Summary
Background
Hepatic portal venous gas (HPVG) is a rare imaging finding in children. It can be an important manifestation of severe diseases such as necrotizing enterocolitis (NEC) in neonates or bowel wall rupture in older children. However, there are many other diseases presenting with HPVG that do not necessarily require a surgical intervention.
Case Report
In the period between 2011–2015, there were 12 cases of HPVG in children aged up to 24 months in our hospital. We did not include children with NEC. We retrospectively analyzed clinical data and US examinations as regards the suspected causes and final diagnoses.
Only 1 patient with HPVG required an immediate surgical intervention. This was – a 4-month-old girl 32 days after a repair of a congenital diaphragmatic hernia, with ultrasound signs of acute bowel wall necrosis. During surgery a bowel strangulation was revealed.
Other causes included: – 4 patients with bowel inflammation (including complications of neoplastic diseases such as leukemia and Hodgkins’disease); – 3 patients with food allergy; – 1 patient with acute gastroenteritis; – 1 patient with hepatic injury because of a suspected metabolic disease; – 1 incidental finding revealed before closing a ventricular septum defect; – 1 patient during follow-up performed 2 weeks after a reconstruction of bowel continuity.
Conclusions
HPVG is not always a sign of a life-threatening condition and it should not be by itself an indication for surgical treatment.
HPVG requires a close monitoring of the clinical status, which is crucial for further management. In patients in non-severe clinical condition, we propose to perform a follow-up ultrasound imaging within 1–2 days, and not to extend diagnostic procedures, especially in case of ultrasound picture normalization.
An abdominal ultrasound examination appears to be the method of choice for the identification of gas in the hepatic portal system in children.
MeSH Keywords: Enterocolitis, Necrotizing; Gastroenterology; Portal Vein
Background
Hepatic venous gas (HPVG) is a rare finding, especially in children. It is usually seen as a sign of a serious disease, which results in introducing parenteral nutrition, antibiotics or even surgery, e.g. in pre-term neonates with severe necrotizing enterocolitis (NEC) or in the case of perforation of the gastrointestinal tract in older children.
However, there is a number of other conditions that can also cause HPVG that do not require any surgical intervention and should only be monitored by imaging.
Case Report
Based on abdominal ultrasound findings, we determined the following causes of HPVG – food allergy (3 cases), enterocolitis (4 cases, inclusive of neoplasm treatment complications), acute gastroenteritis caused by rotaviruses and adenoviruses (1 case), hepatic injury because of a suspected metabolic liver disease (1 case), an incidental finding revealed before closing a ventricular septum defect (1 case), and one patient 2 weeks after reconstuction of bowel continuity. Only 1 patient with HPVG required an immediate surgical intervention. This was a 4-month-old girl, 32 days after repair of a congenital diaphragmatic hernia with ultrasound signs of acute bowel wall necrosis. Bowel strangulation was revealed during surgery. The clinical data of patients are presented in Table 1, which contains also the type of imaging modality used and the time to resolution of abnormal ultrasound image.
Table 1.
The clinical data of patients.
| No. | Age (months) | Gender | Indication for imaging | Diagnosis | Normalisation of ultrasound findings (days) | Performance of abdominal radiograph/signs of HPVG | Surgical treatment |
|---|---|---|---|---|---|---|---|
| 1 | 1 | M | Low body mass, diarrhoea | Acute gastroenteritis because of rotavirus and adenovirus infection | 3 | No | No |
| 2 | 1 | M | Lower gastrointestinal tract haemorrhage | Anaemia, food allergy | 47 | No | No |
| 3 | 2 | M | History of abdominal surgery 2 days after birth because of ileus | Hepatic injury because of a suspected liver metabolic disease | 1 | Yes/no | No |
| 4 | 4 | F | Bruising of the lower half of the body after surgery for congenital diaphragmatic hernia | Bowel stranglulation | 4 | Yes/signs of subileus | Yes |
| 5 | 4 | M | Abdominal pain, lower gastrointestinal tract haemorrhage | Food allergy | 1 | No | No |
| 6 | 4 | M | Condition after gastroschisis. 2 weeks after reconstruction of continuity of bowel (after jejunostomy) | Routine imaging | Partial resolution of symptoms, no follow-up | No | No |
| 7 | 4 | M | Haematemesis, lower gastrointestinal tract haemorrhage | Food allergy | 1 | Yes/no | No |
| 8 | 4 | M | Routine imaging before surgical closing a ventricular septum defect | Ventricular septum defect | No follow-up | No | No |
| 9 | 5 | F | Follow-up after necrotizing enterocolitis and resection of the ileum in the third month of life | Enteritis | 1 | No | No |
| 10 | 8 | M | Fever, diarrhoea | Enteritis | 2 | No | No |
| 11 | 23 | M | Abdominal pain in acute myeloid leukaemia | Acute myeloid leukaemia, enteritis | 2 | Yes/signs of ileus | No |
| 12 | 24 | M | Diarrhoea and vomiting in acute myeloid leukaemia | Jejunitis | 3 | Yes/bowel wall pneumatosis | No |
In each case an abdominal ultrasound was performed that revealed hyperechogenic air bubbles in the portal vein and a number of hyperechogenic foci in the liver parenchyma (Figures 1–3). In 5 patients, an abdominal radiograph was performed on the same day as ultrasound examination, as ordered by a surgeon, which did not reveal any signs of HPVG (Figure 4). The examination showed bowel wall pneumatosis only in one of the patients who had enteritis due to acute myeloid leukemia.
