Abstract
Objective
Few studies have examined unique factors predicting psychological distress among sexual minority (i.e., lesbian and bisexual) women post breast cancer diagnosis. The present study assessed the association of minority stress and psychosocial resource factors with depression and anxiety symptoms among sexual minority breast cancer survivors.
Methods
201 sexual minority women who had ductal carcinoma in situ (DCIS) or stage I-IV breast cancer participated in this study through the Love/Avon Army of Women (AOW). Self-report questionnaires were used to assess demographic and clinical factors, minority stress factors (discrimination, minority identity development, outness), psychosocial resources (resilience, social support), and psychological distress (anxiety and depression). These factors were included in a structural equation model, testing psychosocial resources as mediators between minority stress and psychological distress.
Results
There were no significant differences noted between lesbian and bisexual women. The final structural equation model demonstrated acceptable fit across all sexual minority women, χ2 = 27.83, p > 0.05; confirmatory fit index = 0.97, root-mean-square error of approximation = 0.04, Tucker-Lewis Index = 0.93. The model accounted for significant variance in psychological distress (56%). Examination of indirect effects confirmed that exposure to discrimination was associated with distress via association with resilience.
Conclusions
Factors unique to sexual minority populations, such as minority stress, may be associated with higher rates of psychological distress among sexual minority breast cancer survivors. However, presence of psychosocial resources may mediate relationships with distress in this population; enhancement of resilience, in particular, could be an aim of psychological intervention.
Keywords: Cancer, Minority Stress, Psychological Distress, Women, Lesbian, Bisexual
Background
Breast cancer can have a pervasive effect on a woman’s psychological functioning (Jassim, Whitford, Hickey, & Carter, 2015; Lester et al., 2015), and psychological outcomes may differ for certain subgroups of women, such as sexual minority (i.e., lesbian, bisexual, female-partnered) women. Both a breast cancer diagnosis and the process of undergoing treatment can result in psychological distress, including symptoms of depression and anxiety, among women in general (Donovan, Gonzalez, Small, Andrykowski, & Jacobsen, 2014; Saboonchi et al., 2014). Up to 40% of breast cancer survivors experience depression and/or anxiety within the first year post-diagnosis and also report concerns about cancer recurrence and mortality (Von Ah & Kang, 2008). While these concerns typically decrease over time, up to 25% of cancer survivors may experience depression or anxiety five years or more post-diagnosis (Maass, Roorda, Berendsen, Verhaak, & de Bock, 2015; Saboonchi et al., 2014). Elevated levels of psychological distress are associated with increased risk of cancer-related morbidity and mortality (Hamer, Chida, & Molloy, 2009; Mao et al., 2007), and models that can identify women at risk of long-term distress are needed.
The research literature has only just begun to focus on outcomes of breast cancer diagnosis and treatment among sexual minority women in the United States (Bare, Margolies, & Boehmer, 2014; Boehmer, 2015). With a few exceptions, these studies have compared quality of life and psychological outcomes between sexual minority women and their heterosexual counterparts (Boehmer, Glickman, & Winter, 2012; Jabson & Bowen, 2014; Jabson, Donatelle, & Bowen, 2011; Kamen, Mustian, Dozier, Bowen, & Li, 2015). The results of these studies have been mixed. Comparisons between sexual minority and heterosexual survivors have indicated that prevalence of psychological distress may be similar between the two groups, but that unique factors, such as minority stress, may predict distress for sexual minority but not heterosexual women (Boehmer, Glickman, Milton, & Winter, 2012; Boehmer, Glickman, & Winter, 2012).
Minority stress, or the chronic and cumulative stress to which individuals with stigmatized sexual minority identities are exposed, comprises experiences of discrimination, minority identity development, internalized homophobia, and concealment of one’s sexual minority identity due to fear of judgment (Meyer, 2003). Previous research has indicated that sexual minority women experience discrimination at higher rates than their heterosexual counterparts (Lehavot & Simoni, 2011), and that exposure to discrimination may explain disparities in mental health outcomes among sexual minority women (Cochran, Mays, & Sullivan, 2003; Fredriksen-Goldsen, Kim, Barkan, Balsam, & Mincer, 2010; Meyer, 1995). In addition to exposure to discrimination from distal sources, sexual minority women must proximally integrate their sexual identity and same-sex sexual attraction into their sense of selves, a process made challenging by the predominantly heterosexual models of identity and relationships to which a woman may be exposed (Peterson & Gerrity, 2006). Acceptance of anti-gay messages espoused by society (i.e., internalized homophobia) and development of a negative sense of self as a sexual minority individual has been linked with psychological distress (Kertzner, Meyer, Frost, & Stirratt, 2009). Finally, regardless of exposure to discrimination or sexual minority identity development, sexual minority women must make decisions about whether and to whom they are going to disclose their sexual identity. This process, often referred to as “coming out,” can be stressful, particularly in the context of cancer (Boehmer & Case, 2004). Given that cancer treatment requires socially intimate interactions with multiple new providers in new clinical settings, and that the beliefs of individual providers or the culture of a healthcare system may not be immediately apparent, sexual minority cancer patients must make a decision about coming out to each provider with whom they interact and may be concerned that their care will be compromised if a provider feels negatively about their sexual identity (Kamen, Smith-Stoner, Heckler, Flannery, & Margolies, 2015).
The minority stress model as originally conceptualized also incorporated ameliorating factors that may reduce the impact of minority stress experiences on health (Meyer, 2003). One of these ameliorating factors, psychological resilience, is a complex construct which encompasses an individual’s ability to adapt to stress. Previous literature has indicated that effective coping and emotion regulation in the face of discrimination may build resilience among sexual minority individuals, and may thereby be associated with better psychological health (Kwon, 2013). Resilience is bidirectionally related to perception of and satisfaction with social support (DiFulvio, 2011). Sexual minority women who report more social support report reduced reactivity to discrimination (Szymanski, Chung, & Balsam, 2001), and survivors of cancer who report more social support also report reduced distress (Kamen, Mustian, Heckler, et al., 2015). While recent expansions of the minority stress theory have indicated that psychological processes may mediate the effect of minority stress on psychological functioning, many of these studies have focused on negative and exacerbating processes such as rumination and emotion dysregulation (Hatzenbuehler, 2009). Few studies have examined factors such as resilience and receipt of social support in the context of minority stress and psychological functioning among sexual minority people (Kwon, 2013).
