar]
- 9.Wazen JJ, Spitzer JB, Ghossaini SN, et al. Transcranial contralateral cochlear stimulation in unilateral deafness. Otolaryngology-Head and Neck Surgery. 2003;129:248–54. doi: 10.1016/S0194-5998(03)00527-8. [DOI] [PubMed] [Google Scholar]
- 10.Niparko JK, Cox KM, Lustig LR. Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otology and Neurotology. 2003;24:73–8. doi: 10.1097/00129492-200301000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Harford E, Barry J. A Rehabilitative Approach to the Problem of Unilateral Hearing Impairment: The Contralateral Routing of Signals Cros. The Journal of speech and hearing disorders. 1965;30:121–38. doi: 10.1044/jshd.3002.121. [DOI] [PubMed] [Google Scholar]
- 12.Williams VA, McArdle RA, Chisolm TH. Subjective and objective outcomes from new BiCROS technology in a veteran sample. Journal of the American Academy of Audiology. 2012;23:789–806. doi: 10.3766/jaaa.23.10.5. [DOI] [PubMed] [Google Scholar]
- 13.Ericson H1 SI, Högset O, Devert G, Ekström L. Contralateral routing of signals in unilateral hearing impairment. A better method of fitting. Scand Audiol. 1988;17:111–6. doi: 10.3109/01050398809070699. [DOI] [PubMed] [Google Scholar]
- 14.FDA. Summary and Certification. 510(k) Summary Number K0218372002. [Google Scholar]
- 15.Bosman AJ, Hol MK, Snik AF, et al. Bone-anchored hearing aids in unilateral inner ear deafness. Acta oto-laryngologica. 2003;123:258–60. doi: 10.1080/000164580310001105. [DOI] [PubMed] [Google Scholar]
- 16.Wazen JJ, Ghossaini SN, Spitzer JB, et al. Localization by unilateral BAHA users. Otolaryngology–head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2005;132:928–32. doi: 10.1016/j.otohns.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 17.Agterberg MJ, Hol MK, Van Wanrooij MM, et al. Single-sided deafness and directional hearing: contribution of spectral cues and high-frequency hearing loss in the hearing ear. Frontiers in neuroscience. 2014;8:188. doi: 10.3389/fnins.2014.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Wanrooij MM, Van Opstal AJ. Contribution of head shadow and pinna cues to chronic monaural sound localization. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2004;24:4163–71. doi: 10.1523/JNEUROSCI.0048-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma) American Academy of Otolaryngology-Head and Neck Surgery Foundation, INC. Otolaryngology-Head and Neck Surgery. 1995;113:179–80. doi: 10.1016/S0194-5998(95)70101-X. [DOI] [PubMed] [Google Scholar]
- 20.Dillon H. Hearing Aids. New York: Thieme; 2001. pp. 434–50. [Google Scholar]
- 21.Killion MC, Niquette PA, Gudmundsen GI, et al. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. The Journal of the Acoustical Society of America. 2004;116:2395–405. doi: 10.1121/1.1784440. [DOI] [PubMed] [Google Scholar]
- 22.Snapp HA, Fabry DA, Telischi FF, et al. A clinical protocol for predicting outcomes with an implantable prosthetic device (Baha) in patients with single-sided deafness. Journal of the American Academy of Audiology. 2010;21:654–62. doi: 10.3766/jaaa.21.10.5. [DOI] [PubMed] [Google Scholar]
- 23.Blauert J. Spatial Hearing: THe Psychophysics of Human Sound Localization. London, England: The MIT Press; 1997. [Google Scholar]
- 24.Middlebrooks JC, Green DM. Sound localization by human listeners. Annual review of psychology. 1991;42:135–59. doi: 10.1146/annurev.ps.42.020191.001031. [DOI] [PubMed] [Google Scholar]
- 25.Letowski T, Letowski S. Localization Error: Accuracy and Precision of Auditory Localization. http://www.intechopen.com/books/advances-in-sound-localization/localization-error-accuracy-and-precision-of-auditory-localization2011.
- 26.Grantham DW, Ashmead DH, Ricketts TA, et al. Horizontal-plane localization of noise and speech signals by postlingually deafened adults fitted with bilateral cochlear implants. Ear and hearing. 2007;28:524–41. doi: 10.1097/AUD.0b013e31806dc21a. [DOI] [PubMed] [Google Scholar]
- 27.Snapp H, Angeli S, Telischi FF, et al. Postoperative validation of bone-anchored implants in the single-sided deafness population. Otology and Neurotology. 2012;33:291–6. doi: 10.1097/MAO.0b013e3182429512. [DOI] [PubMed] [Google Scholar]