Figure 1.
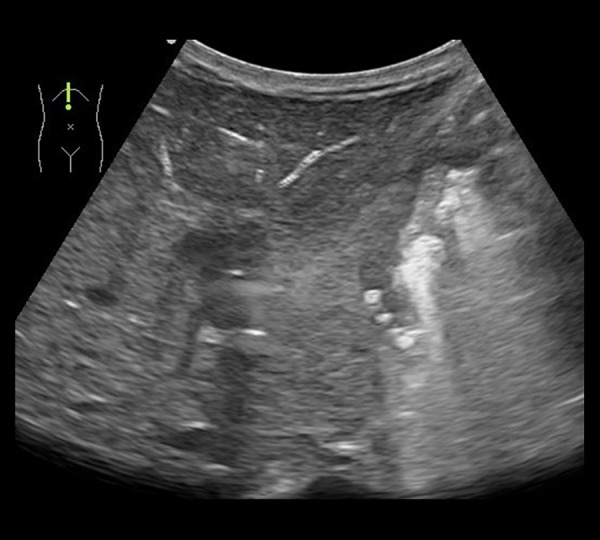
Adbominal ultrasound in a 4-month-old boy shows small hyperechogenic reflections branching in the liver parenchyma.
Figure 2.
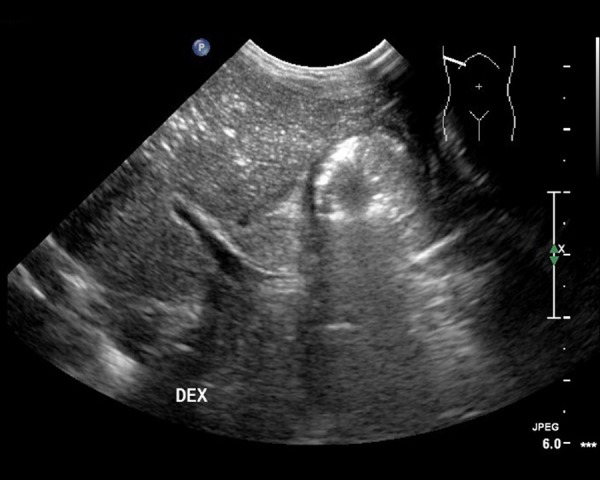
Follow-up abdominal US examination in a 5-month-old girl after NEC and a partial small bowel resection performed in the third month of age. The US image shows small gas bubbles in the liver parenchyma and in the branches of the portal vein.
Figure 3.
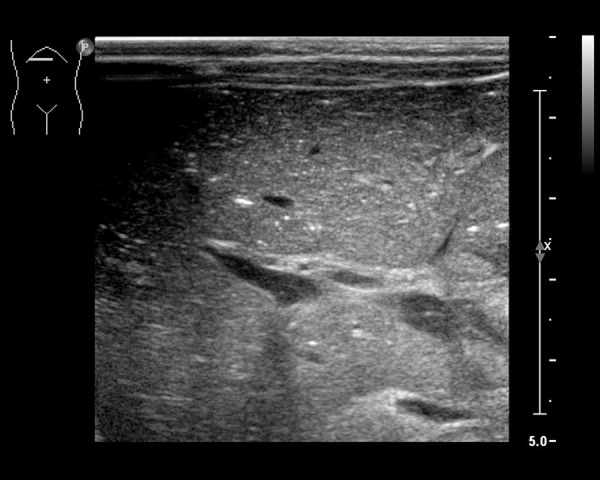
US scan of a 2-month-old boy with a suspicion of a metabolic disease of the liver.