Furthermore, only a handful of preliminary studies have examined psychological outcomes, minority stress, and positive psychosocial resources among sexual minority breast cancer survivors. In a national convenience sample of sexual minority breast cancer survivors, Jabson et al. (2011) reported that perceived discrimination and social support were associated with quality of life among sexual minority breast cancer survivors. This study did not include a comprehensive assessment of minority stress, psychosocial resources beyond social support, or psychological distress outcomes. Similarly, Boehmer et al. (2013) showed that minority stress factors were associated with psychological distress among lesbian and bisexual women with early stage breast cancer, but this study specifically excluded women with advanced (e.g., recurrent or metastatic) breast cancer and did not examine the mediating role of psychosocial resources. Based on research with sexual minority populations in general, development of resilience could mediate the impact of minority stress on psychological distress among sexual minority breast cancer survivors by reducing reactivity and increasing coping (Kwon, 2013; McElroy, Wintemberg, Cronk, & Everett, 2016). Perception of and satisfaction with social support in turn could be related to discrimination, degree of outness and development of sexual minority identity through stronger bonds to the LGBT community, and could mediate the impact of these factors on psychological distress (Legate, Ryan, & Weinstein, 2012). Studies that examine psychological distress in sexual minority women specifically, and that incorporate both minority stress and psychological resources, would enable more accurate screening and better tailored interventions for this underserved and at-risk group (Boehmer et al., 2013; Kamen et al., 2016).
The objective of the current study was to evaluate a model of psychological distress among sexual minority breast cancer survivors derived from the existing minority stress literatures (Hatzenbuehler, 2009; Meyer, 1995, 2003). Analyses assess the unique contribution of both minority stress factors (i.e., discrimination, minority identity, and disclosure of minority identity or “outness”) and psychosocial resources (i.e., resilience, social support) to variance in self-report of depression and anxiety, controlling for demographic and clinical variables. The study’s first hypothesis was that discrimination and negative minority identity would be associated with elevated psychological distress, while greater outness, resilience, and social support would be associated with lower psychological distress. A second hypothesis was that psychosocial resources would mediate the statistical association between minority stress and two psychological measures of distress: depression and anxiety. See Figure 1 for the hypothesized mediation model.
Figure 1.
Hypothesized associations between manifest and latent variables.
Methods
Design
The parent study from which this dataset was drawn was cross-sectional, survey-based, and leveraged the Love/Avon Army of Women (AOW), an online recruitment resource designed to partner a diverse group of women with the research community in an effort to accelerate breast cancer research (Stanton et al., 2013). The parent study used the AOW for a targeted recruitment of heterosexual and sexual minority adults (18+ years of age) with breast cancer of any stage. Recruitment and study procedures were approved by the IRB of both Boston University and the University of Rochester.
Interested participants contacted the parent study’s research team and underwent a 5 minute screening process, which involved questions about cancer and treatment history, self-identification of sexual orientation (lesbian, bisexual, heterosexual, other), and preferred gender of sexual partner (female, male, both, or other). Survivors who were eligible and who provided verbal consent were then administered a 35 minute long phone interview. Participants for the current study were limited to sexual minority breast cancer survivors who had ductal carcinoma in situ (DCIS) or stage I-IV breast cancer, including recurrent or metastatic cancers.
Measures
Demographic and clinical factors
Participants were asked their age, racial/ethnic background, partnership status, highest level of education attained, and income. They were asked to define their sexual orientation and their preferred gender of sexual partner. Only participants who identified as lesbian/bisexual or reported preferring to partner with women were included in the current study. Participants were also asked their date of cancer diagnosis (used to calculate time from diagnosis date to interview date), cancer stage at time of interview, and type of cancer treatment(s) received (i.e., surgery, chemotherapy, radiotherapy).
Minority stress factors
Discrimination, minority identity, and outness were assessed with three measures. Discrimination was assessed by asking whether participants had ever felt discriminated against because of their sexual orientation or gender (yes to either type of discrimination vs. neither type of discrimination; Stuber, Galea, Ahern, Blaney, & Fuller, 2003); both sexual orientation and gender were included based on previous research showing that sexual minority women are more likely to experience gender-based discrimination than their heterosexual counterparts (Boehmer, Glickman, Milton, et al., 2012). Minority identity was assessed using the LGB Identity Scale, which measures five facets of sexual minority identity: Identity Confusion, Internalized Homophobia, Need for Privacy, Need for Acceptance, and Difficult Process (example item: “I would rather be straight if I could”; Mohr & Fassinger, 2000). The latter four subscales were summed to create a total score for Negative Identity, as indicated by factor analysis conducted by the scale’s authors. Each of the subscales had appropriate internal consistency (α=0.68–0.79), as did the Negative Identity scale (α=0.85). Finally, the Outness Inventory was used to assess the number of different types of people to whom a woman had disclosed her sexual minority identity (e.g., “your co-workers,” “your straight friends”; Mohr & Fassinger, 2000). The set of items for this inventory had appropriate internal consistency (α=0.72).
Psychosocial resources
Resilience and social support were assessed with two measures. The Resilience Scale-14 was used to measure resilience, defined as “emotional stamina” and adaptability in the face of stress (example item: “My belief in myself gets me through hard times”; Wagnild & Young, 1993). This scale was developed and normed specifically with a sample of women (Wagnild & Young, 1990) but has since been validated in broader populations (Wagnild, 2009). It had good internal consistency in the current study (α=0.87). The six item short form of the Interpersonal Support Evaluation List (ISEL-SF) was used to measure perceived availability of instrumental support, material aid, people to talk to about personal problems, and people to engage in activities with (example item: “When I feel lonely, there are several people I can talk to”; Arena et al., 2006; McGregor et al., 2001). This measure demonstrated appropriate internal consistency (α=0.67).
Psychological distress
Depression and anxiety were measured using the Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983). This instrument has been widely used to assess psychological distress in cancer populations. For this study’s primary analyses, depression and anxiety symptoms were evaluated separately and as continuous scores. Consistent with previous research, individuals were also categorized as having borderline abnormal depression or anxiety if their depression or anxiety subscale scores were 8–10, and clinically significant depression if their depression or anxiety subscale scores were 11 or greater (Singer et al., 2009). The depression (α=0.78) and anxiety (α=0.82) subscales each demonstrated appropriate internal consistency.
Statistical Analyses
Descriptive statistics were computed for demographic and clinical characteristics as well as psychological distress and all minority stress and coping factors using SPSS 22.0 (IBM Corp., Chicago, IL). Variables were compared between lesbian and bisexual women to assess differences between subgroups of sexual minority women. To test the first hypothesis, univariate associations were calculated between demographic and clinical variables and psychological distress (depression and anxiety), using linear regression; categorical variables were dummy-coded with a reference category. Next, associations were calculated between minority stress, psychological resources, and psychological distress, using partial correlations controlling for demographic and clinical factors significantly associated with depression and/or anxiety in univariate analyses.
To test the second hypothesis, assessing whether the association of minority stress with psychological distress might be statistically mediated by coping factors, path analysis was conducted using structural equation modeling (SEM) in AMOS 22.0 (IBM Corp., Chicago, IL) with maximum likelihood parameter estimation (Raykov & Marcoulides, 2006). SEM allowed for construction of a latent variable for psychological distress, comprised of both depression and anxiety as measured by the HADS. SEM also allowed for simultaneous modeling of direct effects of independent variables on psychological distress and indirect effects of minority stress factors through psychosocial resources. Indirect effects were calculated as the product of path coefficients from minority stress factors to psychological resources and from resources to distress. All assumptions of SEM were checked before beginning analyses. Expanding on the approach recommended by MacKinnon (2008), mediation was assessed in a three-step process. First, the total effect (direct and indirect) of each minority stress variable on psychological distress was examined. Next, the direct effect of each minority stress variable on each psychosocial resource variable was examined. Finally, the specific indirect effect of each minority stress variable on psychological distress through each psychosocial resource variable and the specific direct effect of each minority stress variable on psychological distress was examined. A significant specific indirect effect was taken as evidence of mediation, with complete mediation evident in the context of a significant specific indirect effect and a non-significant direct effect. 95% confidence intervals for each effect were calculated using bootstrapping with 2,000 draws. Model fit was evaluated using omnibus χ2, the comparative fit index (CFI), the Tucker-Lewis Index (TLI), and the root mean square error of approximation (RMSEA). Models were considered to have good fit if the χ2 was nonsignificant (p>0.05), the CFI was greater than 0.95, the TLI was greater than 0.90, and the RMSEA was less than 0.05 (Raykov & Marcoulides, 2006).
To address the possibility of confounding, all demographic and clinical variables were evaluated first for statistical association with psychological resources or psychological distress and second for theoretical likelihood of confounding the relationships between minority stress and psychological distress, minority stress and psychological resources, or psychological resources and psychological distress. Confounders that were statistically associated or theoretically likely were included in the model as predictors of psychological resources, psychological distress, or both, as indicated by theory and the existing minority stress literature (Boehmer, Glickman, & Winter, 2012; Lehavot & Simoni, 2011; Meyer, 2003). Categorical demographic variables were entered into the model using dummy codes and a reference category as indicated in Table 1.
Table 1.
Descriptive statistics for demographic and clinical factors and univariate association (via linear regression) with depression and anxiety (N=201)
| Variable | Association with depression | Association with anxiety | |
|---|---|---|---|
| Age, Mean (SD) | 53 (8.48) | −0.07 | −0.14* |
| Sexual Orientation, n (%) | |||
| Lesbian a | 172 (85.6) | -- | -- |
| Bisexual | 29 (14.4) | −0.04 | 0.01 |
| Race, n (%) | |||
| White a | 177 (88.1) | -- | -- |
| Other/non-White | 24 (11.9) | 0.03 | 0.04 |
| Ethnicity, n (%) | |||
| Non-Hispanic a | 193 (96.0) | -- | -- |
| Hispanic/Latina | 8 (4.0) | −0.01 | −0.12 |
| Marital status, n (%) | |||
| Never married | 73 (36.3) | 0.08 | −0.05 |
| Married a | 86 (42.8) | -- | -- |
| Separated/divorced/widowed | 36 (17.9) | 0.26** | −0.01 |
| Unknown | 6 (3.0) | 0.14 | 0.03 |
| Education, n (%) | |||
| Some college or less | 49 (24.4) | 0.16* | 0.05 |
| College degree | 66 (32.8) | 0.22** | 0.21** |
| Graduate degree a | 86 (42.8) | -- | -- |
| Employment, n (%) | |||
| Unemployed | 62 (30.8) | 0.15* | 0.01 |
| Employed/self-employed a | 139 (69.2) | -- | -- |
| Income, n (%) | |||
| Less than $30,000/year | 49 (24.4) | 0.17** | 0.04 |
| $30,000–$70,000/year a | 79 (39.3) | -- | -- |
| Over $70,000/year | 69 (34.3) | −0.06 | −0.08 |
| Unknown | 4 (2.0) | −0.03 | −0.11 |
| Time since cancer dx, Mean (range) | 4.56 (0–27) | −0.10 | −0.02 |
| Highest stage of cancer, n (%) | |||
| Ductal carcinoma in situ a | 38 (18.9) | -- | -- |
| Stage I | 63 (31.3) | −0.09 | 0.03 |
| Stage II | 64 (31.8) | −0.04 | 0.07 |
| Stage III | 15 (7.5) | 0.05 | 0.05 |
| Stage IV | 16 (8.0) | 0.06 | 0.02 |
| Unknown | 5 (2.5) | 0.06 | 0.06 |
| Breast cancer recurred, n (%) | 31 (15.4) | −0.01 | −0.08 |
| Other cancer dx, n (%) | 42 (20.9) | 0.04 | 0.09 |
| Type of cancer treatment, n (%) | |||
| Lumpectomy | 115 (57.2) | <0.01 | 0.11 |
| Mastectomy/Bilateral mastectomy | 120 (59.7) | 0.02 | −0.09 |
| Chemotherapy | 119 (59.2) | 0.12** | 0.02 |
| Radiotherapy | 114 (56.7) | −0.05 | 0.06 |
| Hormone therapy | 139 (69.2) | −0.01 | 0.04 |
Note.