Figure 4.
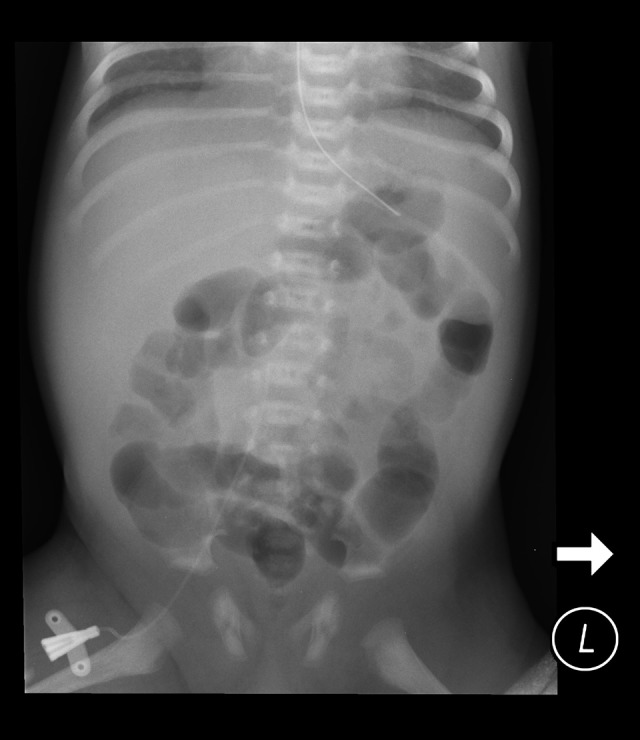
The same patient as in Figure 3. Abdominal radiograph shows no signs of HPVG.
Eleven patients were followed up with ultrasound examination within several days after HPVG diagnosis. One patient was not followed up because of a transfer to another hospital. We observed a complete resolution of HPVG in all 10 patients – in four cases, it was seen on the next day, in 5 cases within 2–4 days. Only one child had persistent HPVG on ultrasound examinations within the next 28 days, and a complete resolution was seen on day 47. This patient was 1-month old and had lower gastrointestinal haemorrhage and a co-existing allergy to milk protein and anaemia. In one case HPVG partially normalized and was not followed up by further imaging. None of the patients required abdominal CT.
Discussion
The mechanisms of HPVG have not been clearly explained. There are several theories, and the most prevalent include [1–3]:
migration of air bubbles through the portal capillaries due to an increased pressure in the intestinal loops.
break-down of the intestinal mucous membrane and subsequent migration of a gas formed by microorganisms in the intestinal lumen with through mesenteric veins into the portal system.
presence of gas-producing bacteria in the inflammatory areas in the abdomen, e.g. in acute appendicitis or enteritis.
Gas in the portal vein migrates to its intrahepatic branches and then to peripheral parts of the liver parenchyma [1,2,4].
HPVG is not a stand-alone disease but it accompanies other diseases of the abdomen [4].
On an abdominal radiograph, HPVG can be seen as branching peripheral radiolucencies. However, the sensitivity of this examination is low, and it allows to recognize HPVG mostly in severe clinical conditions [1,5].
Computed tomography (CT) is the gold standard for the detection of HPVG in adults [1]. It is a useful tool enabling an early detection of HPVG with a possible determination of its cause [2,6]. Certain CT settings (e.g. the lung window) help to detect even small amount of air in liver parenchyma [1,2]. Gas in the portal venous system appears usually in the peripheral branches of the portal vein, primarily in the anterior hepatic segments, within 2 cm of the liver capsule. This should be differentiated from the presence of gas in the biliary system where gas is observed in the central parts of the liver, more than 2 cm from the liver capsule. This difference in air distribution between the portal vein system and the biliary system results primarily from the opposite directions of flow of venous blood and bile [1,4].
CT is not the method of choice in children because of a large radiation dose. Therefore, ultrasound imaging is used instead, which is safe and can be used serially to diagnose pathology and follow-up. On ultrasound, HPVG presents as hyperechogenic air bubbles moving in the direction of blood flow in the portal vein or as scattered small hyperechogenic points in the liver parenchyma [1,5]. The available literature on HPVG concerns primarily adult patients. In children, NEC is reported as the most frequent cause of HPVG [7,8]. Other causes of HPVG in children include umbilical vein cannulation, haemolytic disease, Crohn’s disease, intestinal tuberculosis, ileus, intestinal perforation and abdominal surgery [5,9].