. reference category;
p < .05 (two-tailed);
p < .01 (two-tailed)
Results
Participant characteristics
A total of 201 sexual minority women consented to participate in the telephone interview; 86% (n=172) identified as lesbian, while 14% (n=29) identified as bisexual. See Table 1 for demographic details. The mean age of all cancer survivors in this sample was 53 years (range 28 to 74). The majority (88%) were non-Hispanic White. The modal level of education was a graduate school degree (42%) and the majority of participants (73%) made over $30,000 a year. Over half of the sample (66%) was partnered. The majority of participants (63%) had stage I or II breast cancer. Most participants had undergone surgery (97%), chemotherapy (59%), radiotherapy (57%), and/or hormone treatment (70%). On average, survivors had been first diagnosed with breast cancer 5 years ago (range 0 to 27). No statistically significant differences were detected in demographic characteristics between lesbian and bisexual cancer survivors.
In univariate associations, the demographic characteristics of being separated/divorced/ widowed (vs. married), having a college or less than college education (vs. graduate education), being unemployed, having an income less than $30,000 per year (vs. $30,000-$70,000 per year), and having received chemotherapy were all positively associated with depression at the p < 0.05 level. Age was the only demographic characteristic negatively associated with anxiety, while having a college education (vs. graduate education) was positively associated with anxiety at the p < 0.05 level. See Table 1.
Psychological distress, minority stress factors, and coping factors
Means and standard deviations (SD) for psychological distress, minority stress factors, and psychosocial resources are presented in Table 2. The mean score for depression symptoms was 3.97 (SD=3.36); 10.9% of participants (n=22) reported borderline abnormal depression (8–10), while 4.5% (n=9) reported clinically significant depression (>11). The mean score for anxiety symptoms was 5.50 (SD=3.95); 15.9% of participants (n=32) reported borderline abnormal anxiety (8–10), while 12.9% (n=26) reported clinically significant anxiety (>11). A total of 47.8% of the sample (n=96) had experienced discrimination based on their sexual minority identity, 45.8% (n=92) had experienced discrimination based on their gender, and 50.2% (n=101) had experienced discrimination based on their sexual minority identity, gender, or both. See Table 2. No statistically significant differences in psychological distress, minority stress factors, or coping factors were detected between lesbian and bisexual cancer survivors (data not shown).
Table 2.
Descriptive statistics for minority stress, psychosocial resource, and psychological distress factors (N=201).
| Variable | ||
|---|---|---|
| Discrimination | n (%) | |
| Based on sexual minority | 96 (47.8%) | |
| Based on gender | 92 (45.8%) | |
| Based on one or both | 101 (50.2%) | |
| Minority Identity | Mean (SD) | Range |
| Internalized Homophobia | 1.48 (0.75) | 1–7 |
| Need for Privacy | 3.66 (1.40) | 1–7 |
| Need for Acceptance | 1.88 (0.90) | 1–7 |
| Difficult Process | 2.34 (1.28) | 1–7 |
| Negative Identity | 2.34 (0.79) | 1–7 |
| Outness, Mean (SD) | 6.19 (1.23) | 1–7 |
| Resilience, Mean (SD) | 85.94 (8.75) | 14–98 |
| Social Support, Mean (SD) | 22.30 (2.32) | 6–24 |
| Depression, Mean (SD) | 3.97 (3.36) | 0–21 |
| Anxiety, Mean (SD) | 5.50 (3.95) | 0–21 |
In testing the first hypothesis, discrimination, resilience, and social support were significantly associated with depression using bivariate partial correlations controlling for age, education, income, employment, and receipt of chemotherapy. Discrimination, negative identity (from the Minority Identity scale), resilience, and social support were significantly associated with anxiety. In addition, depression and anxiety were significantly correlated (r=0.48). See Table 3.
Table 3.
Correlations among minority stress, psychosocial resource, and psychological distress factors, controlling for age, marital status, education, employment, income, and receipt of chemotherapy (N = 201).
| Variable | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| 1. Discrimination | 1 | |||||
| 2. Negative Identity | −0.01 | 1 | ||||
| 3. Outness | 0.07 | −0.39** | 1 | |||
| 4. Resilience | −0.16* | −0.12 | 0.02 | 1 | ||
| 5. Social Support | −0.16* | −0.12 | 0.05 | 0.29** | 1 | |
| 6. Depression | 0.18** | 0.09 | 0.14 | −0.43** | −0.27** | 1 |
| 7. Anxiety | 0.17* | 0.16* | 0.07 | −0.44** | −0.20** | 0.48** |
Note.
p < .05 (two-tailed);
p < .01 (two-tailed)
To address the potential limitation of combining lesbian and bisexual women in a single analysis, bivariate associations with both depression and anxiety were compared between the lesbian and bisexual subsamples. Differences in the values of associations between the subsamples were minimal. Also, associations were re-run without the 29 bisexual women to assess whether associated factors differed for lesbian women alone. The reported associations remained unchanged when looking only at the lesbian breast cancer survivors (data not shown).
Structural equation model for mediation of minority stress by psychosocial resources
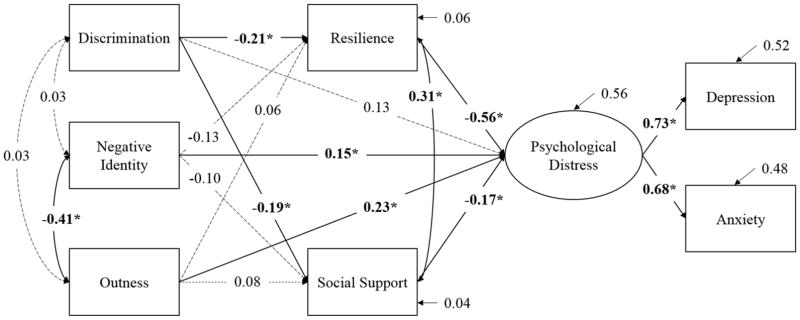
In testing the second hypothesis using structural equation modeling, a latent variable was constructed for psychological distress, comprising depression and anxiety. After the associations between minority stress factors and psychosocial resources were evaluated, these factors were entered into the model as manifest variables. Based on univariate associations and existing theory (Boehmer, Glickman, & Winter, 2012; Lehavot & Simoni, 2011; Meyer, 2003), age, education, income, and marital status were included in the model as potential confounders. Age was identified as a potential confounder of the relationships between negative identity and resilience and resilience and anxiety, and was included in the model as a predictor of both resilience and anxiety. Income was identified as a potential confounder of the relationships between resilience and depression and social support and depression, and was included as a predictor of resilience, social support, and depression. Education was identified as a potential confounder of the relationship between outness and resilience and resilience and depression, and was included as a predictor of resilience and depression. Marital status was identified as a potential confounder of the relationship between social support and depression, and was included as a predictor of social support and depression. Including these potential confounders did not materially affect the estimated association between variables in the model. The hypothesized model, which included psychosocial resource factors as mediators between minority stress and psychological distress, fit the data well, χ2 = 27.83, p > 0.05; CFI = 0.97; RMSEA = 0.04; TLI = 0.93. See Figure 2 for the complete model with standardized path estimates (confounders not shown).
Figure 2.
Completed structural equation model including standardized estimates (N = 201).
Notes. * Path is significant at p<0.05. The associations between minority stress and both psychological resources and psychological distress control for age and education; the associations between psychological resources and psychological distress control for age, income, education, and marital status (confounders not shown).
The total effects (direct and indirect) from all three minority stress factors to psychological distress were significant (discrimination standardized β=0.24, 95% CI = 0.09–0.40; negative identity β=0.26, 95% CI = 0.11–0.40; outness β=0.23, 95% CI = 0.08–0.34). The direct effects from outness (β=0.23, 95% CI = 0.11–0.36) and negative identity (β=0.15, 95% CI = 0.01–0.31) to psychological distress were significant and positive, while the direct effect from discrimination to distress was non-significant. The direct effects from resilience (β= −0.56, 95% CI = −0.73- −0.43) and social support (β= −0.17, 95% CI = −0.32- −0.01) to psychological distress were similarly significant, though negative. Discrimination demonstrated a significant positive indirect association with psychological distress through resilience (β=0.15, 95% CI = 0.07–0.25), indicating the presence of mediation. No other significant indirect effects emerged (see Table 4 for details). The model, including all direct and indirect effects, explained a total of 56.3% of the variance in the latent variable for psychological distress. However, associations with minority stress factors only explained a total of 7.3% and 6.0% of the variance in resilience and social support, respectively.
Table 4.
Standardized indirect effects of minority stress factors on psychological distress via psychosocial resources (N = 201).
| Indirect effect | β | SE | p |
|---|---|---|---|
| Discrimination via resilience | 0.15 | 0.04 | 0.02 |
| Discrimination via social support | 0.03 | 0.02 | 0.16 |
| Negative identity via resilience | 0.08 | 0.05 | 0.15 |
| Negative identity via social support | 0.02 | 0.02 | 0.34 |
| Outness via resilience | −0.02 | 0.05 | 0.65 |
| Outness via social support | −0.01 | 0.02 | 0.42 |
Discussion
Lesbian and bisexual breast cancer survivors may experience mental health disparities relative to their heterosexual counterparts (Kamen, Mustian, Dozier, et al., 2015), and their psychological well-being may be impacted by unique factors such as minority stress (Boehmer, Glickman, & Winter, 2012; Boehmer et al., 2013). The current study assessed the association of demographic, clinical, minority stress, and psychosocial resource factors with psychological distress in a sample of sexual minority breast cancer survivors. As such, this study represents one of the few attempts to characterize both minority stress and positive psychosocial resources, such as resilience, in the context of breast cancer. The study’s first hypothesis, that discrimination and negative minority identity would be positively associated while greater outness, resilience, and social support would be negatively associated with psychological distress, was partially supported. Both discrimination and negative identity were significantly and positively associated with psychological distress in bivariate analyses and a structural equation model. Similarly, resilience and social support had significant negative associations on psychological distress, while outness, contrary to the hypothesis, had a significant positive association. The study’s second hypothesis, that psychosocial resources would mediate the association between minority stress and psychological distress, was also partially supported. Resilience significantly mediated the relationship between discrimination and psychological distress, though social support did not serve as a significant mediator.