NEC is a disease that affects primarily pre-term neonates. It affects 1–5% of children treated in intensive care units and up to 10% of children with a birth mass lower than 1500 g [10,11]. Notably, 10% cases of HPVG can affects full-term children with a disease that predisposes to impaired perfusion of the mesentery (e.g. patent ductus arteriosus, congenital heart defects, sepsis, polycythaemia, foetal cocaine exposure, RDS, umbilical vein cannulation) [5].
When the clinical presentation is not typical for NEC, including an unusual patient age, other causes of HPVG should be taken into account. In our study the most frequent causes of HPVG were enterocolitis and food allergies. Clinical condition of the most patients did not require surgical intervention. Ultrasound imaging was the modality of choice for both the diagnosis and monitoring of HPVG. In the majority of cases, a resolution of ultrasound findings was observed within 1–4 days after diagnosis.
Therefore, we recommend that patients who do not require surgery be followed up with an abdominal ultrasound 1–2 days after diagnosis of HPVG. Moreover, we recommend to refrain in most cases from using abdominal radiography and abdominal CT.
Conclusions
HPVG is not an absolute indication for surgery and does not necessarily indicate a severe disease. HPVG requires close clinical monitoring of the patient, based on which treatment should be planned.
If there are no indications for surgery, we recommend to perform abdominal ultrasound within 1–2 day after the diagnosis, without the need of using other imaging modalities such as abdominal radiography or abdominal CT, especially in case of image normalization in follow-up ultrasound studies.
Abdominal ultrasound is sufficient to detect HPVG in children and should be used as a method of choice, also for follow-up.
References
- 1.McElvanna K, Campbell A, Diamond T. Hepatic portal venous gas – three non-fatal cases and review of the literature. Ulster Med J. 2012;81(2):74–78. [PMC free article] [PubMed] [Google Scholar]
- 2.Nelson AL, Millington TM, Sahani D, et al. Hepatic portal venous gas: The ABCs of management. Arch Surg. 2009;144(6):575–81. doi: 10.1001/archsurg.2009.88. [DOI] [PubMed] [Google Scholar]
- 3.Tan EW, Smith MD. A rare occurrence of hepatic portal venous gas in a patient with chemotherapy-induced enterocolitis: The rise of benign aetiologies. J Surg Case Rep. 2015;9:1–3. doi: 10.1093/jscr/rjv114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allaparthi SB, Anand CP. Acute gastric dilatation: A transient cause of hepatic portal venous gas – case report and review of the literature. Case Rep Gastrointest Med. 2013;2013:723160. doi: 10.1155/2013/723160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abboud B, El Hachem J, Yazbeck T, Doumit CL. Hepatic portal venous gas: Physiopathology, etiology, prognosis and treatment. World J Gastroenterol. 2009;15(29):3585–90. doi: 10.3748/wjg.15.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alqahtani S, Coffin CS, Burak K, et al. Hepatic portal venous gas: A report of two cases and a review of the epidemiology, pathogenesis, diagnosis and approach to management. Can J Gastroenterol. 2007;21(5):309–13. doi: 10.1155/2007/934908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moser A, Stauffer A, Wyss A, et al. Conservative treatment of hepatic portal venous gas consecutive to acomplicated diverticulitis: A case report and literature review. Int J Surg Case Rep. 2016;23:186–89. doi: 10.1016/j.ijscr.2016.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inokuchi R, Fukuda T, Yahagi N, Nakamura K. Severe hepatic portal venous gas that spontaneously resolved within a day. Intensive Care Med. 2014;40:1369. doi: 10.1007/s00134-014-3390-9. [DOI] [PubMed] [Google Scholar]
- 9.Alp H, Orbak Z, Sepetcigil O, et al. Abdominal tuberculosis in a child presenting with radiological evidence of pneumatosis intestinalis and portal venous gas. J Health Popul Nutr. 2010;28(6):628–32. doi: 10.3329/jhpn.v28i6.6612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epelman M, Daneman A, Navarro OM, et al. Necrotizing enterocolitis: Review of state-of-the-art imaging findings with pathologic correlation. Radiographics. 2007;27:285–305. doi: 10.1148/rg.272055098. [DOI] [PubMed] [Google Scholar]
- 11.Eaton S, Rees CM, Hall NJ. Current research in necrotizing enterocolitis. Early Hum Dev. 2016;97:33–39. doi: 10.1016/j.earlhumdev.2016.01.013. [DOI] [PubMed] [Google Scholar]