A notable percentage of sexual minority breast cancer survivors in this sample reported borderline abnormal or clinically significant levels of depression and anxiety (15.4% and 28.8%, respectively). A theoretically-based model was able to account for a significant proportion (56%) of the variance in these psychological distress outcomes. It is notable that even among these well-educated, high socioeconomic status women, exposure to discrimination was common; over half of the sample reported having experienced discrimination based on their sexual minority identity, gender, or both. Experience of discrimination related to sexual minority identity or gender was associated with both depression and anxiety. However, in a model including both minority stress factors and psychosocial resources, the direct effect of discrimination on psychological distress was non-significant. Rather, as mentioned above, resilience, or the capacity to recover emotional equilibrium after hardship, mediated the association between discrimination and psychological distress. While assessing minority stress factors such as discrimination may be important, therefore, it is also important to attend to positive psychosocial resources that may be associated with psychological wellness.
The current study was cross-sectional and can speak only to statistical and not predictive associations between variables; however, this mediation of the relationship between discrimination and distress may point to processes described by Hatzenbuehler (2009) in his extension of the minority stress model. Specifically, discrimination may impact psychological functioning only insofar as individuals are unable to muster psychosocial resources in response. Individuals who cope with exposure to discrimination and other manifestations of minority stress by developing resilience may be buffered against distress (Kamen, Burns, & Beach, 2011). While the current study was focused on positive psychosocial resources and not maladaptive coping strategies, previous research has indicated that those who dwell on or ruminate about experiences of discrimination, or who anticipate future discrimination, may be more likely to experience anxiety and depression (Hatzenbuehler, Dovidio, Nolen-Hoeksema, & Phills, 2009). It is possible, however, that the directionality of the relationships may differ for certain individuals in certain circumstances; for example, greater resilience could foster less frequent anticipation of discrimination. Further research will be needed to test associations between minority stress, psychosocial resources, and coping strategies longitudinally in samples of sexual minority cancer survivors to evaluate the temporal relationships between these variables.
It is also notable that outness, generally considered to be a positive and adaptive process for sexual minority women, was associated with increased psychological distress among the current sample of sexual minority breast cancer survivors. Outness was also negatively associated with negative minority identity, as would be expected; those who have come out to a greater number of individuals would be less likely to feel shame or internalized homophobia about their same-sex attraction or sexual identity. However, for as much as outness may serve as a marker for identity growth and development, it may also lead to increased stress and anxiety. Cancer diagnosis and treatment involves interacting with dozens of health and social service providers and a lesbian cancer survivor must decide to whom she comes out. Previous research has indicated that the process of coming out in cancer care can be stressful for sexual minority patients (Margolies, 2014). Coming out can also be stressful in the life of sexual minority women in general, and can expose women to additional discrimination and prejudice. Some sexual minority women with cancer report that they experience rejection and social isolation because of fear of cancer felt by their sexual minority community (Sinding, Grassau, & Barnoff, 2006), causing additional outness-related distress. Further research is necessary to unpack unique associations between cancer, distress, and outness, and to identify what psychological mechanisms may operate in tandem with outness to increase psychological distress.
In keeping with the results of previous studies, this study found few differences between lesbian and bisexual cancer survivors. Though other studies have noted that bisexual women in the population at large have worse mental health than lesbian women (Fredriksen-Goldsen et al., 2010), it may be that the experience of breast cancer overshadows any differences between sexual orientation groups in psychological distress. It may also be that the sample for the current study was too homogeneous in terms of demographic and other background characteristics to highlight differences between bisexual and lesbian breast cancer survivors. Larger population-based studies with more diverse samples and more specific efforts to recruit bisexual women are needed to fully examine these differences by sexual orientation.
The findings of this study, while preliminary, point to potential areas for future research and intervention development. Given the importance of intervening to reduce psychological distress and the association of resilience, as a statistical mediator, with distress, interventions to facilitate the development of resilience among sexual minority breast cancer survivors may be warranted. Future research to inform such an intervention development effort should use a more comprehensive assessment of both adaptive and maladaptive coping strategies. Coping and resilience-building interventions could be expanded to the community context to aid in the development of psychosocial resources among healthy community-dwelling sexual minority women (McElroy, Wintemberg, Cronk, & Everett, 2015). Targeted interventions could then be used to bolster these skills among women diagnosed with and undergoing treatment for breast cancer.
Limitations and Strengths
Findings of the current study must be interpreted in the light of several limitations. First, this was a cross-sectional, self-report based study, and therefore describing temporal and causal relationships is not possible; only associations between variables of interest are described. These associations may be skewed by self-report bias. Results should be replicated using longitudinal designs and assessment modalities other than phone interview (e.g., paper-and-pencil, online). Second, the sample for this study was largely non-Hispanic White, very well educated, and an average of 5 years post breast cancer diagnosis. Generalizability is limited with regards to other populations of sexual minority breast cancer survivors, or sexual minority cancer survivors more broadly. Because of the study’s relatively small sample size, it was impossible to stratify or examine subgroups of survivors that may have different mental health outcomes. In addition, the data used for this study did not include the complement of variables needed to conduct a full test of the minority stress model.
The current study also had several strengths. It is the first study focused on sexual minority breast cancer survivors to evaluate the contribution of positive psychosocial resources to mental health. In a structural equation model assessing psychological distress, both resilience and social support were significant factors. Efforts to address depression and anxiety among sexual minority cancer survivors should consider capitalizing on and enhancing these psychosocial resources.
Conclusion
The current study is one of the few to look at the association of minority stress and psychosocial resources with psychological distress in sexual minority breast cancer survivors. Our results, while preliminary, indicate the importance of attending to psychological mediation factors such as resilience, even in the context of unique stressors such as discrimination and outness. This study will hopefully serve as a jumping off point for further research aimed at improving the mental health of sexual minority women with breast cancer, and sexual minority cancer populations more generally.
Acknowledgments
Funding: This study was supported by National Cancer Institute grants K07 CA190529 (PI: Kamen), UG1 CA189961 and R25CA102618-01A1 (PI: Morrow), and the American Cancer Society grant RSGT-06-135-01-CPPB (PI: Boehmer). Additional supplemental funding was made available by a Boston University School of Public Health pilot grant. Recruitment of breast cancer survivors was made possible by the Dr. Susan Love Research Foundation’s Love/Avon Army of Women Program.
Footnotes
Conflict of Interest: All authors declare that they have no conflicts of interest.
References
- Arena PL, Carver CS, Antoni MH, Weiss S, Ironson G, Duran RE. Psychosocial responses to treatment for breast cancer among lesbian and heterosexual women. Women Health. 2006;44(2):81–102. doi: 10.1300/j013v44n02_05. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17255060. [DOI] [PubMed] [Google Scholar]
- Bare MG, Margolies L, Boehmer U. Omission of Sexual and Gender Minority Patients. Journal of Clinical Oncology. 2014 doi: 10.1200/JCO.2014.55.6126. [DOI] [PubMed] [Google Scholar]
- Boehmer U. Breast cancer in lesbian and bisexual women. In: Boehmer U, Elk R, editors. Cancer and the LGBT Community: Unique Perspectives from Risk to Survivorship. Cham: Springer; 2015. pp. 141–157. [Google Scholar]
- Boehmer U, Case P. Physicians don’t ask, sometimes patients tell: disclosure of sexual orientation among women with breast carcinoma. Cancer. 2004;101(8):1882–1889. doi: 10.1002/cncr.20563. [DOI] [PubMed] [Google Scholar]
- Boehmer U, Glickman M, Milton J, Winter M. Health-related quality of life in breast cancer survivors of different sexual orientations. Qual Life Res. 2012;21(2):225–236. doi: 10.1007/s11136-011-9947-y. [DOI] [PubMed] [Google Scholar]
- Boehmer U, Glickman M, Winter M. Anxiety and depression in breast cancer survivors of different sexual orientations. J Consult Clin Psychol. 2012;80(3):382–395. doi: 10.1037/a0027494. [DOI] [PubMed] [Google Scholar]
- Boehmer U, Glickman M, Winter M, Clark MA. Lesbian and bisexual women’s adjustment after a breast cancer diagnosis. Journal of American Psychiatric Nurses Association. 2013;19(5):280–292. doi: 10.1177/1078390313504587. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12602425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFulvio GT. Sexual minority youth, social connection and resilience: from personal struggle to collective identity. Soc Sci Med. 2011;72(10):1611–1617. doi: 10.1016/j.socscimed.2011.02.045. [DOI] [PubMed] [Google Scholar]
- Donovan KA, Gonzalez BD, Small BJ, Andrykowski MA, Jacobsen PB. Depressive symptom trajectories during and after adjuvant treatment for breast cancer. Ann Behav Med. 2014;47(3):292–302. doi: 10.1007/s12160-013-9550-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Balsam KF, Mincer SL. Disparities in health-related quality of life: a comparison of lesbians and bisexual women. Am J Public Health. 2010;100(11):2255–2261. doi: 10.2105/AJPH.2009.177329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Chida Y, Molloy GJ. Psychological distress and cancer mortality. J Psychosom Res. 2009;66(3):255–258. doi: 10.1016/j.jpsychores.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Dovidio JF, Nolen-Hoeksema S, Phills CE. An Implicit Measure of Anti-Gay Attitudes: Prospective Associations with Emotion Regulation Strategies and Psychological Distress. J Exp Soc Psychol. 2009;45(6):1316–1320. doi: 10.1016/j.jesp.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabson JM, Bowen DJ. Perceived stress and sexual orientation among breast cancer survivors. J Homosex. 2014;61(6):889–898. doi: 10.1080/00918369.2014.870814. [DOI] [PubMed] [Google Scholar]
- Jabson JM, Donatelle RJ, Bowen DJ. Relationship between sexual orientation and quality of life in female breast cancer survivors. J Womens Health (Larchmt) 2011;20(12):1819–1824. doi: 10.1089/jwh.2011.2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jassim GA, Whitford DL, Hickey A, Carter B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst Rev. 2015;5:CD008729. doi: 10.1002/14651858.CD008729.pub2. [DOI] [PubMed] [Google Scholar]
- Kamen C, Burns M, Beach SR. Minority stress in same-sex male relationships: when does it impact relationship satisfaction? J Homosex. 2011;58(10):1372–1390. doi: 10.1080/00918369.2011.614904. [DOI] [PubMed] [Google Scholar]
- Kamen C, Heckler C, Janelsins MC, Peppone LJ, McMahon JM, Morrow GR, … Mustian KM. A Dyadic Intervention to Reduce Psychological Distress Among Lesbian, Gay, and Heterosexual Cancer Survivors. LGBT Health. 2016;3(1) doi: 10.1089/lgbt.2015.0101. E-pub before print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamen C, Mustian KM, Dozier A, Bowen DJ, Li Y. Disparities in psychological distress impacting lesbian, gay, bisexual and transgender cancer survivors. Psychooncology. 2015 doi: 10.1002/pon.3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamen C, Mustian KM, Heckler C, Janelsins MC, Peppone LJ, Mohile S, … Morrow GR. The association between partner support and psychological distress among prostate cancer survivors in a nationwide study. J Cancer Surviv. 2015;9(3):492–499. doi: 10.1007/s11764-015-0425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamen C, Smith-Stoner M, Heckler CE, Flannery M, Margolies L. Social support, self-rated health, and lesbian, gay, bisexual, and transgender identity disclosure to cancer care providers. Oncology nursing forum. 2015;42(1):44–51. doi: 10.1188/15.ONF.44-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertzner RM, Meyer IH, Frost DM, Stirratt MJ. Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. Am J Orthopsychiatry. 2009;79(4):500–510. doi: 10.1037/a0016848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon P. Resilience in lesbian, gay, and bisexual individuals. Pers Soc Psychol Rev. 2013;17(4):371–383. doi: 10.1177/1088868313490248. [DOI] [PubMed] [Google Scholar]
- Legate N, Ryan RM, Weinstein N. Is Coming Out Always a “Good Thing”? Exploring the Relations of Autonomy Support, Outness, and Wellness for Lesbian, Gay, and Bisexual Individuals. Social Psychological and Personality Science. 2012;3(2):145–152. doi: 10.1177/1948550611411929. [DOI] [Google Scholar]
- Lehavot K, Simoni JM. The impact of minority stress on mental health and substance use among sexual minority women. J Consult Clin Psychol. 2011;79(2):159–170. doi: 10.1037/a0022839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester J, Crosthwaite K, Stout R, Jones RN, Holloman C, Shapiro C, Andersen BL. Women with breast cancer: self-reported distress in early survivorship. Oncology nursing forum. 2015;42(1):E17–23. doi: 10.1188/15.ONF.E17-E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maass SW, Roorda C, Berendsen AJ, Verhaak PF, de Bock GH. The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas. 2015;82(1):100–108. doi: 10.1016/j.maturitas.2015.04.010. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. Mahwah, NJ: Erlbaum; 2008. [Google Scholar]
- Mao JJ, Armstrong K, Bowman MA, Xie SX, Kadakia R, Farrar JT. Symptom burden among cancer survivors: impact of age and comorbidity. J Am Board Fam Med. 2007;20(5):434–443. doi: 10.3122/jabfm.2007.05.060225. [DOI] [PubMed] [Google Scholar]
- Margolies L. The psychosocial needs of lesbian, gay, bisexual, or transgender patients with cancer. Clinical journal of oncology nursing. 2014;18(4):462–464. doi: 10.1188/14.CJON.462-464. [DOI] [PubMed] [Google Scholar]
- McElroy JA, Wintemberg JJ, Cronk NJ, Everett KD. The association of resilience, perceived stress and predictors of depressive symptoms in sexual and gender minority youths and adults. Psychology & Sexuality. 2015 doi: 10.1080/19419899.2015.1076504. [DOI] [Google Scholar]
- McElroy JA, Wintemberg JJ, Cronk NJ, Everett KD. The association of resilience, perceived stress and predictors of depressive symptoms in sexual and gender minority youths and adults. Psychology & Sexuality. 2016;7(2):116–130. doi: 10.1080/19419899.2015.1076504. [DOI] [Google Scholar]
- McGregor BA, Carver CS, Antoni MH, Weiss S, Yount SE, Ironson G. Distress and internalized homophobia among lesbian women treated for early stage breast cancer. Psychology of Women Quarterly. 2001;25(1):1–9. doi: 10.1111/1471-6402.00001. [DOI] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36(1):38–56. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7738327. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, Fassinger RE. Measuring dimensions of lesbian and gay male experience. Measurement and evaluation in counseling and development : the official publication of the Association for Measurement and Evaluation in Counseling and Development. 2000;33:66–90. [Google Scholar]
- Peterson TL, Gerrity DA. Internalized homophobia, lesbian identity development, and self-esteem in undergraduate women. J Homosex. 2006;50(4):49–75. doi: 10.1300/J082v50n04_03. [DOI] [PubMed] [Google Scholar]
- Raykov T, Marcoulides GA. A first course in structural equation modeling. 2. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 2006. [Google Scholar]
- Saboonchi F, Petersson LM, Wennman-Larsen A, Alexanderson K, Brannstrom R, Vaez M. Changes in caseness of anxiety and depression in breast cancer patients during the first year following surgery: patterns of transiency and severity of the distress response. Eur J Oncol Nurs. 2014;18(6):598–604. doi: 10.1016/j.ejon.2014.06.007. [DOI] [PubMed] [Google Scholar]
- Sinding C, Grassau P, Barnoff L. Community support, community values:the experiences of lesbians diagnosed with cancer. Women Health. 2006;44(2):59–79. doi: 10.1300/j013v44n02_04. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17255059. [DOI] [PubMed] [Google Scholar]
- Singer S, Kuhnt S, Gotze H, Hauss J, Hinz A, Liebmann A, Schwarz R. Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. British journal of cancer. 2009;100(6):908–912. doi: 10.1038/sj.bjc.6604952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton AL, Morra ME, Diefenbach MA, Miller SM, Slevin Perocchia R, Raich PC, … Marcus AC. Responding to a significant recruitment challenge within three nationwide psychoeducational trials for cancer patients. J Cancer Surviv. 2013;7(3):392–403. doi: 10.1007/s11764-013-0282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuber J, Galea S, Ahern J, Blaney S, Fuller C. The association between multiple domains of discrimination and self-assessed health: a multilevel analysis of Latinos and blacks in four low-income New York City neighborhoods. Health Serv Res. 2003;38(6 Pt 2):1735–1759. doi: 10.1111/j.1475-6773.2003.00200.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14727795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymanski DM, Chung YB, Balsam KF. Psychosocial correlates of internalized homophobia in lesbians. Measurement and evaluation in counseling and development : the official publication of the Association for Measurement and Evaluation in Counseling and Development. 2001;34:27–38. [Google Scholar]
- Von Ah D, Kang DH. Correlates of mood disturbance in women with breast cancer: patterns over time. J Adv Nurs. 2008;61(6):676–689. doi: 10.1111/j.1365-2648.2007.04563.x. [DOI] [PubMed] [Google Scholar]
- Wagnild G. A review of the Resilience Scale. J Nurs Meas. 2009;17(2):105–113. doi: 10.1891/1061-3749.17.2.105. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19711709. [DOI] [PubMed] [Google Scholar]
- Wagnild G, Young HM. Resilience among older women. Image J Nurs Sch. 1990;22(4):252–255. doi: 10.1111/j.1547-5069.1990.tb00224.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2292448. [DOI] [PubMed] [Google Scholar]
- Wagnild G, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–178. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7850498. [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6880820. [DOI] [PubMed] [Google Scholar]